Abstract
Over the last two decades, lymphoma idiotype vaccines have been the first human cancer vaccines to show striking evidence of biological and clinical efficacy on the one hand, as well as clinical benefit on the other. More recently, however, three large-scale, independent, randomized clinical trials on idiotypic vaccination have failed to achieve their main clinical endpoints for reasons likely to depend more on flaws in each clinical trial’s study design than on each vaccination strategy per se. Independently of these considerations, a major hurdle for the development of this substantially innocuous and yet potentially very effective type of treatment has been the fact that, even to date, no factors ascertainable before vaccination have been prospectively singled out as predictors of subsequently vaccine-induced, idiotype-specific immune as well as clinical responses. The aim of this review article is precisely to analyze what has been and what could be done in this respect in order to give a greater chance of success to future trials aimed at regulatory approval of idiotype vaccines.
Keywords: Clinical outcome, Clinical trial, Idiotype, Immune response, Lymphoma, Vaccine
THE IDIOTYPE
The term idiotype refers to the entire collection of antigenic determinants called idiotopes, which are displayed on an individual immunoglobulin molecule. Idiotopes can be found solely in the hypervariable regions of the immunoglobulin variable domain, are somatically generated and are recognized as foreign because the limited amount of them normally present in an individual is intrinsically insufficient to elicit the activation of any self-tolerance mechanism[1]. Although it seems plausible that most immunologically relevant idiotopes should structurally encompass, completely or in part, the complementarity-determining regions of the immunoglobulin’s variable regions[2], it is important to stress that the two terms are not synonymous, insofar as the former are involved in the definition of the antigenic properties of the immunoglobulin, while the latter take part in the definition of its specificity as an antibody (Figure 1). In this respect, idiotopes are more thoroughly classified in two categories, that is, public and private idiotopes. The former are largely derived from the immunoglobulin’s framework region sequences, whereas the latter mostly arise from the unique immunoglobulin’s complementarity-determining region sequences. The implications of this different localization are extremely important, particularly when we consider the whole immunoglobulin no longer in functional terms, that is as an antibody, but rather as an immunological target itself, that is as a collection of antigens in the context of a cancer vaccine-induced, anti-idiotypic immune activation. In particular, only humoral responses against the private idiotopes will have value for tumor suppression, since other antibodies, if at all raised, will be absorbed by the serum immunoglobulins. Similarly, only private idiotopes will ultimately function as a collection of clonal markers for each tumor[3]. Since each immunoglobulin features its own idiotype and identical idiotypes define identical immunoglobulins, the clonal idiotype of a B-cell malignancy can serve as a complete, tumor-specific antigen for vaccine therapy, as long as the tumor cells express it intact as their functional B-cell receptor on the cell membrane and in the form of idiotopes associated with the HLA molecules for epitope presentation[4].
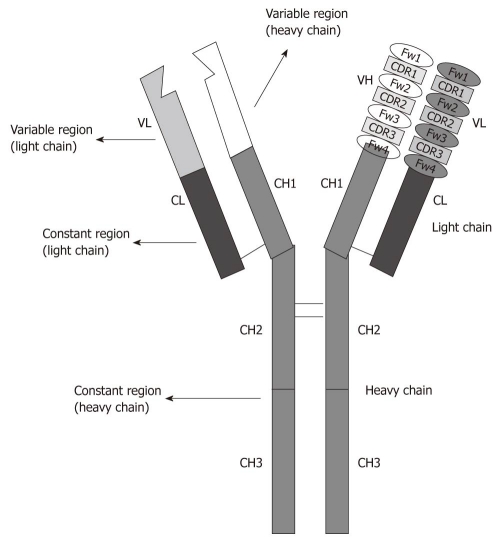
Figure 1.
Schematic representation of a monomeric immunoglobulin. Idiotopes are scattered throughout the heavy and light chains’ variable regions. Fw: Framework region; CDR: Complementarity-determining region.
IDIOTYPE PRODUCTION METHODS
Although a number of different procedures are currently employed to reproduce the clonal, patient- and tumor-specific idiotype in the lab, most of them are based on one of the following general methods: large scale culture of hybridomas, recombinant technology and DNA vaccines. While this last option aims at generating a vaccine based on the idiotype-encoding DNA sequence, and has so far found little application in human clinical trials[5], the first two methods aim at reproducing the soluble protein idiotype, which is subsequently integrated in the vaccine formulation, as has been the case in several phase-I, -II and -III clinical studies[6]. It goes without saying that DNA vaccines imply the generation of the idiotype by the patient himself, as some of his somatic cells are transfected through the administration of the DNA sequences encoding only for the idiotype. In contrast, the ultimate product of hybridoma methodology or recombinant technology applications is a whole, idiotype-containing immunoglobulin. Given the specific topic of this review, only studies conducted with soluble protein, whole-immunoglobulin idiotype vaccines will be analyzed, as no clinical trial on idiotype DNA vaccines or on soluble idiotype fragments would allow any conclusions to be drawn on the role of potential factors predicting the induction of specific immune responses because of the very limited number of patients enrolled[7,8].
