Abstract
Background
Oropharyngeal (OP) pH monitoring has been developed as a new way to diagnose supraesophageal gastric reflux (SEGR), but has not been well-validated. Our aim was to determine the correlation between OP pH and gastroesophageal (GER) events detected by multichannel intraluminal impedance-pH (MII-pH).
Methods
Fifteen patients (11 Males, median age 10.8 yrs) with suspected GER were prospectively evaluated with ambulatory 24-h OP pH monitoring (positioned at the level of the uvula) and concomitant esophageal MII-pH monitoring. Potential OP events were identified by the conventional pH threshold of <4, and by the following alternative criteria: 1) relative pH drop >10% from 15-min baseline and 2) absolute pH drop below thresholds of <5.5, 5.0, and 4.5. The 2-min window preceding each OP event was analyzed for correlation with an episode of GER detected by MII-pH.
Key Results
A total of 926 GER events were detected by MII-pH. Application of alternative pH criteria increased the identification of potential OP pH events; however, a higher proportion of oropharyngeal events had no temporal correlation with GER (45-81%), compared to the conventional definition of pH<4 (40%). A total of 306 full-column acid reflux episodes were dectected by MII-pH, of which 10(3.3%) were also identified by OP pH monitoring.
Conclusions & Inferences
Use of extended pH criteria increased the detection of potential SEGR events, but the majority of decreases in OP pH were not temporally correlated with GER. Oropharyngeal pH monitoring without concurrent esophageal measurements may over-estimate the presence of SEGR in children.
Keywords: esophageal impedance, gastroesophageal reflux, oropharyngeal pH monitoring, supraesophageal gastric reflux
Introduction
Recent evidence-based, consensus statements on gastroesophageal reflux disease (GERD) in children and adults categorize the condition into esophageal and extra-esophageal syndromes.(1, 2) Extra-esophageal manifestations are postulated to occur when gastric refluxate enters into areas above the protection of the upper esophageal sphincter (UES), also known as supra-esophageal gastric reflux (SEGR). Laryngeal and pulmonary manifestations linked to reflux include hoarseness, sore throat, globus sensation, chronic cough, asthma, and bronchiolitis obliterans syndrome in post-lung transplant patients.(3-6) Although the association between reflux and extra-esophageal symptoms has been well described,(7, 8) establishment of a clear, causal relationship has been elusive. Consequently, although SEGR is commonly implicated, formal diagnosis and management remains clinically challenging.
Symptoms or clinical findings alone cannot be relied upon for accurate diagnosis of SEGR. Abnormal distal esophageal acid exposure on pH monitoring can indicate the presence of pathologic GERD, but does not provide proof of causality for extra-esophageal symptoms. The presence of abnormal proximal esophageal acid reflux on dual-sensor pH monitoring has not been shown to predict response to therapy either.(9)
Current diagnostic methods are limited by the lack of consensus regarding the optimal pH criteria for SEGR. The minimum amount of supra-esophageal acid exposure needed to produce clinically significant pathologic changes is unknown, but a SEGR event is conventionally defined as a drop in proximal pH below 4, in association with a preceding or simultaneous distal reflux event. Although appropriate for the distal esophagus and GERD, use of this pH cutoff for SEGR has been brought into question. First of all, it has been observed that approximately 30% of acid refluxate has a pH >4 by the time it reaches the proximal esophagus.(10) Furthermore, recent data have suggested that nonacid reflux with pH 4-7 may contribute to airway and respiratory disease.(11-13) Thus, the traditional cutoff of pH<4 for SEGR may actually underestimate the presence of clinically significant reflux. Several recent studies have suggested using higher pH cutoffs for proximal pH monitoring. Weiner et al. defined a SEGR event as a rapid (0.5 – 2 seconds), vertical drop in oropharyngeal pH of at least 10% from a running pH baseline.(14) Ayazi et al. proposed using a cutoff of pH <5.5 when the patient is upright, and a lower cutoff of pH<4.5 when the patient is supine.(15)
Recent advances in diagnostic technologies along with use of these alternative criteria may be able to overcome some of the previous limitations encountered with traditional pH monitoring. The Restech Dx-pH sensor is a minimally invasive, transnasal catheter which features an ion flow sensor that is able to measure the pH of both liquid and aerosolized droplets in the posterior oropharynx. We hypothesized that direct measurement of oropharyngeal pH using the Restech probe may provide an accurate, but less-invasive diagnostic tool for SEGR compared to current methods. The aim of this study was to monitor oropharyngeal pH with this newly designed sensor and to determine the correlation between changes in oropharyngeal pH and gastroesophageal reflux events characterized by MII-pH monitoring.
Materials and Methods
Patients
This was a prospective study in which patients referred for investigation of possible GERD were recruited at Children’s Hospital Boston between November 2009 and June 2010. Patients were included if they (a.) had already been scheduled for an esophageal MII-pH probe study as part of their evaluation by their primary gastroenterologist (b.) had discontinued acid suppression therapy at least 72 hours before testing; (c.) had no history of congenital anomalies; and (d.) had no history of gastric or esophageal surgery. Additional exclusion criteria included: inability to tolerate placement of two intranasal probes and inability to refrain from use of acid suppression medications prior to or during study duration. Permission to conduct the study was approved by the investigational review board of Children’s Hospital Boston and informed consent was obtained for each participant.
Esophageal Impedance-pH Monitoring
Each study was performed using an ambulatory MII-pH system (Sandhill Scientific, Highlands Ranch, CO). Two different age-appropriate impedance catheters were used in the study: pediatric (2-10 yr) and adult (>10 yr). Each catheter had seven impedance sensors and one distal pH sensor. The polyurethane catheter was passed transnasally and positioned with the distal pH sensor 5 cm above the proximal border of the lower esophageal sphincter (LES). Catheter location was confirmed by chest X-ray and adjusted following guidelines from the European Society for Pediatric Gastroenterology, Hepatology and Nutrition so that the distal pH sensor was at the third vertebral body above the diaphragmatic angle.
