Abstract
Objectives
To describe the characteristics of hospitalizations for patients who utilize clinical programs that provide care coordination for children with multiple, chronic medical conditions.
Study design
Retrospective analysis of 1,083 patients hospitalized between June 2006 and July 2008 who utilize a structured, pediatric complex-care clinical program within four children's hospitals. Chronic diagnosis prevalence (technology assistance, neurologic impairment and other complex chronic conditions), inpatient resource utilization (length of stay, 30-day readmission), and reasons for hospitalization were assessed across the programs.
Results
Over the two year period, complex-care program patients experienced a mean 3.1 (SD 2.8) admissions, 12.2 days (SD 25.5) in the hospital per admission, and a 25.4% thirty-day hospital readmission rate. Neurologic impairment (57%) and presence of a gastrostomy tube (56%) were the most common clinical characteristics of program patients. Notable reasons for admission included major surgery (47.1%), medical technology malfunction (9.0%), seizure (6.4%), aspiration pneumonia (3.9%), vomiting / feeding difficulties (3.4%), and asthma (1.8%).
Conclusions
Hospitalized patients who utilized a structured clinical program for children with medical complexity experienced lengthy hospitalizations with high early readmission rates. Reducing hospital readmission may be one potential strategy to lower inpatient expenditures in this group of children with high resource utilization.
Keywords: children with medical complexity, hospitalization, children's hospital, neurologic impairment, technology dependence, children with special health care needs
An estimated 13–18% of children and youth in the United States have a chronic health condition that requires health services beyond that needed by healthy children.(1, 2) A growing subset of these children have a complicated, fragile chronic disease or multiple chronic medical problems that lead clinicians to consider them medically complex.(3, 4) This emerging population of children with medical complexity is perceived to require high intensity, coordinated care from primary, community and multiple-specialty providers.(5)
The health care needs of children with medical complexity may extend beyond the capacity of some pediatric practices to coordinate care for them from a medical home.(6) This may be especially true for children who do not have a unifying diagnosis that matches with an existing specialty clinical program (e.g., a multi-disciplinary outpatient clinic for patients with spina bifida) designed to promote care coordination among different providers within one setting.(7) Such children are at particularly high risk for fragmented, uncoordinated care that contributes to unfavorable health outcomes.(7–11)
New outpatient and inpatient complex-care clinical programs are emerging to meet the needs and improve the health outcomes of children with medical complexity who do not receive coordinated care in the existing healthcare system.(3, 6, 12–15) The scope of diseases and chronic medical conditions encountered by children utilizing these programs remain poorly described. Although the majority of their healthcare expenditures are believed to occur in the inpatient setting, there is limited information describing patterns and indications for hospitalization.(4) The objectives of the work were to: 1) describe the demographic and clinical characteristics of patients who receive care within different structured outpatient and inpatient complex-care clinical programs for children with medical complexity; and, 2) describe their indications for and use of inpatient resources.
Methods
This is an IRB-approved retrospective cohort analysis of hospitalizations experienced by patients with a history of utilizing a structured complex-care clinical program for children with medical complexity within one of four freestanding children's hospitals (Table I). These programs were chosen as a convenience sample for evaluation based on their participation in a quality improvement forum for children with medical complexity in April 2008.(14) Although these programs are situated in geographically diverse sections of the country, they are not intended to be representative of all complex-care clinical programs for children with medical complexity.
Table 1.