Most, if not all idiotype vaccine-related achievements in terms of proofs of principle have been achieved using idiotype-containing, clonal immunoglobulins obtained through hybridoma-based methodology[9,10]. Among the growing hybridomas, one is ultimately selected according to a number of morphological, genetic, immunological and quantitative features. In particular, this hybridoma should grow relatively rapidly, possess an idiotype molecular fingerprint fully overlapping with that of the corresponding tumor cell[11], and also secrete a sufficient amount of the tumor-specific immunoglobulin to guarantee enough material for all vaccine doses, as well as for the post-vaccine immunological tests[12]. It is intuitive that this methodology, as valuable as it has been from a scientific point of view, can often be time-consuming, logistically demanding, and overall very expensive[6].
A viable methodological alternative to hybridomas is represented by recombinant technology aiming at a molecular rescue of the idiotype, which involves polymerase chain reaction-based amplification and cloning of the genes encoding for the tumor-specific immunoglobulin variable regions, followed by their ligation into plasmid or viral vectors for protein expression in mammalian (e.g. murine lymphoma), insect (e.g. sf9), bacterial (e.g. Escherichia coli) or plant (e.g. tobacco) cells[13]. Depending on the specific method utilized, the ultimate recombinant, custom-made idiotype can still be embedded into a full-length tetrameric immunoglobulin in which a common heavy chain backbone may consist of either a human IgG3 or IgG1 scaffold. All in all, it is important to note that when hybridoma methodology is employed, the whole immunoglobulin obtained is virtually identical, at least in terms of amino acid sequence, to that featured by the original tumor, while when recombinant technology is utilized this can be said only for the idiotype itself, as the heavy chains differ quite substantially.
THE MAIN IDIOTYPE VACCINE FORMULATION
Independently of the method used to reproduce the tumor-specific, soluble protein idiotype in the lab, the most widely used vaccine formulations employ chemical conjugation with the powerful immunogenic carrier keyhole Limpet Hemocyanin (KLH)[14]. The function of this molecule is indeed that of enhancing idiotype immunogenicity, which despite the specificity of the private idiotope collection remains substantially low. Furthermore, clinical grade granulocyte-monocyte colony-stimulating factor (GM-CSF) is used as an immunologic adjuvant to be added to the ultimate vaccine formulation[15]. The typical dose of both idiotype and KLH has been 0.5 mg of each per vaccination since the inception of the use of this experimental approach in humans[16], while the dose of GM-CSF has ranged from 100 to 500 mcg per vaccination in different clinical trials, but with no evidence of substantially different outcome among them[17]. So far, the most impressive clinical results with idiotypic vaccination have been obtained in patients with follicular lymphoma[18]. However, given the peculiar focus of this review, some inferences will also be made based on the sole idiotype vaccine clinical trial ever conducted in patients with mantle cell lymphoma[19].
POTENTIAL FACTORS PREDICTING RESPONSE TO IDIOTYPIC VACCINATION
In principle, potential factors predicting whether idiotypic vaccination may induce clinically-relevant immune responses could independently depend on several biological aspects involving each patient per se, the type of lymphoma, the tumor-specific immunoglobulin as a whole, each idiotype, the pre-vaccine treatment administered to patients, the number of vaccine doses administered and the duration of the vaccination program in which patients are enrolled. Moreover, it has to be underlined that any of these factors which may be retrospectively singled out from closed clinical trials should also undergo further subsequent verification in a prospective manner, as it is not unusual that the latter ends up disproving the validity of the former’s conclusions. Finally, it has to be borne in mind that each patient’s tumor-specific idiotype is a weak antigen that normally does not elicit any immune response in the autologous setting.
Factors directly related to the patient himself or herself may play a role before, during and even after the vaccine administration program takes place. For instance, age could be a crucial factor insofar as elderly patients may feature a lymphoma-harboring immune system that is per se weaker than that of younger patients, or might become weaker due to the pre-vaccine therapy. Yet, no study has ever focused on ascertaining whether an age threshold might or should be established, above which vaccination may be meaningless and even detrimental to the success of clinical trials, particularly in follicular lymphoma[20], a disease affecting and recruiting in clinical trials many elderly patients. Another factor depending on each patient and virtually impossible to both assess and chart is his or her immune function status at the time of each vaccination, as most if not all clinical trials allow postponing vaccine dose administration by 1 wk or so in case of concomitant disease (e.g. bacterial or viral infections), but it is not known whether either the acute illness or the vaccination schedule modification might affect idiotype vaccine effectiveness.
The type of lymphoma may also affect idiotype vaccine efficacy, although too few attempts other than against follicular lymphoma have been made to draw firm conclusions. For instance, it is possible that small lymphocytic lymphoma, with its lower expression of tumor surface immunoglobulin than that of other B-cell malignancies, may be less amenable to this vaccination strategy. It suffices to say that, in principle, any B-cell lymphoma[21] whose cells express a full immunoglobulin on their surface may potentially benefit from the otherwise innocuous[22] idiotypic vaccination. However, further studies would be required to convert this speculation into a factual statement, particularly in relapsed/refractory large B-cell as well as in mantle cell lymphoma.
