Abstract
Background and Objectives:
Neuraxial anesthesia in the elderly is associated with exaggerated responses to conventional doses of local anesthetics, thereby increasing the incidence of hemodynamic complications. A double-blind prospective study was carried out in our institute with an aim to compare the hemodynamic stability and quality of the conventional dose of hyperbaric bupivacaine (LA) with low dose of LA and sufentanil in elderly patients scheduled for lower limb surgery, randomized to receive combined spinal epidural anesthesia.
Methods:
A total of 50 elderly patients of ASA grade I and II, divided randomly into groups I and II, of either sex undergoing lower limb surgery under combined spinal epidural anesthesia at our institute attached to a Government Medical College were enrolled for study. Group I received 2.5 ml of intrathecal hyperbaric bupivacaine (LA), while group II received 1.5 ml of intrathecal LA+0.1 ml sufentanil (5 μg). Both initial and postoperative subarachnoid block characteristics, hemodynamic and respiratory parameters, duration of analgesia, and side effects were observed and recorded. Statistical analysis was carried out using Chi-square and paired t test.
Results:
Demographic profile was comparable in both groups. Group I had a greater incidence of hypotension and, consequently, higher use of vasopressors (P<0.05). Onset of sensory analgesia, time to achieve peak sensory level, and recovery from motor blockade were significantly earlier in group II (P<0.05). Postoperative consumption of LA through epidural route was significantly higher in group I (P<0.05). The side effect profile was similar, except for a significantly higher incidence of shivering in group I (P<0.05).
Conclusions:
The study established that the dose of a local anesthetic can be safely and significantly lowered by 40%, with addition of low-dose sufentanil, thereby avoiding the hemodynamic fluctuation and providing a stable perioperative and postoperative period in the geriatric population. In addition, duration of sensory analgesia is prolonged and postoperative requirement for the epidural top-up also decreases.
Keywords: Geriatric, hyperbaric bupivacaine, lower limb surgery, spinal anesthesia, sufentanil
INTRODUCTION
Advanced diagnostic and therapeutic facilities have enhanced the life expectancy of humans, as a result of which geriatric population is expected to increase 25% by 2020 across the world.[1] Although the criterion of 65 years of age and greater is followed worldwide for classifying this subset of population into geriatric category, the biological age, which results from cellular aging, is more important than the chronological age in defining the capacity of the elderly to cope with the massive surgical and anesthetic stress.[2,3] Age is considered as one of the strongest predictors in population undergoing anesthetic stress of a severe cardio-respiratory outcome such as hypotension, arrhythmias, heart failure and death. As a result, mortality increases twofold in this subset of population as compared to young healthy adults, especially in patients undergoing major surgery.[4–6]
A skillful and a clinically precise anesthetic management of geriatric population requires in-depth knowledge of the numerous pathophysiological alterations and functional changes at this advanced age due to altered and more variable pharmacokinetics and pharmacodynamics and associated comorbidities.[7,8]
Neuraxial anesthetic blockade has a definite advantage in elderly patients over general anesthesia, as it reduces surgical stress by blocking nociceptive impulses from the operative site and a decreased sympathetic efferent nerve activity, thus minimizing cardio-respiratory complications and overall morbidity and mortality.[9,10] Other advantages of neuraxial block in the high-risk elderly population include reduction in blood loss, avoidance of general anesthesia, comfortable recovery, decreased incidence of deep vein thrombosis, better homeostasis of the neuroendocrine system, and improved immune response.[11]
The incidence of hypotension is in the range of 30-60% depending on the level of sympathetic block, age of patient, preoperative condition, blood volume, type of surgery, and amount of blood loss.[12] Hypotension may be so severe that it can impair renal functions or cause renal failure, abnormal rhythm and rate of respiration, bradycardia, and even cardiac arrest.[13]
Recently, the focus has shifted from the traditional approach to spinal anesthesia, with a decrease in conventional doses of local anesthetics (LA) and concomitant use of adjuvants. Antinociceptive synergism between intrathecal opioids and LA is an established fact, as central neuraxial administration of opioids in conjunction with LA not only improves the quality of intraoperative analgesia but also prolongs the duration and effectiveness of postoperative analgesia.[14]
Sufentanil is N-4 thienyl derivative of fentanyl and is more lipid soluble and has greater affinity for opioid receptors than fentanyl or morphine. When compared with fentanyl, sufentanil has a smaller volume of distribution and shorter elimination half-life. It is 7-10 times more potent than fentanyl and 100 times more potent than morphine.[15] Sufentanil has been shown to be better in attenuating hemodynamic and hormonal response to surgical stimuli as compared to fentanyl.[16,17]
Keeping in view the various merits of sufentanil, we planned to carry out a double-blind prospective study at our institute with an aim to compare the hemodynamic stability and quality of the conventional dose of LA by administering low dose of LA and sufentanil in elderly patients scheduled for lower limb surgery, and randomized to receive combined spinal epidural anesthesia.
