Abstract
Background:
The objective of the present study was to compare the onset, degree and recovery time of sensory and motor block and hemodynamic effects of intrathecal bupivacaine alone and bupivacaine with sufentanil or butorphanol in endoscopic urological surgeries.
Methods:
In a randomized, double-blind study, 90 patients of either sex and age, belonging to ASA Grades I and II, scheduled for elective endoscopic urological surgeries under spinal anesthesia, were allocated into three groups of 30 each. Patients received either 2.5 ml of 0.5% hyperbaric buypivacaine 12.5 mg (Group A), 1.5 ml of 0.5% hyperbaric bupivacaine 7.5 mg with 10 μg sufentanil (Group B) or 1.5 ml of 0.5% hyperbaric bupivacaine 7.5 mg with 25 μg butorphanol (Group C). Vital parameters, level, duration and regression of sensory block and motor block and side-effects were recorded and compared.
Statistical Analysis:
Analysis of variance (ANOVA), post hoc test and Chi-square test were used.
Results:
Intrathecal addition of sufentanil/butorphanol prolonged the duration of sensory block (DOSB) compared with bupivacaine alone (DOSB being 156.83±23.83 min, 170.87 ± 22.21 min and 171.17 ± 23.99 min in groups A, B and C, respectively) without altering the duration of motor blockade. Bromage score 3 was achieved in 100%, 90% and 54.4% patients in groups A, B and C, respectively. The time to first request for analgesia was 112 ± 46.3 min, 323 ± 65.0 min and 299 ± 73.9 min in groups A, B and C, respectively. Complications were reduced by the addition of butorphanol, which also has a lower tendency than sufentanil to produce pruritus (60%).
Conclusions:
The analgesia was significantly prolonged in groups B and C; group C had a less-intense motor block. Complications were reduced by the addition of butorphanol, which also has a lower tendency than sufentanil to produce pruritus. Thus, this combination of butorphanol with low-dose bupivacaine is especially beneficial in the geriatric group of patients who have multiple co-morbid conditions.
Keywords: Butorphanol, intrathecal adjuvants, sufentanil
INTRODUCTION
Opioids and local anesthetics administered together intrathecally have a potent synergistic effect, improving the quality of intraoperative and postoperative analgesia. A combination of these agents allows for a reduction in the dose of both the classes of drugs, lessening the likelihood of side-effects attributable to each, which is particularly beneficial in geriatric patients.[1,2] Urological surgeries being largely restricted to the geriatric population pose a challenge as intravenous crystalloid and vasopressor administration to prevent hypotension may be detrimental to such patients.[2]
Based on “Combination Wisdom,” fentanyl was used widely with minidose bupivacaine in the mid-eighties. Sufentanil, an N-4 theinyl derivative of fentanyl, has significant differences in pharmacokinetic properties.[3–8] Reduced dose of bupivacaine with sufentanil provides successful anesthesia and stability of cardiac output, which is especially important in the elderly.[9]
Butorphanol is a synthetic lipoophilic opioid analgesic used in epidural analgesia and in animal studies,[10–12] but there are very few studies in the literature on the clinical characteristics of intrathecal butorphanol.[13] We therefore conducted the present study to evaluate the efficacy of intrathecal sufentanil and butorphanol as adjuvants to bupivacaine in various endoscopic urological procedures.
METHODS
This was a prospective, double-blind, randomized study. After obtaining approval from the hospital ethics committee and written informed consent, 90 patients of either sex and age, belonging to ASA Grades I and II, scheduled for elective endoscopic urological surgeries under spinal anesthesia, were randomly divided in a double-blind manner into three groups of 30 patients each using a computer-generated random number list.
Group A (Control): Patients were given subarachnoid block with 2.5 ml of 0.5% hyperbaric buypivacaine.
Group B: Patients were given subarachnoid block with 1.5 ml of 0.5% hyperbaric bupivacaine and 10 μg sufentanil.
Group C: Patients were given subarachnoid block with 1.5 ml of 0.5% hyperbaric bupivacaine and 25 μg butorphanol.
The procedure of giving subarachnoid block was carried out by a senior anesthesiologist and data was collected by another anesthesiologist who was unaware of the nature and volume of the drug given.
Patients with neurological disease, spinal deformities, mental disorders, local skin infection or disease, history of anaphylaxis to local anesthetics; sufentanil and butorphanol, coagulation disorders, severe liver disease, impaired renal functions, weight >100 kg and opioid dependence were excluded from the study.