A recent report[23], not yet fully published, has focused on the idiotype-containing, whole tumor immunoglobulin as the source of a potentially very important factor predicting the ultimate clinical outcome of patients undergoing idiotypic vaccination, that is the original heavy chain isotype of the immunoglobulin. In particular, as discussed in depth below, retrospective data from an incomplete randomized clinical trial seem to indicate that follicular lymphoma patients, whose tumors featured an idiotype-containing IgM, experienced a better post-vaccine clinical outcome than their peers whose tumor featured an idiotype-containing IgG. However, it has to be remembered that similar results originated from retrospective studies, namely those focusing on the prognostic role played by different Fc γ receptor genotypes featured by follicular lymphoma immunoglobulins (Table 1) on the outcome of patients receiving idiotypic vaccination[24,25] have previously generated the same understandable excitement, but were not confirmed in subsequent prospective trials[26].
Table 1.
Relevance of potential factors predicting idiotype vaccine-induced clinical outcome in major clinical trials
| No. of patients | Comparison | Type of study | Results | Ref. |
| 136 | FcγRIIIa 158 | Retrospective analysis | Better outcome for V/V | [24,25] |
| 289 | FcγRIIIa 158 | Prospective analysis | No outcome difference | [38] |
| 117 | Idiotype/Isotype | Retrospective analysis | Better outcome for IgM | [23] |
FcγRIIIa: Fc γ receptor IIIa; V/V: Valine/valine.
Being a weak antigen, each tumor-specific idiotype may also be more or less prone to function as a valuable vaccine core product. Moreover, depending on the type of lymphoma, each idiotype may or may not contain acquired potential glycosylation sites[27], which are indeed present in most, if not all, cases of follicular lymphoma[28,29] but may be lacking in many cases of the other B-cell malignancies still expressing a tumor-specific immunoglobulin on the surface of the tumor clone[30]. It goes without saying that, when present, these acquired potential glycosylation sites may or may not actually be glycosylated on the original tumor cell, and when they are, it is virtually impossible that the idiotype contained in the vaccine formulation, however obtained in the lab, will feature the same glycosylation pattern. In fact, no matter the idiotype production method utilized, the glycosylation machinery involved is not derived from human cells, but rather from other mammalian, insect, or plant cells[18]. Whether all these features depending on each single idiotype and on its production technique, if thoroughly studied, may ultimately allow researchers to predict which idiotype vaccine could and could not be employed in patient after patient for clinically-successful immunization remains to be determined.
As briefly mentioned above, the overall idiotype vaccine formulation utilized in most large clinical trials has remained unchanged over the years. The only component that has been subjected to substantial dose changes is the adjuvant, that is, GM-CSF. However, even when employed within the same trial[17] at different doses, such differences have not emerged as a potential factor predicting better or worse clinical and immunological outcomes.
Pre-vaccine treatment and its enhancing or detrimental role towards successful immunization by means of idiotype vaccines has been the subject of much speculation, but no trial has actually been conducted to confirm and quantify, for instance, the alleged negative role of pre-vaccine rituximab, which causes a complete and relatively long-lasting normal B-cell depletion, and is thought to prevent the immune system from fully or partly responding to idiotypic vaccination[20]. Similarly, it is thought to be desirable that patients receiving pre-vaccine chemotherapy should be allowed to recover, at least from a quantitative standpoint, their normal immune function status[26]. Yet, most past trials have been designed to include a pre-determined duration of the off-therapy period between the end of chemotherapy and the administration of the first idiotype vaccine dose[6]. Therefore, it is not known whether patients who responded to vaccination from an immunological and clinical response may have simply been those with a fully recovered immune function before vaccination start, or whether this is a detail of no importance.
Finally, another potential factor predicting the clinical outcome of patients undergoing idiotypic vaccination might be the length of the vaccination program. However, no clinical trial has ever been designed to assess whether prolonged idiotypic vaccination is intrinsically more or less efficacious than a program relying on the administration of only a few vaccine doses. In the former case, this could be theoretically true either because some patients start responding to the vaccine later than others[22] or because long-term boost may prevent the loss of the immune response elicited against the tumor-specific idiotype. In the latter scenario, this might be hypothesized as the result of a potential induction of immunologic tolerance against the same weak antigen through an extended vaccination schedule[22].
MAJOR CLINICAL TRIALS AND POTENTIAL RESPONSE PREDICTING FACTORS
Over the last decade, four independent clinical trials have attempted to formally prove the clinical benefit of idiotypic vaccination: a phase-II, non-randomized proof-of-principle study not aimed at regulatory approval, which achieved its main clinical endpoint, and three large-scale, phase-III randomized studies (Table 2) designed to achieve such a goal, although, as predicted well before their conclusion[31], they ultimately failed to achieve their main clinical endpoint[6]. All these studies have been designed based on the assumption that a vaccine-induced, idiotype-specific immune response is crucial to improve disease-free survival in lymphoma patients. However, it is still theoretically possible that the simple capacity of responding to an idiotype vaccine is sufficient to achieve that clinical goal, irrespective of whether the elicited immune response is idiotype-specific or not[32]. Moreover, the only way to formally prove that the idiotype specificity of a vaccine-induced immune response is the key to an improved clinical outcome would consist of randomizing lymphoma patients to receive either their own, tumor-specific idiotype vaccine or a control vaccine formulation containing an irrelevant idiotype produced in the same way[6].
