Abstract
BACKGROUND
While victims of intimate partner violence (IPV) present to health care settings for a variety of complaints; rates and predictors of case identification and intervention are unknown.
OBJECTIVE
Examine emergency department (ED) case finding and response within a known population of abused women.
DESIGN
Retrospective longitudinal cohort study.
SUBJECTS
Police-involved female victims of IPV in a semi-rural Midwestern county.
MAIN MEASURES
We linked police, prosecutor, and medical record data to examine characteristics of ED identification and response from 1999–2002; bivariate analyses and logistic regression analyses accounted for the nesting of subjects’ with multiple visits.
RESULTS
IPV victims (N = 993) generated 3,426 IPV-related police incidents (mean 3.61, median 3, range 1–17) over the 4-year study period; 785 (79%) generated 4,306 ED visits (mean 7.17, median 5, range 1–87), which occurred after the date of a documented IPV assault. Only 384 (9%) ED visits occurred within a week of a police-reported IPV incident. IPV identification in the ED was associated with higher violence severity, being childless and underinsured, more police incidents (mean: 4.2 vs 3.3), and more ED visits (mean: 10.6 vs 5.5) over the 4 years. The majority of ED visits occurring after a documented IPV incident were for medical complaints (3,378, 78.4%), and 72% of this cohort were never identified as victims of abuse. IPV identification was associated with the day of a police incident, transportation by police, self-disclosure of “domestic assault,” and chart documentation of mental health and substance abuse issues. When IPV was identified, ED staff provided legally useful documentation (86%), police contact (50%), and social worker involvement (45%), but only assessed safety in 33% of the women and referred them to victim services 25% of the time.
CONCLUSION
The majority of police-identified IPV victims frequently use the ED for health care, but are unlikely to be identified or receive any intervention in that setting.
KEY WORDS: intimate partner violence, police incidents, health care screening, risk identification, interventions, emergency departments
BACKGROUND
Intimate partner violence (IPV) is a major source of morbidity and mortality, with women suffering a lifetime prevalence rate of 22% and long-term consequences,1–6 including chronic pain, anxiety, depression, somatic concerns, and substance abuse.7–11 There is ample evidence that routine IPV screening will identify victims,12,13 but no high-quality evidence showing that screening in health care settings improves outcomes for abused women.14 Most provider organizations recommend routine screening,15–18 and emergency departments (EDs) have mandated protocols for screening and intervention.19 However, neither the US Preventive Services Task Force (USPSTF) nor the Canadian Task Force on Preventative Health Care endorses these recommendations.14,20 This perspective has been reinforced by a large randomized trial of IPV screening that found no significant differences between intervention and control groups at 18 months.21 The accompanying editorial suggested that health care’s focus should be shifted from universal screening to case finding and identifying effective interventions for IPV. However, rates and predictors of current case finding and interventions are unknown. This knowledge is needed before we can discuss whether identification and intervention in health care settings have the potential to reduce the number of future IPV-related incidents.
An integrated longitudinal database of prosecutor, police, and ED records for a cohort of police-identified IPV victims allows us to address three questions: (1) How effective are providers at IPV case finding? (2) What are the person- and visit-level characteristics associated with case finding? (3) What interventions are provided when IPV is identified? Based on prior work,22,23 we hypothesized that IPV case finding would be predominately related to victim presentation with IPV assault.
METHODS
This is a retrospective longitudinal cohort study of county-wide ED and criminal justice records for all female IPV victims identified by police and prosecutors during the year 2000. We examined all ED visits and IPV-related police events for a 4-year period (1999–2002), within 8 emergency departments (EDs), 12 police jurisdictions, and the prosecuting attorney’s office, with attention to the temporal relationship of ED visits to police-reported IPV incidents. The institutional review boards of involved hospital systems approved this study with HIPAA exemption, in cooperation with the Michigan Department of Community Health.
Study Population Our cohort was composed of women aged 16 or older identified as victims in heterosexual IPV assault cases in which police submitted charging requests to the prosecuting attorney in the year 2000.
Setting The semi-rural Midwest county, population 238,603, with 98,192 women aged 16 and above, has two hospital systems with eight EDs, which follow state law, JCAHO guidelines20, and hospital protocols requiring: (1) screening for violence on ED intake forms, (2) reporting of any assault-related injury to a police agency, (3) documenting known details of the assault, (4) safety planning, (5) medical social work evaluation, and (6) referral to community victim service agencies. Geography and medical utilization patterns are such that women would be unlikely to seek care in adjacent counties.
