Abstract
The prevalence of osteoporosis in India is high and osteoporotic fractures are thought to occur early in Indian women. The aim was to study the prevalence of osteopenia and osteoporosis in women aged above 40 years. Women aged above 40 years attending the out patient department of this hospital were offered bone densitometry. A significant positive correlation was found between age and time since menopause and bone mineral density (BMD). Differences in the prevalence of osteoporosis were noted on the basis of socioeconomic strata. There was no statistically significant difference observed in BMD for many of the other accepted risk factors such as age at menarche, lactation, and exercise.
Keywords: Bone mineral density, DEXA, osteopenia, osteoporosis
INTRODUCTION
One of the most rapidly emerging global health problems in postmenopausal women is osteoporosis. In India, osteoporosis is highly prevalent, with an estimated 30 million women diagnosed to have osteoporosis.[1] Studies suggest that Indians have lower bone density than their North American and European counterparts and that osteoporotic fractures occur 10-20 years earlier in Indians.
The aim of our study was to assess bone mineral density (BMD) in women above 40 years of age and to study the prevalence of osteopenia and osteoporosis in pre- and postmenopausal women. We also wanted to study the risk factors leading to osteopenia and osteoporosis.
MATERIALS AND METHODS
This was a cross-sectional study. Women aged 40 years and above attending OPD from January 1, 2008 to December 31, 2008 were offered bone densitometry. Those with established osteoporosis and on medication, which decreases bone density, were excluded from the study. The participants were 105 women, aged 40 years and above who attended the out patient clinic. A standardized proforma was filled which included age, dietary history, drugs and smoking, age at menarche, breast-feeding and duration, and age at menopause.
The BMD of the lumbar spine was measured by Dual-energy X-ray absorptiometry (DEXA) technique using Lunar DPX-PRO densitometers. Vertebral measurements were noted at L2-L4 level .The results of BMD were expressed as T score as defined by WHO. Fisher's exact test was applied to calculate the statistical significance. Upon detection of osteopenia or osteoporosis, patients were referred for treatment.
RESULTS
Out of 105 subjects studied, osteopenia was found in 31.4% subjects and osteoporosis in 14.3% subjects.
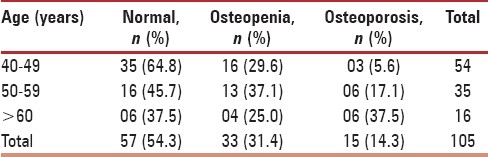
Age
Increasing age was found to be an important risk factor for osteoporosis. This difference in the older age group was statistically significant (P = 0.016) [Table 1].
Table 1.
Age and BMD
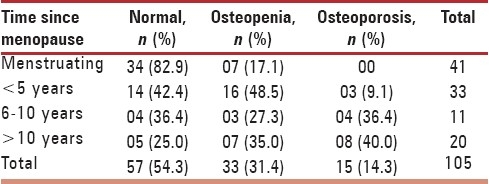
Time Since Menopause
After the menopause, the incidence of both osteopenia and osteoporosis rose significantly and the time since menopause was found to be a major risk factor in this regard. Statistically, time since menopause was a significant risk factor for osteoporosis at the lumbar spine. (P = 0.00) [Table 2].
Table 2.
Time since menopause and BMD
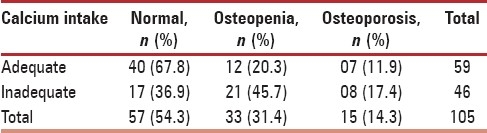
Calcium Intake
Adequate calcium intake was found to have a significant positive impact on BMD. These findings were found to be statistically significant (P = 0.006) [Table 3].
Table 3.
Calcium intake and BMD
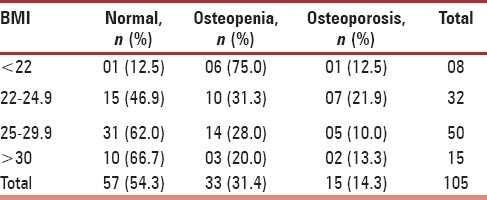
BMI
BMD was higher in obese women, but the difference between this group and those with normal BMI did not achieve statistical significance (P = 0.075) [Table 4].
Table 4.
BMI and BMD
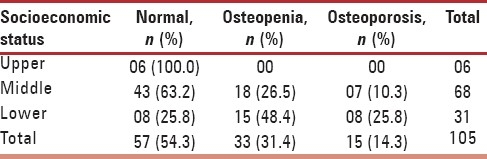
Socioeconomic Status
Women from the lower socioeconomic strata had a significantly higher percentage of osteopenia and osteoporosis (P = 0.001) [Table 5].
Table 5.
Socioeconomic status and BMD
Age at Menarche, Lactation, and Exercise
They were not found to be statistically significant as risk factors for osteoporosis (P > 0.05).
