Abstract
Objective:
To determine the prevalence of premenstrual cyclic symptoms in perimenopausal age.
Subjects and Methods:
Women attending Bhavan's SPARC Maitreyi's Health Care Programme (HCP) for women around 40 years of age were included in the study. Last 200 women who attended from April 2002 to October 2004 are included for analysis. Out of these 107 qualified for final analysis as others were post hysterectomy or post menopausal. Thirty five symptoms listed under premenstrual tension syndrome were analysed.
Results:
Forty one women (38.3%) had 3 or more symptoms whilst 15 (14.0%) had 5 or more cyclic symptoms. Five women (4.7%) reported that the symptoms were severe. Eleven women had seeked treatment for premenstrual tension syndrome (PMTS). The commonest symptom was mastalgia or heaviness of breasts. Next was whilst also was reported by several women. Women reported anger attacks and reported depression.
Conclusion:
PMTS was common between 36 and 55 years. About half of them have experienced 3 more symptoms and 1 in 20 may require treatment.
Keywords: Premenstrual tension, perimenopause, premenstrual tension syndrome
INTRODUCTION
Women require special need-based health care programs as they pass through the menopausal transition. With this vision, a multisystem multispecialty health check-up and follow-up care program (Maitreyi health care program [HCP]) was initiated by our team about a decade ago, and this has been continued at the Medical Research Center, Kasturba Health Society, Mumbai. More than a thousand women have benefited from this program. The comparative effects of three plant products on perimenopausal symptoms, quality of life (QOL) and clinical biochemistry have been reported by our group earlier.[1,2] Our observation of frequent mood changes and sleep disturbances in women in the premenopausal group prompted us to undertake a study of cyclic symptoms in Maitreyi HCP.[3] In this communication, we describe the preliminary findings from the analysis of premenstrual symptoms in 200 consecutive women who underwent a comprehensive check-up in the Maitreyi HCP.
Diagnosis of premenstrual tension syndrome (PMTS) is based on the following criteria as per the American Association of Obstetricians and Gynecologists[4] :
A 30% increase in the intensity of symptoms of premenstrual syndrome (measured using a standardized instrument) from cycle days 5–10 as compared with the 6-day interval before the onset of menses and documentation of these changes for at least two consecutive cycles.
At least one of the following affective and somatic symptoms during the 5 days before menses in previous cycles. Affective symptoms: depression, angry outbursts, irritability, anxiety, confusion, social withdrawal. Somatic symptoms: breast tenderness, abdominal bloating, headache, swelling of extremities; symptoms relieved from days 4 through 13 of the menstrual cycle.
Objective
To determine the prevalence of premenstrual cyclic symptoms in women who attended the Maitreyi HCP.
METHODS
Maitreyi's HCP for women above 35 includes comprehensive health questionnaire, gynecological and physician's check-up, biochemical investigations of complete blood count, glucose tolerance test, lipid profile, liver functions, serum creatinine and serum thyroid stimulating hormone. Pap smear, pelvic sonography and urine and stool examination for occult blood are also included. A multidisciplinary trans-system team offers this community-oriented programme to women with voluntary services by the consultants. Bone mineral density and mammography are advised as per the age and risk factors. This analysis is a preliminary report restricted to the premenstrual cyclic symptomatolgy in 200 consecutive women who attended this program over 2½ years.
A special case record form has been used and a detailed medical and surgical history is included in the same. Posthysterectomy and postmenopausal cases were excluded from analysis. One hundred and seven women qualified for the analysis. Twelve women who continued to menstruate beyond 50, up to 55 years, have been included in the analysis. Only those who had symptoms at least during two consecutive cycles or more were included in the analysis.