Patients were kept nil per orally for at least 6 h prior to surgery. In premedication, diazepam 10 mg and ranitidine 150 mg orally was given on the night before surgery and diazepam 5 mg with ranitidine 150 mg orally was given at 6.00 am in the morning on the day of surgery.
On arrival in the operation theater, an intravenous (IV) infusion was started in all the patients with ringer's lactate solution and they were monitored for heart rate, noninvasive blood pressure, respiratory rate and oxygen saturation.With strict aseptic precautions, subarachnoid block was given at the level of L 3-4 intervertebral space using a 26 G quincke's needle at the rate of approximately 0.2 ml/s in lateral position and the patient was immediately turned to supine position.
Level of sensory block was determined by pinprick test every 2 min until the level had established. The maximum upper level of sensory block and the time taken to attain this maximum upper level was recorded by another anesthesiologist who was unaware of the type of drug administered.
Motor block of the lower extremities was measured according to the modified Bromage scale every 2 min till the achievement of Bromage score 3 or up to a maximum of 15 min, whichever was earlier. Definition of motor blockade was according to the modified Bromage scale.
-
0
- able to flex the whole lower limb at the hip
-
1
- able to flex the knee but unable to raise the leg at the hip
-
2
- able to planter flex the ankle but unable to flex the knee
-
3
- no movement of lower limb
Motor block was assessed and graded at the end of surgery and then at 15-min intervals using the modified Bromage scale. Time until full return of lower extremity motor function (Score = 0) was noted.
The quality of postoperative analgesia was assessed using a 0–10 linear visual analogue scale (VAS) every 15 min until the first request of supplement analgesia. Side-effects such as nausea, vomiting, hypotension (systolic blood pressure <90 mmHg or fall in systolic blood pressure >20% of baseline value), bradycardia (heart rate <50 beats/min), pruritus, respiratory depression (respiratory rate <10 breaths/min or oxygen saturation <90%) or any other complication were noted. Follow-up was carried out 48 h postoperatively for any side-effects. Hypotension was treated with incremental doses of mephentermine (3 mg) intravenously and bradycardia was treated with injection atropine intravenously.
The data obtained were subjected to statistical analysis using analysis of variance (ANOVA), post hoc test and Chi-square test with a P-value of <0.05 as significant.
RESULTS
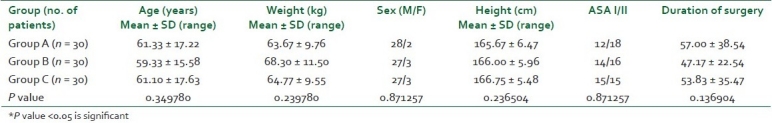
Patients in all the three groups were comparable in terms of age, sex, weight, height, ASA physical status, preoperative hemodynamic variables and duration of surgery, i.e. factors that would have influenced the block[14] [Table 1].
Table 1.
Distribution of subjects according to demographic profile
The characteristics of sensory block in the three groups are summarized in Tables 2 and 3. There was no difference between groups B and C in the time to reach peak level (9.9 min and 10.43 min, respectively) and in the median value highest level of block as assessed by needle prick (T9). But, a higher level of median value of sensory block (T6) was achieved in a shorter period of time (9.17 min) in group A. Addition of sufentanil and butorphanol significantly prolonged the duration of sensory block (DOSB) compared with bupivacaine alone (DOSB being 156.83 ± 23.83 min, 170.87 ± 22.21 min and 171.17 ± 23.99 min in groups A, B and C, respectively).
Table 2.
Characteristics of sensory block
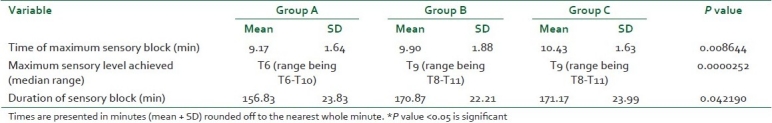
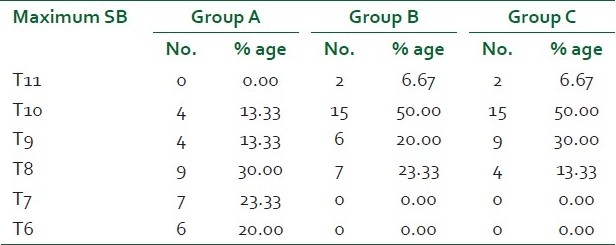
Table 3.