DISCUSSION
Prior to this study, retrospective data (from February 2006 to December 2007) on BMD was collected on 983 women in the age group of 40-70 years coming for routine health check. The subjects came from middle and upper-middle class families.[2]
As per the WHO classification, 23.2% of our study subjects had osteoporosis and 40% had osteopenia. The percentage of women with T scoreless than -2.5 was highest in the seventh decade. There was a rapid fall in BMD from the fifth to sixth decade, and the bone loss reduced in the seventh decade.[2] Thus, osteoporosis and osteopenia are a major concern even in middle and upper-middle class Indian women.
This spurred our interest, and we decided to undertake this prospective study to look for the prevalence of osteopenia and osteoporosis and to identify risk factors for the same on the basis of BMD measurements in women aged 40 years and above.
The mean age of this study group was 50.46 ± 7.60 years, with the age ranging from 40 to 72 years. In the women of the 40-49 year age group, only 5.6% had osteoporosis at the spine as against 37.5% in the age group more than 60 years. In concordance with this study, Gandhi and Shukla[3] in their study of women aged 40 years and above, found that out of 200 women, 34% had osteopenia and 8% had osteoporosis. Out of the osteoporotic women, 31.25% were in the age group 46-50 years and 25% in the age group of 51-55 years. Of the osteopenic women, 51.47% were still menstruating and so were 31.25% of the osteoporosis. In women above 60 years, there was an almost 100% incidence of either osteopenia or osteoporosis.
Similarly, Larijani et al.[4] compared BMD in different age decades in women and found that spinal BMD in age group 40-49, 50-59, and 60-69 years, was lower by 3%, 1%, and 4% than previous age decades, respectively.
From available studies and the findings of this study, it is evident that as age advances, so does the incidence of osteopenia and osteoporosis. It is interesting to note in this study that there is a large incidence of osteopenia in the 40-49 years age group, which indicates that there may be a role for using preventive measures in the third decade of life rather than waiting for osteoporosis to develop in the fourth and fifth decade of life.
In this study, the mean age at menarche of the study group was 13.21 years. In 43 women with late menarche, 48.8% had normal BMD at the spine and 16.3% had osteoporosis. In contrast, Cury et al.[5] suggested that late menarche (after 16 years) increased the risk of osteoporosis by twofold. In 999 women aged between 50 and 96 years, it was found that in women with early menarche (8-12 years), 28.9% had osteoporosis and in women with late menarche (16-21 years), 46.0% had osteoporosis.
Robbins et al.[6] studied the osteoporotic fracture rate in postmenopausal women, and the results of their study are comparable to ours. They found that out of 1132 women with osteoporotic fractures, 17.6% had early menarche (<12 years) and 27.9% had late menarche (>14 years).
Literature suggests that early menarche is associated with higher bone mass, because of early release of estrogen and exposure of bones to estrogen for more number of years. However, in this study, the prevalence of osteoporosis was not significantly associated with age at menarche (P = 0.0673). This could be due to small numbers as only two subjects with early menarche were present for statistical comparison.
Increasing time since menopause was a risk factor for osteoporosis, and this was statistically significant in our study. A similar relation between time since menopause and BMD was found by Finkelstein et al.[7] on 3302 women, where it was found that BMD loss accelerates substantially in the late perimenopause and continues at a similar pace in the first few postmenopausal years. The rates of loss from the spine were 0.022 per year, respectively (P < 0.001).
This has been corroborated by several other authors. Therefore, there appears to be a definitive association between the time since menopause and osteoporosis.
The findings of this study are concordant with other studies and strongly support the role of calcium intake in the diet on BMD. Adequate calcium intake also reduces the incidence of osteoporosis.
Duration of lactation did not have any significant impact on the prevalence of osteoporosis in our women. However, in contrast Gur et al.[8] found that the bone density is adversely affected by a long period of breast feeding. A prospective study by Laskey et al.[9] in 1999 found that the lactation associated decrease in bone mineral mass was temporary and reversed when breast feeding declined and stopped.
The mean BMI of the study group was 26.7. The findings of this study show an inverse relationship between BMI and BMD. With increasing BMI, the number of women with normal BMD score also increased. However, statistically, BMI as a risk factor was not found to be significant this study (Spine P = 0.075). This may be due to the small sample size in this study.
Acha et al.[10] studied the relationship between BMI and hip fracture in 2653 individuals of 65 years or older which comprised of 57.9% females and found that individuals who were underweight were at greater risk for hip fracture and higher BMI was associated with lower risk of fracture. They found that each one-unit increase in BMI was associated with 9% decreased risk of hip fracture.
In this study, in women who exercised regularly the BMD was normal in 72.4% as against 40% among those who did not exercise. Different levels of exercise did not have any statistically significant impact on the prevalence of osteopenia and osteoporosis.
Lee et al.[11] found that total and regional BMD did not correlate with physical fitness level. They studied 107 premenopausal and 71 postmenopausal women with 35.7% of the first group and 46.5% of the second group performing minimum 30 min of exercise daily and found that the mean BMD of the first group (1.27 g/cm2) was higher than the second group (1.10 g/cm2).
Majority of studies carried out on exercise and its effect on BMD have not shown any relation between BMD and exercise in the postmenopausal age. However, literature suggests that exercise may have a significant impact on BMD at the age when peak bone mass is attained. This was shown by Boot on 500 children and adolescents aged 4-20 years.
