Abstract
As students at the David Geffen School of Medicine at UCLA, the student authors were given the opportunity to develop their own creative projects which would be used to teach future medical students. They chose their own topics, planned and researched their projects, and then implemented the projects in interactive digital Adobe Flash files. In the first project they created interactive case-based radiology teaching files. In the second project they integrated photographic images into the existing illustrative anatomy files. Students in subsequent years have learned from these files on computers both at home and in the school's anatomy lab. The experience of creating the files served as an opportunity for hands-on learning for the student authors, both of the material and of the practice of teaching. In this paper they describe why they undertook these projects, what exactly they did, and the impact their creation had on them. The projects demonstrate that student-driven educational materials are both possible and beneficial. Furthermore, their experience has allowed them to conclude that faculty at other medical schools should consider providing students with opportunities to develop their own creative projects that contribute to the curriculum.
Keywords: creative project, teaching, anatomy, radiology, medical school curriculum
The first two years of education at the David Geffen School of Medicine at UCLA are generally made up of faculty-driven lectures, labs, and problem-based learning (1). However, students are free to choose how to spend eight weeks in the summer between first and second years. One option is to contribute to the school's digital educational materials, either by improving existing materials or by designing, researching, and creating new materials.
While such contributions are beneficial in multiple ways, one aspect of key importance is learning how to teach. To design the materials, students must think about how people learn and translate that into the actual production of the new learning materials. Although generally acknowledged to be an important skill, the ability to teach is not directly addressed in most medical school curricula. For doctors, teaching is of prime importance in educating not only medical students but also colleagues and patients. According to the 2009 medical school graduation questionnaire by the Association of American Medical Colleges, 32.6% of graduating medical students in the United States indicate that they are interested in becoming academics/full-time university faculty (2). For such students, the experience in teaching is particularly valuable, if not crucial.
The value of the student in medical curriculum development has been well described previously (3, 4). Administrators, medical educators, and students alike have attested to the benefit of the student perspective in curriculum review and development. One author described the contribution students can make as promoting a ‘consumer-friendly curriculum’ (4). Indeed, it stands to reason that students are uniquely positioned to offer feedback based on their first-hand experiences with the curriculum and their understanding of what it is like to be a student at a particular point in time (4). For instance, we noticed a limitation of our existing anatomy educational files in that they included drawn representations only, so we started a project to create photographic correlates. The curricula improvements are customized to the specific needs of the school and its students, allowing for expanding specialty areas and filling in missing pieces. As each school's curriculum is individually specialized, so too can be its improvements. By continual revision of the teaching materials and new creative projects run by students under the tutelage of faculty members, the curriculum may become more student-friendly, and thus may improve every year. Furthermore, involving students in the development of new teaching materials may improve their knowledge and skills, and ultimately create better doctors and better outcomes for patients.
Medical students can provide a creative resource in a medical school, as they are motivated, have a diverse array of backgrounds and experiences, and have ideas which are outside the traditional academic box. One medical school benefited from its students’ unique understanding through implementation of a student-created website to consolidate, integrate, and develop web resources for their peers (5). Another school described the use of student-generated digital teaching modules in its clinical anatomy course (6). As digital resources are utilized more heavily in medical school, the input and perspective of medical students as a younger generation more familiar with the technology will become ever more valuable.
Our Projects
After a whirlwind first year of medical school, we entered what would be our last summer break with a number of exciting opportunities and experiences to choose from to fill our two months. Many of our classmates started research projects to continue their process of discovery in their field of interest. But we took advantage of the opportunity to sit down with one of our anatomy professors and examine the curriculum we had just completed. Based on our unique perspective, we discussed what could be improved to optimize the learning experience for future classes, and then made it happen.
Interactive digital files produced by the anatomy faculty and made in Adobe Flash are the primary educational medium for presenting the vast amount of material that the first-year medical student is required to know for anatomy, histology, and radiology at the David Geffen School of Medicine. At the beginning of the summer, we formed a panel of students who volunteered to edit and provide feedback on the new generation of digital files that were being created. In the first few panel meetings, a number of ideas were discussed and inspired several independent projects. Based on our own interests, we came up with specific additions that we thought would benefit the current curriculum and discussed these with faculty members. They encouraged us to develop these ideas into our own projects and gave us resources to make them happen, such as the graphic designers at the Integrative Anatomy Design Center at UCLA.