Oropharyngeal pH Monitoring
The Restech Dx-pH probe (Respiratory Technology Corp., San Diego, CA) is a transnasal, antimony-based pH sensor. The tip of the probe is tear-drop shaped which is designed to aid in maintenance of moisture saturation of the sensor from exhaled breath condensation on the tip surface. A colored light emitting diode (LED) at the tip aids in trans-oral visualization during placement. Shortly after the esophageal MII-pH probe was placed, the Restech probe was inserted into the same nare until the flashing LED was seen in the back of the subject’s throat and then positioned so that the LED was at the level of the uvula. Both catheters were then secured to the patient’s face and neck using Tegaderm.
Recording Technique
The internal clocks of both data recorders were synchronized prior to the start of the monitoring period to assure simultaneous monitoring of esophageal pH-MII and oropharyngeal pH. After appropriate placement of both sensors, data recording was started. The pH-MII and Restech probes were electronically synchronized a second time by simultaneously pressing the event button on both recorders five times in short succession. Patients were instructed to eat a regular diet with a minimum of 3 hours between each meal. When patients experienced symptoms, changed body position, or ate meals, they recorded these events on the pH-MII data recorder by pressing the appropriate button. Patients were also asked to record events on a written symptom/event diary as well. Logs were reviewed by one of the authors (E.C.) at the end of the study to ensure accurate completion.
Once the esophageal and oropharyngeal monitoring studies were completed, both catheters were removed. Data from both digital recorders was downloaded to a password-protected compter and the data was analyzed with commercially-available software (BioView Analysis, Sandhill Scientific, Highlands Ranch, CO and DataView Lite, Respiratory Technology Corp, San Diego, CA). As described in previous studies, data collected during meal periods were excluded from the analysis. All subjects tolerated the procedure well without incident or complications.
Definitions – Esophageal MII-pH Episodes
Each of the esophageal MII-pH tracings was manually analyzed by one investigator (E.C.). Each gastroesophageal reflux episode was individually scored. A liquid reflux episode detected by impedance was defined as a retrograde drop in impedance of >50% of the baseline impedance value in the distal 2 channels. A reflux episode was defined as acid if there was an associated drop in distal esophageal pH to <4, and non-acid if there was no associated drop in esophageal pH to <4. Full-column reflux was defined as an episode that reached the highest pair of impedance sensors. A pH-only episode was defined as a fall in distal pH to <4 lasting at least 5 seconds detected by the pH sensor only, without a retrograde drop in impedance. If there was evidence of an anterograde drop in impedance of >50% of the baseline impedance value immediately preceding or simultaneous to the drop in distal esophageal pH, the pH-only episode was considered to be swallow-associated.
A distal esophageal pH probe was considered abnormal using the criteria established by the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition if the pH was <4 for greater than 6% of the time for children >1 year old.(16) Patients were classified as having abnormal MII-pH testing if the total number of reflux events recorded was greater than 73, according to normal adult standards.(17) No pediatric normal values exist for MII-pH in this age group, although pediatric control data suggest that pediatric normal values may be similar to those in adults.(18)
Definitions – Oropharyngeal pH Episodes
Oropharyngeal pH tracings were also manually analyzed by one investigator (E.C.). Because there is no consensus on the appropriate pH criteria which should be applied to oropharyngeal pH data, several different definitions were applied. Proximal pH data were evaluated according to the conventional definition of SEGR (proximal pH drop <4). In addition, alternative definitions were also applied: (1) pH drop of at least 10% from a running baseline(14) and (2) pH drop below thresholds of <5.5, 5.0, or 4.5 for a minimum of 5 seconds. The number of potential reflux events was determined using each definition separately. Correlation between oropharyngeal pH and esophageal impedance was determined based on the temporal relationship between oropharyngeal and esophageal reflux events. For each proximal pH event that was detected, the preceding 2-minute window of the concurrent distal esophageal MII-pH tracing was examined for a distal reflux event to be considered as an episode of SEGR (Figures 1a and 1b).
Figure 1A amp; 1B. Combined Restech oropharyngeal pH and esophageal MII-pH monitoring.

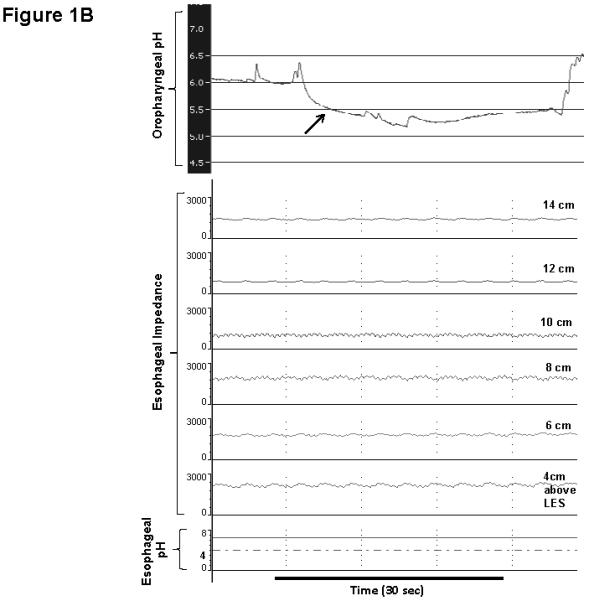
1A) The shaded box depicts an episode of acidic, full-column esophageal reflux. This liquid reflux episode is denoted by retrograde drops in esophageal impedance (black arrow) and extends to 14 cm above the LES. This episode is also associated with a simultaneous drop in distal esophageal pH <4 (bottom tracing). The Restech probe (top tracing) also shows a corresponding drop in oropharyngeal pH <5.5(white arrow). 1B) An example of a drop in oropharyngeal pH <5.5 (white arrow) detected by Restech probe without any corresponding changes in esophageal impedance or distal esophageal pH.