The majority of women were from the middle class and most of them were highly literate and employed. The results from this study suggest that women from lower socioeconomic status were at higher risk of osteoporosis. The findings were statistically significant (P = 0.001). Good nutrition and healthy lifestyle in the upper classes as compared to the lower socioeconomic strata probably accounts for their higher bone density.
Gur et al.[8] categorized 569 postmenopausal women into four groups in relation to educational level. They found that at the spine and the femur BMD was significantly lower in women who were illiterate, as compared to the highest BMD in women with education up to postgraduate level. They explained the mechanism of association between education and osteoporosis on the basis of socioeconomic status, which acts as a good predictor for educational level.
CONCLUSION
In this study, findings suggest a significant positive correlation between age and time since menopause and BMD. Differences in the prevalence of osteoporosis exist on the basis of socioeconomic strata. The study highlights the protective role played by calcium intake. The results of this study did not reveal a statistically significant difference in BMD for many of the other accepted risk factors such as age at menarche, lactation, and exercise. It appears that more studies with larger numbers may need to be carried out to establish their role.
The International Osteoporosis Foundation suggests screening of women after age of 65 years. However, changing life style in young people (dieting, smoking, and lack of exercise) has made them vulnerable to osteoporosis at an earlier age. Further in India, there is a higher prevalence of other risk factors such as low socioeconomic strata, low calcium in the diet, Vitamin D deficiency, low education level, premature menopause, multiparity, and extended lactation, putting women at higher risk for osteopenia and osteoporosis.
It is recommended that adolescents (i.e., at the time of formation of peak bone mass) should consume a diet-rich in calcium. Sun light exposure for Vitamin D absorption and exercise should also be encouraged. These measures are efficacious, safe, and cost-effective. Osteoporosis is associated with high morbidity and mortality. However, preventive measures can be instituted with early identification and diagnosis. Pharmacological interventions are expensive and should, therefore, be targeted to only those at high risk of fractures.
As evident in this study, osteopenia is already present in women between 40 and 49 years, so measurement of BMD from the age of 40 years will help in diagnosis at an early stage. Early diagnosis in such women will prevent the morbidity and mortality due to osteoporosis by facilitating interventions such as calcium and Vitamin D supplementation and the use of antiresorptive agents.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Shah RS, Savardekar LS. Symposium, Forum 9. Mumbai India: 2005. Post menopausal osteoporosis in India: Growing public health concern; pp. 12–6. [Google Scholar]
- 2.Unni J, Kadam N, Chiplonkar S, Khadilkar A. Bone mineral density at the lumbar spine in Indian women: Unpublished Data: Presented at the 12th World Congress on Menopause, Madrid, Spain. [Google Scholar]
- 3.Gandhi A, Shukla A. Evaluation of BMD of women above 40 years of age. J Obstet Gynaecol India. 2005;55:265–7. [Google Scholar]
- 4.Larijani B, Hossein-Nezhad A, Mojtahedi A, Pajouhi M, Bastanhagh MH, Soltani A, et al. Normative data of bone mineral density in healthy population of Tehran, Iran: A Cross sectional study. BMC Musculoskelet Disord. 2005;6:38. doi: 10.1186/1471-2474-6-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cury AF, Zacchello KP. Osteoporosis: Prevalence and risk factors among > 49 year-old women in private practice environment. Acta Ortop Bras. 2007;15:146–50. [Google Scholar]
- 6.Robbins J, Aragaki AK, Kooperberg C, Watts N, Wactawski-Wende J, Jackson RD, et al. Factors associated with 5-year risk of hip fracture in postmenopausal women. JAMA. 2007;298:2389–98. doi: 10.1001/jama.298.20.2389. [DOI] [PubMed] [Google Scholar]
- 7.Finkelstein JS, Brockwell SE, Mehta V, Greendale GA, Sowers MR, Ettinger B, et al. Bone mineral density changes during the menopause transition in a multiethnic cohort of women. J Clin Endocrinol Metab. 2008;93:861–8. doi: 10.1210/jc.2007-1876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gur A, Sarac AJ, Nas K, Cevik R. The relationship between educational level and bone mineral density in postmenopausal women. BMC Fam Pract. 2004;5:18. doi: 10.1186/1471-2296-5-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Laskey MA, Prentice A. Bone mineral changes during and after lactation. Obstet Gynecol. 1999;94:608–15. doi: 10.1016/s0029-7844(99)00369-5. [DOI] [PubMed] [Google Scholar]
- 10.Acha AA, Ostir GV, Markides KS, Ottenbacher KJ. Cognitive status, body mass index and hip fracture in hispanic older adults. J Am Geriatr Soc. 2006;54:1251–5. doi: 10.1111/j.1532-5415.2006.00820.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee JS, Kawakubo K, Sato H, Kobaayashi Y, Haruna Y. Relationship between total and regional bone mineral density and menopausal state, body composition and life style factors in overweight Japanese women. Int J Obes Relat Metab Disord. 2001;25:880–6. doi: 10.1038/sj.ijo.0801620. [DOI] [PubMed] [Google Scholar]


