Abstract
Objective:
To compare the three common methods of endotracheal tube cuff inflation (sealing pressure, precise standard pressure or finger estimation) regarding the effective tracheal seal and the incidence of post-intubation airway complications.
Methods:
Seventy-five adult patients scheduled for N2 O free general anesthesia were enrolled in this study. After induction of anesthesia, endotracheal tubes size 7.5 mm for female and 8.0 mm for male were used. Patients were randomly assigned into one of three groups. Control group (n=25), the cuff was inflated to a pressure of 25 cm H2O; sealing group (n=25), the cuff was inflated to prevent air leaks at airway pressure of 20 cm H2O and finger group (n=25), the cuff was inflated using finger estimation. Tracheal leaks, incidence of sore throat, hoarseness and dysphagia were tested.
Results:
Although cuff pressure was significantly low in the sealing group compared to the control group (P<0.001), the incidence of sore throat was similar in both groups. On the other hand, cuff pressure as well as the incidence of sore throat were significantly higher in the finger group compared to both the control and the sealing group (P<0.001 and P=0.008). The incidence of dysphagia and hoarseness were similar in the three groups. None of the patients in the three groups developed air leak around the endotracheal tube cuff..
Conclusions:
In N2O, free anesthesia sealing cuff pressure is an easy, undemanding and safe alternative to the standard technique, regarding effective sealing and low incidence of sore throat.
Keywords: Airway Morbidity, cuff pressure, endotracheal tube
INTRODUCTION
The cuffs of an endotracheal tube are used to prevent gas leak and also pulmonary aspiration in intubated patients. Despite the use of high-volume, low-pressure cuffs, certain patients remain at risk for cuff-induced laryngotracheal morbidity, even with short-duration anesthesia.[1–3] The main symptom reported after tracheal intubation is sore throat, but patients also report hoarseness and dysphagia.[4–6] Although the exact pathophysiology of post-intubation airway symptoms is not fully known, mucosal damage occurring at the cuff level is thought to be an important causative factor for tracheal morbidity.[7–11] Tracheal arterial capillary pressure decreases when the cuff exerts pressure greater than 30 cm H2O, causing tracheal ischemia proportional to the pressure exerted by the cuff and to the duration of exposure.[12] The ideal cuff pressure has not certainty been defined, but most anesthesiologists generally recommend a target of 20 to 30 cm H2O.[13] The length of time needed for an elevated cuff pressure to cause these complications is unclear, but mucosal damage has been demonstrated after only 15 minutes in an animal model.[14]
The three common methods of endotracheal tube cuff inflation used in clinical setting are the use of sealing pressure, inflation to a precise pressure (25 cm H2O), or estimation of the cuff pressure by finger palpation. The aim of our study is to compare the three techniques regarding the prevention of tracheal leak and the incidence of post-intubation airway morbidity. We presuppose that inflation of the cuff to a sealing pressure is an easy way to maintain safe and effective cuff pressure as well as minimize post-intubation airway symptoms.
METHODS
After approval from Research and Ethics Committee and written informed consent, 75 patients with ASA physical status I or II were enrolled in this prospective, controlled, randomized, blinded study. All patients were scheduled for surgical procedures under N2O free general anesthesia with an expected duration of 90 min or more. Patients undergoing head or neck surgery or patients with tracheotomy, laryngeal disease or laryngeal surgery, or those requiring placement of a nasogastric tube, or in whom intubation will be difficult (two or more trials), were excluded from the study.