Data Collection We abstracted administrative records for the years 1999–2002 from all ED and criminal justice systems. Coding schemes for ED and police/prosecutor narratives were developed by independent review of all available records for a randomly selected subsample of 28 cases using consensus coding among five investigators, followed by iterative revisions during abstraction of the first several hundred cases, with re-abstraction of earlier records for any newly identified variables.
Prosecutor and Police All police and prosecutor case notes were reviewed for 993 “index assaults,” defined as the first police-reported assault in 2000 that brought the victim into the criminal justice system. We abstracted variables related to the victim, perpetrator, and assault incident, categorizing IPV severity into three categories: potentially lethal violence (choking, threatening with or using a weapon), high violence (threats to kill, rape, punching, stalking, broken bones, other injury), and lower violence (absence of the above potentially lethal or high violence indicators). Police administrative records from all 12 jurisdictions within the county provided counts and dates for all prior and subsequent IPV-related police incident reports during the 4-year study period. Based on input from our community advisory board and victim focus groups, police incidents were included if they mentioned both members of the study couple, even if they did not specifically reference IPV or result in chargeable offenses.
Emergency Department Records from all eight EDs, two level 1 trauma centers, and six affiliated tertiary care EDs were manually reviewed, including intake and discharge forms, physician dictations, paramedic and nursing notes, injury body map forms, photographs, social work notes, and violent injury report forms. A structured abstraction form captured date of visit, mode of arrival, chief complaint(s), discharge diagnoses, references to mental health or substance abuse conditions, staff actions regarding IPV and victim demographics (age, race, marital status, insurance status). Double coding was done during and at study completion for two 10% samples; kappa = 0.88 for IPV identification.
Data Analysis We first conducted person-level comparisons, stratifying by whether the participant had ever used the ED, during or after the date when IPV was first identified through either criminal justice or ED records. Among victims using the ED, we stratified by whether IPV had been identified during any ED visit. Using chi-square for categorical and T-tests for continuous variables, we compared person-level characteristics of women whose IPV victimization was, versus was not, identified in the ED setting for: age, race, marital status, insurance, presence of children, IPV severity, mean and median number of police calls for IPV, and mean and median number of ED visits that occurred after a documented IPV assault. We then looked at visit-level characteristics, using logistic regression, adjusting for demographic, couple-related, and IPV event characteristics, to examine ED visit characteristics associated with IPV identification, looking particularly at whether the ED visit was temporally related (within 1 day) to a police call for service, transportation by police, the nature of the chief complaint, and whether mental health or substance abuse issues were noted.
ED Response to IPV For each case of identified IPV, we assessed the frequency and visit characteristics associated with documentation of five key components of the ED policy: (1) legally useful documentation, defined as: inclusion of direct quotes by the patient about the assault; documentation of forensic evidence; documentation of the identity of the assailant as spontaneously uttered by the patient; any statement that the injuries sustained are consistent with the described assault; (2) police report, as evidenced by documentation of police contact, Violent Injury Report form, or release form allowing ED staff to provide medical details or photographed injuries to police; (3) safety assessment or planning, defined liberally as any mention of patient safety; (4) ED social worker involvement.
Models accounted for nesting of multiple visits per person. Statistical analyses were conducted using Statistical Package for the Social Sciences (SPSS, Inc.), version 16.0.
RESULTS
The 993 victims of IPV assault in 2000 generated 3,426 police calls and 5,738 ED visits over the 4-year study period (1999–2002). Seventy-nine percent of the cohort (n = 785) had at least one ED visit after the date of the first IPV assault; the mean number of visits was 7.17 (median of 5, range 1–87). Mean number of police incidents over the 4-year period was 3.61 (median 3, range 1–17).
Table 1 illustrates differences between women who used, versus did not use, the ED subsequent to an IPV assault. ED users were more likely to be unmarried and African American, but were similar in assault severity and likelihood of seeking a civil personal protection order. However, ED users were more likely to have a subsequent police-reported IPV incident, with higher numbers of police calls for service (mean of 3.6) compared to 2.7 among non-ED users.