Characteristics of Structured Clinical Programs for Children with Medical Complexity
| Characteristic | Structured Clinical Program | ||||
|---|---|---|---|---|---|
| Medically Complex Service, Children's Memorial Hospital, Chicago | Medical Home Program for Special Needs Children, Arkansas Children's Hospital | Complex Care Service, Children's Hospital Boston | Rainbow Initiative, Children's Hospital Boston | Special Needs Program, Children's Hospital, Wisconsin | |
| Service Model | Inpatient: Dedicated Service |
Outpatient: Consultative |
Outpatient: Consultative Inpatient: Dedicated Service |
Outpatient: Primary Care |
Outpatient: Consultative Inpatient: Consultative and Dedicated Service |
| Patient Characteristics Considered during Selection for Program Enrollment |
|
|
|
|
|
| Clinician Types | Pediatric hospitalists, social worker, case manager | Neonatologists, Developmental / general pediatricians, nurse care coordinators, social workers, psychologists, speech therapists | Developmental / general pediatricians, social worker, nurse care coordinators | General pediatricians, social worker, nurse care coordinator | General pediatricians, Intensivists, nurse care coordinators |
| Number of Patients Enrolled in the Service | 234 | 345 | 832 | 500 | 403 |
| % of children with one or more hospitalizations during the study period | 71.8% | 73.0% | 84.9% | 37.8% | 59.3% |
The characteristics of each program are described in Table I. The programs developed independently, but all share the common goal of optimizing the health of children with medical complexity and minimizing their inpatient resource utilization through care coordination among a child's hospital, outpatient and community providers. Rainbow-Boston is the only program that provides primary care for their patients; this characteristic distinguishes the Rainbow-Boston program from the Complex Care Service-Boston program. All programs describe multiple chronic illnesses or involvement with multiple pediatric specialists as patient characteristics that are typically associated with program enrollment. Only one service (Complex Care Service – Boston) describes neurodevelopmental disability as a highlighted characteristic for selection. Patients are referred to the programs by local primary, specialty and hospital providers. The Arkansas and Milwaukee programs are unique in that they receive many referrals directly from their hospital's neonatal and medical intensive care units, respectively. Rainbow-Boston accepted healthy siblings of complex patients, but they are not included in this study.
Hospitalization data for program patients were obtained from the Pediatric Health Information System (PHIS), an administrative database of inpatient admissions for children within freestanding children's hospitals.(16) All hospitals are affiliated with the Child Health Corporation of America (CHCA, Shawnee Mission, KS), a business alliance of 42 children's hospitals. Data quality and reliability are maintained through a joint effort between CHCA and Thompson Healthcare (New York, NY). Program patients were linked with PHIS hospitalization data using their medical record number and PHIS unique identifier.
Study inclusion criteria were children with medical complexities who experienced (1) at least one health encounter with a structured complex-care clinical program during their life; and (2) one or more hospitalizations between July 2006 and June 2008. For each patient, all hospitalizations within the study period, affiliated with any medical or surgical service, were included for analysis.
Demographic characteristics analyzed across complex-care clinical program patients were age, sex, race/ethnicity (Caucasian non-Hispanic, black, Hispanic, other), and insurance type (public, private, self-pay) as available within PHIS.(16)
Diagnosis characteristics abstracted were the number of diagnoses encountered by each child during a hospitalization and the name of each diagnosis. PHIS contains up to 21 individual International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis codes for each hospitalization. We categorized individual diagnosis codes into three clinical categories based on previous studies: Feudtner et al (2000)'s Complex Chronic Conditions, neurologic impairment and technology assistance.(5, 17–19)
Neurologic impairment and technology-assistance were chosen as proxies of functional impairment and because of their presence within the patient selection characteristics of two of the five programs.(20, 21) Neurologic impairment (NI) was defined as static and progressive, central and/or peripheral neurologic diagnoses associated with chronic functional and or/intellectual impairment.(22–24) The NI category was an extension of Feudtner's neuromuscular diagnoses described above. Example diagnoses included encephalopathy and peripheral nervous system disorders. Technology assistance was defined as a medical device used to maintain a child's health status.(25, 26) Examples of technologies included gastrostomy, tracheostomy, cerebrospinal fluid ventricular shunt, and permanent indwelling catheter.5, 19–21
Hospitalization characteristics included the number of hospitalizations (and intensive care hospitalizations), length of stay per hospitalization, readmission within 30 days of a previous admission, and total charges per hospitalization. We also analyzed the principal diagnosis and procedure ICD-9-CM code for each admission as an indicator of the primary reason for admission.