Table 2.
Overview of randomized clinical trials addressing the clinical benefit of idiotypic vaccination in patients with follicular lymphoma
| Pre-treatment | Pre-vax status | Random | Endpoint | Results | Ref. |
| 6-8 × PACE q 3w | CR | 2:01 | DFS | Better outcome if vaccinated | [34,35] |
| 8 × CVP q 3w | CR, PR | 2:01 | PFS | No difference | [38] |
| 4 × rituximab q 1w | CR, PR, SD | 1:01 | TTP | No difference | [39] |
PACE: Cyclophosphamide, doxorubicin, etoposide and prednisone; q 3w: 1 cycle every 3 wk; CR: Complete response; DFS: Disease-free survival; CVP: Cyclophosphamide, vincristine, prednisone; PR: Partial response; PFS: Progression-free survival; q 1w: 1 dose weekly; SD: Stable disease; TTP: Time to progression.
The first study reported the outcome of 25 patients with follicular lymphoma after induction of a second complete response with standard chemotherapy without rituximab and subsequent extensive idiotypic vaccination[26]. In this case, the tumor-specific idiotype was reproduced in the lab through hybridoma methodology. A vaccine-induced, humoral and/or cellular, idiotype- and/or tumor-specific immune response was elicited in 20/25 patients. The median duration of the second complete response among these patients was statistically significantly longer than the median duration of their first complete response. Moreover, in all cases it was also conspicuously longer than 13 mo, which is the unchanged median duration of a second complete response induced by standard chemotherapy without rituximab over the last three decades. On the contrary, the five patients who did not respond to vaccination from an immunological standpoint had a second complete response shorter than both 13 mo and their first complete response. All these findings, both combined and in isolation, were unprecedented in follicular lymphoma treatment[33], and even in a non-randomized context, clearly proved for the first time the clinical benefit associated with the use of a human therapeutic cancer vaccine[32]. Besides allowing vaccine administration only to patients in second complete clinical response after uniform salvage chemotherapy not including rituximab, this study’s design prevented initiation of vaccination until a documented quantitative recovery of each patient’s immune status was documented in terms of normal numbers of circulating CD19-, CD3-, CD4- and CD8-positive cells, independently of the time required to achieve such recovery in each case. However, given the single-arm nature of the study, it is not possible to conclude whether this detail may in the future predict or explain a greater chance of favorable immune and clinical outcome.
The only phase-III, randomized clinical trial based on hybridoma-rescued idiotype vaccines was launched at the National Cancer Institute 10 years ago[34]. Based on a previous phase-II study[17] that had succeeded in proving clinical efficacy[6] of idiotypic vaccination in patients with follicular lymphoma, this trial was also designed to provide actual immunizations with the idiotype vaccine or the control only to patients achieving a clinical complete response following pre-vaccine chemotherapy. However, the cyclophosphamide, doxorubicin, etoposide and prednisone (PACE) regimen was not widely used for follicular lymphoma treatment even before the advent of rituximab, and as soon as it became evident that the addition of rituximab to any chemotherapy regimen dramatically improved response rates in follicular lymphoma patients[20], the absence of this monoclonal antibody in the pre-vaccine treatment schema made patient enrollment in this trial virtually unethical. In any case, while the study was open, it randomized newly-diagnosed follicular lymphoma patients achieving chemotherapy-induced first complete response to receive the vaccine formulation either with or without the customized, tumor-specific idiotype component. While waiting for the full report of this largely incomplete trial to be published, it is worth underlining that this study has shown for the second time evidence of clinical benefit associated with the administration of the bona fide customized vaccine. In particular, only one hundred and seventeen patients have received either vaccine formulation instead of the three hundred and seventy-five patients that were supposed to be effectively randomized[35]. Moreover, the statistically significant (P = 0.045) advantage in disease-free survival achieved by the patients receiving the bona fide vaccine (44.2 mo vs 30.6 mo for the control arm) falls decisively short of the threshold (P < 0.01) originally stipulated by the company with the Food and Drug Administration as the main clinical endpoint for regulatory approval[6].
In this study, patients were vaccinated after post-chemotherapy off therapy of preset duration. Therefore, it is not clear whether the immune status of each patient at the time of vaccination was somehow assessed. However, as briefly mentioned above, an unexpected, retrospective finding has been preliminarily reported from this study[23]. Of the seventy-six patients actually receiving their bona fide idiotype vaccine, thirty-six featured an IgM, while forty featured an IgG tumor immunoglobulin isotype. Of the forty-one patients in the control arm, twenty-five featured an IgM, while fifteen featured an IgG tumor immunoglobulin isotype and one had a mixed IgM/IgG isotype. No difference in disease-free survival was observed when comparing vaccinated and control patients whose tumor idiotype displayed an IgG. The IgM subgroup of patients receiving the bona fide vaccine fared significantly better than those in the control arm (median time to relapse: 50.6 mo vs 27.1 mo, P = 0.002). All these subgroups of patients presented with numbers too small, and the study design ensured that this statistical difference could be confirmed in a prospective, randomized study adequately powered to address this issue. Of course, it will be important to assess the existence or lack of possible correlation between tumor-associated immunoglobulin isotype on the one hand, and both outcome results and specific immune responses elicited by vaccination on the other. Similarly, it could be of interest to retrospectively try to confirm or disproof these findings in all concluded, large-scale trials featuring a common pre-vaccine treatment for all enrolled patients. In any case, should this outcome difference between patients with idiotype-bearing IgM or IgG isotype be confirmed in more sizeable studies, hybridoma-derived idiotype vaccines may once again regain scientific supremacy over recombinant idiotype vaccines, even if patients with an IgG-borne tumor-specific idiotype are excluded from vaccination protocols. In fact, nowadays the production of recombinant idiotype vaccines reproduces an idiotype systematically mounted on a shared IgG scaffold, and this might be seen as detrimental with respect to the ultimate idiotype immunogenicity.