METHODS
After approval from the ethical committee of the institute, the present study was carried out on 50 elderly patients of ASA grade I and II of either sex undergoing lower limb surgery under combined spinal epidural anesthesia at our institute attached to a Government Medical College. After obtaining written consent from patients, they were randomly divided by a computer-generated code into two groups of 25 each, group I and group II. Patients having any abnormality of the spine, skin infection, local cellulites, coagulation disorders, allergy to LA, neurological disorders, etc, were excluded from the study. Patients in Group I served as control group and received 2.5 ml (12.5 mg) of 0.5% hyperbaric bupivacaine. Group II patients received 1.5 ml (7.5 mg) of 0.5% hyperbaric bupivacaine +0.1 ml (5 μg) sufentanil + 0.9 ml normal saline to make a total volume of 2.5 ml. The study solutions were prepared by an anesthesia technician who was given written instructions but was not aware of the study details. Patients were kept fasting for at least six hours preoperatively and received tablet Ranitidine 150 mg and tablet alprazolam 0.25 mg one night before and 2 hours before on the morning of surgery with a sip of water.
In the operation theatre, baseline pulse rate, blood pressure, respiratory rate, and pulse oximetry (SpO2) were observed and recorded for every patient. A good intravenous access was secured with a large bore cannula and preloading was done with Ringer Lactate solution in doses of 10 ml/kg of body weight.
Epidural injection was administered to patients on a horizontal table in the sitting position in L3-4 inter-vertebral space with 18G Tuohy needle and a catheter was secured at 4-5 cm into the epidural space. Subarachnoid block was performed with 26G spinal needle at L4-5 space and drugs were injected after establishing a clear and free flow of the cerebrospinal fluid (CSF). Immediately after injecting the drug, patients were turned to supine position. The level and onset of sensory analgesia was checked with bilateral pin prick method and quality of sensory block was assessed using a visual analog scale for pain measurement (0 - no distress to 10 - unbearable distress). Motor blockade was checked using Bromage scale before and after surgery. (Grade 1 - free movement of legs and feet, grade 2 - just able to flex knees with free movement of feet, grade 3 - unable to flex knees, but with free movement of feet, and grade 4 - unable to move legs or feet).
Parameters like pulse rate (PR), systolic blood pressure (SBP), diastolic blood pressure (DBP), respiratory rate (RR), and pulse oximetry (SpO2) were observed continuously and recorded every 5 min for the first 30 min after giving subarachnoid block, thereafter every 10 min throughout the surgery. Hypotension was defined as a fall in SBP of greater than 25% of base value or SBP less than 95 mm of Hg in the first 20-30 min after giving the block and was treated with increments of injection Ephedrine 5 mg. Supplemental oxygen (3 L/min) was given to every patient through a venturi mask during the surgery. Side effects like nausea, vomiting, pruritis, etc were observed for and recorded on the performa. Postoperatively, patients were administered analgesia on demand through epidural catheter with 0.125% plain bupivacaine 8 ml during each top-up. At the end of study, complete data were compiled systematically and subjected to statistical analysis using Student's paired t-test and Chi-square test. P < 0.05 was considered as significant and P < 0.001 as highly significant.
RESULTS
The present study was conducted to assess the effect of low-dose hyperbaric bupivacaine and sufentanil intrathecally in causing minimal hypotension after spinal anesthesia in elderly patients undergoing lower limb surgeries.