Table 1.
Characteristics of IPV-Involved Women Who Use the ED and Who Are Identified as IPV+
| Total | Used ED during study time period | IPV ever identified at ED visit (among 785 ED users) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| ED users | Did not use ED | Identified | Never identified | ||||||||
| N | (%) | N | (%) | p-value | N | (%) | N | (%) | p-value | ||
| Total | 993 | 785 | (79%) | 208 | (21%) | 213 | (27%) | 572 | (73%) | ||
| Age | 0.079 | 0.414 | |||||||||
| Less than 25 | 359 | 294 | (37.5) | 65 | (32.7) | 71 | (33.3) | 223 | (39.0) | ||
| 25–30 | 225 | 186 | (23.7) | 39 | (19.6) | 50 | (23.5) | 136 | (23.8) | ||
| 31–40 | 260 | 203 | (25.9) | 57 | (28.6) | 60 | (28.2) | 143 | (25.0) | ||
| Over 40 | 140 | 102 | (13.0) | 38 | (19.1) | 32 | (15.0) | 70 | (12.2) | ||
| Race | 0.021 | 0.913 | |||||||||
| Caucasian | 554 | 439 | (57.5) | 115 | (62.8) | 121 | (57.6) | 318 | (57.4) | ||
| African American | 364 | 306 | (40.1) | 58 | (31.7) | 83 | (39.5) | 223 | (40.3) | ||
| Other minority | 29 | 19 | (2.5) | 10 | (5.5) | 6 | (2.9) | 13 | (2.3) | ||
| Marital | <0.001 | 0.580 | |||||||||
| Ever married | 305 | 214 | (27.3) | 91 | (43.8) | 55 | (25.8) | 159 | (27.8) | ||
| Never married | 688 | 571 | (72.7) | 117 | (56.2) | 158 | (74.2) | 413 | (72.2) | ||
| Insurance | 0.149 | 0.024 | |||||||||
| Ever private | 312 | 280 | (38.1) | 32 | (47.1) | 66 | (31.7) | 214 | (40.7) | ||
| Medicaid/self pay | 490 | 454 | (61.9) | 36 | (52.9) | 142 | (68.3) | 312 | (59.3) | ||
| Has children | 0.383 | 0.039 | |||||||||
| Child(ren) | 638 | 499 | (63.6) | 139 | (66.8) | 123 | (57.7) | 376 | (65.7) | ||
| No children | 355 | 286 | (36.4) | 69 | (33.2) | 90 | (42.3) | 196 | (34.3) | ||
| IPV severity | 0.211 | <0.001 | |||||||||
| Lethal | 301 | 235 | (29.9) | 66 | (31.7) | 67 | (31.5) | 168 | (29.4) | ||
| High violence | 385 | 315 | (40.1) | 70 | (33.7) | 106 | (49.8) | 209 | (36.5) | ||
| Lower violence | 307 | 235 | (29.9) | 72 | (34.6) | 40 | (18.8) | 195 | (34.1) | ||
| Personal protection order | 0.649 | 0.474 | |||||||||
| Applied for PPO | 168 | 135 | (17.2) | 33 | (15.9) | 40 | (18.8) | 95 | (16.6) | ||
| No PPO | 825 | 650 | (82.8) | 175 | (84.1) | 173 | (81.2) | 477 | (83.4) | ||
| No. of ED visits (4 years) | <0.001 | ||||||||||
| Mean (SD) | ---- | 7.2 | (8.1) | ---- | ---- | 10.6 | (11.7) | 5.5 | (5.7) | ||
| Range | (1–88) | (1–87) | (1–75) | ||||||||
| No. of police calls (4 years) | <0.001 | <0.001 | |||||||||
| Mean (SD) | 3.4 (3.1) | 3.6 (3.1) | 2.7 (3.2) | 4.2 (3.6) | 3.3 (2.8) | ||||||
| Range | (1–31) | (1–26) | (1–31) | (1–26) | (1–18) | ||||||
ED = Emergency department
IPV = Intimate partner violence
Among ED users, women who were ever identified as IPV victims were less likely to have children and more likely to be uninsured or have Medicaid; they also had higher numbers of IPV-related police calls and were more severely abused. IPV-identified ED patients had nearly twice as many ED visits as never-identified patients, mean 10.6 vs. 5.7.