As mentioned above, previous studies have tentatively singled out factors that seemed to predict, with the confidence derived from highly statistically significant differences in clinical outcome, which patients are more likely to respond to idiotypic vaccination[24,25]. However, no confirmatory evidence has subsequently emerged from prospective trials meant to put such preliminary findings to the test. In particular, the extensive experience in idiotypic vaccination at Stanford University[36,37] had led to the retrospective conclusion that immunoglobulin G Fc receptor (FcγR) polymorphisms might accurately predict the clinical response of lymphoma patients to idiotypic vaccination. In particular, in a group of 136 patients, it was found that those with FcγRIIIa 158 valine/valine (V/V) genotype had a longer progression-free survival [16] than those with valine/phenylalanine (V/F) or phenylalanine/phenylalanine (F/F) genotypes (V/V, 8.21 years vs V/F, 3.38 years, P = 0.004; V/V 8.21 years vs F/F, 4.47 years, P = 0.035). When the researchers analyzed whether such a statistically significant correlation could be related to the pre-vaccine response to chemotherapy[36], they also found that in patients with pre-vaccine complete response, the 5-year progression-free survival was 69% for those with a subsequent idiotype-specific humoral response and/or V/V genotype, but only 40% for patients with neither. The median time to progression was 10.47 years vs 3.46 years (P = 0.012). In patients with pre-vaccine, chemotherapy-induced partial response, the 5-year progression-free survival was 57% for patients with the specific humoral response and/or V/V genotype, but only 17% for patients with neither. The median time to progression had not been reached in the former vs 1.31 years (P = 0.001) in the latter group.
However, these strong and consistent retrospective results were not prospectively confirmed by the same scientists in their large, randomized, phase-III clinical trials employing a recombinant idiotype vaccine[37]. Even more disappointingly, this study showed no statistically significant differences in progression-free survival between vaccinated patients and those in the control arm, possibly because vaccination was administered not only to patients who had achieved a pre-vaccine, chemotherapy-induced complete response, but also to those with pre-vaccine, post-chemotherapy partial response.
Finally, another independent study based on a novel recombinant idiotype vaccine also failed to show statistically significant differences in time to progression between vaccinated patients and those in the control arm[38]. As rituximab had meanwhile become part of the standard of care for patients with follicular lymphoma, the goal of this trial was to assess whether idiotypic vaccination could further improve survival of follicular lymphoma patients solely pre-treated with four weekly doses of rituximab. As such, most patients were ultimately vaccinated with both active disease and severe B-cell depletion, and this potentially double-negative status at the time of vaccination is likely to have influenced the disappointing outcome of the trial far more than the quality of the recombinant vaccine per se[6]. In particular, patients in the control arm seemed to have experienced a statistically significant better outcome than those in the experimental arm, a difference that disappeared when standard follicular lymphoma prognostic factors were retrospectively applied to both groups and factored in the analysis[38].
As inferred above, despite lacking comparative data to make a stronger case, the use of rituximab without allowing conspicuous B-cell recovery prior to initiation of idiotypic vaccination is likely to diminish and perhaps even abolish the likelihood of a vaccine-induced, idiotype-specific immune response. We do not know for sure whether idiotype specificity is crucial for the vaccine to exert a clinical effect, but it seems quite established that patients with no vaccine-induced immune response at all are less likely to experience any clinical benefit[26]. In a study of idiotypic vaccination for patients with mantle cell lymphoma, it was concluded that pre-vaccine chemo-immunotherapy containing rituximab delays humoral responses, but does not affect cellular responses[19]. However, it should be underlined that the delayed humoral responses observed in that study were all directed against the highly-immunogenic carrier 14] contained in the vaccine formulation, not against the idiotype, which is a far weaker and yet the sole vaccine formulation antigen that matters[39].
CONCLUSION
There are many questions still unanswered regarding idiotypic vaccination. We do not know whether there may be substantial outcome differences when using the whole immunoglobulin or the sole Fab[7], when reproducing the idiotype through hybridoma or recombinant methodology, when vaccinating newly-diagnosed or relapsed patients, when treating patients with follicular or other types of lymphoma. Similarly, many potentially crucial details concerning this immunotherapeutic approach remain to be determined, such as the number of doses, the pre-vaccine treatment, and the type of indispensable immune response that it should be induced via vaccination. Finally, it is now paramount to verify whether patients with IgM- and IgG-borne idiotypes undergoing vaccination have indeed a critically different outcome, particularly taking into account that, outside of idiotype vaccine trials, most standard diagnostic protocols for surface immunoglobulin-positive B-cell lymphomas do not include a routine determination of the immunoglobulin isotype.