Statistical Analysis
We compared nominal patient characteristics (race/ethnicity, insurance type, sex, and diagnosis clinical categories) among each service using chi-square tests. We compared continuous characteristics (age, number of diagnoses) using wilcoxon rank sum and t-tests based on normality. Statistical Analysis Software (SAS Institute, Inc, Cary, NC) version 9.1.3 was used for all analyses.
Results
There were 1,083 children with a history of a pediatric complex-care clinical program. These patients accounted for 1.7% of all patients hospitalized, 3.8% (n = 3,365) of the total number of hospitalizations and 5.5% ($12.6 million) of the total aggregate hospital charges for all children admitted to the hospital during the two year study period. The median age for all complex-care clinical program patients at the beginning of the study period was 3.2 years [interquartile range (IQR) 1.1, 10.0)]. Arkansas had the youngest patients [median 0.8 years (IQR 0.2, 1.9)] and Boston – Complex Care had the oldest patients [median 5.3 (IQR 1.7, 14.4)], p<.01. 49% of all complex-care patients utilized public health insurance.
The mean number of diagnoses per admission for all complex-care program patients was 9.5 (SD 5.4). 91% of all patients had one or more diagnoses within the diagnosis categories of interest (complex chronic conditions, neurologic impairment, or medical technology assistance) compared with 35% of hospitalized patients who were not affiliated with a complex-care clinical program. 83% of all hospitalized complex-care clinical program patients had one or more of complex chronic conditions, and 41% had two or more complex chronic conditions. The most frequent conditions were neuromuscular (51.4%), cardiac (28.3%), and congenital/genetic defect (25.3%) (Table II).
Table 2.
Diagnosis Characteristics of Patients Enrolled in a Structured Clinical Program for Children with Medical Complexity
| Characteristic | All Complex Care Patients Combined | Structured Clinical Program | ||||
|---|---|---|---|---|---|---|
| Chicago, IL | Little Rock, AR | Boston - CCS | Boston -Rainbow | Milwaukee, WI | ||
| Number of Diagnoses | ||||||
| Mean (SD) no. of diagnoses | 9.5 (5.4) | 9.2 (4.4) | 6.6 (4.9) | 10.5 (4.8) | 7.3 (4.7) | 12.0 (5.6) |
| Diagnosis Categories | ||||||
| Patients with a diagnosis within one or more of the 3 diagnosis categories (%) | 91% | 91% | 93% | 96% | 78% | 96% |
| Complex Chronic Conditions (%) | 83% | 82% | 79% | 93% | 38% | 88% |
| Neurological Impairment (%) | 57% | 70% | 33% | 83% | 71% | 63% |
| Technology Assistance (%) | 69% | 69% | 64% | 79% | 47% | 79% |
57% of all hospitalized complex-care clinical program patients had neurologic impairment. Arkansas had the lowest prevalence of neurologic impairment (33.1%) (Table II). The most frequent neurologic impairment diagnoses were seizures/epilepsy (32.7%), cerebral palsy (23.8%), and brain/spinal cord anomaly (11.3%). 69% of all complex-care clinical program patients had technology assistance. Gastrostomy tube (55.9%), cerebrospinal fluid shunt (13.2%), and tracheostomy tube (12.0%) were the most frequent technologies utilized by complex-care clinical program patients.