Only ED visits occurring after the first documented IPV assault (n = 4,306) were used for our visit-level analysis. The vast majority (82.3%) occurred more than 30 days after a police call for service. Less than 5% of visits occurred within a day of a police incident; another 4% occurred in the following week, yielding approximately 9% that were temporally related to a police-reported IPV incident. As demonstrated in Table 2, the rate of IPV identification by ED staff was four times greater if the visit occurred within a day of a police incident than at any other point in time. Likewise, when police brought the victims to the ED, the odds that IPV would be noted by ED staff were doubled. However, even in these cases, IPV was rarely listed as the chief complaint.
Table 2.
Characteristics of ED Visits Where IPV Is Identified (N = 4,306)
| Total N | IPV identified at ED visit | ||||
|---|---|---|---|---|---|
| N | Rate | aOR | 95% CI | ||
| Total | 4,306 | 321 | 7.5 | ||
| ED visit relative to police incident | |||||
| ED IPV >1 day BEFORE police call | 72 | 36 | 50.0 | (Ref = NOT ±1 day)† | |
| ED visit ±1 day of police call | 203 | 125 | 61.6 | 12.60** | (7.86–20.20) |
| ED visit 2–7 days AFTER | 181 | 26 | 14.4 | - | |
| ED visit 8–30 days AFTER | 308 | 17 | 5.5 | - | |
| ED visit >30 days AFTER | 3,542 | 117 | 3.3 | - | |
| Brought by police | |||||
| No | 4,237 | 300 | 7.1 | (Reference) | |
| Yes | 69 | 21 | 30.4 | 2.06 | (0.97–4.38) |
| Chief complaints | |||||
| Medical | 3,378 | 116 | 3.4 | (Reference) | |
| MH/SA | 294 | 54 | 18.4 | 0.92 | (0.44–1.93) |
| Injury | 470 | 35 | 7.4 | 0.53 | (0.10–2.67) |
| Assault (including IPV)† † | 164 | 116 | 70.7 | 17.16** | (9.43–31.24) |
| Mental health noted | |||||
| No | 3,621 | 228 | 6.3 | (Reference) | (2.92–11.02) |
| Yes | 683 | 92 | 13.5 | 5.67** | |
| Substance use/abuse noted | |||||
| No | 3,717 | 222 | 6.0 | (Reference) | |
| Yes | 589 | 99 | 16.8 | 1.47 | (0.97–2.23) |
ED = Emergency department
IPV = Intimate partner violence
aOR = Adjusted odds ratio, accounting for clustering of multiple visits
†Comparison is between IPV noted ±1 day of police incident vs. other time periods
††Twenty-one of the 164 assault-related chief complaints were noted to be IPV
*p < 0.05, **p < 0.001
The vast majority (78.4%) of all ED visits were for medical complaints, even for patients presenting within 1 day of an IPV-related police incident. Only 3.8% of ED visits had a chief complaint of assault; in 70% of assault cases, ED staff documented IPV. Chief complaints related to mental health or substance abuse, including “crisis,” “suicidal,” and “overdose,” had a higher rate of IPV identification (18.4%) than chief complaints related to injury (7.4%) or medical concerns (3.4%). Of 321 ED visits where IPV was ever identified, 178 (55.5%) were documented by triage nurses, 159 (49.5%) by treatment nurses, and 259 (80.7%) by physicians. Physicians had higher rates of IPV identification (16.2%) relative to triage (6.2%) and treatment (7.5%) nurses when the chief complaint was mental health or substance abuse.
Of the five categories of actions/interventions listed in the ED policy for IPV-identified visits, ED providers were best at documenting legally useful notes (81.6%), particularly when the chief complaint was an assault (AOR = 5.17, 95% CI = 2.25–11.88, reference = medical complaint), and they communicated with police about 50% of the time. They were less likely to involve a social worker (45%), and documentation of safety assessment/planning and/or referral to victim services was present in only 33% and 25%, respectively. IPV-identified visits occurring within a day of a police incident resulted in more police contact (AOR = 2.26, 95% CI = 1.22–4.20) and safety assessment (AOR = 2.01; 95% CI = 1.08–3.75) compared to those that were not within a day of police incident, but not in referrals to social work or victim services. Visits with both IPV and a mental health chief complaint were less likely to involve police (AOR = 0.19; 95% CI = 0.6–0.55), but more likely to involve the social worker (AOR = 4.25; 95% CI = 1.89–9.56) compared to visits with a medical chief complaint.