The American Society of Obstetricians and Gynecologists and the American Psychiatric Society have now brought out the consensus criteria for inclusion of the condition in PMTS or Premenstrual Dysphoric Disorder (PMDD), the latter usually requiring treatment for neuropsychiatric symptoms. Accordingly, PMTS is said to be present when the woman reports three or more of the following symptoms in two cycles or more[4–6]:
There are 36 symptoms as listed below in the SF-36 mental component.[7] In the present analysis, the symptoms were classified as per the Medical Outcomes Study Short Form-36 for assessment of premenstrual symptoms, and the presence of three of these occurring over two or more cycles was labelled as PMTS:
Anxiety, irritability, depression, tension, mood swings, loss of self-control, difficulty in concentration, insomnia, confusion, headache, crying attacks, fatigue, aches, breast tenderness, cramps, bloatedness, food craving, visual disturbances, tiredness, fatigue, puffiness of the face, weight gain, altered libido, aggression, nausea, vomiting, acne, skin rashes, constipation, diarrhea, joint stiffness, backache, abdominal cramps/pain, anger attacks, aggravation of epilepsy, aggravation of asthma.
RESULTS
Of 107 women, 26 (24.3%) did not report any premenstrual symptoms at all and 81 (75.7%) reported at least one symptom [Table 1].
Table 1.
Number of symptoms experienced by women in different age groups in two or more cycles
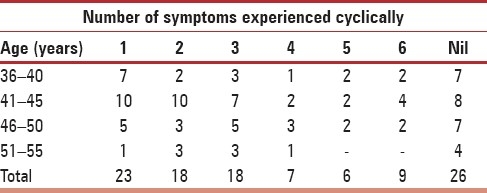
Maximum frequency was seen in women from 35 to 50 years of age. Older women did not have as many symptoms.
Forty women (37.4%) who reported premenstrual symptoms had three or more cyclic symptoms for more than two cycles and could be classified as those with PMTS. Fifteen (14%) had five or more symptoms cyclically in at least two cycles. Almost 10% reported five or more symptoms inclusive of anger attacks and could be labelled as PMDD.
An analysis of most frequent symptoms was also made. Mastalgia was the most common symptom (50.5%), followed by mood changes (46.7%), depression (7.5%) and anger attacks (6.5%). PMDD was present in 10% of the cases who were referred to a clinical psychologist or a psychiatrist.
DISCUSSION
Many women have premenstrual cyclic symptoms of psychological or physical nature and, sometimes, these limit their functional capacity. The symptoms due to neurohormonal imbalance or ageing may start as early as 35 years of age. PMTS is an entity that causes considerable morbidity, and in about 3% of the women, it may disrupt the woman's life when severe symptoms recur. When there are severe symptoms like anger attacks, depression and suicidal thoughts, special attention including psychiatric consultation may be required, i.e. the PMDD. The prevalence of PMTS in general is about 2–10% for disabling symptoms, while minor symptoms may be present in up to 85% of the women.[4–6,8] In the present series, 75.7% reported at least one symptom cyclically.
In the present series, a high prevalence of PMTS and PMDD was observed in premenopausal women. Halbreich has reported that in about 20% of the women, the symptoms are severe enough to warrant treatment.[5] Dean et al. have reported a prevalence of 19–30% when all women from 18 to 45 years of age were screened.[6] Freeman et al. reported that PMTS is common in younger women with many children.[8] In a recent survey of 3,913 women of 15-54 years of age, Tschudin et al. observed that about 10% reported PMTS and 3.1% reported PMDD. The prevalence was higher in women older than 35 years.[9]
When the Indian scenario is considered, Chaturvedi et al. in the 1990s have reported a prevalence of 20% in a general population and severe symptoms in 8%.[10] The same authors have, in a later study, reported suicidal ideas and/or death wish during the premenstrual period in 10% of the subjects, more so among college students and industrial working women as compared with housewives.[11] Banerjee et al., in a group of 62 women, reported PMDD in 6.4%.[12]