Symptom Association Analysis
A symptom event was considered temporally associated with an episode of GER or SEGR if it occurred within the 2 minutes before or after the reflux episode. The symptom index (SI), defined as: number of symptoms associated with reflux/total number of symptoms, was considered to be positive if the value was ≥50%.(19) The symptom sensitivity index (SSI), defined as: number of reflux episodes associated with symptoms/total number of reflux episodes, was considered to be positive if the value was ≥10% .(20)
Statistical Analysis
To determine the sample size for the study, our primary outcome was the proportion of SEGR episodes identified by esophageal MII-pH monitoring (as defined by episodes of full-column, acid reflux) which were also detected by the Restech Dx-pH Measurement System, using a drop from baseline pH of at least 10%. As such, the outcome represents a series of Bernoulli trials where each trial results in either a success (Restech probe detects SEGR when the MII-pH probe detects SEGR) or a failure. Given that patients may experience several SEGR events over a 24-hour period and these events within patients will be correlated, a variance inflation factor (VIF) was incorporated into the usual 95% CI for the binomial proportion.(21) Based on prior data, we estimated an intraclass correlation of 0.22, leading to a variance inflation factor (VIF) of 5.63.
Since the Dx-pH measurement system is designed to be used in place of more invasive esophageal probes for the detection of SEGR events, we hypothesized that the Dx-pH would detect at least 90% of SEGR events identified by MII-pH. Based on the binomial proportion calcuation, we estimated that a total of 195 SEGR events would be required in order to obtain a 95% CI where the true proportion of SEGR events also detected by the Restech probe is 0.90, with a lower bound of no less than 0.80. Our prior research suggests that the mean number of SEGR events detected by the MII-pH proximal probe per patient in a 24 hour period is approximately 13 events. Therefore, dividing a total of 195 SEGR episodes by 13, we estimated that a sample size of 15 patients would be required.
Summary statistics for continuous variables were expressed as either mean ± standard deviation for normally distributed outcomes, or median with associated interquartile range (IQR) for non-normally distributed outcomes. Frequency distributions were used for categorical variables. Tests of group differences in the outcome were made using Student t test of the Wilcoxon rank-sum test depending on whether or not the covariate was approximately normally distributed. Pearson χ2 or Fisher exact test was used in the case of categorical covariates. Correlation was assessed using the Spearman Rank correlation test. Data analysis was generated using Statistical Package for the Social Sciences, version 18.0 (SPSS, Chicago, IL, USA).
Results
A total of 15 patients (11 male; median age 10.8 years, IQR 8.3 -12.4 years) with suspected GERD were recruited and underwent the study protocol (mean duration of testing: 22.9 ± 4.5 hours). Indications for testing in all children was suspicion of gastroesophageal reflux; nine subjects presented with both esophageal and extra-esophageal symptoms, fivesubjects presented with esophageal symptoms only, and one subject presented with extra-esophageal symptoms only. Esophageal symptoms reported included heartburn, regurgitation and chest pain. Extra-esophageal symptoms included cough, throat clearing, and intractable sore throat.
Gastroesophageal Reflux
A total of 926 reflux events were detected by impedance. Of these, 743 (80.2%) GER episodes were acidic (pH <4). There were 306 episodes of acid reflux which extended to the most proximal pair of impedance sensors and determined to be full-column. For our primary outcome, the Restech Dx-pH probe detected 10 out of 306 full-column, acid GER episodes, for an estimated sensitivity of 3.3% (95% CI 1.6%, 5.9%); the association between oropharyngeal events with other types of distal reflux is shown in Table 1. A separate analysis including only subjects who reported extra-esophageal symptoms was not significantly different. In this subgroup (n=10). A total of 643 reflux events were detected by MII-pH. Of these, 211 episodes were both acidic and full-column. The Restech probe detected 8 out of 211 full-column, acid GER episodes, for an estimated sensitivity of 3.8% (95% CI 1.9%, 7.3%) which is not statistically significant from the sensitivity if all patients are included (3.3% all vs 3.8% only those with symptoms). The proportion of oropharyngeal events in these patients which correlated with distal GER was also not significantly different: pH <4 – 1 out of 3 (33%) events correlated with GER; pH <4.5 – 1 out of 7 (14%) events correlated with GER; pH <5 – 2 out of 25 (8%) events correlated with GER; pH <5.5 – 18 out of 140 (13%) events correlated with GER ; pH drop >10% - 9 out of 76 (12%) events correlated with GER . Therefore the results do not change when only symptomatic patients are analyzed
Table 1.
Proportion of distal esophageal reflux events detected by MII-pH with corresponding changes in oropharyngeal pH detected by Restech probe.
| Type of Distal Reflux | Total number of events | Number of events with corresponding change in OP pH (%) |
|---|---|---|
| Full Column, Acid GER | 306 | 10 (3.3%) |
|
Full Column, Non-acid
GER |
55 | 1 (1.8%) |
| pH-Only Event | 85 | 11 (12.9%) |
| All GER by MII-pH | 926 | 21 (2.3%) |
GER, gastroesophageal reflux; OP, oropharyngeal; MII-pH, multiple intraluminal impedance-pH
The majority of GER episodes (745/926) occurred in the upright position. The median number of GER episodes per subject per 24 hours was 59 (IQR 26.5 - 80). The median acid exposure time in the distal esophagus was 5.2% (IQR 3.1% – 9.6%). In total, 7 subjects had an abnormal pH parameter for distal reflux, while 6 subjects had an abnormal number of reflux events (>73 per 24 hour period). There was significant correlation between the number full-column reflux episodes reaching the proximal esophagus and the total number in the distal esophagus (r = 0.783, P =0.001).