All in all, the quest for one or more reliable factors both assessable prior to starting the production of an idiotype vaccine and capable of predicting its clinical usefulness remains a crucial element in the continuing development of this active immunotherapy strategy. It is desirable that new trials, including those currently ongoing and based on recombinant idiotype vaccines produced in tobacco plants[40,41], are able to close the current knowledge gap in this field.
Footnotes
Peer reviewer: Charles H Lawrie, DPhil, University Research Lecturer, PI, Lymphoid Malignancy Research Group, Nuffield Department of Clinical Laboratory Sciences, University of Oxford, Rm 4834, Level 4, John Radcliffe Hospital, Oxford, OX3 9DU, United Kingdom
S- Editor Tian L L- Editor Webster JR E- Editor Zheng XM
References
- 1.Bendandi M. Role of anti-idiotype vaccines in the modern treatment of human follicular lymphoma. Expert Rev Anticancer Ther. 2001;1:65–72. doi: 10.1586/14737140.1.1.65. [DOI] [PubMed] [Google Scholar]
- 2.Baskar S, Kobrin CB, Kwak LW. Autologous lymphoma vaccines induce human T cell responses against multiple, unique epitopes. J Clin Invest. 2004;113:1498–1510. doi: 10.1172/JCI20312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McCarthy H, Ottensmeier CH, Hamblin TJ, Stevenson FK. Anti-idiotype vaccines. Br J Haematol. 2003;123:770–781. doi: 10.1046/j.1365-2141.2003.04698.x. [DOI] [PubMed] [Google Scholar]
- 4.Bendandi M. The role of idiotype vaccines in the treatment of human B-cell malignancies. Expert Rev Vaccines. 2004;3:163–170. doi: 10.1586/14760584.3.2.163. [DOI] [PubMed] [Google Scholar]
- 5.Stevenson FK, Ottensmeier CH, Rice J. DNA vaccines against cancer come of age. Curr Opin Immunol. 2010;22:264–270. doi: 10.1016/j.coi.2010.01.019. [DOI] [PubMed] [Google Scholar]
- 6.Bendandi M. Idiotype vaccines for lymphoma: proof-of-principles and clinical trial failures. Nat Rev Cancer. 2009;9:675–681. doi: 10.1038/nrc2717. [DOI] [PubMed] [Google Scholar]
- 7.Navarrete MA, Heining-Mikesch K, Schüler F, Bertinetti-Lapatki C, Ihorst G, Keppler-Hafkemeyer A, Dölken G, Veelken H. Upfront immunization with autologous recombinant idiotype Fab fragment without prior cytoreduction in indolent B-cell lymphoma. Blood. 2011;117:1483–1491. doi: 10.1182/blood-2010-06-292342. [DOI] [PubMed] [Google Scholar]
- 8.Rice J, Ottensmeier CH, Stevenson FK. DNA vaccines: precision tools for activating effective immunity against cancer. Nat Rev Cancer. 2008;8:108–120. doi: 10.1038/nrc2326. [DOI] [PubMed] [Google Scholar]
- 9.Carroll WL, Thielemans K, Dilley J, Levy R. Mouse x human heterohybridomas as fusion partners with human B cell tumors. J Immunol Methods. 1986;89:61–72. doi: 10.1016/0022-1759(86)90032-3. [DOI] [PubMed] [Google Scholar]
- 10.Rodríguez-Calvillo M, Inogés S, López-Díaz de Cerio A, Zabalegui N, Villanueva H, Bendandi M. Variations in "rescuability" of immunoglobulin molecules from different forms of human lymphoma: implications for anti-idiotype vaccine development. Crit Rev Oncol Hematol. 2004;52:1–7. doi: 10.1016/j.critrevonc.2004.05.002. [DOI] [PubMed] [Google Scholar]
- 11.Bendandi M, Tonelli R, Maffei R, Botti S, Turi C, Sartini R, Inogés S, Calvillo MR, Zinzani PL, Pession A, et al. Identification of the B-cell tumor-specific molecular fingerprint using non-radiolabelled PCR consensus primers. Ann Oncol. 2001;12:1479–1484. doi: 10.1023/a:1012586905273. [DOI] [PubMed] [Google Scholar]
- 12.Bendandi M. Anti-idiotype vaccines for human follicular lymphoma. Leukemia. 2000;14:1333–1339. doi: 10.1038/sj.leu.2401861. [DOI] [PubMed] [Google Scholar]
- 13.Park HJ, Neelapu SS. Developing idiotype vaccines for lymphoma: from preclinical studies to phase III clinical trials. Br J Haematol. 2008;142:179–191. doi: 10.1111/j.1365-2141.2008.07143.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harris JR, Markl J. Keyhole limpet hemocyanin: molecular structure of a potent marine immunoactivator. A review. Eur Urol. 2000;37 Suppl 3:24–33. doi: 10.1159/000052389. [DOI] [PubMed] [Google Scholar]