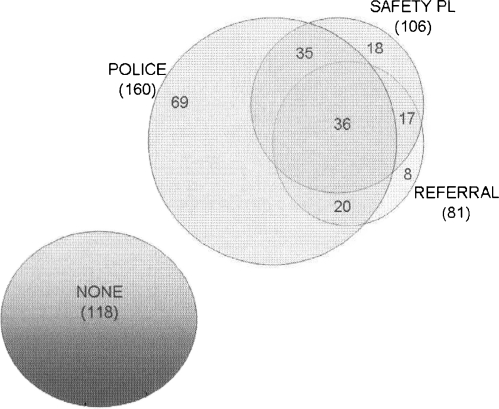
While legally useful documentation and ED social work involvement clearly have value, they did not always translate into interventions for victims. Figure 1 illustrates the clustering of three ED interventions (police contact, safety planning, and referrals to IPV services) that occurred when IPV was identified. For 118 visits (36.8%), there were no documented ED interventions. Contact with police was the step most often taken alone, with no accompanying actions (n = 69). Safety planning and referrals almost always occurred together when an ED social worker was involved. Of 321 visits in which IPV was identified, only 36 included all five responses recommended in the ED policy manual.
Figure 1.
Co-occurrence of ED actions for IPV-identified visits (N = 321).
DISCUSSION
We find the vast majority of police-identified women victims of IPV are using the ED for health care, but providers are missing important opportunities to identify and provide interventions for IPV. Consistent with our hypothesis, victims were rarely identified unless transported by police or voicing a chief complaint of IPV. If identified, only a fraction were referred to a social worker, assessed for safety, or referred to victim services. Only 11% of ED visits in which IPV was identified included all five responses recommended in the ED policy manual.
The US Preventative Service Task Force rates the evidence for IPV screening and identification as inconclusive.14 However, preventative interventions that are rarely or incompletely implemented are unlikely to be found effective. The MacMillan study21 was important because it demonstrated the safety of IPV screening, but it is important to note that their screening intervention group did not receive any intervention beyond a referral, and the control group was also screened and referred only at the end of the visit as opposed to the beginning. This likely negated any ability to detect a difference but does not mean that screening and referral were ineffective since, unlike our results, IPV-identified women in both groups exhibited long-term reductions in IPV recurrence.21 MacMillan et al. are to be commended for overcoming the challenges inherent in conducting a randomized clinical trial with abused women, but, for ethical reasons, their study was not able to duplicate actual “treatment as usual,” which is likely to be similar to that found in our study.
There are good reasons to think that IPV indentified in an ED setting may be of higher risk. Using police records, we were able to determine that the level of both overall and subsequent police-reported IPV was higher among those who were identified compared to those never identified in the ED. These results are consistent with those of others who have found IPV identification in the ED to be a predictor of future IPV.24
Beyond the group that arrived with a police escort or self-identified with IPV assault, most IPV identification in our study appeared to be case finding by the physician, which occurred more often in patients with mental health and/or substance abuse complaints. However, the overall low rates of IPV identification create the imperative for developing more systematic methods of both identification and response. Knowing that 15–20% of female patients are positive for past year abuse,6,12 the assumption should be that all patients can benefit from an opportunity to disclose IPV, and, regardless of disclosure, the health care system should function as a safety net, providing information about community-based interventions for family violence to all patients.
While identification is necessary, it is not sufficient for addressing IPV.25 In this study, less than a third of women identified as IPV victims received any documented counseling or referral. Previous work has found that less than half of women whose positive IPV screen was given to the provider discussed the issue during their visit,21,26 indicating that the lack of efficacy found in screening studies may be attributable to the lack of an effective intervention accompanying the screening.