Distribution of subjects according to maximum upper level of sensory block
Regarding motor block characteristics [Table 4], in group A, a majority of the patients achieved complete motor block (100%) in comparison with patients in group B (90%) and group C (54.5%), who had a Bromage score of 3. The duration of motor block was 132±20.8 min, 130±23.2 min and 131±23.6 min, respectively in groups A, B and C.
Table 4.
Characteristics of motor block and analgesic requirement
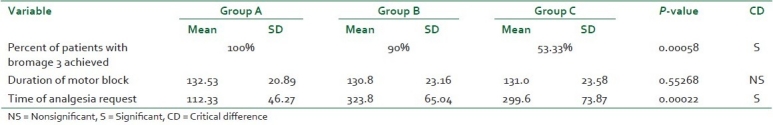
On intergroup comparison, VAS was of a significantly higher value in group A than in groups B and C. The trend of increase in VAS was significantly earlier in group A as compared with groups B and C. No significant difference in VAS scores was observed between groups B and C (P-value < 0.05) [Figure 1]. The time to first request for analgesia was noted postoperatively and was compared between the three groups. It was 112 ± 46.3 min, 323 ± 65.0 min and 299 ± 73.9 min in groups A, B and C, respectively [Table 4].
Figure 1.
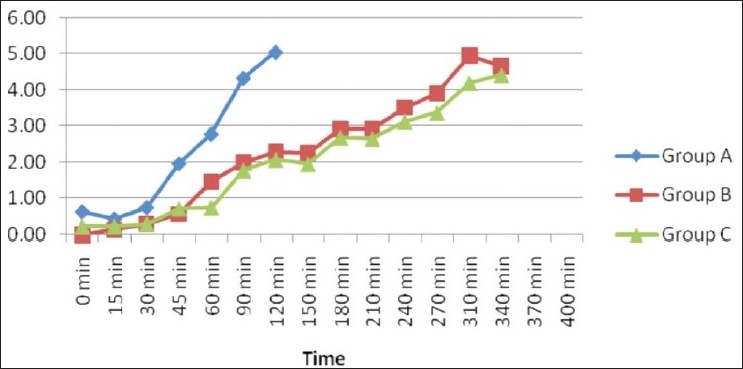
Trends in postoperative visual analogue scale
All the patients in the three study groups showed a statistically significant decrease in heart rate and mean blood pressure. However, this decrease was clinically nonsignificant. The magnitude of decrease (critical difference) was lesser in groups B and C as compared with group A with regard to trends in intraoperative heart rate as well as mean blood pressure. There were no significant variations observed in respiratory rate in any of the groups both intraoperatively and postoperatively.
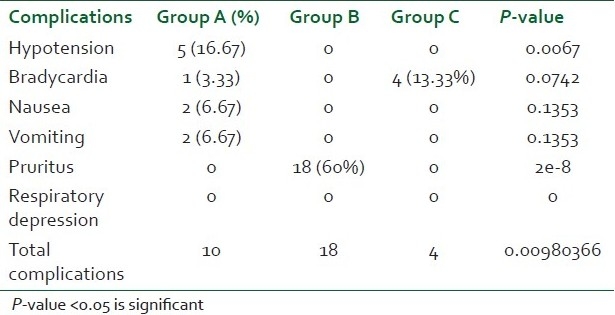
Side-effects observed [Table 5] in this study included hypotension, bradycardia, nausea, vomiting, pruritus and respiratory depression. Incidence of hypotension was highest in group A (16.67%) as compared with groups B and C, which was statistically significant. The incidence of nausea and vomiting was statistically insignificant in group A. Pruritus was observed in 60% of the patients in the sufentanil group (highly significant P value), with the intensity of pruritus being tolerable and not requiring any treatment. No episode of respiratory depression and desaturation was observed in any of the groups.
Table 5.
Comparison of perioperative side-effects
DISCUSSION
Perioperative complications impeding the effective and safe use of spinal anesthesia are hemodynamic instability in extremes of age. Most of such patients undergoing endoscopic urological procedures are elderly, and a majority of them have coexisting cardiac, pulmonary and other co-morbid conditions. Different techniques to lower the incidence of the above hemodynamic complications include unilateral spinal anesthesia, use of low-dose local anesthetics and addition of narcotics or other adjuvants to local anesthetics.