Inpatient Resource Utilization
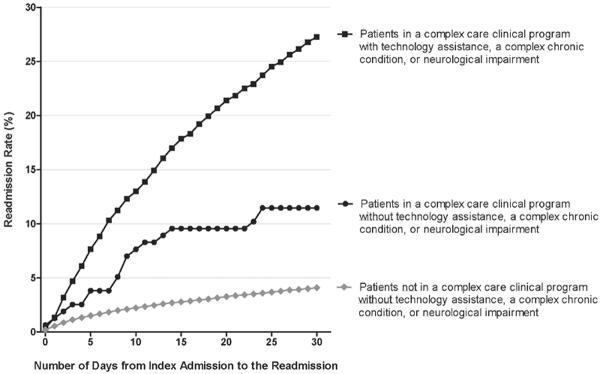
During the two year study period, complex-care clinical program patients experienced a mean of 3.1 (standard deviation [SD] 2.8) admissions, 12.2 days (SD 25.5) in the hospital for each admission, and a 25.4% readmission rate within 30 days of a prior hospitalization (Table III). Complex-care clinical program patients with technology assistance, neurologic impairment or other complex chronic conditions experienced the highest 30-day readmission rates, compared with program patients without these clinical characteristics and non-program patients without these clinical characteristics (Figure).
Table 3.
Inpatient Health Services of Patients Enrolled in a Structured Clinical Program for Children with Medical Complexity Who Were Hospitalized Between 2006 and 2008.
| Health Services (Accrued Over the 2 Year Period) | All Complex Care Patients Combined | Structured Clinical Program | ||||
|---|---|---|---|---|---|---|
| Chicago, IL | Little Rock, AR | Boston - CCS | Boston - Rainbow | Milwaukee, WI | ||
| Mean number of hospitalizations per patient (standard deviation) | 3.1 (2.8) | 2.7 (2.3) | 2.6 (2.4) | 3.7 (3.1) | 2.7 (2.5) | 3.7 (3.4) |
| Mean length of stay per hospitalization (standard deviation) | 12.2 (25.5) | 12.9 (23.6) | 23.1 (39.4) | 8.8 (16.1) | 8.5 (21.3) | 8.8 (20.2) |
| Mean total number of hospital days for all admissions (standard deviation) | 24.2 (39.5) | 23.1 (33.2) | 41.9 (53.3) | 18.9 (29.8) | 15.4 (32.5) | 19.9 (36.1) |
| % Readmission within 30 days | 25.4% | 15.0% | 27.5% | 32.0% | 24.0% | 28.8% |
| % Admissions associated with intensive care unit services | 13.2% | 19.6% | 13.1% | 11.0% | 16.0% | 10.4% |
Figure.
Cumulative readmission rates occurring for each day following an index admission up to 30 days after discharge. Readmission rates are presented for three mutually-exclusive groups: a) patient enrolled in a structured clinical program with technology assistance, a complex chronic condition or neurologic impairment, b) patients enrolled in a program who do not have these characteristics, and c) for a baseline reference, patients not enrolled in a program who do not have these characteristics.
Principal Procedures
Almost half (47.1%) of all complex-care clinical program patient admissions were –related primarily to a surgical operation or major procedure. Operations and procedures related to gastroenterologic and nutritional needs (18.5%) were the most common, followed by airway and respiratory (16.6%) and nervous system (7.6%). Continuous mechanical ventilation and positive airway pressure (7.9%), gastrostomy insertion and replacement (5.2%) and electroencephalographic monitoring (3.7%) were the most commonly observed individual operations and procedures.
Principal Diagnoses
Respiratory tract problems were the most common reason (29.0%) for hospitalization among all complex-care clinical program patients. The most common primarily diagnoses were pneumonia and bronchiolitis (9.4%), respiratory insufficiency unspecified (5.6%), pneumonitis due to inhalation of food or vomitus (3.9%) and asthma (1.8%). Gastroenterologic and nutritional problems were the second most common reason (15.8%) for hospitalization. The most common principal diagnoses associated with admissions for gastroenterologic and nutritional reasons were vomiting and feeding difficulties (3.4%), dehydration (3.1%), and failure to thrive (2.2%).