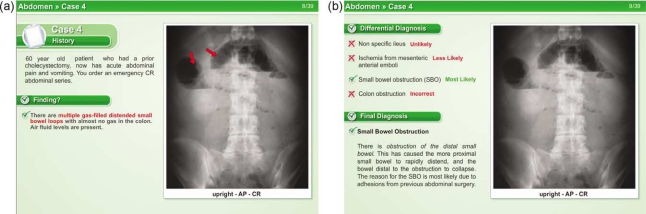
The first of these projects involved the radiology teaching files, which are integrated throughout the first- and second-year curriculum to teach basic radiologic anatomy. We noted that while the existing radiology files pointed out the important structures on radiographic images, they were lacking in clinical context. We developed new digital files to present the material in an interactive case-based format that included the classic findings of common injuries and diseases, differential diagnoses, and clinical correlations. Dozens of cases were organized and compiled into a large anthology and sent out to the class the following year. An example of a typical case (Fig. 1) shows a brief history of a 60-year-old patient with a prior cholecystectomy who now presents with acute abdominal pain and vomiting; students are asked to interpret an abdominal plain film for findings, differential diagnosis, and final diagnosis. Once the answers are chosen, the student clicks a button and the correct answers are revealed. Over the course of the summer, we completed radiology case files for the head and neck, thorax, abdomen, pelvis, spine, upper extremity, and lower extremity.
Fig. 1.
Representative screenshots from radiology case module demonstrate the combination of imaging with interactive questions.
The second project we chose to undertake involved the anatomy curriculum, a centerpiece of first-year medical curricula nationwide and a defining experience for us as first-year students. In our anatomy course, students learn the required material through both the study of cadavers and reading a variety of digital files showing illustrations of anatomical structures. Students have access to the files at home for preparation and review, as well as in the lab to use as references to locate structures in cadavers and visualize the important spatial relationships.
In our experience, however, these idealized color-coded diagrams were strikingly different from what we saw in our cadavers. We decided to enhance the existing illustrated files by adding labeled photographic images of cadaveric dissections (Fig. 2). We reviewed the existing files to determine what we thought would be helpful to future students, and then made our ideas reality using digital cameras to photograph dissected cadavers as well as views of our own unique cadaveric dissections. One of the new dissections we performed was a layer-by-layer approach to the brachial plexus, which we knew by personal experience to be one of the more challenging concepts to learn in the upper extremity region. We integrated the photographic images into existing anatomy laboratory modules; students can now compare the illustrated and photographic views of cadavers side by side, enhancing integrative learning of idealistic and real-life anatomy.
Fig. 2.
Students using the files in the anatomy lab.
Reflections
We found the experience of creating these new learning materials to be both exciting and fulfilling. The projects enabled us to expand upon particular interests in a way that has historically not been encouraged in traditional medical school curricula. By working on projects that we found interesting, we enjoyed learning about and exploring our chosen topics. The option of being able to choose projects and the methods for carrying them out gave us a sense of ownership, control, and responsibility for making them into good final products. Over the following years we have been thrilled to see our creations used and appreciated by subsequent classes (Box 1), and this signified for us that our effort was well spent.
Box 1. Comments solicited from students in subsequent classes who learned from our files.
‘It was incredibly helpful to be able to visualize true human anatomy in the case files, especially when it came to complex systems of nerves and arteries such as the brachial plexus. The ability to highlight different vessels and quiz myself using the modules was a great study tool. Finally, being able to access such focused, real-life modules out of the anatomy lab allowed me to study anatomy at home as well, which was invaluable in keeping a balanced schedule during anatomy-heavy blocks. I wish they had used more cadaver images - I don't remember there being very many!’
‘I did use the radiology case files. These were particularly helpful in reviewing concepts that Dr. Zucker had gone over in lecture. Being able to link an image to an actual patient made it easier to remember certain disease processes on tests.’