Supra-Esophageal Gastric Reflux
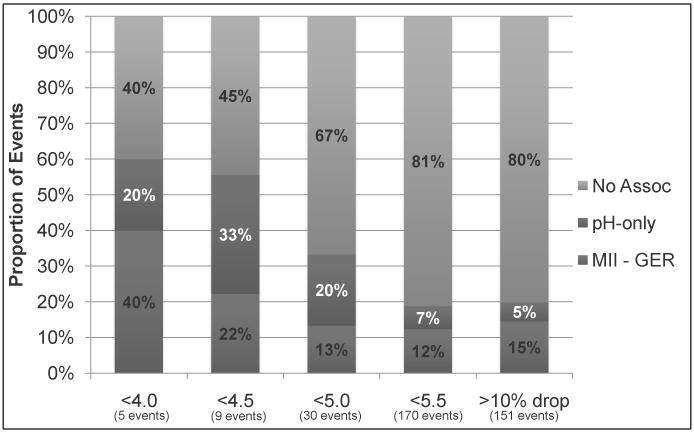
Overall, the detection of oropharyngeal pH events increased substantially with extended definitions of SEGR, compared to the conventional definition of pH <4 (Figure 2). The mean number oropharyngeal events with pH <4 was 0.3 ± 0.6 per subject, compared with 0.6 ± 1.1 events with pH <4.5; 2.0 ± 4.0 events with pH <5; 11.3 ± 21.5 events with pH <5.5; and 10.1 ± 13.9 events with pH drop >10%. The proportion of oropharyngeal pH events which were not temporally related to an episode of a distal reflux ranged from 40% to 81%, depending on the proximal pH criteria used (Figure 3). It is interesting that 91% of oropharyngeal events which were correlated with a distal pH-only event were also associated with evidence of an antegrade liquid swallow on impedance.
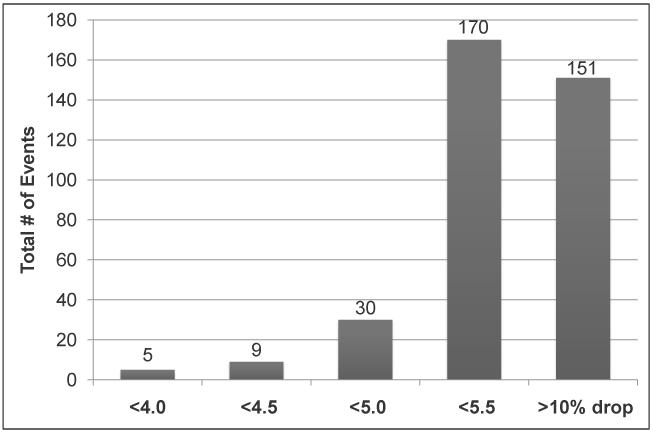
Figure 2. Impact of pH definition on the total number of oropharyngeal events detected by Restech pH probe.
As shown here, the number of events detected increased with extended definitions of SEGR.
Figure 3. Association of oropharyngeal pH events with gastroesophageal reflux.
As can be seen, the proportion of oropharyngeal events unassociated with distal GER increased with extended definitions of SEGR.
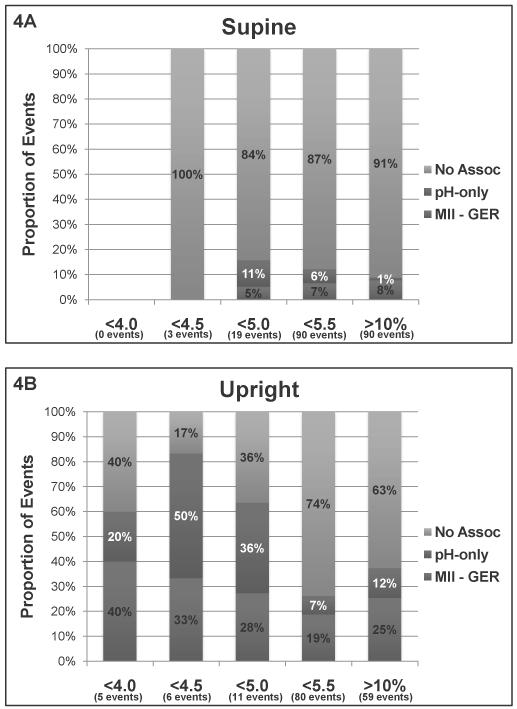
Distal GER events occurred predominantly (80.5%) in the upright position; similarly, when the conventional pH <4 cutoff was used, 100% of oropharyngeal pH events also occurred while upright. When extended pH criteria were applied, the opposite trend was observed, with 63% of pH <5 events, 53% of pH <5.5 events and 64% of pH drop >10% events occurring in the supine position. Furthermore, the proportion of oropharyngeal events which were not associated with GER was higher when subjects were supine compared to upright (Figure 4). There was no significant association between the number of oropharyngeal pH events detected using the various criteria (pH< 4.0, <4.5, <5.0, <5.5 or >10% drop) and any conventional reflux parameters such as percent time distal pH <4, total number of GER events, or number of full-column GER events. Likewise, there was no correlation between the percent time oropharyngeal pH <4.0, <4.5, <5.0, or <5.5, and any MII-pH reflux parameters.