There is a close association between mood disorders and the sleep rhythm and disturbances in sleep pattern in premenopausal age.[3–13,14]
Management Strategies
Many women and their physicians regard PMTS as a physiological phenomenon and do not think treatment is necessary. However, it does affect QOL in some and it is therefore essential to identify which women will benefit from lifestyle management and which will require pharmacological intervention. Those who want to reach their full functional potential and who find that the symptoms are hampering their progress or interfering with normal daily routine should be certainly offered safe pharmacological interventions provided that they come for routine follow-ups. Because there are many etiological factors that have been described as probably causative, and multiple causes may be present in an individual woman, there is a wide variety of treatment options and combinations depending on specific symptoms and their severity. The postulated causes range from hormonal imbalances like progesterone deficiency, prolactin excess, thyroid hypofunction, fluctuation in circulating level of estrogen; electrolyte disturbances like rennin-angiotensin alterations, antidiuretic hormone excess, decreased colloidosmotic pressure; neurotransmitter disturbances with serotonin or gamma-amino-butyric-acid, or β-endorphin activity alternations, serotonin metabolism alternations or prostaglandin imbalance; cytokine imbalances like excess of interleukin (IL)-6, IL-1 β and tumor necrosis factor (TNF)-α; nutritional deficiencies like vitamin B or vitamin D deficiency; lack of exercise or psychosocial disturbances.[8–10,13–15] The treatment therefore will depend on the particular symptom complex in the individual woman.[16,17] In concordance with other authors, we have also observed PMTS in cases with subclinical hypothyroidism.[18] Thyroid replacement therapy is usually simple to follow. Lifestyle measures like regular exercise, balanced nutritious diet and regular hours of sleep will benefit all, and may be adequate for some.[19–21] For others, pharmacological interventions may be helpful if required.
The therapy is multipronged and has to be individualized. While simple measures like the institution of physical exercises, relaxation techniques like yoga and vitamin and mineral supplements are adequate for most women,[19–24] some require hormonal therapy with combined oral contraceptives or regulation of fluid and electrolytes. As a matter of fact, combined oral contraceptives are used frequently in the more severe cases and, drosperidone, containing newer combinations, is relatively free from side-effects.[16,17,25] Selective estrogen modulators, including nonsteroidal agents like centchroman, also could be useful, particularly in women with contraindications to hormones.[26] Group sessions with psychologists also have shown benefit. Few women need psychiatric consultation and will benefit from antidepressants, particularly sertraline or fluoxetine, while some respond to prolactin inhibitors like bromocriptine or cabergoline.[27,28]
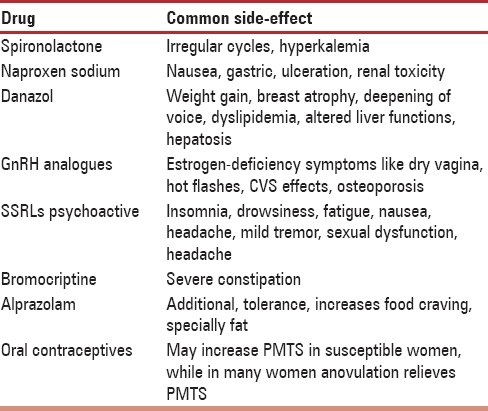
Complementary and alternative therapies like soy, Hypericum perforatum and Gingko biloba have a definite role to play.[24,29–31] Evening Primrose oil does not have significant efficacy.[32] We have observed relief of mild to moderate premenstrual symptoms with soy, Gycyrrhiza glabra and Withania somnifera.[1,2] We have also observed complete relief of PMTS in two women treated with an extract rich in Saraca asoka, prescribed for menorrhagia, which was also controlled.[33] There is need for more research in this area because commonly used drugs may have side-effects that may prevent regular long-term use [Table 2].
Table 2.