Malfunction, complication, or infection related to medical technology was the third most common medical reason for hospitalization among all complex-care patients (9.0%). The most common principal diagnoses associated with these problems were related to nervous system devices (2.5%) including cerebrospinal fluid shunts; gastroenterologic technology (2.5%) including gastrostomy, ileostomy, colostomy, other enterostomy tubes and stoma; vascular devices including central venous catheters (2.3%); and tracheostomy (1.6%).
Discussion
Hospitalized patients who utilized a complex-care clinical program for children with medical complexity in this study experienced multiple, lengthy hospitalizations. These findings were similar across disparate settings, patient enrollment characteristics and referral patterns of the complex-care clinical programs. However, these programs shared a common purpose – to reduce unnecessary inpatient resource utilization. The reasons for hospitalization in our study suggest that some hospitalizations may be avoidable with improved delivery of care. Reducing early hospital readmissions, in particular, may be one potential strategy to lower inpatient expenditures in this group of children with high resource utlization.
Recent studies have focused on children with medical complexity and described methods of identification, inpatient resource utilization, and the management of some of their specific conditions.(5, 27–29) Our study adds an inpatient resource perspective of children with medical complexity who are cared for in complex-care clinical programs. It is concerning that readmission is occurring so frequently among these children in our study across programs despite exposure to clinical services charged to provide coordination of high quality care. Early hospital readmission is emerging as an indicator of substandard quality of care and potential source of cost-savings if avoided.(30, 31) The high 30-day readmission rate (25%) observed in the present study exceeds the 30-day readmission rate reported in adults with chronic illness (19%).(32)
There is a critical need to understand the patient and health system factors that influence inpatient resource utilization, such as readmission, for these children and determine which factors are ameliorable with improved delivery of care. Improved communication among providers during transition from hospital to home and clear provider roles and responsibilities for care plan continuation following hospital discharge may help prevent the need to return back to the hospital.(33) This may be particularly evident with hospitalizations associated with uncontrolled illness, such as asthma and seizures, that may be sensitive to prevention with high quality ambulatory care and proactive care planning.(34, 35) Additionally, we observed high readmission rates in children with technology assistance; nearly one out of every ten admissions among program patients was associated with technology malfunction. Early readmission for technology malfunction, such as ventricular shunt failure, may be avoidable with the implementation of high quality operative and procedural techniques.(36)
Despite these efforts, there will be unavoidable admissions among complex-care program patients and we should strive to optimize inpatient care efficiency without compromising safety. We observed length of stay variability among the programs in this study, suggesting that there may be different local practice patterns that impact length of stay with potential opportunities for improvement of care efficiency. For example, respiratory problems accounted for nearly 1/3 of admissions among these children. There is limited evidence to guide inpatient physicians on how to best manage respiratory problems in children with neurologic impairment, the most common clinical population among complex-care program patients.(21) Moreover, pediatric physicians and trainees report deficiencies caring for children with neurologic impairment and negative provider attitudes toward this population are associated with substandard practices of care.(37–39) Identifying best practices for inpatient respiratory illness management among children with neurologic impairment while improving providers' attitudes and care skills toward these children may help standardize high quality of care delivery across hospitals.
Our study has the following limitations. The programs evaluated in this study have heterogeneous settings, clinician training backgrounds, and patient selection criteria. Local referral patterns influenced the variability of patient attributes and inpatient resource utilization among the programs. For example, the Arkansas outpatient program uniquely received patient referrals from the neonatal intensive care unit. This may help explain their patients' longer length of stay, which included the neonatal admission; and younger age. Arkansas program patients had the lowest prevalence of neurologic impairment, which may have been related to clinicians waiting until the patients are older to assign a neurologic impairment diagnosis (e.g., cerebral palsy).
There are hospitalized children with complex medical needs and complex medical diagnoses who are not captured by the clinical programs in this study. The study findings are therefore not intended to generalize to all clinical programs that provide care for children with medical complexity or to the population of children with medical complexity at large. Clinical data, such as degree of uncontrolled chronic illness and medical fragility, were not attainable from the dataset. We did not analyze hospital utilization by timing of complex-care program enrollment. Further analysis is needed to determine if hospital utilization decreases with prolonged exposure to care coordination within a program.