Figure 4A amp; 4B. Comparison of oropharyngeal pH and esophageal MII-pH correlation between supine and upright body positions.
As can be seen, when subjects were supine (4A), the proportion of oropharyngeal events without an associated episode of GER was higher than when subjects were upright (4B).
Symptom Association
All subjects reported at least one symptom during the 24 hour monitoring period. A total of 260 symptom events were recorded; of these, 46.9% were temporally associated with a GER event and 2.3% were associated with an oropharyngeal pH event. Out of 926 GER events detected by MII-pH, 184 (20%) were associated with symptoms. In comparison, 2/5 (40%) pH<4 events, 3/9 (33%) pH<4.5 events, 6/30 (20%) pH<5 events, 11/170 (7%) pH<5.5 events, and 14/151 (9%) pH drop >10% events detected by the Restech probe were symptom-associated. Five out of fifteen (33%) subjects had a positive symptom index (SI) while 7/15 (47%) subjects had a positive symptom sensitivity index (SSI) for GER events detected by MII-pH. No subjects had a positive SI for oropharyngeal pH events, while 3/15 (20%) subjects had a positive SSI for oropharyngeal pH events. The Restech probe failed to identify 5 subjects with a positive symptom index (SI) and 4 subjects with a positive symptom sensitivity index (SSI) based on MII-pH results
Discussion
By using simultaneously recorded ambulatory 24-h esophageal MII-pH and oropharyngeal pH monitoring, we sought to systematically assess the correlation between changes in oropharyngeal pH and more than 900 episodes of GER. For the first time, concurrent intraesophageal impedance and pH recording was used to validate whether changes in pH detected by the Restech oropharyngeal catheter were in association with either acid or non-acid GER episodes. Overall, the proportion of acidic, full-column reflux episodes which were simultaneously detected by the oropharyngeal pH probe was low (3.3%). Furthermore, our study also demonstrated that the majority of acid and weakly-acidic oropharyngeal events which were identified had no temporal correlation with GER events detected by esophageal MII-pH monitoring. The clinical significance these changes in oropharyngeal pH unrelated to reflux is not known. Finally, subjects were less likely to have a positive symptom correlation with oropharyngeal pH monitoring than with esophageal MII-pH monitoring.
The role of reflux in extra-esophageal syndromes is supported by established associations, but remains poorly defined. This is likely due in part to the non-specific nature of extra-esophageal symptoms and the lack of pathognomonic endoscopic or laryngoscopic features. Unfortunately, the presence of abnormal distal or proximal acid reflux on pH monitoring has not been shown to predict the response of extra-esophageal symptoms to PPI therapy or antireflux surgery.(9, 22, 23) In an effort to improve the diagnostic accuracy for reflux-related respiratory and laryngeal symptoms, some investigators have proposed placement of a proximal pH sensor in the pharynx or oropharynx.(24) In the past, oropharyngeal pH monitoring has been limited by a high frequency of artifacts.(25) The Restech oropharyngeal pH probe and sensor utilized in this study was designed to avoid these limitations. This probe also has the added advantage of reduced patient discomfort and easier placement compared to an intra-esophageal catheter, but it has not yet been validated for the detection of SEGR in children.
Conventionally, the threshold used in distal esophageal pH monitoring was based on studies showing that heartburn is associated with esophageal exposure to a pH less than 4.(26) The sub-acute nature of many extra-esophageal symptoms has made it difficult to establish a similar pH threshold for oropharyngeal pH monitoring. There is mounting evidence that use of the same pH<4 threshold may be inappropriate for SEGR. First of all, neutralization of acidic gastric refluxate occurs when saliva is swallowed, which results in a gradient of increasing pH from the distal to proximal esophagus and oropharynx.(27, 28) A pH threshold of <4 would therefore miss some episodes of abnormal oropharyngeal exposure to gastric refluxate. In addition, there is emerging evidence that extra-esophageal symptoms are clinically associated with weakly-acidic reflux (pH 4-7).(29-31) Studies demonstrating the damaging effects of pepsin in nonacidic refluxate on laryngeal epithelium add further evidence towards this biologic plausibility.(32)
Investigators have therefore recently proposed the use of alternative pH criteria based on less acidic pH thresholds or relative drops in pH to improve the diagnosis of SEGR.(14, 15) In the present study, we applied these non-validated criteria in addition to the conventional pH threshold of <4 to oropharyngeal pH data obtained from children with suspected reflux. When the conventional threshold of pH <4 was used, we demonstrated very little evidence of oropharyngeal acid exposure. This is consistent with recent studies using the Restech probe in normal adult volunteers, in which both the median number of oropharyngeal events with pH <4 and median percent time pH <4 were also found to be zero.(15, 33, 34) Even among patients with suspected reflux, an oropharyngeal threshold of pH <4 may be too stringent and insensitive to identify episodes of SEGR.
When extended pH criteria were applied in the present study, there was a considerable increase in the number of events detected which qualified as SEGR, potentially increasing the diagnostic yield of oropharyngeal pH monitoring. The percentage of events which were not associated with a distal GER event however, increased disproportionately with these alternative pH criteria. We doubt that a prolonged delay (>2 min) between an episode of GER and subsequent acidification of the oropharynx would account for the lack of correlation. If that were the case, we would still expect to see a direct correlation between overall oropharyngeal acid exposure (e.g. percent time below pH cutoff) with distal reflux parameters, which was not observed.
