Abstract
Purpose
To compare the prevalence of high out-of-pocket burdens among patients with cancer with other chronically ill and well patients, and to examine the sociodemographic characteristics associated with high burdens among patients with cancer.
Methods
The sample included persons 18 to 64 years of age who received treatment for cancer, taken from a nationally representative sample of the US population from the 2001 to 2008 Medical Expenditure Panel Survey. We examined the proportion of persons living in families with high out-of-pocket burdens associated with medical spending, including insurance premiums, relative to income, defining high health care (total) burden as spending more than 20% of income on health care (and premiums).
Results
The risk of high burdens is significantly greater for patients with cancer compared with other chronically ill and well patients. We find that 13.4% of patients with cancer had high total burdens, in contrast to 9.7% among those with other chronic conditions and 4.4% among those without chronic conditions. Among nonelderly persons with cancer, the following were associated with higher out-of-pocket burdens: private nongroup insurance, age 55 to 64 years, non-Hispanic black, never married or widowed, one child or no children, unemployed, lower income, lower education level, living in nonmetropolitan statistical areas, and having other chronic conditions.
Conclusion
High burdens may affect treatment choice and deter patients from getting care. Thus, although a detailed patient-physician discussion of costs of care may not be feasible, we believe that an awareness of out-of-pocket burdens among patients with cancer is useful for clinical oncologists.
INTRODUCTION
In recent years, because of emerging technologies and changing diagnostic and treatment patterns, cancer-related expenditures have risen and are expected to rise faster than those in any other area of health care.1,2 The rising economic burden of cancer care on patients has been acknowledged by the American Society of Clinical Oncology, which recommended in its guidance statement on the cost of cancer care that patient-physician discussion regarding the cost of care be recognized as an important component of high-quality care and that resources be developed to educate patients about the costs of treatment and guide them in choosing treatment options.3 On the other hand, a recent study found that between 1987 and the period of 2001 to 2005, the share of cancer costs financed by private insurance rose from 42% to 50%, whereas the out-of-pocket share fell from 17% to 8%, suggesting that out-of-pocket burdens of cancer treatment are declining.4 Thus, whether and to what extent the rising costs of cancer treatment are leading to high out-of-pocket burdens for patients with cancer are empirical questions.
Many previous studies have focused on lifetime or annual costs of cancer.5–9 Our focus instead is on out-of-pocket burdens. High out-of-pocket burdens can reduce access to care and may affect treatment choice. Recent studies have shown that cancer survivors are more likely to delay or forgo medical treatment compared with those without cancer.10,11 Furthermore, in a recent survey, 84% of oncologists reported that patients' out-of-pocket spending influenced treatment recommendations.12 Because of differences in benefit generosity, utilization and burdens may vary significantly by type of insurance.13,14 Most nonelderly families have employer-sponsored insurance. In 2002 and 2003, 69% of nonelderly families had access to employer coverage, and 96% of these families had private health insurance.15 Thus, loss of employment may lead to loss of health insurance coverage. Studies have shown that cancer-related needs can lead to loss of employment and income.16–19 The key features that distinguish our study are that first, we examined health care burdens relative to income, and second, we included expenditures on health insurance premiums in our total burden measure, providing a more accurate picture of health-related financial strain.
In this report, we compare the prevalence of high burdens among patients with cancer with other chronically ill and well patients. Next, we examine the variation in burdens among patients with cancer by insurance status and identify other sociodemographic characteristics associated with high burdens.
METHODS
Data
The data are from the Medical Expenditure Panel Survey–Household Component (MEPS-HC), sponsored by the Agency for Healthcare Research and Quality (Rockville, MD). Every year, the MEPS panel is selected from among a sample of households that participated in the National Health Interview Survey (NHIS) in the previous year. MEPS is a 2-year rotating panel of households designed to yield nationally representative estimates of health care expenditures for the civilian, noninstitutionalized population. Data are collected through five rounds of interviews and include information on medical expenditures, insurance coverage and premiums, and other socioeconomic characteristics.20
Summarizing response rates for our sample was difficult, because there are eight panels and multiple rounds within each panel. Taking into account the NHIS response rate, 74.3% of MEPS-eligible households provided data for all of the first three rounds of 2001, computed as the product of round-specific response rates (81%, 95%, and 96% in rounds one, two, and three, respectively).
For the burden analysis among patients with cancer receiving treatment, we pooled 2001 to 2008 MEPS-HC data (2 years from panels six to 12 and 1 year from panel 13) to obtain a sample large enough to make reliable estimates for subgroups of patients with cancer. The unit of observation was a person 18 to 64 years of age. The pooled sample included 4,243 persons with cancer and 148,971 persons not receiving cancer treatment. Adults receiving treatment for cancer were those who reported any medical events associated with cancer during the calendar year.