- 15.Kwak LW, Young HA, Pennington RW, Weeks SD. Vaccination with syngeneic, lymphoma-derived immunoglobulin idiotype combined with granulocyte/macrophage colony-stimulating factor primes mice for a protective T-cell response. Proc Natl Acad Sci U S A. 1996;93:10972–10977. doi: 10.1073/pnas.93.20.10972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kwak LW, Campbell MJ, Czerwinski DK, Hart S, Miller RA, Levy R. Induction of immune responses in patients with B-cell lymphoma against the surface-immunoglobulin idiotype expressed by their tumors. N Engl J Med. 1992;327:1209–1215. doi: 10.1056/NEJM199210223271705. [DOI] [PubMed] [Google Scholar]
- 17.Bendandi M, Gocke CD, Kobrin CB, Benko FA, Sternas LA, Pennington R, Watson TM, Reynolds CW, Gause BL, Duffey PL, et al. Complete molecular remissions induced by patient-specific vaccination plus granulocyte-monocyte colony-stimulating factor against lymphoma. Nat Med. 1999;5:1171–1177. doi: 10.1038/13928. [DOI] [PubMed] [Google Scholar]
- 18.de Cerio AL, Zabalegui N, Rodríguez-Calvillo M, Inogés S, Bendandi M. Anti-idiotype antibodies in cancer treatment. Oncogene. 2007;26:3594–3602. doi: 10.1038/sj.onc.1210371. [DOI] [PubMed] [Google Scholar]
- 19.Neelapu SS, Kwak LW, Kobrin CB, Reynolds CW, Janik JE, Dunleavy K, White T, Harvey L, Pennington R, Stetler-Stevenson M, et al. Vaccine-induced tumor-specific immunity despite severe B-cell depletion in mantle cell lymphoma. Nat Med. 2005;11:986–991. doi: 10.1038/nm1290. [DOI] [PubMed] [Google Scholar]
- 20.Bendandi M. Aiming at a curative strategy for follicular lymphoma. CA Cancer J Clin. 2008;58:305–317. doi: 10.3322/CA.2008.0011. [DOI] [PubMed] [Google Scholar]
- 21.Inogés S, Rodríguez-Calvillo M, López-Díaz de Cerio A, Zabalegui N, Pérez-Calvo J, Panizo C, Hernandez M, Cuesta B, Rocha E, Bendandi M. Feasibility of idiotype vaccination in relapsed B-cell malignancies. Haematologica. 2003;88:1438–1440. [PubMed] [Google Scholar]
- 22.Inoges S, Lopez-Diaz de Cerio A, Zabalegui N, Soria E, Villanueva H, Panizo C, Rodriguez-Caballero A, Suarez L, Pastor F, Rodriguez-Calvillo M, et al. Prolonged idiotypic vaccination against follicular lymphoma. Leuk Lymphoma. 2009;50:47–53. doi: 10.1080/10428190802601122. [DOI] [PubMed] [Google Scholar]
- 23.Schuster SJ, Santos CF, Neelapu SS, Berry DA, Popa MA, McCord AM, Chong EA, Kwak L. Vaccination with IgM but not IgG idiotype prolongs remission duration in follicular lymphoma patients. Blood. 2010;116:429A. [Google Scholar]
- 24.Weng WK, Czerwinski D, Timmerman J, Hsu FJ, Levy R. Clinical outcome of lymphoma patients after idiotype vaccination is correlated with humoral immune response and immunoglobulin G Fc receptor genotype. J Clin Oncol. 2004;22:4717–4724. doi: 10.1200/JCO.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 25.Weng WK, Czerwinski D, Levy R. Humoral immune response and immunoglobulin G Fc receptor genotype are associated with better clinical outcome following idiotype vaccination in follicular lymphoma patients regardless of their response to induction chemotherapy. Blood. 2007;109:951–953. doi: 10.1182/blood-2006-03-013136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Inogès S, Rodrìguez-Calvillo M, Zabalegui N, Lòpez-Dìaz de Cerio A, Villanueva H, Soria E, Suárez L, Rodríguez-Caballero A, Pastor F, García-Muñóz R, et al. Clinical benefit associated with idiotypic vaccination in patients with follicular lymphoma. J Natl Cancer Inst. 2006;98:1292–1301. doi: 10.1093/jnci/djj358. [DOI] [PubMed] [Google Scholar]
- 27.Coelho V, Krysov S, Ghaemmaghami AM, Emara M, Potter KN, Johnson P, Packham G, Martinez-Pomares L, Stevenson FK. Glycosylation of surface Ig creates a functional bridge between human follicular lymphoma and microenvironmental lectins. Proc Natl Acad Sci U S A. 2010;107:18587–18592. doi: 10.1073/pnas.1009388107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhu D, McCarthy H, Ottensmeier CH, Johnson P, Hamblin TJ, Stevenson FK. Acquisition of potential N-glycosylation sites in the immunoglobulin variable region by somatic mutation is a distinctive feature of follicular lymphoma. Blood. 2002;99:2562–2568. doi: 10.1182/blood.v99.7.2562. [DOI] [PubMed] [Google Scholar]