Common side-effects of existing pharmacologic therapies for PMTS
Effect on Work and QOL
Recently, two well-designed studies have shown that PMTS leads to loss of work hours and economic losses, and does not allow women to reach their full potential.[34–36]
Effective and safe therapy is indicated. It is also important to bear in mind that other chronic diseases like migraine or depression or irritable bowel syndrome could be exaggerated during the premenstrual phase, and a multidisciplinary team should evaluate and manage such cases.[36,37]
CONCLUSION
PMTS is a common condition sometimes precipitated by stress. There are multiple etiological factors and a number of options are available for treatment. It is very important to ensure that the first option is nonpharmacological as many women may respond to it. Pharmacotherapy can be added in recalcitrant cases and must be individualized as per the woman. Great care should be taken to avoid side-effects and drug interactions because multiple therapies may be used. Medicinal plants may be a safe alternative in some women. Because PMTS could be a predictor for menopausal syndrome, it will be useful to warn women with PMTS and their families of a flare up or the need for long-term follow-up. Freeman et al. and Arpel et al. have reported PMTS to be predictive of menopausal syndrome in a long-term follow-up study and have shown the association of hormonal imbalance with depressive symptoms in women.[8,38]
Acknowledgments
We are thankful to Dr. Rama Vaidya, Dean, MRC-KHS, Dr. Deepak Dave, Director, Clinical Research and Dr. A.B. Vaidya, Research Director, Medical Research Center - Kasturba Health Society, Vile Parle, Mumbai, for their continued guidance during the Maitreyi program. We are also thankful to the Kasturba Health Society, Sewagram, Wardha, for infrastructural support.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Pandey SN, Vaidya RA, Joshi JV, Agashe S, Chandrashekhar S, Nagral KI, Vaidya AB. The role of phytoalternatives in treating vasomotor symptoms of menopause. Indian Drugs. 2006;42:1–8. [Google Scholar]
- 2.Pandey SN, Vaidya AB, Vaidya RA, Joshi JV, Agashe S, Chandrashekhar S, et al. Evaluation of antioxidant and lipid modulating effect of Soy isoflavones and root powder of Glycyrrhiza glabra Linn in peri-/ postmenopausal women. Indian Drugs. 2006;43:130–5. [Google Scholar]
- 3.Vaidya RA, Pandey SN, Vaidya V, Shringi MS, Vaidya AD. Sleep disorders at menopause and beyond.An Emergent Challenge. IMS Newsl. 2003;5:1–17. [Google Scholar]
- 4.Practice Bulletin No 15. Washington DC: 2000. Apr, American College of Obstetricians and Gynecologists. Premenstrual Syndrome. [Google Scholar]
- 5.Halbreich U, Borenstein J, Pearlstein T, Kahn LS. The prevalence, impairment, impact and burden of premenstrual dysphoric disorder (PMS/ PMDD) Psychoneuroendocrinology. 2003;28:1–23. doi: 10.1016/s0306-4530(03)00098-2. [DOI] [PubMed] [Google Scholar]
- 6.Dean BB, Borenstein JE, Knight K, Yonkers K. Evaluating the criteria used for identification of PMS. Womens Health (Larchmt) 2006;15:546–55. doi: 10.1089/jwh.2006.15.546. [DOI] [PubMed] [Google Scholar]
- 7.Ware JE, Snow KK, Kosisnki M, Gandek B. SF-36 Health Survey Manual and Interpretation Guide. Boston: The Health Institute; 1993. [Google Scholar]
- 8.Freeman EW, Sammel MD, Lin H, Nelson DB. Associations of hormones and menopausal status with depressed mood in women with no history of depression. Arch Gen Psychiatry. 2006;63:375. doi: 10.1001/archpsyc.63.4.375. [DOI] [PubMed] [Google Scholar]