Administrators who are developing a dedicated inpatient or outpatient clinical program for children with medical complexity may consider recruiting clinicians and staff with the clinical competency to care for children with neurologic impairment, the most common underlying chronic condition observed among the programs in this study. Existing complex-care clinical program clinicians and their hospitals may consider tracking hospitalization and early readmission rates for illnesses experienced by children with medical complexity that may be sensitive to mitigation by high quality ambulatory or surgical care, as well as coordination of care. Future studies should evaluate the impact of complex-care program enrollment and specific care delivery attributes on hospitalization and readmission reduction of these illnesses, among other important outcomes for this patient population.
Acknowledgments
Supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development career development awards (K23 HD052553 and HD058092 to R.S and J.B., respectively). The funder was not involved in the design and conduct of the study, in the collection, analysis, and interpretation of the data, and in the preparation, review, or approval of the manuscript.
Abbreviations
- (CYSHCN)
children and youth with special health care needs
- (CCC)
complex chronic conditions
- (CI)
confidence interval
- (ICD-9-CM)
International Classification of Diseases, Ninth Revision, Clinical Modification
- (IQR)
interquartile range
- (NI)
neurologic impairment
- (SD)
standard deviation
- (TA)
technology-assistance
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors declare no conflicts of interest.
References
- 1.Newacheck PW, Strickland B, Shonkoff JP, Perrin JM, McPherson M, McManus M, et al. An epidemiologic profile of children with special health care needs. Pediatrics. 1998;102(1 Pt 1):117–23. doi: 10.1542/peds.102.1.117. [DOI] [PubMed] [Google Scholar]
- 2.van Dyck PC, Kogan MD, McPherson MG, Weissman GR, Newacheck PW. Prevalence and characteristics of children with special health care needs. Arch Pediatr Adolesc Med. 2004;158:884–90. doi: 10.1001/archpedi.158.9.884. [DOI] [PubMed] [Google Scholar]
- 3.Gordon JB, Colby HH, Bartelt T, Jablonski D, Krauthoefer ML, Havens P. A tertiary care-primary care partnership model for medically complex and fragile children and youth with special health care needs. Arch Pediatr Adolesc Med. 2007;161:937–44. doi: 10.1001/archpedi.161.10.937. [DOI] [PubMed] [Google Scholar]
- 4.Neff JM, Sharp VL, Popalisky J, Fitzgibbon T. Using medical billing data to evaluate chronically ill children over time. J Ambul Care Manage. 2006;29:283–90. doi: 10.1097/00004479-200610000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Cohen A, Kuo D, Agrawal R, Berry J, Simon T, Bhagat S, et al. Children with Medical Complexity: An Emerging Population for Clinical and Research Activities. Pediatrics. 2010 doi: 10.1542/peds.2010-0910. Accepted for publication December 2010, in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kelly A, Golnik A, Cady R. A medical home center: specializing in the care of children with special health care needs of high intensity. Matern Child Health J. 2008;12:633–40. doi: 10.1007/s10995-007-0271-7. [DOI] [PubMed] [Google Scholar]
- 7.Stone BL, Murphy NA, Mundorff MB, Parker HB, Peterson PR, Srivastava R. Children with chronic complex medical illnesses: Is inpatient care family-centered? J Pediatr Rehabil Med. 2008;1:237–43. [PMC free article] [PubMed] [Google Scholar]