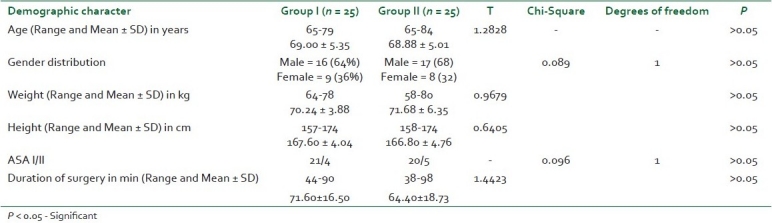
As evident from [Table 1], all patients were aged above 65 years and the mean age in group I was 69.00 ± 5.35 as compared to 68.88 ± 5.01 in group II. A majority of patients in both groups were male, being 64% in group I and 68% in group II. Female population comprised 36% in group I and 32% in group II. The mean weight in group I was 70.24 ± 3.88, with a range of 64-78 kg, whereas the corresponding values in group II showed a mean weight of 71.68 ± 6.35, with a range of 58-80 kg. Mean height of the population in group I was 167.60 ± 4.04 cm, with a range of 157-174 cm, which was comparable with height of group II population, with a mean of 166.80 ± 4.76 and a range of 158-174 cm. Similarly, mean values for duration of surgery were identical in both groups. On statistical analysis, the demographic profile in both groups was comparable and non-significant on statistical analysis (P > 0.05).
Table 1.
Distribution of demographic profile of patients in groups I and II
The baseline preoperative mean pulse rate in group I was 76.48 ± 11.46, with a range of 63-110 per min, while it was 74.24 ± 5.46, with a range of 60-102 per min in group II. The mean systolic blood pressure in group I (123.68 ± 12.32) was comparable to the mean SBP in group II (124.32 ± 12.34). Similarly, mean DBP in group I (78.80 ± 6.78) was comparable to mean DBP in group II (79.96 ± 6.39). On statistical analysis, no significant difference was found on comparison of preoperative hemodynamic parameters in both groups (P > 0.05).
However, minimal fluctuations were seen in the mean pulse rate in both groups throughout the study period.
Table 2 shows mean ± SD values of intraoperative systolic and diastolic blood pressure at different time intervals of both groups. The baseline value of mean systolic blood pressure in group I was 124.56 ± 12.08, with a range of 100-150 mm Hg and that of group II was 124.08 ± 13.81 with a range of 100-158 mm Hg, which was comparable and statistically not significant (P > 0.05). The mean SBP in group I at 5 min (105.28 ± 18.34) and 10 min (105.04 ± 12.18) showed highly significant variation from corresponding values at 5 min (121.52 ± 16.97) and 10 min (118.56 ± 15.43) in group II (P < 0.001). The mean systolic blood pressure at 15 min in group II showed a declining value (115.68 ± 16.31), and the difference remained significant from group I (106.80 ± 11.65) on statistical comparison (P < 0.05).
Table 2.
Intraoperative systolic and diastolic blood pressure in both groups
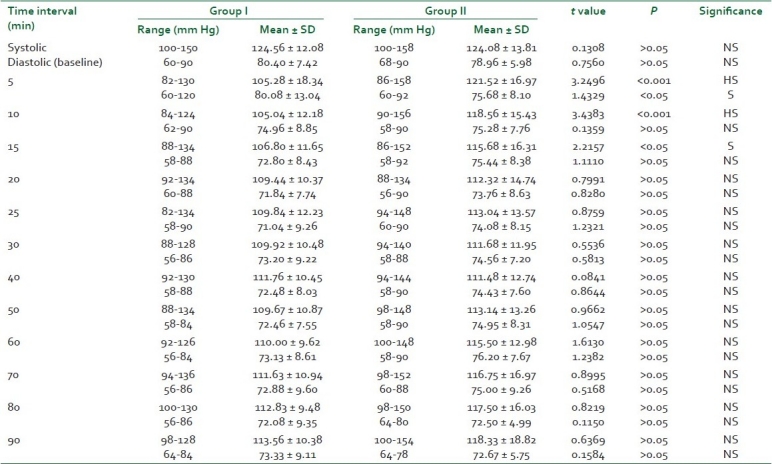
Thereafter, mean SBP in both groups remained stable and no statistical significant difference was noted between both groups throughout the study period (P > 0.05).
Surprisingly, the statistical changes in diastolic blood pressure were significant (P < 0.05) only during the first 5 min in both groups [Table 3], and thereafter the mean ± SD values of intraoperative diastolic blood pressure at different time intervals of both groups showed no significant differences throughout the study period (P > 0.05).
Table 3.