Although low-dose bupivacaine reduced the cardiovascular effects, it was not enough to provide an adequate level of sensory block.[14] Intrathecal opioids are synergistic with local anesthetics and intensify the sensory block without increasing the sympathetic block.[9,15]
“Combination Wisdom” allows the use of a lower dose of the local anesthetic agent with adjuvants, which offers hemodynamic stability. Opioids in conjunction with local anesthetics improve the quality of intraoperative analgesia and prolong the duration of postoperative analgesia.[16]
Local anesthetics such as bupivacaine act mainly by blockade of voltage-gated Na+ channels in the axonal membrane and presynaptic inhibition of calcium channels.[17] The μ-agonists sufentanil and butorphanol exert their action by opening the K+ channels and reducing the Ca++ influx, resulting in inhibition of transmitter release.[18,19] A combination of these effects may explain the observed synergism between bupivacaine and sufentanil/butorphanol. The synergism is characterized by enhanced somatic analgesia without an effect on the degree or level of local anesthetic-induced sympathetic or motor blockade.[19]
The principal findings of this study are that the addition of 10 μg sufentanil or 25 μg butorphanol to spinal anesthesia with hyperbaric 0.5% bupivacaine intensifies the sensory blockade and increases the duration of sensory blockade without increasing the intensity of motor blockade and requirement of rescue analgesia. These findings are in consistence with the findings of Vinita et al. and Dahlgren et al.[13,20]
The onset of sensory block was significantly more rapid in group A (9.17 ± 1.64 min) as compared with groups B and group C, which had an onset of 9.90 ± 1.88 min and 10.43 ± 1.63 min, respectively. This is in accordance with previous studies by Dahlgren et al.,[20] who noticed that the group receiving sufentanil 5 μg had a much delayed onset of spinal anesthesia in parturients. The maximum upper level of sensory block achieved was higher in the group of patients administered bupivacaine alone (T6) as compared with the sufentanil–bupivacaine (T9) and butorphanol–bupivacaine groups (T9).
Both these adjuvant opioids did not cause any significant increase in motor blockade and their combination with bupivacaine may thus be used for ambulatory analgesia. This was consistent with previous studies.[13,21] Butorphanol combination causes less-intense motor blockade than sufentanil combination with bupivacaine.
VAS was significantly of a higher value in group A than in groups B and C. The trend of increase in the median value of VAS was significantly earlier in group A as compared with groups B and C. There was a significant prolonged duration of analgesia in all the patients enrolled in the sufentanil group and the butorphanol group over the bupivacaine-alone group. Our results were similar to Dahlgren et al. And Courtney et al.[20,22] who demonstrated that the addition of sufentanil 5.0 μg and 7.5 μg to hyperbaric bupivacaine significantly prolonged the duration of analgesia compared to bupivacaine alone.
Regarding side-effects, the incidence of hypotension was observed in group A and not in groups B or C. Endoscopic urological surgeries are carried out in elderly patients wherein hypotension is more hazardous because they may have decreased physiological reserve and compromised blood supply to various vital organs.[23] Also, to avoid procedure-related complications like TURP syndrome, restricted fluid has to be administered, which is unavoidable with ongoing hypotension, which were more prevalent in group A. Opioids delivered by the spinal route decrease the dose of bupivacaine but may produce nausea, vomiting, urinary retention and respiratory depression and pruritus as the side-effects. In this study, the primary side-effects were pruritus with sufentanil combination and bradycardia with butorphanol combination. In other studies, the incidence of pruritus varied from 70.3 to 80% analgesia with 10 μg intrathecal sufentanil combination with bupivacaine.[24,25] Vinita et al. found a 20% incidence of sedation in the butorphanol group, but all the patients were arousable and it was not associated with respiratory depression, which was not present in our study group.
The practice of low-dose local anesthetic with adjuvant is gaining momentum in ambulatory settings because it is a safe, rapid, inexpensive technique with lower postoperative morbidity. Small-dose bupivacaine provides successful anesthesia and gives better cardiac output stability than a large dose.[9] Sufentanil or butorphanol use in various endoscopic urological procedures should be promoted in view of reduced incidence of hemodynamic adverse effects in the geriatric population. The sample size in our study was small but had significantly important results, and we suggest future studies to be undertaken with a larger population size.
CONCLUSIONS
To conclude, our study favors the use of sufentanil (10 μg) or butorphanol (25 μg) combination with low-dose hyperbaric bupivacaine (7.5 mg) in elderly patients undergoing endoscopic urological procedures, e.g. TURP in spinal anesthesia, because:
This combination prolongs the duration of sensory block.