The accumulated literature on health care response to IPV establishes that health care providers are an important but somewhat weak link in the process. Therefore, if we wish to get results that are different than those presented here, we need to abandon the strategy of relying on busy health care providers for both IPV screening and interventions. Given that victims of IPV will continue to use health care settings, and the overwhelming evidence indicates that routine screening does detect abuse, future IPV research needs to focus on developing and testing effective system-level responses to screening and intervention. Patient portals as part of electronic medical records provide an excellent opportunity to implement a population-based public health approach to IPV identification. Once IPV is identified, providers should be kept informed as women trust and want their health care providers to be involved;27 however, the providers’ role should be additive and supportive of a system-level process that reliably links to social work and trauma-informed interventions. Evidence of effectiveness could include an assessment of the various forms of counseling and referral provided in health care settings that have been shown to be effective for other behavioral conditions.28–30 It has been established that the way services are organized and provided can have a large impact on whether or not they are used. For example, on-site interventions for mental health and substance abuse provided during health care visits are associated with less stigma and higher rates of engagement than off-site referrals.31,32
IPV research has also suffered from a lack of validated outcomes with which to determine the effectiveness of an intervention. Our study points to the potential of using criminal justice records to track police-reported IPV and eliminate the problem of victims being lost to follow-up. Integrated databases among health, criminal justice, and social service agencies can be a source for tracking adverse outcomes and identifying uptake of services. With patients’ permission, interagency communication about IPV injury could help build a prosecutor’s case and document assaults or threats designed to interfere with witnesses’ testifying. Immediately feasible is the possibility of expanding social work interventions during the health care visit. Brief motivational interventions at the time of visit have been shown to improve health behaviors and decrease rates of injury;33–35 they may be applicable to IPV.36
LIMITATIONS
As a retrospective study in one Midwestern county, results may not be generalizable to other venues. Like all studies that rely on records generated for administrative purposes, data are limited by what is documented and fail to capture undocumented events. Therefore, IPV that did not rise to the level of a police report did not make it into our study. Our linking strategy included both electronic and manual methods with rigorous validation; however, women’s names and addresses may change over time, and patients sometimes deliberately give wrong names or dates of birth, so it is possible we missed some ED visits. Finally, our data encompass the period from 1999–2002, selected because we could leverage data collected during a CDC-funded ED IPV surveillance effort. During that time period, local EDs and criminal justice providers had extensive resources for IPV training. Since then, similar to national trends, there have been dramatic increases in ED volumes, and there have not been any new IPV interventions, so the this study may represent a best case scenario.
CONCLUSION
We find that the vast majority of police-identified female IPV victims are using the ED for health care, but they are unlikely to be identified or receive intervention for IPV in the ED setting. Results add to a body of literature indicating that current screening practices are ineffective, and policy-driven interventions for identified victims of violence are, at best, erratically implemented. Because the majority of victims do not present for assault or injury, case finding is unlikely to be effective for identifying patients in need of intervention. New system-level strategies are needed to ensure routine opportunities for patient self-disclosure, access to needed resources, and the ability to track outcomes. Only then will we be able to develop and evaluate interventions for IPV in health care settings.
Acknowledgments
The authors wish to thank Patricia Smith, Director, Violence Against Women Prevention Program, Michigan Department of Community Health; the Kalamazoo County Prosecutor’s Office, all members of the Community Advisory Board, the YWCA Domestic Violence Program, and the many research assistants who worked on this project. This project builds on data collected for the MEDCIIN Projects under the CDC cooperative agreement U17/CCU551067.
Conflict of Interest None disclosed.
Research support was primarily provided by a grant from the National Institute of Justice: NIJ 2006-WG-BX-0007; additional support for investigator time was provided by NIMH K23 MH64572 (Rhodes) and K01MH75965-01 (Cerulli) and the Center for Health Equity Research and Promotion, Philadelphia VA Medical Center (Dichter). Opinions or points of view expressed are those of the author(s) and do not necessarily reflect the official position or policies of the U.S. Department of Justice the Department of Veterans Affairs or the United States Government.
References
- 1.Cascardi M, Langhinrichsen J, Vivian D. Marital aggression: Impact, injury, and health correlates for husbands and wives. Arch Intern Med. 1992;152:1178–1184. doi: 10.1001/archinte.152.6.1178. [DOI] [PubMed] [Google Scholar]
- 2.Vivian D, Langhinrichsen-Rohling J. Are bi-directionally violent couples mutually victimized?: A gender-sensitive comparison. Violence Vict. 1994;9:107–124. [PubMed] [Google Scholar]
- 3.Bachman R, Salzman, LE. Violence against women: Estimates from the redesigned study. Washington, DC: US Department of Justice, Bureau of Justice Statistics; 1995. BJS Publication No. 154–348.