Characteristics of the neuraxial blockade in both groups
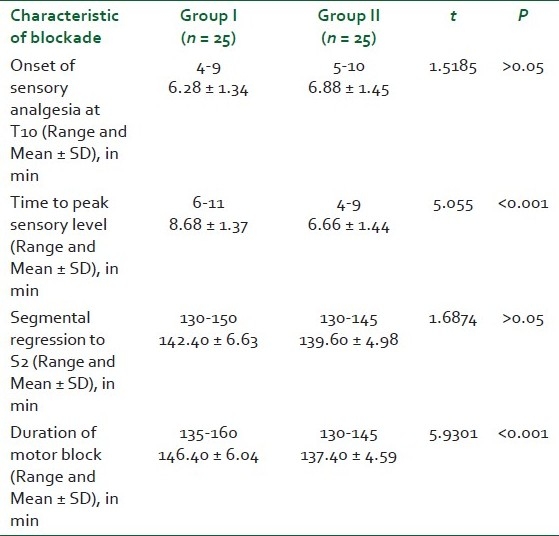
The mean time taken for the onset of adequate sensory analgesia at T10 in group I was 6.28 ± 1.34, with a range of 4-9 min group I as compared to a mean time of 6.88 ± 1.45 with a range of 5-10 min in group II and the difference was not significant on statistical comparison (P > 0.05). The mean time to reach a peak sensory block level in group I (8.68 ± 1.37) was achieved much later than that of group II (6.66 ± 1.44), which was highly significant (P < 0.001) on statistical comparison. Mean time taken to S2 segment regression in group I (142.40 ± 6.63) was almost comparable to that of group II (139.60 ± 4.98) and statistical analysis showed insignificant difference (P > 0.05). However, the duration of motor blockade revealed a highly significant statistical entity (P < 0.001), as complete recovery of motor power was much earlier in the group II (137.40 ± 4.59) as compared to group I (146.40 ± 6.04) [Table 3].
Statistical analysis
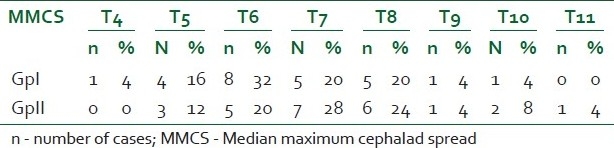
Table 4 shows the distribution of cases according to MMCS (ie, maximum upper level of sensory block assessed in the midline) in both groups. Sensory blockade was assessed by the pin prick method. In group I, most cases (32%) had sensory blockade up to T6 level with a range of T4-T10, whereas in group II, most cases (28%) had sensory blockade up to T7 level, with a range of T5-T11. Statistical analysis revealed a Chi-square value of 3.593 with 7 degrees of freedom and the difference in MMCS in both groups was insignificant (P > 0.05).
Table 4.
Median maximum cephalad spread in both groups
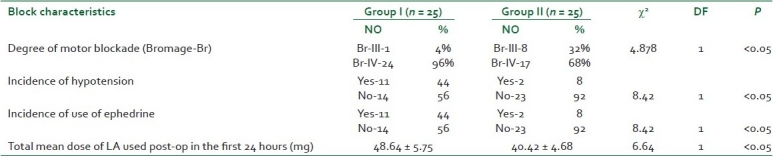
Degree of motor block was assessed according to the Bromage scale. Grade IV motor block was observed in 96% of cases in group I and 68% of cases in group II, whereas grade III motor block was seen in only 4% of cases in group I and 32% of cases in group II. The block being more intense in group I than in group II and on statistical analysis showed significant difference (P < 0.05). The incidence of hypotension was much higher in group I (44%) as compared to group II (8%), which was statistically significant (P < 0.05). As a result the consumption of vasopressors was significantly higher (P < 0.05) in group I as compared to group II. Postoperatively, consumption of analgesic dose of bupivacaine through epidural catheter was significantly higher (P < 0.05) in the non-sufentanil group [Table 5].
Table 5.
Degree of motor blockade, incidence of hypotension, use of vasopressors, and total local analgesic dose consumption postoperatively
Shivering was observed in seven cases in group I as compared to none in group II, which showed a significant value on statistical comparison (P < 0.05). Pruritis was seen in three cases in group II, whereas none of the cases in group I had pruritis, which was not significant on statistical comparison (P > 0.05). No patients in either group experienced nausea, vomiting, respiratory depression, or urinary retention [Figure 1].
Figure 1.