All patients were premedicated with 0.2 mg/kg diazepam administrated orally 90 min before anesthesia induction. On arrival to the operating room, standard anesthetic technique was conducted by consultant anesthesiologist of more than 15 year experience who is blind to the study design. After fixation of standard monitoring and preoxygenation for 3 min, anesthesia was induced with fentanyl 2 μg/ kg and propofol 2.5 mg/kg. Neuromuscular block was achieved with rocuronium bromide 0.6 mg/kg.Tracheal intubation was performed when maximum neuromuscular blocking effect assessed by the train-of-four count at the adductor pollicis was achieved. A Guedel airway was used for all patients during anesthesia. Endotracheal tubes (Lo-Contour; Mallinckrodt, Athlone, Ireland) with high residual volume, low-pressure cuff, with an inner diameter of 7.5 mm for female and 8.0 mm for male, were used in our study. Patients were randomly assigned, by opening a sealed envelope, to one of three groups. In the control group (n = 25), the ETT cuff was aspirated as much as possible and then inflated with air to achieve a cuff pressure of 25 cm H2O. In the sealing group (n = 25), the ETT cuff was aspirated as much as possible and then inflated with air to prevent air leaks during the inspiratory phase of mechanical ventilation of the patient when peak airway pressure was 20 cm H2 O. In the finger group (n = 25), the ETT cuff was aspirated as much as possible and then inflated to a suitable pressure by palpation of the external balloon. The volume used to fill the cuff and the cuff pressure were recorded in each group using hand-held, manometer P-V gauge (Mallinckrodt Medical, St. Louis, MO) by an anesthesiologist who was blind to the studied group. The same anesthesiologist assessed tracheal leak by both audible technique and by observing the difference between inspiratory and expiratory tidal volume. Mechanical ventilation was controlled and adapted to maintain end-tidal carbon dioxide at 30–35 mmHg. Anesthesia was maintained with sevoflurane (1–2% end-tidal) and 30% oxygen in air, supplemented by boluses of fentanyl (1–2 μg/kg). At the end of surgery, neuromuscular block was reversed with neostigmine 0.05 mg/kg and atropine 0.025 mg/kg and the pharynx was gently suctioned. Before tracheal extubation, patients breathed 100% oxygen for 5 min and the ETT was removed as soon as all of the following criteria were met: Full reversal of neuromuscular block (ulnar nerve T4/T1 ratio = 1); spontaneous breathing; and the ability to follow verbal commands (hand grip or eye opening) or else demonstrate purposeful unilateral movement (attempting self-extubation).The duration of surgery and intubation were recorded. Intravenous paracetamol and morphine were used for postoperative analgesia. At the time of discharge from the post-anesthesia care unit (PACU) and 24 h after tracheal extubation, patients were asked about three laryngotracheal complaints: Sore throat, hoarseness and dysphagia by an independent observer who was unaware of the patient allocation groups. He assessed the severity of these symptoms on a visual analog scale (VAS; where 0 = no discomfort and 10 = worst discomfort possible).
Statistical analysis
Demographic data, duration of surgery and intubation, dose of fentanyl, the volume of air injected in the cuff and intra-cuff pressure were analyzed by one-way ANOVA test with Bonferroni correction. Unpaired Student's t-test was used to compare the control group and the other two groups. Gender ratio and the differences in the incidence of the laryngotracheal symptoms were analyzed by Fisher's exact or Chi-square tests. Probability (p-value) less than 0.05 was considered statistically significant. Analysis was performed using Statistica software version 7.0 for Windows (Statsoft, Inc.).
RESULTS
There were no significant difference between the three groups regarding demographic data, duration of surgery and intubation and intraoperative fentanyl dose [Table 1]. The cuff pressure was significantly low in the sealing group compared to the control group (P < 0.001), whereas it was significantly high in the finger group compared to both the control and the sealing group (P < 0.001) [Table 1 and Figure 1]. Similarly the volume of air to fill the cuff was insignificantly low (P < 0.09) in the sealing group compared to the control group, nevertheless it was significantly high in the finger group compared to the other two groups (P < 0.001) [Table 1 and Figure 1]. None of the patients in the three groups developed air leak around the ETT cuff.
Table 1.
Demographic data and intra-operative characteristics of patients in the three groups
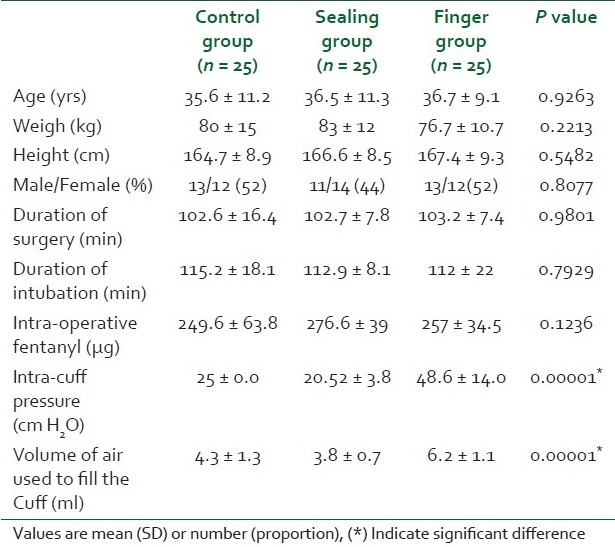
Figure 1.