- 29.Radcliffe CM, Arnold JN, Suter DM, Wormald MR, Harvey DJ, Royle L, Mimura Y, Kimura Y, Sim RB, Inogès S, et al. Human follicular lymphoma cells contain oligomannose glycans in the antigen-binding site of the B-cell receptor. J Biol Chem. 2007;282:7405–7415. doi: 10.1074/jbc.M602690200. [DOI] [PubMed] [Google Scholar]
- 30.Zabalegui N, de Cerio AL, Inogés S, Rodríguez-Calvillo M, Pérez-Calvo J, Hernández M, García-Foncillas J, Martín-Algarra S, Rocha E, Bendandi M. Acquired potential N-glycosylation sites within the tumor-specific immunoglobulin heavy chains of B-cell malignancies. Haematologica. 2004;89:541–546. [PubMed] [Google Scholar]
- 31.Bendandi M. Clinical benefit of idiotype vaccines: too many trials for a clever demonstration? Rev Recent Clin Trials. 2006;1:67–74. doi: 10.2174/157488706775246120. [DOI] [PubMed] [Google Scholar]
- 32.Longo DL. Idiotype vaccination in follicular lymphoma: knocking on the doorway to cure. J Natl Cancer Inst. 2006;98:1263–1265. doi: 10.1093/jnci/djj371. [DOI] [PubMed] [Google Scholar]
- 33.Johnson PW, Rohatiner AZ, Whelan JS, Price CG, Love S, Lim J, Matthews J, Norton AJ, Amess JA, Lister TA. Patterns of survival in patients with recurrent follicular lymphoma: a 20-year study from a single center. J Clin Oncol. 1995;13:140–147. doi: 10.1200/JCO.1995.13.1.140. [DOI] [PubMed] [Google Scholar]
- 34.Neelapu SS, Gause BL, Nikcevich DA, Schuster SJ, Winter J, Gockerman JP, Loughran T, Takeshita K, Inghirami G, McGaughey D, et al. Phase III randomized trial of patient-specific vaccination for previously untreated patients with follicular lymphoma in first complete remission: protocol summary and interim report. Clin Lymphoma. 2005;6:61–64. doi: 10.3816/clm.2005.n.031. [DOI] [PubMed] [Google Scholar]
- 35.Schuster SJ, Neelapu SS, Gause BL, Muggia FM, Gockerman JP, Sotomayor EM, Winter JN, Flowers CR, Stergiou AM, Kwak LW. Idiotype vaccine therapy (BiovaxID) in follicular lymphoma in first complete remission: Phase III clinical trial results. J Clin Oncol. 2009;27:2A. [Google Scholar]
- 36.Hsu FJ, Caspar CB, Czerwinski D, Kwak LW, Liles TM, Syrengelas A, Taidi-Laskowski B, Levy R. Tumor-specific idiotype vaccines in the treatment of patients with B-cell lymphoma--long-term results of a clinical trial. Blood. 1997;89:3129–3135. [PubMed] [Google Scholar]
- 37.Levy R, Robertson MJ, Ganjoo K, Leonard JP, Vose J, Denney D. Results of a Phase 3 trial evaluating safety and efficacy of specific immunotherapy, recombinant idiotype (Id) conjugated to KLH (Id-KLH) with GM-CSF, compared to non-specific immunotherapy, KLH with GM-CSF, in patients with follicular non-Hodgkin’s lymphoma (fNHL); Proceedings of the 99th Annual Meeting of the American Association for Cancer Research; 2008 Apr 12-16; San Diego, CA. Philadelphia (PA): AACR; 2008. Abstract LB-204. [Google Scholar]
- 38.Freedman A, Neelapu SS, Nichols C, Robertson MJ, Djulbegovic B, Winter JN, Bender JF, Gold DP, Ghalie RG, Stewart ME, et al. Placebo-controlled phase III trial of patient-specific immunotherapy with mitumprotimut-T and granulocyte-macrophage colony-stimulating factor after rituximab in patients with follicular lymphoma. J Clin Oncol. 2009;27:3036–3043. doi: 10.1200/JCO.2008.19.8903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Inoges S, de Cerio AL, Soria E, Villanueva H, Pastor F, Bendandi M. Idiotype vaccines for human B-cell malignancies. Curr Pharm Des. 2010;16:300–307. doi: 10.2174/138161210790170111. [DOI] [PubMed] [Google Scholar]
- 40.McCormick AA, Reddy S, Reinl SJ, Cameron TI, Czerwinkski DK, Vojdani F, Hanley KM, Garger SJ, White EL, Novak J, et al. Plant-produced idiotype vaccines for the treatment of non-Hodgkin's lymphoma: safety and immunogenicity in a phase I clinical study. Proc Natl Acad Sci U S A. 2008;105:10131–10136. doi: 10.1073/pnas.0803636105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bendandi M, Marillonnet S, Kandzia R, Thieme F, Nickstadt A, Herz S, Fröde R, Inogés S, Lòpez-Dìaz de Cerio A, Soria E, et al. Rapid, high-yield production in plants of individualized idiotype vaccines for non-Hodgkin's lymphoma. Ann Oncol. 2010;21:2420–2427. doi: 10.1093/annonc/mdq256. [DOI] [PubMed] [Google Scholar]