- 8.Gupta VB, O'Connor KG, Quezada-Gomez C. Care coordination services in pediatric practices. Pediatrics. 2004;113:1517–21. [PubMed] [Google Scholar]
- 9.Slonim AD, LaFleur BJ, Ahmed W, Joseph JG. Hospital-reported medical errors in children. Pediatrics. 2003;111:617–21. doi: 10.1542/peds.111.3.617. [DOI] [PubMed] [Google Scholar]
- 10.Newacheck PW, Hughes DC, Hung YY, Wong S, Stoddard JJ. The unmet health needs of America's children. Pediatrics. 2000;105:989–97. [PubMed] [Google Scholar]
- 11.Pless IB, Satterwhite B, Van Vechten D. Division, duplication and neglect: patterns of care for children with chronic disorders. Child Care Health Dev. 1978;4:9–19. doi: 10.1111/j.1365-2214.1978.tb00067.x. [DOI] [PubMed] [Google Scholar]
- 12.Cohen E, Friedman J, Nicholas DB, Adams S, Rosenbaum P. A home for medically complex children: the role of hospital programs. J Healthc Qual. 2008;30:7–15. doi: 10.1111/j.1945-1474.2008.tb01137.x. [DOI] [PubMed] [Google Scholar]
- 13.Kelly AM, Kratz B, Bielski M, Rinehart PM. Implementing transitions for youth with complex chronic conditions using the medical home model. Pediatrics. 2002;110:1322–7. [PubMed] [Google Scholar]
- 14.Agrawal R, Ballantine A, Srivastava R, Berry JG. Collaborative Developments in Complex Care. Hospital Pediatrics: American Academy of Pediatrics. 2008;1:18–9. [Google Scholar]
- 15.Berman S, Rannie M, Moore L, Elias E, Dryer LJ, Jones MD., Jr. Utilization and costs for children who have special health care needs and are enrolled in a hospital-based comprehensive primary care clinic. Pediatrics. 2005;115:e637–42. doi: 10.1542/peds.2004-2084. [DOI] [PubMed] [Google Scholar]
- 16.PHIS Team . Pediatric Health Information System Data Dictionary. Child Health Corporation of America; Shawnee Mission, KS: Oct, 2006. [Google Scholar]
- 17.Feudtner C, Christakis DA, Connell FA. Pediatric deaths attributable to complex chronic conditions: a population-based study of Washington State, 1980–1997. Pediatrics. 2000;106:205–9. [PubMed] [Google Scholar]
- 18.Feudtner C, Hays RM, Haynes G, Geyer JR, Neff JM, Koepsell TD. Deaths attributed to pediatric complex chronic conditions: national trends and implications for supportive care services. Pediatrics. 2001;107:E99. doi: 10.1542/peds.107.6.e99. [DOI] [PubMed] [Google Scholar]
- 19.Feudtner C, Silveira MJ, Christakis DA. Where do children with complex chronic conditions die? Patterns in Washington State, 1980–1998. Pediatrics. 2002;109:656–60. doi: 10.1542/peds.109.4.656. [DOI] [PubMed] [Google Scholar]
- 20.Palfrey JS, Sofis LA, Davidson EJ, Liu J, Freeman L, Ganz ML. The Pediatric Alliance for Coordinated Care: evaluation of a medical home model. Pediatrics. 2004;113:1507–16. [PubMed] [Google Scholar]
- 21.Srivastava R, Stone BL, Murphy NA. Hospitalist care of the medically complex child. Pediatr Clin North Am. 2005;52:1165–87. doi: 10.1016/j.pcl.2005.03.007. [DOI] [PubMed] [Google Scholar]
- 22.Lasser MS, Liao JG, Burd RS. National trends in the use of antireflux procedures for children. Pediatrics. 2006;118:1828–35. doi: 10.1542/peds.2006-1185. [DOI] [PubMed] [Google Scholar]
- 23.Schneier AJ, Shields BJ, Hostetler SG, Xiang H, Smith GA. Incidence of pediatric traumatic brain injury and associated hospital resource utilization in the United States. Pediatrics. 2006;118:483–92. doi: 10.1542/peds.2005-2588. [DOI] [PubMed] [Google Scholar]