- 4.Sutherland C, Bybee D, Sullivan C. The long-term effects of battering on women's health. Women’s Health. 1998;4:41–70. [PubMed] [Google Scholar]
- 5.Catalano SM. Criminal Victimization, 2004. Data from the National Crime Victimization Survey. Washington, DC: Bureau of Justice Statistics, Office of Justice Programs, US Department of Justice; 2005.
- 6.Tjaden P, Thoennes N. Prevalence, incidence, and consequences of violence against women: Findings from the National Violence Against Women Survey. Washington, DC: National Institute of Justice and Centers for Disease Control and Prevention; 1998. [Google Scholar]
- 7.Stein M, Kennedy C. Major depressive and post-traumatic stress disorder comorbidity in female victims of intimate partner violence. J Affect Disorders. 2001;66:133–138. doi: 10.1016/S0165-0327(00)00301-3. [DOI] [PubMed] [Google Scholar]
- 8.Campbell J. Health consequences of intimate partner violence. Lancet. 2002;359:1331–1336. doi: 10.1016/S0140-6736(02)08336-8. [DOI] [PubMed] [Google Scholar]
- 9.Coid J, Petruckevitch A, Chung W, Richardson J, Morrey S, Feder G. Abusive experiences and psychiatric morbidity in women primary care attenders. Brit J Psychiat. 2003;183:332–339. doi: 10.1192/bjp.183.4.332. [DOI] [PubMed] [Google Scholar]
- 10.Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) study. Am J Prev Med. 1998;14:245–258. doi: 10.1016/S0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 11.Coker A, Davis KE, Arias I, et al. Physical and mental health effects of intimate partner violence for men and women. Am J Prev Med. 2002;23:260–268. doi: 10.1016/S0749-3797(02)00514-7. [DOI] [PubMed] [Google Scholar]
- 12.Abbott J, Johnson R, Koziol-McLain J, Lowenstein SR. Domestic violence against women: Incidence and prevalence in an emergency department population. JAMA. 1995;273:1763–1767. doi: 10.1001/jama.273.22.1763. [DOI] [PubMed] [Google Scholar]
- 13.McCloskey LA, Lichter E, Ganz ML, et al. Intimate partner violence and patient screening across medical specialties. Acad Emerg Med. 2005;12:712–722. doi: 10.1111/j.1553-2712.2005.tb00938.x. [DOI] [PubMed] [Google Scholar]
- 14.Neilson HD, Nygren P, McInerney Y, Klein J. Screening women and elderly adults for family and intimate partner violence: A review of the evidence for the US Preventive Services Task Force. Ann Intern Med. 2004;140:387–396. doi: 10.7326/0003-4819-140-5-200403020-00015. [DOI] [PubMed] [Google Scholar]
- 15.American College of Obstetricians and Gynecologists. ACOG issues technical bulletin on domestic violence. http://www.acog.org/departments/dept_notice.cfm?recno=17&bulletin=585, accessed, 2-7-11 [PubMed]
- 16.Violence position paper: American Academy of Family Physicians Website. http://www.aafp.org/online/en/home/policy/policies/v/violencepositionpaper.html accessed, 2-7-11
- 17.American Association of Pediatrics Website http://aappolicy.aappublications.org/misc/Identifying_and_Responding_to_Domestic_Violence.dtl., accessed 2-7-11
- 18.The Joint Commission Accreditation Program: Hospital: Provision of care, treatment, and services, 2008. Joint Commission Website. http://www.jointcommission.org/AccreditationPrograms/Hospitals/. Accessed September 23, 2008.
- 19.MacMillan HL, Wathen CN with the Canadian Task Force on Preventive Health Care. Prevention and Treatment of Violence Against Women. In: Systematic Review & Recommendations. London, Ontario: Canadian Task Force; 2001. CTFPHC Technical Report No. 01–4.