- 9.Tschudin S, Bertea PC, Zemp E. Prevalence and predictors of premenstrual syndrome and premenstrual dysphoric disorder in a population-based sample. Arch Womens Ment Health. 2010 doi: 10.1007/s00737-010-0165-3. [DOI] [PubMed] [Google Scholar]
- 10.Chaturvedi SK, Chandra PS, Issac MK, Sudarshan CY, Beena MB, Sarmukkadam SB, et al. Premenstrual experiences: the four profiles and factorial patterns. J Psychosom Obstet Gynaecol. 1993;14:223–35. doi: 10.3109/01674829309084444. [DOI] [PubMed] [Google Scholar]
- 11.Chaturvedi SK, Chandra PS, Gururaj G, Pandian RD, Beena MB. Suicidal ideas during premenstrual phase. J Affect Disord. 1995;34:193–9. doi: 10.1016/0165-0327(95)00017-h. [DOI] [PubMed] [Google Scholar]
- 12.Banerjee N, Roy KK, Takkar D. Premenstrual dysphoric disorder-a study from India. Int J Fertil Womens Med. 2000;45:342–4. [PubMed] [Google Scholar]
- 13.Maguire J, Mody I. Steroid hormone fluctuations and GABA(A)R plasticity. Psychoneuroendocrinology. 2009;34:S84–90. doi: 10.1016/j.psyneuen.2009.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Baker FC, Colrain IM. Daytime sleepiness, psychomotor performance, waking EEG spectra and evoked potentials in women with severe premenstrual syndrome. J Sleep Res. 2010;19:214–27. doi: 10.1111/j.1365-2869.2009.00782.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Scully P, McKernan DP, Keohane J, Groeger D, Shanahan F, Dinan TG, et al. Plasma cytokine profiles in females with irritable bowel syndrome and extra-intestinal co-morbidity. Am J Gastroenterol. 2010 doi: 10.1038/ajg.2010.159. [DOI] [PubMed] [Google Scholar]
- 16.Rapkin A. A review of treatment of premenstrual syndrome and premenstrual dysphoric disorder. Psychoneuroendocrinology. 2003;28:39–53. doi: 10.1016/s0306-4530(03)00096-9. [DOI] [PubMed] [Google Scholar]
- 17.Jarvis CI, Lynch AM, Morin AK. Management strategies for premenstrual syndrome/premenstrual dysphoric disorder. Ann Pharmacother. 2008;42:967–78. doi: 10.1345/aph.1K673. [DOI] [PubMed] [Google Scholar]
- 18.Shringi MS, Galvankar P, Vaidya RA, Sankari K, Bhatt M, Joshi B, et al. Therapeutic profile of an Ayurvedic formulation Ashotone-® in DUB. Indian Pract. 1999;53:193–8. [Google Scholar]
- 19.Daley A. Exercise and premenstrual symptomatology: a comprehensive review. J Womens Health (Larchmt) 2009;18:895–9. doi: 10.1089/jwh.2008.1098. [DOI] [PubMed] [Google Scholar]
- 20.Dvivedi J, Kaur H, Dvivedi S. Effect of 1 week ‘61-points relaxation training’ on cold pressor test induced stress in premenstrual syndrome. Indian J Physiol Pharmacol. 2008;52:262–6. [PubMed] [Google Scholar]
- 21.Lustyk MK, Gerrish WG, Shaver S, Keys SL. Cognitive-behavioral therapy for premenstrual syndrome and premenstrual dysphoric disorder: a systematic review. Arch Womens Ment Health. 2009;12:85–96. doi: 10.1007/s00737-009-0052-y. [DOI] [PubMed] [Google Scholar]
- 22.Whelan AM, Jurgens TM, Naylor H. Herbs, vitamins and minerals in the treatment of premenstrual syndrome: a systematic review. Can J Clin Pharmacol. 2009;16:e407–29. [PubMed] [Google Scholar]
- 23.Bertone-Johnson ER, Chocano-Bedoya PO, Zagarins SE, Micka AE, Ronnenberg AG. Dietary vitamin D intake, 25-hydroxyvitamin D(3) levels and premenstrual syndrome in a college-aged population. J Steroid Biochem Mol Biol. 2010;121:434–7. doi: 10.1016/j.jsbmb.2010.03.076. [DOI] [PubMed] [Google Scholar]