Provides appropriate sensory level for patients undergoing endoscopic urological surgeries. Sensory levels above T9 are undesirable as pain due to perforation of the prostatic capsule (like in TURP, TURBT) will not be apparent to the patient if this complication occurs, so higher levels as in group A are undesirable.[26]
The intensity and the duration of motor block achieved with this combination favored early ambulation. Butorphanol combination provides less intense motor block than sufentanil combination.
Provides effective and better quality of analgesia.
Hemodynamic stability with these combinations.
Comparing side-effects, butorphanol has the advantage of not having pruritus as a side-effect.
Hence, this combination of sufentanil and butorphanol with low-dose bupivacaine in spinal anesthesia is equally acceptable clinically in terms of characteristics of sensory block, motor block, duration of analgesia and greater hemodynamic stability as compared with bupivacaine alone. Complications were reduced by the addition of butorphanol, which also has a lower tendency than sufentanil to produce pruritus. Thus, this combination of butorphanol with low-dose bupivacaine is especially beneficial in the geriatric group of patients, who have multiple co-morbid conditions.
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared.
REFERENCES
- 1.Ben-David B, Frankel R, Arzumonov T, Marchevsky Y, Volpin G. Minidose Bupivacaine-Fentanyl Spinal Anaesthesia for Surgical Repair of Hip fracture of aged. Anesthesiology. 2000;92:6–10. doi: 10.1097/00000542-200001000-00007. [DOI] [PubMed] [Google Scholar]
- 2.McCrae AF, Wildsmith JA. Prevention and treatment of hypotension during central neuraxial block. Br J Anesth. 1993;70:672–80. doi: 10.1093/bja/70.6.672. [DOI] [PubMed] [Google Scholar]
- 3.Buggy D, Higgins P, Moran C, O’Brien D, O’Donovan F, McCarroll M. Prevention of spinal anaesthesia induced hypotension in the elderly; comparison between preanesthetic administration of crystalloids, colloids and no prehydration. Anesth Analg. 1997;84:106–10. doi: 10.1097/00000539-199701000-00020. [DOI] [PubMed] [Google Scholar]
- 4.Stahl KD, Van Bever W, Janssen P, Simon EJ. Receptor affinity and pharmacological potency of a series of narcotic analgesic, anti-diarrheal and neuroleptic drugs. Eur J Pharmacol. 1977;46:199–205. doi: 10.1016/0014-2999(77)90334-x. [DOI] [PubMed] [Google Scholar]
- 5.Meuldermans WE, Hurkmans RM, Heykants JJ. Plasma Protein binding and distribution of fentanyl, sufentanil, alfentanil and lofentanil in blood. Arch Int Pharmacodyn Ther. 1982;257:4–19. [PubMed] [Google Scholar]
- 6.Bovill JG, Sebel PS, Blackburn CL, Oei-Lim V, Heykants JJ. The Pharmacokinetics of sufentanil in surgical patients. Anesthesiology. 1984;61:502–6. doi: 10.1097/00000542-198411000-00004. [DOI] [PubMed] [Google Scholar]
- 7.de Lange S, Boscoe MJ, Stanley TH, Pace N. Comparison of sufentanil-O2 and fentanyl-O2 for coronary artery surgery. Anesthesiology. 1982;56:112–8. doi: 10.1097/00000542-198202000-00006. [DOI] [PubMed] [Google Scholar]
- 8.de Lange S, Boscoe MJ, Stanley TH, de Bruijin N, Philbin DM, Coggins CH. Antidiuretic and growth hormone responses during coronary artery surgery with sufentanil-oxygen and alfentanil-oxygen anesthesia in man. Anesth Analg. 1982;61:434–8. [PubMed] [Google Scholar]
- 9.Asehnaue K, Larousse E, Tadie Jm, Minville V, Droupy S, Benhamou D. Small dose bupivacaine- sufentanil prevents cardiac output modifications after spinal anaesthesia. Anesth Analg. 2005;101:1512–5. doi: 10.1213/01.ANE.0000180996.91358.CC. [DOI] [PubMed] [Google Scholar]