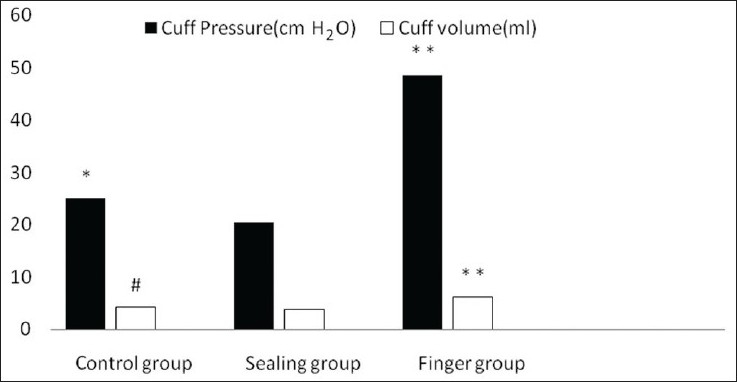
ETT cuff pressure (cm H2O) and air volume (ml) used to fill the cuff in the three groups. (*) Indicates significant difference between control and sealing group. (**) Indicates significant difference between finger and other two groups. (#) Indicates insignificant difference between control and sealing group
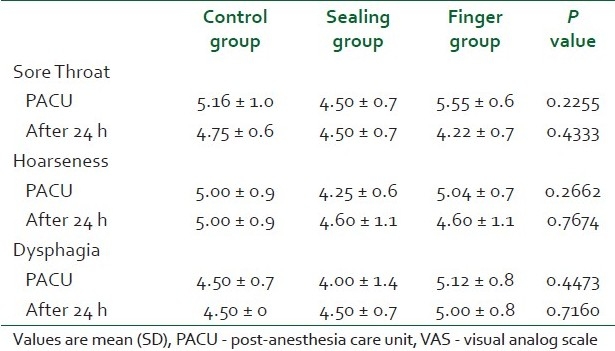
The incidence of sore throat was similar for the control and sealing groups in the PACU and at 24 hours, whereas for the finger group the incidence of sore throat was significantly higher than the other two group in the PACU and at 24 hours (P = 0.008 and P = 0.003), while the incidence of dysphagia and hoarseness was similar in the three groups at both the recording times [Table 2]. The severity visual analog scale (VAS) of sore throat, dysphagia and hoarseness were similar for the three groups in the PACU and at 24 hours [Table 3].
Table 2.
Incidence of laryngotracheal complaints in the post-anesthesia care unit and in the first postoperative day
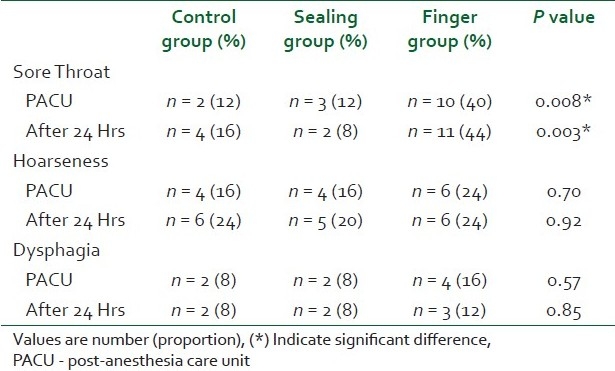
Table 3.
Severity of laryngotracheal complaints VAS in the post-anesthesia care unit and in the first postoperative day
DISCUSSION
Our prospective randomized controlled double-blind study showed similar incidence of sore throat in both sealing and control groups, which was significantly lower than that in the finger group, whereas the incidence of hoarseness and dysphagia was similar in the three groups.
In the present study, though significant low-cuff pressures in the sealing group (20 cm H2O) compared to the control group (25 cm H2O), the incidence or intensity of postoperative laryngotracheal complaints was not reduced. This was expected as the cuff pressure in the control group was still in the safe range (below 30 cm H2 O) which is unlikely to impair tracheal capillary mucosal perfusion. On the other hand, the cuff pressure in the finger group (48 cm H2O) had greatly exceeded the critical value, which could explain the higher incidence of sore throat in this group compared to the sealing and control groups.
Many studies had assessed the relationship between ETT cuff pressure and the occurrence of laryngotracheal complaints with contradictory results.[4–8,11] A recent study[7] failed to show a significant effect of ETT cuff pressure on postoperative sore throat frequency. However, the study design, anesthetic technique and intubating circumstances were not controlled and a nasogastric tube was inserted in most patients.
Conversely, our study, as well as several clinical studies have shown a lower frequency of sore throat when cuff pressure was maintained below the critical value of 30 cm H2O during anesthesia.[1–8] Moreover, the effect of endotracheal tube cuff pressure exceeding tracheal capillary mucosal perfusion was confirmed in experimental settings.[14]
One of the common practice for anesthetists is to palpate the external balloon (contiguous with the cuff) after intubation to attempt to obtain a rough estimation of the intra-cuff pressure; our study supported by other several studies[15–17] have suggested that this is unreliable technique which could result in unnecessary high intra-cuff pressure with consequent laryngotracheal complains. Thus it is necessary to use a manometer to adequately assess intra-cuff pressure or to inflate the cuff with air to a sealing pressure.