For the after-tax burden analysis, we used the 2004 MEPS-HC, the most recent year for which simulated taxes are available. We simulated state and federal income taxes as well as Social Security and Medicare taxes. State and federal income taxes were simulated using the National Bureau of Economic Research TAXSIM model available at http://www.nber.org/∼taxsim/.
To examine burdens among cancer survivors who were not actively receiving treatment, we used the NHIS-MEPS linked sample. We could not use MEPS to identify cancer survivors from 2001 to 2007, because before 2007, survey participants were asked only about current conditions. However, cancer survivors are identified in the NHIS questionnaire for one randomly selected adult per household. The NHIS-MEPS linked sample for 2001 to 2008 includes 2,105 persons receiving cancer treatment, 2,005 cancer survivors not receiving cancer treatment, and 59,597 persons without cancer.
Measure of Out-of-Pocket Burdens
Our burden measure included out-of-pocket expenditures for all health care services, because health care burdens among those with cancer may be greater than the cost of cancer treatment. Health care burdens were defined at the family level as the share of family-level pretax income spent on health-related expenditures, because family members generally share financial resources. Families were defined as health insurance eligibility units (ie, persons related by blood, marriage, or adoption who would typically be eligible for coverage under a private family policy). Family-level burdens were then assigned to individuals within the family, and the results are presented at the person level, enabling us to quantify the number of persons at risk for high health care expenditure burdens.
In keeping with the literature, high burdens were defined as health-related spending in excess of 20% of income.21–25 Although there is no consensus on what constitutes affordable costs, our results are robust when we use alternative thresholds such as 10% and 30%. Health care burden includes expenditures on all health care services. Total burden includes out-of-pocket expenditures on health insurance premiums in addition to out-of-pocket expenditures on health care services.
Two main methods used elsewhere in the literature are first, the population mean of the burden ratio, and second, the ratio of aggregate out-of-pocket expenditures to aggregate income.26 Unlike these alternative measures, which are based on means, our approach identified those with the highest burdens, given the right-skewed distribution of expenditures.
Cancer and Other Medical Conditions
Our analysis is based on treated prevalence (ie, persons who reported medical treatment for cancer anytime during a year). Medical conditions were collected from households verbatim and coded by professional coders using the International Classification of Diseases, Ninth Revision (ICD-9). Condition categories were created using the AHRQ Clinical Classification Software (CCS), which compiles ICD-9 codes into clinically meaningful categories.27
We classified persons into three mutually exclusive categories: cancer (ie, persons with one or more medical events [ambulatory visits, hospital, prescription medications, or other services] associated with CCS codes 11 to 45); other chronic condition (ie, persons with no medical events associated with cancer but with one or more medical events associated with other chronic conditions); and no chronic condition (ie, persons with no medical events associated with cancer or any other chronic condition). Chronic conditions were defined based on the fully specified ICD-9-CM diagnosis codes using the Healthcare Cost and Utilization Project Chronic Condition Indicator.28
Most skin cancers are not fatal, and some studies exclude skin cancers other than melanoma. However, because our focus was on financial burdens, our analysis includes all skin cancers. Our results when we excluded CCS code 23 (other nonepithelial skin cancer) were virtually identical.
Insurance Status
The nonelderly population, 18 to 64 years of age, was classified into four insurance categories: private group (employment-related) insurance, private nongroup (individual) insurance, public insurance, and no coverage. Persons with no private or public coverage anytime during the year were classified as having no coverage. Persons with multiple types of coverage during the year were assigned the coverage with the longest duration based on monthly insurance indicators. It is important to distinguish between the two types of private insurance, because nongroup insurance is generally more expensive and provides less generous benefits.29
Health Insurance Premiums
In MEPS, out-of-pocket premiums are collected from household respondents for private group and nongroup coverage. Although we focused on the nonelderly population, the burden measure includes health-related expenses for all family members. Therefore, we also simulated Medicare Part B premiums, taking into account that Medicaid pays Part B premiums for Medicare beneficiaries enrolled in Medicaid. Only 4.4% of nonelderly patients with cancer (190 of 4,243) lived in a household that included an elderly person. All premium amounts were prorated to account for the duration of coverage during the year.
Income
We constructed family-level income, adding income for all persons in the health insurance eligibility unit. We imposed a $100 floor for family income to deal with cases in which families had very low or negative incomes. The $100 income floor affected only 2.9% of the observations in our sample. Our results were not sensitive to this adjustment.
Expenditures by Service Type
Expenditures were classified into four service categories: hospital stays, ambulatory visits, prescription medications, and all other services. Ambulatory care visits included office-based provider visits and outpatient visits. Prescription medications included all purchases of medications prescribed for the treatment of any condition. All other services included emergency room visits, home health visits, dental visits, and other medical expenditures.