- 10.Hurle MA, Goirigolzarri I, Valdizan EM. Involvement of the cyclic AMP system in the switch from tolerance into supersenstivity to the antinociceptive effect of the opioid sufentanil. Br J Pharmacol. 2000;130:174–80. doi: 10.1038/sj.bjp.0703304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wongchanpai W, Tsang BK, HOI K. Antinociceptive effect of intrathecal butorphanol through opioid receptors: Compared to morphine. Pharmacol Biochem Behav. 1998;61:910–5. doi: 10.1016/s0091-3057(97)00558-3. [DOI] [PubMed] [Google Scholar]
- 12.Wongchanapai W, Tsang BK, He Z, Ho IK. Relative involvement of spinal opioid receptors in physical dependence on intrathecal butorphanol and morphine. Pharmacol Biochem Behav. 1998;60:899–907. doi: 10.1016/s0091-3057(98)00074-4. [DOI] [PubMed] [Google Scholar]
- 13.Singh V, Gupta LK, Singh GP. Comparison among intrathecal fentanyl and butorphanol in combination with bupivacaine for lower limb surgeries. J Anesth Clin Pharmacol. 2006;22:371–5. [Google Scholar]
- 14.Lambert DH. Factors influencing spinal anaesthesia. Int Anesthesiol Clin. 1989;27:1320. doi: 10.1097/00004311-198902710-00004. [DOI] [PubMed] [Google Scholar]
- 15.Braga Ade F, Braga FS, Poterio GM, Pereira RI, Reis E, Cremonesi E. Sufentanil added to hyperbaric bupivacaine for subarachnoid block in caesarean section. Eur J Anaesthesiol. 2003;20:631–5. doi: 10.1017/s0265021503001017. [DOI] [PubMed] [Google Scholar]
- 16.Maves TJ, Gebhart GF. Antinociceptive synergy between intrathecal morphine and lidocaine during visceral and somatic nociception in the Rat. Anesthesiology. 1992;76:91–9. doi: 10.1097/00000542-199201000-00014. [DOI] [PubMed] [Google Scholar]
- 17.Butterworth JF, 4th, Strichartz GR. Molecular mechanism of L.A.: A review. Anesthesiology. 1990;72:71–4. doi: 10.1097/00000542-199004000-00022. [DOI] [PubMed] [Google Scholar]
- 18.Tejwani GA, Rattan AK, McDonald JS. Role of spinal opioid receptors in the antinociceptive interactions between intrathecal morphine and bupivacaine. Anesth Analg. 1992;74:726–34. doi: 10.1213/00000539-199205000-00018. [DOI] [PubMed] [Google Scholar]
- 19.Akerman B, Arwestrom E, Post C. Local anaesthetics potentiate spinal morphine antinociception. Anesth Analg. 1988;67:943–8. [PubMed] [Google Scholar]
- 20.Dahlgren G, Hultstrand C, Jakobsson J, Norma M, Eriksson EW, Martin H. Intrathecal sufentanil, fentanyl or placebo added to bupivacaine for cesarean section. Anesth Analg. 1997;85:1288–93. doi: 10.1097/00000539-199712000-00020. [DOI] [PubMed] [Google Scholar]
- 21.Hamilton CL, Cohen SE. High Sensory Block after Intrathecal Sufentanil for Labor Analgesia. Anesthesiology. 1995;83:1118–21. doi: 10.1097/00000542-199511000-00028. [DOI] [PubMed] [Google Scholar]
- 22.Courtney MA, Bader AM, Hartwell B, Hauch M, Grennan MJ, Datta S. Perioperative analgesia with subarachnoid sufentanil administration. Reg Anesth. 1992;17:274–8. [PubMed] [Google Scholar]
- 23.Lim HH, Ho KM, Choi WY, Teoh GS, Chiu KY. The use of intravenous atropine after a saline infusion in the prevention of spinal anaesthesia induced hypotension in elderly patients. Anesth Analg. 2000;91:1203–6. doi: 10.1097/00000539-200011000-00029. [DOI] [PubMed] [Google Scholar]
- 24.Ferouz F, Norris MC, Arkoosh VA, Leighton BL, Boxer LM, Corba RJ. Baricity, needle direction, and intrathecal sufentanil labor analgesia. Anesthesiology. 1997;6:592–8. doi: 10.1097/00000542-199703000-00010. [DOI] [PubMed] [Google Scholar]
- 25.Karaman S, Kocabas S, Uyar M, Hayzaran S, Firat V. The effects of sufentanil or morphine added to hyperbaric bupivacaine in spinal anaesthesia for Caesarean section. Eur J Anaesthesiol. 2006;23:285–91. doi: 10.1017/S0265021505001869. [DOI] [PubMed] [Google Scholar]
- 26.Malhotra V. Transurethral resection of the prostate. Anesthesiol Clin North America. 2000;18:883–97. doi: 10.1016/s0889-8537(05)70200-5. [DOI] [PubMed] [Google Scholar]