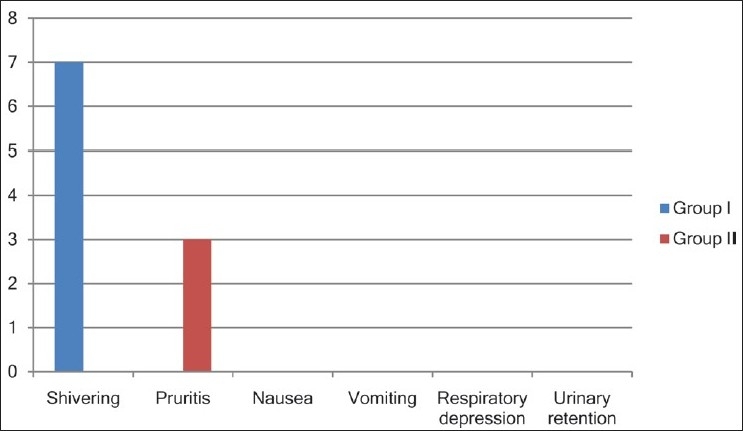
Comparison of adverse effects in both groups
DISCUSSION
Administration of general anesthesia in the elderly population is always challenging, due to reduced cardiac index, reduced hepato-renal blood flow, reduced baroreflex responses, increased work of breathing, and reduced alveolar exchange due to aging. These factors can cause overdosing of intravenous and inhalational anesthetic agents and, consequently, a increased incidence of side effects of these agents.[18] At the molecular and cellular level, cardiac morphological changes include decrease in the number of myocytes, decrease in connective matrix tissue, and increase in left ventricular wall thickness, all of which result in decreased cardiac contractility, increased action potential time, and decreased coronary perfusion.[19,20] Similarly, aging-induced cardiovascular alterations, autonomic changes, and consequent decrease in peripheral vascular resistance may produce exaggerated and intense hemodynamic fluctuations, including hypotension and bradycardia. On the other hand, due to age-related decrease in the volume of CSF and relative increase in the density of CSF, there occurs a greater diffusion of LA solution leading to wider block extension during neuraxial anesthesia.[21] The surgical and anesthetic stress causes exaggerated sympathetic activation, an increase in catabolic hormones and hypermetabolism in the elderly. These result in delayed emergence, increased fatigue, prolonged recovery, intestinal paralysis, decreased splanchnic perfusion, and numerous other complications, leading to a higher incidence of perioperative morbidity and death.[22–25]
A spinal block given to a high-risk patient must provide anesthesia of high quality and with adequate duration in order to avoid the negative effects of any additional anesthesia. Intraoperative hypotension following spinal anesthesia can be deleterious, especially in the geriatric population with limited cardiorespiratory reserve. It has been suggested that a combination of opioids and LA administered intrathecally has a synergistic analgesic effect characterized by enhanced somatic analgesia without an effect on the degree and level of LA-induced sympathetic or motor block.[26]
The demographic profile of our patients is comparable to the profile of various other similar studies, except for the age group, which was higher in our study. This is quite important in the context that we intended to study the dose reduction of LA and addition of low-dose sufentanil with the main aim of providing hemodynamic stability in geriatric patients, as this subset of population demonstrates exaggerated hemodynamic responses to various anesthetic techniques.[17,27,28]
The mean pulse rate showed no remarkable difference in either groups throughout the study period, which establishes the efficacy of sufentanil in providing stable heart rate on intrathecal use similar to the earlier observations by various researchers.[17,29,30] Patients who received intrathecal sufentanil had a significantly lower mean systolic blood pressure during the first 15 minutes and a lower mean diastolic blood pressure for the first 5 minutes, which stabilized after that and remained stable throughout the study period in both groups. However, the overall incidence of hypotension was significantly higher in the non-sufentanil group (44%) as compared to sufentanil group (8%), with a consequent higher use of ephedrine in this subset of population. Similar observations were the hallmark of earlier such studies, except for minor variations.[17,28,30]
However, in the present study, the number of patients requiring treatment for hypotension was 44% in the control group, whereas Olofsson et al. treated 88% patients for hypotension in their control group. The higher incidence of hypotension in their study might be because of the different criteria for defining hypotension (decrease in SBP>25% from the baseline or SBP<100 mm Hg.). Our criteria for hypotension was defined as decrease in SBP<95 mm Hg or 25% decrease from the baseline. The overall observed hemodynamic stability was comparatively better in patients who received small doses of intrathecal bupivacaine and sufentanil. This can be attributed to the low-dose combination of LA and sufentanil in providing a potent synergistic analgesic effect. Yet, intrathecal opioid neither by itself nor in combination with LA causes any further depression of efferent sympathetic activity. Therefore, it is possible to enhance sensory blockade without altering the degree of sympathetic blockade, and hence a lower incidence of intraoperative hypotension.