In observation of the significant lower cuff pressure found in the sealing group than in the control group, air volume to fill the cuff was (against expectation) insignificantly smaller in sealing group compared to the control group. This could be explained by the high compliance of the high-volume, low-pressure cuff which allow the pressure to increase slowly between the pressures of 10 and 20 cm H2O, after which the addition of small volumes increases the cuff pressure significantly.[18]
In the current study, the incidence of sore throat was significantly higher in the finger group compared to both sealing and control group, whereas the incidence of both hoarseness and dysphagia was similar in the three groups. This finding have been supported by other investigators,[11,16] who claimed the high tracheal cuff pressure as an important factor in the development of tracheal mucosal ulcerations whose severity was correlated to postoperative sore throat incidence. While other postoperative symptoms, principally hoarseness and dysphagia, were related to tracheal intubation and airway management, explaining their similar incidence in all groups.
Several studies confirmed that females are more commonly and strongly affected by intubation-related complaints.[19–21] This inequity was not supported in our study. This could be explained by our small sample size, which designed to investigate the effect of pressure rather than the effect of gender on the incidence of post-intubation complaints.
As N2O has been declined in current anesthesia practice, to our knowledge, only Biro et al.[22] had studied the effect of the intra-cuff sealing pressure up to an airway pressure of 25 cm H2 O on the incidence of postoperative sore throat in a N2O-free anesthesia. They failed to show any protective effect of limiting endotracheal tube cuff pressure on post-intubation sore throat incidence. This could be explained by the use of a cuff pressure below the critical value (30 cm H2O). On the other hand, Braz et al.[16] support the idea of intra-cuff sealing pressure even in presence of N2O and postulated that “When it is not possible to monitor the cuff pressure, such as in head and neck surgeries carried out with N2O, preference should be given to the sealing cuff pressure, which prevents the occurrence of high cuff pressure, especially during the first 60 minutes of N2O anesthesia.”.
In our study we did not evaluate leakage of liquid past the cuffs of tracheal tubes in our three designed cuff pressure groups. This was a limitation of our study as the sealing cuff pressure is known to be able to prevent leakage of inspired gas but it does not necessarily prevent the aspiration of regurgitated gastric contents. This will be investigated in our next study.
CONCLUSION
In anesthesia in which N2O is not used, an ETT sealing cuff pressure is a handy, undemanding and safe alternative to the standard technique of inflating the cuff to a pressure of 25 cm H2O, regarding prevention of air leak and low incidence of sore throat. Nevertheless estimation of the cuff pressure by finger palpation is an unreliable technique, which could result in high incidence of laryngotracheal complaints.
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared.
REFERENCES
- 1.Mandoe H, Nikolajsen L, Lintrup U, Jepsen D, Molgaard J. Sore throat after endotracheal intubation. Anesth Analg. 1992;74:897–900. [PubMed] [Google Scholar]
- 2.Nordin U, Lindholm CE, Wolgast M. Blood flow in the rabbit tracheal mucosa under normal conditions and under the influence of tracheal intubation. Acta Anaesthesiol Scand. 1977;21:81–94. doi: 10.1111/j.1399-6576.1977.tb01198.x. [DOI] [PubMed] [Google Scholar]
- 3.Seegobin RD, van Hesselt GL. Endotracheal cuff pressure and tracheal mucosal blood flow: Endoscopic study of effects of four large volume cuffs. Br Med J (Clin Res Ed) 1984;288:965–8. doi: 10.1136/bmj.288.6422.965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Loeser EA, Orr DL, 2nd, Bennett GM, Stanley TH. Endotracheal tube cuff design and postoperative sore throat. Anesthesiology. 1976;45:684–7. doi: 10.1097/00000542-197612000-00023. [DOI] [PubMed] [Google Scholar]