- 24.Nagata C, Hirokawa K, Shimizu N, Shimizu H. Soy, fat and other dietary factors in relation to premenstrual symptoms in Japanese women. BJOG. 2004;111:594–9. doi: 10.1111/j.1471-0528.2004.00130.x. [DOI] [PubMed] [Google Scholar]
- 25.Lopez LM, Kaptein A, Helmerhorst FM. Oral contraceptives containing drospirenone for premenstrual syndrome. Cochrane Database Syst Rev. 2008;1:CD006586. doi: 10.1002/14651858.CD006586.pub2. [DOI] [PubMed] [Google Scholar]
- 26.Joshi JV, Vaidya RA. Selective Estrogen Receptor Modulators. In: Daftary SN, Desai SV, editors. Obstetrics and Gynaecology for Postgraduates and Practitioners. New Delhi: BI Publications; 2009. pp. 195–209. [Google Scholar]
- 27.Brown J, O’ Brien PM, Marjoribanks J, Wyatt K. Selective serotonin reuptake inhibitors for premenstrual syndrome. Cochrane Database Syst Rev. 2009;2:CD001396. doi: 10.1002/14651858.CD001396.pub2. [DOI] [PubMed] [Google Scholar]
- 28.Aydin Y, Atis A, Kaleli S, Uludağ S, Goker N. Cabergoline versus bromocriptine for symptomatic treatment of premenstrual mastalgia: A randomised, open-label study. Eur J Obstet Gynecol Reprod Biol. 2010;150:203–6. doi: 10.1016/j.ejogrb.2010.02.024. [DOI] [PubMed] [Google Scholar]
- 29.van Die MD, Bone KM, Burger HG, Reece JE, Teede HJ. Effects of a combination of Hypericum perforatum and Vitex agnus-castus on PMS-like symptoms in late-perimenopausal women: findings from a subpopulation analysis. J Altern Complement Med. 2009;15:1045–8. doi: 10.1089/acm.2008.0539. [DOI] [PubMed] [Google Scholar]
- 30.Canning S, Waterman M, Orsi N, Ayres J, Simpson N, Dye L. The efficacy of Hypericum perforatum (St John's wort) for the treatment of premenstrual syndrome: a randomized, double-blind, placebo-controlled trial. CNS Drugs. 2010;24:207–25. doi: 10.2165/11530120-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 31.Ozgoli G, Selselei EA, Mojab F, Majd HA. A randomized, placebo-controlled trial of Ginkgo biloba L.in treatment of premenstrual syndrome. J Altern Complement Med. 2009;15:845–51. doi: 10.1089/acm.2008.0493. [DOI] [PubMed] [Google Scholar]
- 32.Bayles B, Usatine R. Evening primrose oil. Am Fam Physician. 2009;80:1405–8. [PubMed] [Google Scholar]
- 33.Shringi MS, Galvankar P, Vaidya Ra, Sankari K, Bhatt M, Joshi B, Joshi JV, et al. Therapeutic profile of an Ayurvedic formulation Ashotone-® in DUB. Indian Pract. 1999;53:193–8. [Google Scholar]
- 34.Borenstein JE, Dean BB, Leifke E, Korner P, Yonkers KA. Differences in symptom scores and health outcomes in premenstrual syndrome. J Womens Health (Larchmt) 2007;16:1139–44. doi: 10.1089/jwh.2006.0230. [DOI] [PubMed] [Google Scholar]
- 35.Heinemann LA, Minh TD, Filonenko A, Uhl-Hochgräber K. Explorative evaluation of the impact of severe premenstrual disorders on work absenteeism and productivity. Womens Health Issues. 2010;20:58–65. doi: 10.1016/j.whi.2009.09.005. [DOI] [PubMed] [Google Scholar]
- 36.Yang M, Wallenstein G, Hagan M, Guo A, Chang J, Kornstein S. Burden of premenstrual dysphoric disorder on health-related quality of life. J Womens Health (Larchmt) 2008;17:113–21. doi: 10.1089/jwh.2007.0417. [DOI] [PubMed] [Google Scholar]
- 37.Pinkerton JV, Guico-Pabia CJ, Taylor HS. Menstrual cycle-related exacerbation of disease. Am J Obstet Gynecol. 2010;202:221–31. doi: 10.1016/j.ajog.2009.07.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Arpels JC. The female brain hypoestrogenic continuum from the premenstrual syndrome to menopause.A hypothesis and review of supporting data. J Reprod Med. 1996;41:633–9. [PubMed] [Google Scholar]