The high proportion of non-correlating oropharyngeal pH events seen in our study is consistent with other investigations employing concurrent pharyngeal and esophageal pH monitoring in adults. Williams et al, found that 92% of pharyngeal pH decreases of 1-2 pH units and 66% of pH <4 events were artifactual or independent of esophageal acidification.(35) Harrell and colleagues similarly reported that approximately 80% of hypopharyngeal pH drops <4 observed in their study were potentially due to artifacts.(25) Moreover, recent studies which combined the Restech pH probe with concurrent esophageal pH monitoring in adults also found inconsistencies between oropharyngeal and distal esophageal pH data. Golub et al, described a tendency for the oropharyngeal pH probe to register progressively lower pH levels and more non-correlating pH events during sleep, and even suggested that data obtained during sleep should be excluded from analysis, in order to improve correlation with distal events.(36) Chheda et al, also observed a higher rate of false positive and non-corresponding pharyngeal events occurring in the supine position in a study of asymptomatic, normal adult volunteers.(33)
Our study similarly found that a higher proportion of oropharyngeal events recorded while supine were not correlated with distal reflux. One reason for this finding may be that the supine position is a surrogate marker for sleep, when salivary flow is reduced. We postulate that this may lead to drying of the pH electrode and false readings. This phenomenon was initially described by Wiener et al as “pharyngeal pseudoreflux” in reference to artifacts with a gradual descent to pH <4 without a corresponding fall in esophageal pH.(37) Other potential causes for pH artifacts include loss of mucosal contact or undocumented liquid swallows outside of meals. For the time being, given our results, we would suggest limiting use of the Restech pH monitoring device to research purposes and only in conjunction with simultaneous distal esophageal monitoring if it is intended for the detection of supraesophageal gastric reflux. Future studies may consider utilizing the Restech probe to characterize the oropharyngeal pH environment in general and to improve the understanding of pharyngeal pH drops which occur independently of reflux.
In the present study, a proportion of oropharyngeal events detected by Restech, were temporally associated with distal pH<4detected by the pH meter, in the absence of reflux detected by impedance monitoring (pH-only reflux). We propose two potential scenarios which might account for this unexpected but interesting association with pH-only reflux: First given that the act of swallowing triggers a brief simultaneous relaxation of the LES, which may allow a small amount of acid to enter the distal-most esophagus, it is possible that the amount of acid is detected by the distal pH sensor without meeting impedance criteria for reflux , and that this is accompanied by the full-column reflux of a small amount of gaseous or aerosolized acid significant enough to result in pH decline in the oropharyngeal probe too. The other possibility is that there was swallowing of undocumented acidic saliva or more unlikely acidic liquids, leading to both a drop in oropharyngeal and esophageal pH. The exact significance of these episodes needs to be studied further.
Some potential limitations need to be acknowledged with regard to this study. First of all, we were unable to confirm whether full-column episodes extended proximally above the UES in order to be truly considered supra-esophageal. Indeed, episodes of reflux which reach the proximal-most pair of impedance sensors but remain distal to the UES may or may not result in a significant change in oropharyngeal pH. Furthermore, because of the fixed spacing of sensors on the impedance catheter, we were unable to standardize the gap in distance between the proximal sensor and the oropharyngeal pH electrode—which was consistently placed at the level of the uvula. This may account for some of the variability in correlation between esophageal and oropharyngeal measurements. Although this limitation may have led to an underestimation of the Restech probe’s sensitivity for full-column acid reflux, it is clearly unrelated to the Restech’s probe’s poor specificity (i.e. 40-81% of oropharyngeal events had no correlation with any reflux detected by MII-pH). Future studies should consider incorporating pharyngeal impedance in order to better characterize changes in oropharyngeal pH in the context of liquid or gaseous reflux in areas above the UES.
Secondly, because there was no separate control group, we cannot comment directly on how the frequency of oropharyngeal reflux in children with suspected reflux compares with healthy controls. Although normative data is helpful in establishing optimal pH criteria, this was not within the scope our study. Aside from the challenges of performing invasive tests on healthy children, we chose to focus on children with suspected GER in order to maximize encounters with potential SEGR events and gain information about the relationship between oropharyngeal pH and GER.
Finally, the use of two different technologies together raises the possibility of differences in pH sampling rates as well as lack of synchronization between studies leading to errors in correlation. We employed several measures in our protocol to ensure that the two probes were electronically synchronized. Secondly, the addition of esophageal impedance monitoring allowed us to detect the presence of all GER episodes, independent of the distal pH probe.
In conclusion, use of concurrent oropharyngeal pH and esophageal MII-pH monitoring allowed us to evaluate the correlation between gastroesophageal reflux episodes and changes in pH in the posterior oropharyngeal environment. The results of our study indicate that traditional acid reflux (pH <4) to the level of the oropharynx is rare, even in children with suspected reflux. Application of extended pH criteria significantly increases the detection of pH events in the oropharynx qualifying as SEGR. However, the majority of acidic and weakly-acidic changes in oropharyngeal pH are not temporally correlated with GER episodes, especially when subjects are in the supine position, suggesting that they may be artifactual and occur independently of reflux. Thus, 24-hour pH monitoring of the oropharynx without concurrent esophageal monitoring may over-estimate the presence of SEGR in children. Future studies are required to determine the optimal pH criteria for oropharyngeal pH events, and whether oropharyngeal monitoring can be used to more accurately identify patients with abnormal SEGR.
Acknowledgments
This work was supported by grants from the Thrasher Research Fund (EC) and National Institutes of Health, USA: T32DK007477-25 (EC), K23DK073713 (RR), R21DK77678-2 (SN) and K24DK082792A (SN)
Footnotes
- Eric Chiou reports no financial, professional, or personal competing interests.
- Rachel L. Rosen reports no financial, professional, or personal competing interests.
- Hongyu Jiang reports no financial, professional, or personal competing interests.