- 5.Loeser EA, Machin R, Colley J, Orr D, 2nd, Bennett GM, Stanley TH. Postoperative sore throat–importance of endotracheal tube conformity versus cuff design. Anesthesiology. 1978;49:430–2. doi: 10.1097/00000542-197812000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Jensen PJ, Hommelgaard P, Sondergaard P, Eriksen S. Sore throat after operation: Influence of tracheal intubation, intracuff pressure and type of cuff. Br J Anaesth. 1982;54:453–7. doi: 10.1093/bja/54.4.453. [DOI] [PubMed] [Google Scholar]
- 7.Bennett MH, Isert PR, Cumming RG. Postoperative sore throat and hoarseness following tracheal intubation using air or saline to inflate the cuff–a randomized controlled trial. Anaesth Intensive Care. 2000;28:408–13. doi: 10.1177/0310057X0002800409. [DOI] [PubMed] [Google Scholar]
- 8.Suzuki N, Kooguchi K, Mizobe T, Hirose M, Takano Y, Tanaka Y. Postoperative hoarseness and sore throat after tracheal intubation.Effect of a low intracuff pressure of endotracheal tube and usefulness of cuff pressure indicator. Masui. 1999;48:1091–5. [PubMed] [Google Scholar]
- 9.Tu HN, Saidi N, Leiutaud T, Bensaid S, Menival V, Duvaldestin P. Nitrous oxide increases endotracheal cuff pressure and the incidence of tracheal lesions in anesthetized patients. Anesth Analg. 1999;89:187–90. doi: 10.1097/00000539-199907000-00033. [DOI] [PubMed] [Google Scholar]
- 10.Beebe DS. Complications of tracheal intubation. Semin Anesth Perioperat Med Pain. 2001;20:166–72. [Google Scholar]
- 11.Combes X, Schauvliege F, Peyrouset O, Motamed C, Kirov K, Dhonneur G, et al. Intracuff pressure and tracheal morbidity influence of filling with saline during nitrous oxide anesthesia. Anesthesiology. 2001;95:1120–4. doi: 10.1097/00000542-200111000-00015. [DOI] [PubMed] [Google Scholar]
- 12.Nordin U. The trachea and cuff induced tracheal injury. Acta Otolaryngol Suppl. 1977;345:1–71. [PubMed] [Google Scholar]
- 13.Sengupta P, Sessler D, Maglinger P, Wells S, Vogt A, Durrani J, et al. Endotracheal tube pressure in three hospitals, and the volume required to produce an appropriate cuff pressure. BMC Anesthesiol. 2004;4:8. doi: 10.1186/1471-2253-4-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nordin U. The trachea and cuff induced tracheal injury: An experimental study on causative factors and prevention. Acta Otolaryngol Suppl. 1976;345:1–71. [PubMed] [Google Scholar]
- 15.Fernandez R, Blanch L, Mancebo J, Bonsoms N, Artigas A. Endotracheal tube cuff pressure assessment: Pitfalls of finger estimation and need for objective measurement. Crit Care Med. 1990;18:1423–6. [PubMed] [Google Scholar]
- 16.Braz JR, Navarro LH, Takata IH, Nascimento Junior P. Endotracheal tube cuff pressure: Need for precise measurement. Sao Paulo Med J. 1999;17:243–7. doi: 10.1590/s1516-31801999000600004. [DOI] [PubMed] [Google Scholar]
- 17.Parwani V, Hoffman RJ, Russell BC, Preblick C, Hahn IH. Practicing paramedics cannot generate or estimate safe endotracheal tube cuff pressure using standard techniques. Prehosp Emerg Care. 2007;11:307–11. doi: 10.1080/10903120701348248. [DOI] [PubMed] [Google Scholar]
- 18.Guyton D, Banner MJ, Kirby RR. High-volume, low-pressure cuffs. Are they always low pressure? Chest. 1991;100:1076–81. doi: 10.1378/chest.100.4.1076. [DOI] [PubMed] [Google Scholar]
- 19.Christensen AM, Willemoes-Larsen H, Lundby L, Jakobsen KB. Postoperative throat complaints after tracheal intubation. Br J Anaesth. 1994;73:786–7. doi: 10.1093/bja/73.6.786. [DOI] [PubMed] [Google Scholar]
- 20.Hähnel J, Treiber F, Konrad F, Eifert B, Hahn R, Maier B, et al. Trachealabdichtung, Spitzenzentrierung und Inzidenz postoperativer Halsbeschwerden. [A comparison of different endotracheal tubes. Tracheal cuff seal, peak centering and the incidence of postoperative sore throat.] Anaesthesist. 1993;42:232–7. [PubMed] [Google Scholar]
- 21.Kloub R. Sore throat following tracheal intubation. Middle East J Anesth. 2001;1:29–40. [PubMed] [Google Scholar]
- 22.Biro P, Seifert B, Pasch T. Complaints of sore throat after tracheal intubation: A prospective evaluation. Eur J Anesthesiol. 2005;22(4):307–11. doi: 10.1017/s0265021505000529. [DOI] [PubMed] [Google Scholar]