All expenditure amounts were converted using the Consumer Price Index for all urban consumers and reported in 2008 US dollars. Although the Personal Health Care Price Index is recommended for inflating health care expenditures, for our purposes, the Consumer Price Index was the most appropriate, because both income and expenditures needed to be adjusted using the same inflator.
All estimates were weighted to represent the US civilian noninstitutionalized population. SEs were corrected to account for the complex design of MEPS, with Taylor series linearization of the variance. Statistically significant differences are indicated in the tables, and only differences statistically significant at the 5% level are discussed in the text.
RESULTS
How do patients with cancer compare with other chronically ill and well patients in terms of out-of-pocket burdens?
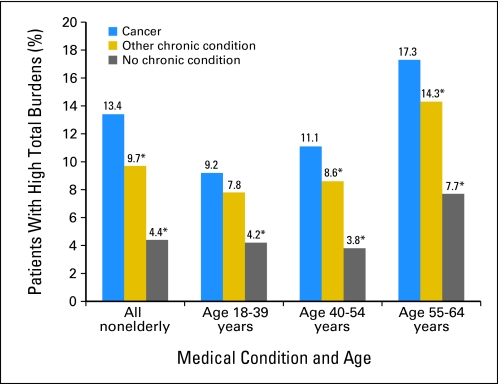
Nonelderly adults with cancer were significantly more likely to have high out-of-pocket burdens compared with other chronically ill and well patients. We found that 13.4% of nonelderly adults with cancer had high total burdens, in contrast to 9.7% of those with other chronic conditions and 4.4% of those without chronic conditions (Fig 1). Mean number of chronic conditions was significantly higher among patients with cancer compared with that among those with other chronic conditions (2.60 [SE, 0.04] v 2.15 [SE, 0.01]).
Fig 1.
Prevalence of high total burdens among nonelderly adults by medical condition and age. Calculations using the Medical Expenditure Panel Survey–Household Component, 2001 to 2008. Total burden includes out-of-pocket expenditures on health insurance premiums and health care services for all family members. (*) Difference from the reference category (cancer) is significant at the 1% level.
Although the prevalence of high burdens among patients with cancer and other chronically ill patients was similar among those age 18 to 39 years, among those age 40 to 54 and 55 to 64 years, patients with cancer were significantly more likely to have high burdens compared with those with other chronic conditions (Fig 1). Among those age 40 to 54 and 55 to 64 years, the number of chronic conditions among patients with cancer was significantly higher compared with that among those with other chronic conditions (2.36 [SE, 0.06] v 2.22 [SE, 0.01] and 3.30 [SE, 0.07] v 2.82 [SE, 0.02], respectively). Among those age 18 to 39 years, the difference in mean number of chronic conditions between patients with cancer and those with other chronic conditions was not significant (1.51 [SE, 0.07] v 1.61 [SE, 0.01]).
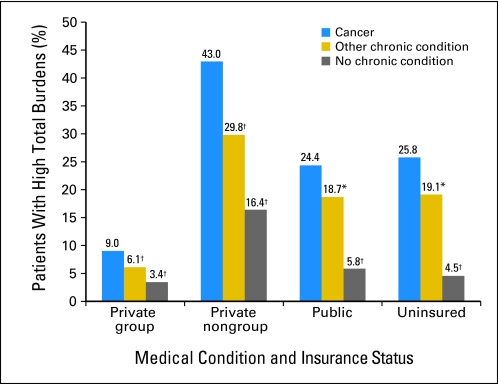
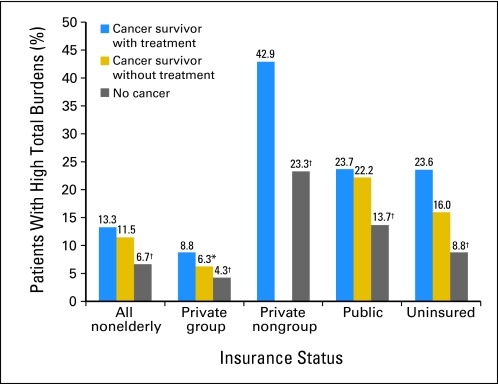
Even when we controlled for insurance status, we found that those with cancer had higher burdens compared with those with other chronic conditions. The difference in prevalence of high burdens was largest among those with private nongroup insurance: with high burdens among 43.0% of adults with cancer versus 29.8% of other chronically ill and 16.4% of well patients (Fig 2).
Fig 2.
Prevalence of high total burdens among nonelderly adults by medical condition and insurance status. Calculations using the Medical Expenditure Panel Survey–Household Component, 2001 to 2008. Total burden includes out-of-pocket expenditures on health insurance premiums and health care services for all family members. (*) Difference from the reference category (cancer) is significant at the 5% level. (†) Difference from the reference category (cancer) is significant at the 1% level.