- Samuel Nurko reports no financial, professional, or personal competing interests.
References
- 1.Sherman PM, Hassall E, Fagundes-Neto U, et al. A global, evidence-based consensus on the definition of gastroesophageal reflux disease in the pediatric population. Am J Gastroenterol. 2009;104:1278–1295. doi: 10.1038/ajg.2009.129. quiz 1296. [DOI] [PubMed] [Google Scholar]
- 2.Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006;101:1900–1920. doi: 10.1111/j.1572-0241.2006.00630.x. quiz 1943. [DOI] [PubMed] [Google Scholar]
- 3.Koufman J. The otolaryngologic manifestations of gastroesophageal reflux disease (GERD): a clinical investigation of 225 patients using ambulatory 24-hour pH monitoring and an experimental investiations of the role of acid and pepsin in the development of laryngeal injury. Laryngoscope. 1991;101:1–78. doi: 10.1002/lary.1991.101.s53.1. [DOI] [PubMed] [Google Scholar]
- 4.Thakkar K, Boatright RO, Gilger MA, El-Serag HB. Gastroesophageal reflux and asthma in children: a systematic review. Pediatrics. 2010;125:e925–930. doi: 10.1542/peds.2009-2382. [DOI] [PubMed] [Google Scholar]
- 5.Sweet M, Patti M, Hoopes C, Hays S, Golden J. Gastro-oesophageal reflux and aspiration in patients with advanced lung disease. Thorax. 2009;64:167–173. doi: 10.1136/thx.2007.082719. [DOI] [PubMed] [Google Scholar]
- 6.Palmer S, Miralles A, Howell D, Brazer S, Tapson V, Davis R. Gastroesophageal reflux as a reversible cause of allograft dysfunction after lung transplantation. Chest. 2000;118:1214–1217. doi: 10.1378/chest.118.4.1214. [DOI] [PubMed] [Google Scholar]
- 7.El-Serag H, Gilger M, Keubeler M, Rabeneck L. Extraesophageal associations of gastroesophageal reflux disease in children without neurologic defects. Gastroenterology. 2001;121:1294–1299. doi: 10.1053/gast.2001.29545. [DOI] [PubMed] [Google Scholar]
- 8.Tolia V, Vandenplas Y. Systematic review: the extra-oesophageal symptoms of gastro-oesophageal reflux disease in children. Aliment Pharmacol Ther. 2009;29:258–272. doi: 10.1111/j.1365-2036.2008.03879.x. [DOI] [PubMed] [Google Scholar]
- 9.Vaezi MF, Richter JE, Stasney CR, et al. Treatment of chronic posterior laryngitis with esomeprazole. Laryngoscope. 2006;116:254–260. doi: 10.1097/01.mlg.0000192173.00498.ba. [DOI] [PubMed] [Google Scholar]
- 10.Emerenziani S, Ribolsi M, Sifrim D, Blondeau K, Cicala M. Regional oesophageal sensitivity to acid and weakly acidic reflux in patients with non-erosive reflux disease. Neurogastroenterol Motil. 2009;21:253–258. doi: 10.1111/j.1365-2982.2008.01203.x. [DOI] [PubMed] [Google Scholar]
- 11.Johnston N, Wells CW, Samuels TL, Blumin JH. Pepsin in nonacidic refluxate can damage hypopharyngeal epithelial cells. Ann Otol Rhinol Laryngol. 2009;118:677–685. doi: 10.1177/000348940911800913. [DOI] [PubMed] [Google Scholar]
- 12.Rosen R, Nurko S. The importance of multichannel intraluminal impedance in the evaluation of children with persistent respiratory symptoms. Am J Gastroenterol. 2004;99:2452–2458. doi: 10.1111/j.1572-0241.2004.40268.x. [DOI] [PubMed] [Google Scholar]
- 13.Patterson N, Mainie I, Rafferty G, et al. Nonacid reflux episodes reaching the pharynx are important factors associated with cough. J Clin Gastroenterol. 2009 doi: 10.1097/MCG.0b013e31818859a3. [DOI] [PubMed] [Google Scholar]
- 14.Wiener G, Tsukashima R, Kelly C, et al. Oropharyngeal pH Monitoring for the Detection of Liquid and Aerosolized Supraesophageal Gastric Reflux. Journal of Voice. 2009;23:498–504. doi: 10.1016/j.jvoice.2007.12.005. [DOI] [PubMed] [Google Scholar]
- 15.Ayazi S, Lipham J, Hagen J, et al. A new technique for measurement of pharyngeal pH: normal values and discriminating pH threshold. J Gastrointest Surg. 2009;13:1422–1429. doi: 10.1007/s11605-009-0915-6. [DOI] [PubMed] [Google Scholar]
- 16.Rudolph C, Mazur L, Liptak G, et al. Guidlines for evaluation and treatment of gastroesophageal reflux in infants and children: recommendations of the North American Society for Pediatric Gastroenterology and Nutrition. J Pediatr Gastroenterol Nutr. 2001;32:S1–31. doi: 10.1097/00005176-200100002-00001. [DOI] [PubMed] [Google Scholar]
- 17.Shay S, Tutuian R, Sifrim D, et al. Twenty-four hour ambulatory simultaneous impedance and pH monitoring: a multicenter report of normal values from 60 healthy volunteers. Am J Gastroenterol. 2004;99:1037–1043. doi: 10.1111/j.1572-0241.2004.04172.x. [DOI] [PubMed] [Google Scholar]