- 24.Srivastava R, Downey EC, Feola P, Samore M, Coburn L, Holubkov R, et al. Quality of life of children with neurological impairment who receive a fundoplication for gastroesophageal reflux disease. J Hosp Med. 2007;2:165–73. doi: 10.1002/jhm.167. [DOI] [PubMed] [Google Scholar]
- 25.Buescher PA, Whitmire JT, Brunssen S, Kluttz-Hile CE. Children who are medically fragile in North Carolina: using Medicaid data to estimate prevalence and medical care costs in 2004. Matern Child Health J. 2006;10:461–6. doi: 10.1007/s10995-006-0081-3. [DOI] [PubMed] [Google Scholar]
- 26.Palfrey JS, Haynie M, Porter S, Fenton T, Cooperman-Vincent P, Shaw D, et al. Prevalence of medical technology assistance among children in Massachusetts in 1987 and 1990. Public Health Rep. 1994;109:226–33. [PMC free article] [PubMed] [Google Scholar]
- 27.Srivastava R, Berry JG, Hall M, Downey EC, O'Gorman M, Dean JM, et al. Reflux related hospital admissions after fundoplication in children with neurological impairment: retrospective cohort study. Bmj. 2009;339:b4411. doi: 10.1136/bmj.b4411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Simon TD, Berry J, Feudtner C, Stone BL, Sheng X, Bratton SL, et al. Children with complex chronic conditions in inpatient hospital settings in the United States. Pediatrics. 126:647–55. doi: 10.1542/peds.2009-3266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Burns KH, Casey PH, Lyle RE, Bird TM, Fussell JJ, Robbins JM. Increasing prevalence of medically complex children in US hospitals. Pediatrics. 126:638–46. doi: 10.1542/peds.2009-1658. [DOI] [PubMed] [Google Scholar]
- 30.Carrns A. Farewell, and don't come back. Health reform gives hospitals a big incentive to send patients home for good. US News World Rep. 147(20):2–3. [PubMed] [Google Scholar]
- 31.Coye MJ. CMS' stealth health reform. Plan to reduce readmissions and boost the continuum of care. Hosp Health Netw. 2008;82:24. [PubMed] [Google Scholar]
- 32.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–28. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 33.Jack BW, Chetty VK, Anthony D, Greenwald JL, Sanchez GM, Johnson AE, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med. 2009;150:178–87. doi: 10.7326/0003-4819-150-3-200902030-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Agency for Healthcare Research and Quality . Ambulatory Care Sensitive Conditions. Deptarment of Health and Human Services; Bethesda: U.S.: 2008. [Google Scholar]
- 35.Bhogal S, Zemek R, Ducharme FM. Written action plans for asthma in children. Cochrane Database Syst Rev. 2006;3:CD005306. doi: 10.1002/14651858.CD005306.pub2. [DOI] [PubMed] [Google Scholar]
- 36.Cochrane DD, Kestle J. Ventricular shunting for hydrocephalus in children: patients, procedures, surgeons and institutions in English Canada, 1989–2001. Eur J Pediatr Surg. 2002;12(Suppl 1):S6–11. doi: 10.1055/s-2002-36864. [DOI] [PubMed] [Google Scholar]
- 37.Iezzoni LI. Going beyond disease to address disability. N Engl J Med. 2006;355:976–9. doi: 10.1056/NEJMp068093. [DOI] [PubMed] [Google Scholar]
- 38.Paris MJ. Attitudes of medical students and health-care professionals toward people with disabilities. Arch Phys Med Rehabil. 1993;74:818–25. doi: 10.1016/0003-9993(93)90007-w. [DOI] [PubMed] [Google Scholar]
- 39.Martin HL, Rowell MM, Reid SM, Marks MK, Reddihough DS. Cerebral palsy: what do medical students know and believe? J Paediatr Child Health. 2005;41:43–7. doi: 10.1111/j.1440-1754.2005.00534.x. [DOI] [PubMed] [Google Scholar]