- 20.United States Preventive Services Task Force (USPSTF) Screening and behavioral counseling interventions in primary care to reduce alcohol misuse: Recommendation statement. Ann Intern Med. 2004;140:554–556. doi: 10.7326/0003-4819-140-7-200404060-00016. [DOI] [PubMed] [Google Scholar]
- 21.MacMillan HL, Wathen CN, Jamieson E, et al. Screening for intimate partner violence in health care settings: A randomized trial. JAMA. 2009;302:493–501. doi: 10.1001/jama.2009.1089. [DOI] [PubMed] [Google Scholar]
- 22.Kothari C, Rhodes KV. Missed opportunities: Emergency department visits by police-identified victims of intimate partner violence. Ann Emerg Med. 2006;47:190–199. doi: 10.1016/j.annemergmed.2005.10.016. [DOI] [PubMed] [Google Scholar]
- 23.Rhodes KV, Frankel R, Levinthal N, Prenoveau E, Bailey J, Levinson W. “You’re not a victim of domestic violence, are you?”. Ann Intern Med. 2007;147:620–627. doi: 10.7326/0003-4819-147-9-200711060-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Houry D, Feldhaus K, Peery B, et al. A positive domestic violence screen predicts future domestic violence. J Interper Violence. 2004;19:955–66. doi: 10.1177/0886260504267999. [DOI] [PubMed] [Google Scholar]
- 25.Moracco KE, Cole TB. Preventing intimate partner violence: Screening is not enough. JAMA. 2009;302:568–570. doi: 10.1001/jama.2009.1135. [DOI] [PubMed] [Google Scholar]
- 26.Rhodes KV, Drum M, Anliker EA, Frankel R, Howes DS, Levinson W. Lowering the threshold for discussions of domestic violence: A randomized controlled trial of computer screening. Arch Intern Med. 2006;165:1–8. doi: 10.1001/archinte.166.10.1107. [DOI] [PubMed] [Google Scholar]
- 27.Gerbert B, Abercrombie P, Caspers N, Love C, Bronstone A. How health care providers help battered women: The survivor’s perspective. Women Health. 1999;29:115–135. doi: 10.1300/J013v29n03_08. [DOI] [PubMed] [Google Scholar]
- 28.Bien TH, Miller WR, Tonigan JS. Brief interventions for alcohol problems: A review. Addiction. 1993;88:315–335. doi: 10.1111/j.1360-0443.1993.tb00820.x. [DOI] [PubMed] [Google Scholar]
- 29.World Health Organization Brief Intervention Study Group (WHOBISG) Cross-national trial of brief interventions with heavy drinkers. Am J Public Health. 1996;86:948–955. doi: 10.2105/AJPH.86.7.948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Glasgow RE, Whitlock EP, Eakin EG, Lichtenstein E. A brief smoking cessation intervention for women in low-income Planned Parenthood clinics. Am J Public Health. 2000;90:786–789. doi: 10.2105/AJPH.90.5.786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ogle RL, Baer JS. Addressing the service linkage problem: Increasing substance abuse treatment engagement using personalized feedback interventions in heavy-using female domestic violence shelter residents. J Interpers Violence. 2003;18:1311–1324. doi: 10.1177/0886260503256659. [DOI] [PubMed] [Google Scholar]
- 32.Oxman TE, Dietrich AJ, Schulberg HC. The depression care manager and mental health specialist as collaborators within primary care. Am J Geriat Psychiat. 2003;11:507–516. [PubMed] [Google Scholar]
- 33.Gentilello LM, Ebel BE, Wickizer TM, Salkever DS, Rivara FP. Alcohol interventions for trauma patients treated in emergency departments and hospitals: A cost benefit analysis. Ann Surg. 2005;241:541–550. doi: 10.1097/01.sla.0000157133.80396.1c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hingson RW, Swahn MH, Sleet DA. Interventions to prevent alcohol-related injuries. In Doll L, Bonzo S, Sleet D, Mercy J, Haas E, eds. Handbook of Injury and Violence Prevention. Springer; 2006.
- 35.Nilsen P, Baird J, Mello MJ. A systematic review of emergency care brief alcohol interventions for injury patients. J Subst Abuse Treat. 2008;35:184–201. doi: 10.1016/j.jsat.2007.09.008. [DOI] [PubMed] [Google Scholar]
- 36.Burke P, Chapman C, Hohman M, et al. Guiding as practice: Motivational interviewing and trauma-informed work with survivors of intimate partner violence. Partner Abuse. 2010;1:92–104. [Google Scholar]