- 18.Rosen R, Furuta G, Fritz J, Donovan K, Nurko S. Role of acid and nonacid reflux in children with eosinophilic esophagitis compared with patients with gastroesophageal reflux and control patients. J Pediatr Gastroenterol Nutr. 2008;46:520–523. doi: 10.1097/MPG.0b013e318158600c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wiener G, Richter J, Copper J, Wu W, Castell D. The symptom index: a clinically important parameter of ambulatory 24-hour esophageal pH monitoring. Am J Gastroenterol. 1988;83:358–361. [PubMed] [Google Scholar]
- 20.Breumelhof R, Smout A. The symptom sensitivity index: a valuable additional parameter in 24-hour esophageal pH monitoring. Am J Gastroenterol. 1991;86:160–164. [PubMed] [Google Scholar]
- 21.Ridout MS, Demetrio CG, Firth D. Estimating intraclass correlation for binary data. Biometrics. 1999;55:137–148. doi: 10.1111/j.0006-341x.1999.00137.x. [DOI] [PubMed] [Google Scholar]
- 22.Kaufman JA, Houghland JE, Quiroga E, Cahill M, Pellegrini CA, Oelschlager BK. Long-term outcomes of laparoscopic antireflux surgery for gastroesophageal reflux disease (GERD)-related airway disorder. Surg Endosc. 2006;20:1824–1830. doi: 10.1007/s00464-005-0329-9. [DOI] [PubMed] [Google Scholar]
- 23.Wo JM, Hunter JG, Waring JP. Dual-channel ambulatory esophageal pH monitoring. A useful diagnostic tool? Dig Dis Sci. 1997;42:2222–2226. doi: 10.1023/a:1018802330957. [DOI] [PubMed] [Google Scholar]
- 24.Wiener GJ, Koufman JA, Wu WC, Cooper JB, Richter JE, Castell DO. Chronic hoarseness secondary to gastroesophageal reflux disease: documentation with 24-h ambulatory pH monitoring. Am J Gastroenterol. 1989;84:1503–1508. [PubMed] [Google Scholar]
- 25.Harrell SP, Koopman J, Woosley S, Wo JM. Exclusion of pH artifacts is essential for hypopharyngeal pH monitoring. Laryngoscope. 2007;117:470–474. doi: 10.1097/MLG.0b013e31802d344c. [DOI] [PubMed] [Google Scholar]
- 26.Tuttle SG, Rufin F, Bettarello A. The physiology of heartburn. Ann Intern Med. 1961;55:292–300. doi: 10.7326/0003-4819-55-2-292. [DOI] [PubMed] [Google Scholar]
- 27.Weusten B, Akkermans L, Van Berge Henegouwen G, Smout A. Spatiotemporal characteristics of physiological gastroesophageal reflux. Am J Physiol. 1994;266:G357–G362. doi: 10.1152/ajpgi.1994.266.3.G357. [DOI] [PubMed] [Google Scholar]
- 28.Shaker R, Milbrath M, Ren J, et al. Esophagopharyngeal distribution of refluxed gastric acid in patients with reflux laryngitis. Gastroenterology. 1995;109:1575–1582. doi: 10.1016/0016-5085(95)90646-0. [DOI] [PubMed] [Google Scholar]
- 29.Mainie I, Tutuian R, Shay S, et al. Acid and non-acid reflux in patients with persistent symptoms despite acid suppressive therapy: a multicentre study using combined ambulatory impedance-pH monitoring. Gut. 2006;55:1398–1402. doi: 10.1136/gut.2005.087668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tutuian R, Vela MF, Hill EG, Mainie I, Agrawal A, Castell DO. Characteristics of symptomatic reflux episodes on Acid suppressive therapy. Am J Gastroenterol. 2008;103:1090–1096. doi: 10.1111/j.1572-0241.2008.01791.x. [DOI] [PubMed] [Google Scholar]
- 31.Sifrim D, Mittal R, Fass R, et al. Review article: acidity and volume of the refluxate in the genesis of gastro-oesophageal reflux disease symptoms. Aliment Pharmacol Ther. 2007;25:1003–1017. doi: 10.1111/j.1365-2036.2007.03281.x. [DOI] [PubMed] [Google Scholar]
- 32.Samuels TL, Johnston N. Pepsin as a causal agent of inflammation during nonacidic reflux. Otolaryngol Head Neck Surg. 2009;141:559–563. doi: 10.1016/j.otohns.2009.08.022. [DOI] [PubMed] [Google Scholar]
- 33.Chheda N, Seybt M, Schade R, Posma G. Normal values for pharyngeal pH monitoring. Ann Otol Rhinol Laryngol. 2009;188:166–171. doi: 10.1177/000348940911800302. [DOI] [PubMed] [Google Scholar]
- 34.Sun G, Muddana S, Slaughter J, et al. A new pH catheter for laryngopharyngeal reflux: Normal values. Laryngoscope. 2009;119:1639–1643. doi: 10.1002/lary.20282. [DOI] [PubMed] [Google Scholar]
- 35.Williams R, Ali G, Wallace K. Esophagopharyngeal acid regurgitation: Dual pH monitoring criteria for its detection and insights into mechanisms. Gastroenterology. 1999;117 doi: 10.1016/s0016-5085(99)70389-6. [DOI] [PubMed] [Google Scholar]
- 36.Golub J, Johns M, Lim J, DelGaudio J, Klein A. Comparison of an oropharyngeal pH probe and a standard dual pH probe for diagnosis of laryngopharyngeal reflux. Ann Otol Rhinol Laryngol. 2009;188:1–5. doi: 10.1177/000348940911800101. [DOI] [PubMed] [Google Scholar]
- 37.Wiener G, Koufman J, Wu W. Chronic hoarseness secondary to gastroesophageal reflux disease: Documentation with 24-h ambulatory pH monitoring. Am J Gastroenterol. 1989;84:1503–1508. al e. [PubMed] [Google Scholar]