The time to reach peak sensory block was significantly shorter in group II (6.66 ± 1.44) (P < 0.001) as compared to group I (8.68 ± 1.37), though no statistically significant difference was found at the onset of adequate analgesia, MMCS, and time to S2 segment regression between both groups (P > 0.05). In the present study, surgical anesthesia was adequate in all patients of both groups and never required supplementary epidural anesthetic doses through epidural catheter during the surgical procedure. The level of analgesia was also adequate in both groups, as shown by Visual Analogue Scale of pain measurement, which was zero at every assessment throughout the observation period. The results are quite similar to the earlier studies with minor variations here and there.
Statistical analysis showed a highly significant difference in the mean duration of motor block in both groups (P < 0.001). This was noted because the study group had less intense motor block with 32% of cases having grade III block and 68% of cases having grade IV block than control group, which has 4% of cases having grade III block and 96% of cases having grade IV block. The block was of shorter duration in the study group than in the control group. However, in the study group, the degree of motor block was adequate for the procedure and surgeons’ satisfaction.[17,29,30]
The results have re-established the synergistic effect of opioid and LA, whereby the quality and duration of sensory block is increased, while degree and duration of motor block is shortened. Therefore, the time to recovery and ambulation decreases, thereby reducing the incidence of deep vein thrombosis. Intrathecal opioids are associated with several known side effects. The incidence of pruritis attributable to opioids ranges between 20 and 80%.[26,31,32] In our study, 12% patients had pruritis in the sufentanil group. The lower incidence of pruritis can be explained on the basis that we used a lower dose of sufentanil. However, none of the patient required any treatment.
Neuraxial opioids carry the risk of respiratory depression, especially in elderly patients.[26,31,32] Respiratory depression after administration of more lipid-soluble agent sufentanil may develop within 30 min of subarachnoid injection. Earlier onset of this condition might be an advantage as compared to the delayed respiratory depression induced by intrathecal morphine since the patient is still in the operating room and well under the anesthesiologist's supervision. But in our study, none of the patients in the sufentanil group had respiratory depression or a lower recording of O2 saturation. There have been cases of respiratory depression and apnea after intrathecal sufentanil in laboring women.[26,31,32] However, in most of these studies, the patient had either received previous parenteral opioid or a dose of intrathecal sufentanil 10 μg or more. We did not come across any case of respiratory depression or apnea after administration of 5 μg intrathecal sufentanil. The possible reason may be that we did not give any parenteral sufentanil in our study, nor did we use a dose of sufentanil larger than 5 μg.
Another common side effect of intrathecally administered opioid is nausea and vomiting.[26,31,32] However, none of our patients had nausea or vomiting, which is again possibly is due to the lower dosage of intrathecal sufentanil. Shivering is also a common complication during spinal anesthesia in elderly patients.[26,31,32] It is known to increase oxygen consumption, ventilation, and cardiac output, which can result in significant morbidity in patients with limited cardiopulmonary reserve. In the present study, 28% in the control group had shivering, whereas none of the patients in the study group had any such episodes.
Similar findings have been reported by earlier studies in patients who underwent transurethral resection of prostate (TURP) under spinal anesthesia.[33] The studies have reported 30% incidence of shivering in the control group, while 5% patients experienced shivering in the bupivacaine and fentanyl group. Addition of fentanyl to low-dose bupivacaine has been shown to decrease the incidence of shivering during spinal anesthesia in elderly patients. Our results have also established that addition of even low-dose intrathecal sufentanil to a lower-dose bupivacaine also decreases the incidence of shivering.
A number of studies have used sufentanil intrathecally in lower limb surgery. In our study, we found that bupivacaine 7.5 mg plus sufentanil 5 mg provides stable hemodynamics and satisfactory anesthesia than the conventional dose (12.5 mg) of bupivacaine.
CONCLUSION
The present work studied the comparative evaluation of adding sufentanil to low dose of bupivacaine with the conventional dose of bupivacaine in elderly patients undergoing lower limb surgery under combined spinal epidural anesthesia. The study has established that the dose of LA can be safely and significantly lowered by 40% with the addition of low-dose sufentanil, thereby avoiding hemodynamic fluctuation and providing a stable peri- and post-operative period in the geriatric population. In addition, the duration of sensory analgesia is prolonged and the postoperative requirement for the epidural top-up is also decreased.
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared.