‘I am a student who needs to quiz myself to learn and it was really helpful to have cases that were applicable to the radiology images on which to quiz myself. Questions and patients always help me remember images more, so that was extremely useful. More of the files should be that way!’
Working on these files proved to be a rigorous learning opportunity. In the process of trying to organize and present the information in order to teach it, we were forced to think deeply about it. Similar to studying a disease for a patient we are treating, we needed to consider and apply the information carefully. This active learning process gave us a solid grasp of the material, and we will remember it longer and understand it better than if we had studied it in a textbook or heard it in a lecture. One could argue that students should be able to learn the material equally well from a textbook or lecture, but we propose that experiental, active learning is more beneficial to student mastery, and, furthermore, more akin to the style of lifelong learning we expect to encounter in medicine.
In addition to learning the material, working on these projects helped us sharpen several skills that are fundamental to the practice of medicine: how to create, how to collaborate, how to find opportunities for quality improvement, and, importantly, how to teach. Although generally acknowledged to be important skills, these are not addressed formally in most current medical school curricula. Being a part of the educational material development process has inspired us to take our ideas and manifest them in concrete ways. It has given us experience in creating which we can apply in diverse future endeavors, from presenting a lecture to writing a textbook chapter or making the next generation of digital learning technologies.
The goal of our projects was to educate future medical students, and the work of creating our materials gave us important practice in teaching. We needed to consider how best to present the information to make it understandable and memorable. This experience has helped prepare us for teaching in the future, which as doctors will be integral to our professional lives as we undertake the teaching of colleagues both formally in lecture settings and informally in the hospital or clinic. Perhaps more importantly, throughout our careers we will be teaching our patients about their diagnoses, treatments, and ways to live a healthy life. We would argue that teaching is at the core of what being a doctor is all about, and that our experience in these projects has been invaluable in making us better teachers in our professional careers.
Conclusion
We found that our projects could serve as valuable educational resources for both ourselves and other medical students. For us, the projects served as an effective exercise in teaching and active learning. For other students, the projects are useful in terms of the material taught and as examples which can be expanded in future educational projects. We were able to complete these projects because we were welcomed into an environment that encouraged us to do so. We are grateful to our faculty for providing us with an opportunity and structure in which we felt we could be creative. We worked with an established digital file structure, but other schools could accomplish similar projects through other media such as webpages or PowerPoint files with equal success. The key aspect which enabled us to work on these projects was medical educators being open to including students in educational material development. We encourage other schools to use our experience as a base upon which to build and expand their own student-driven projects.
Conflict of interest and funding
The authors have not received any funding or benefits from industry or elsewhere to conduct this study
References
- 1.Wilkerson L, Wimmers P, Doyle LH, Uijtdehaage S. Two perspectives on the effects of a curriculum change: student experience and the United States medical licensing examination, step 1. Acad Med. 2007;82:S117–20. doi: 10.1097/ACM.0b013e318141f4f0. [DOI] [PubMed] [Google Scholar]
- 2.Washington, DC: Association of American Medical Colleges; 1995–2010. Medical school graduation questionnaire. Available from: http://www.aamc.org/data/gq/ [Google Scholar]
- 3.Eichna LW. Medical-school education, 1975–1979. A student's perspective. N Engl J Med. 1980;303:727–34. doi: 10.1056/NEJM198009253031304. [DOI] [PubMed] [Google Scholar]
- 4.Huppatz C. The essential role of the student in curriculum planning. Med Educ. 1996;30:9–13. doi: 10.1111/j.1365-2923.1996.tb00710.x. [DOI] [PubMed] [Google Scholar]
- 5.Rosenbaum BP, Gorrindo TL, Patel SG, McTigue MP, Rodgers SM, Miller BM. Medical student involvement in website development. Med Teach. 2009;31:627–33. doi: 10.1080/01421590802206713. [DOI] [PubMed] [Google Scholar]
- 6.Philip CT, Unruh KP, Lachman N, Pawlina W. An explorative learning approach to teaching clinical anatomy using student generated content. Anat Sci Educ. 2008;1:106–10. doi: 10.1002/ase.26. [DOI] [PubMed] [Google Scholar]