REFERENCES
- 1.Naughton C, Feneck RO. The impact of age on six-month survival in patients with cardiovascular risk factors undergoing elective noncardiac surgery. Int J Clin Pract. 2007;61:768–76. doi: 10.1111/j.1742-1241.2007.01304.x. [DOI] [PubMed] [Google Scholar]
- 2.Demongeot J. Biological boundaries and biological age. Acta Biotheor. 2009;57:397–418. doi: 10.1007/s10441-009-9087-8. [DOI] [PubMed] [Google Scholar]
- 3.Inouye SK, Peduzzi PN, Robinson JT, Hughes JS, Horwitz RI, Concato J. Importance of functional measures in predicting mortality among older hospitalized patients. JAMA. 1998;279:1187–93. doi: 10.1001/jama.279.15.1187. [DOI] [PubMed] [Google Scholar]
- 4.Forrest JB, Rehder K, Cahalan MK, Goldsmith CH. Predictors of severe perioperative adverse outcomes. Anesthesiology. 1992;76:3–15. doi: 10.1097/00000542-199201000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Osswald PM, Meier C, Schmegg B, Hartung HJ. Complications of anesthesia in elderly patients. Anaesthesist. 1987;36:292–300. [PubMed] [Google Scholar]
- 6.Forster MC, Calthorpe D. Mortality following surgery for proximal femoral fractures in centenarians. Injury. 2000;31:537–9. doi: 10.1016/s0020-1383(00)00049-8. [DOI] [PubMed] [Google Scholar]
- 7.Roy RC. Anesthetic considerations for the geriatric patient. Anesth Analg. 1998;86:114–8. [Google Scholar]
- 8.Mascarenhas J, Azedevo A, Bettencourt P. Coexisting chronic obstructive pulmonary disease and heart failure: implications for treatment, course and mortality. Curr Opin Pulm Med. 2010;16:106–11. doi: 10.1097/MCP.0b013e328335dc90. [DOI] [PubMed] [Google Scholar]
- 9.Kapral S, Gollmann G, Bachmann D, Prohaska B, Likar R, Jandrasits O, et al. The effects of thoracic epidural anesthesia on intraoperative visceral perfusion and metabolism. Anesth Analg. 1999;88:402–6. doi: 10.1097/00000539-199902000-00034. [DOI] [PubMed] [Google Scholar]
- 10.Rodgers A, Walker N, Schug S, McKee A, Kehlet H, van Zundert A, et al. Reduction of postoperative mortality and morbidity with epidural or spinal anaesthesia: Results from overview of randomised trials. BMJ. 2000;321:1493. doi: 10.1136/bmj.321.7275.1493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Felsby S, Juelsgaard P. Combined spinal and epidural anesthesia. Anesth Analg. 1995;80:821–6. doi: 10.1097/00000539-199504000-00029. [DOI] [PubMed] [Google Scholar]
- 12.Chamberlain DP, Chamberlain BD. Changes in the skin temperature of the trunk and their relationship to sympathetic blockade during spinal anaesthesia. Anaesthesiology. 1986;65:139–43. doi: 10.1097/00000542-198608000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Caplan RA, Ward RJ, Posner K, Cheney FW. Unexpected cardiac arrest during spinal anaesthesia: A closed claims analysis of predisposing factors. Anaesthesiology. 1988;68:5–11. doi: 10.1097/00000542-198801000-00003. [DOI] [PubMed] [Google Scholar]
- 14.Grewal P, Katyal S, Kaul TK, Narual N, Grewal A. A comparative study of effects of fentanyl with different doses of bupivacine in subarachnoid block. J Anaesth Clin Pharmacol. 2003;19:193–7. [Google Scholar]
- 15.Bailey PL, Streisand JB, East KA, East TD, Isern S, Hansen TW, et al. Difference in magnitude and duration of opioid-induced respiratory depression and analgesia with fentanyl and sufentanil. Anaesth Analg. 1990;70:8–15. doi: 10.1213/00000539-199001000-00003. [DOI] [PubMed] [Google Scholar]
- 16.Borgdoff PJ, Lonescu TI, Houweling PL, Knape JT. Large dose intra thecal sufentanil prevents the hormonal stress response during major abdominal surgeries: A comparison with intra venous sufentanil in a prospective randomized trial. Anesth Analg. 2004;99:1114–20. doi: 10.1213/01.ANE.0000131728.68125.4E. [DOI] [PubMed] [Google Scholar]
- 17.Olofsson C, Nygards EB, Bjersten AB, Hessling A. Low dose bupivacaine with sufentanil prevents hypotention after spinal anaesthesia for hip repair in elderly patients. Acta Anaesthesiol Scand. 2004;48:1240–4. doi: 10.1111/j.1399-6576.2004.00504.x. [DOI] [PubMed] [Google Scholar]
- 18.Zaugg M, Lucchinetti E. Respiratory function in the elderly. Anesthesiol Clin North America. 2000;18:47–57. doi: 10.1016/s0889-8537(05)70148-6. [DOI] [PubMed] [Google Scholar]
- 19.Priebe HJ. The aged cardiovascular risk patient. Br J Anaesth. 2000;85:763–78. doi: 10.1093/bja/85.5.763. [DOI] [PubMed] [Google Scholar]
- 20.Rooke GA. Autonomic and cardiovascular function in the geriatric patient. Anesthesiol Clin North America. 2000;18:31–46. doi: 10.1016/s0889-8537(05)70147-4. [DOI] [PubMed] [Google Scholar]
- 21.Hocking G, Wildsmith JAW. Intrathecal drug spread : 568-78. Br J Anaesth. 2004;93:568–78. doi: 10.1093/bja/aeh204. [DOI] [PubMed] [Google Scholar]
- 22.Riles TS, Fisher FS, Schaefer S, Pasternack PF, Baumann FG. Plasma catecholamine concentrations during abdominal aortic aneurysm surgery: The link to perioperative myocardial ischemia. Ann Vasc Surg. 1993;7:213–9. doi: 10.1007/BF02000244. [DOI] [PubMed] [Google Scholar]
- 23.Weissmann C. The metabolic response to stress: An overview and update. Anesthesiology. 1990;73:308–27. doi: 10.1097/00000542-199008000-00020. [DOI] [PubMed] [Google Scholar]
- 24.Steinbrook RA. Epidural anesthesia and gastrointestinal motility. Anesth Analg. 1998;86:837–44. doi: 10.1097/00000539-199804000-00029. [DOI] [PubMed] [Google Scholar]
- 25.Boldt J, Papsdorf M, Piper S, Padberg W, Hempelmann G. Influence of dopexamine hydrochloride on haemodynamics and regulators of circulation in patients undergoing major abdominal surgery. Acta Anaesthesiol Scand. 1998;42:941–7. doi: 10.1111/j.1399-6576.1998.tb05354.x. [DOI] [PubMed] [Google Scholar]
- 26.Tejwani GA, Rattan AK, McDonald JS. Role of spinal opioid receptors in the antiociceptive interactions between intrathecal morphine and bupivacaine. Anaesth Analg. 1992;74:726–34. doi: 10.1213/00000539-199205000-00018. [DOI] [PubMed] [Google Scholar]
- 27.Ben David B, Frankel R, Arzumonov T, Marchevsky Y, Volpin G. Mini dose bupivacaine-fentanyl spinal anesthesia for surgical repair of hip fracture in the aged. Anesthesiology. 2000;92:6–10. doi: 10.1097/00000542-200001000-00007. [DOI] [PubMed] [Google Scholar]
- 28.Asehnoune K, Larousse E, Tadie JM, Miniville V, Droupy S, Benhamou D. Small dose bupivacaine-sufentanil prevents cardiac output modifications after spinal anesthesia. Anesth Analg. 2005;101:1512–5. doi: 10.1213/01.ANE.0000180996.91358.CC. [DOI] [PubMed] [Google Scholar]
- 29.Waxler B, Mondragon SA, Patel SN, Nedumgottil K. Intrathecal lidocaine and sufentanil shorten postoperative recovery after outpatient rectal surgery. Can J Anaesth. 2004;51:680–4. doi: 10.1007/BF03018425. [DOI] [PubMed] [Google Scholar]
- 30.Singh NP, Chhatrapati S. Efficacy of sufentanil with low dose bupivacaine on subarachnoid block for vaginal hysterectomy. Anaesthesiology. 2007;107:A884. [Google Scholar]
- 31.Dickenson AH. Mechanism of the analgesic actions of opiates and opioids. Br Med Bull. 1991;47:690–702. doi: 10.1093/oxfordjournals.bmb.a072501. [DOI] [PubMed] [Google Scholar]
- 32.Fernandez-Galinski D, Rue M, Moral V, Castells C, Puig MM. Spinal anesthesia with bupivacaine and fentanyl in geriatric patients. Anesth Analg. 1996;83:537–41. doi: 10.1097/00000539-199609000-00017. [DOI] [PubMed] [Google Scholar]
- 33.Kararmaz A, Kaya S, Turhanoglu S, Ozyilmaz MA. Low-dose bupivacaine-fentanyl spinal anaesthesia for transurethral prostatectomy. Anesthesia. 2003;58:526–30. doi: 10.1046/j.1365-2044.2003.03153.x. [DOI] [PubMed] [Google Scholar]