How do burdens vary among patients with cancer by sociodemographic characteristics?
Table 1 presents out-of-pocket expenditures on health care and premiums, family income, and percentage with high health care and total burdens by sociodemographic characteristics. Among patients with cancer, those age 55 to 64 years, non-Hispanic blacks, those who were never married or widowed, those with one child or no children, those who were not working, those who were poorer, those with lower education levels, those who lived in nonmetropolitan statistical areas, and those with other chronic conditions were more likely to have high out-of-pocket burdens.
Table 1.
Prevalence of High Financial Burdens by Sociodemographic Characteristics Among Nonelderly Adults With Cancer: 2001 to 2008
| Characteristic | Average Annual Population (×1,000) | Out-of-Pocket Expenditures on Health Care ($) | Out-of-Pocket Expenditures on Health Care and Premiums ($) | Family Income ($) | Health Care Burden > 20% of Income (%) | Total Burden > 20% of Income (%) |
|---|---|---|---|---|---|---|
| Age, years | ||||||
| 18-39 | 1,156 | 1,636 | 3,034 | 58,643 | 7.1 | 9.2 |
| 40-54 | 2,124 | 2,520* | 4,620* | 84,536* | 7.2 | 11.1 |
| 55-64 | 2,535 | 3,057* | 5,695* | 77,446* | 10.1† | 17.3* |
| Sex | ||||||
| Male | 2,223 | 2,769 | 5,129 | 80,541 | 8.5 | 13.9 |
| Female | 3,592 | 2,460 | 4,554 | 73,673* | 8.4 | 13.1 |
| Race/ethnicity | ||||||
| White and other | 5,114 | 2,731 | 5,069 | 80,638 | 8.1 | 13.2 |
| Hispanic | 322 | 1,509* | 2,761* | 49,214* | 9.0 | 11.7 |
| Black (non-Hispanic) | 380 | 1,424* | 2,500* | 40,823* | 13.2† | 17.1 |
| Marital status | ||||||
| Married | 3,676 | 2,991 | 5,799 | 95,837 | 5.4 | 11.1 |
| Never married | 881 | 1,424* | 2,367* | 41,068* | 11.5* | 15.3† |
| Widowed/divorced/separated | 1,258 | 2,181* | 3,462* | 43,868* | 15.2* | 18.9* |
| No. of children in family | ||||||
| 0 | 4,307 | 2,612 | 4,775 | 73,873 | 9.2 | 14.8 |
| 1 | 729 | 2,388 | 4,649 | 81,752 | 8.2 | 11.4 |
| ≥ 2 | 779 | 2,569 | 4,878 | 84,599* | 4.6* | 7.8* |
| Employment status | ||||||
| Full time | 2,968 | 2,473 | 4,616 | 90,129 | 3.4 | 6.6 |
| Part time | 1,232 | 2,436 | 4,977 | 77,365* | 4.7 | 10.5* |
| Not working | 1,616 | 2,879 | 4,907 | 50,087* | 20.6* | 28.1* |
| Poverty category‡ | ||||||
| Poor | 563 | 1,748 | 2,442 | 7,385 | 45.0 | 48.9 |
| Near poor/low income | 661 | 2,231 | 3,821* | 21,378* | 17.7* | 29.7* |
| Middle income | 1,494 | 2,478* | 4,595* | 44,975* | 6.0* | 14.3* |
| High income | 3,097 | 2,852* | 5,487* | 115,673* | 1.0* | 3.1* |
| Education | ||||||
| Less than high school | 671 | 2,372 | 3,563 | 33,622 | 14.4 | 21.0 |
| High school | 1,634 | 2,462 | 4,601 | 59,350* | 10.4† | 17.3 |
| More than high school | 3,570 | 2,672 | 5,085† | 92,341* | 6.4* | 10.2* |
| Urbanicity | ||||||
| MSA | 4,812 | 2,567 | 4,808 | 79,774 | 8.1 | 12.7 |
| Non-MSA | 1,003 | 2,630 | 4,606 | 59,623* | 10.3 | 16.7† |
| Health status | ||||||
| Cancer only | 1,664 | 1,951 | 3,881 | 78,891 | 6.0 | 8.1 |
| Other chronic conditions | 4,151 | 2,830* | 5,131* | 75,259 | 9.4* | 15.5* |
NOTE. Calculations using Medical Expenditure Panel Survey–Household Component, 2001 to 2008. All monetary amounts are converted to 2008 US dollars using the Consumer Price Index for all urban consumers.
Abbreviations: FPL, federal poverty level; MSA, metropolitan statistical area.
Difference from the reference group (first row in each category) is significant at the 1% level.
Difference from the reference group (first row in each category) is significant at the 5% level.
Poor defined as income < 100% of FPL; near poor/low income defined as 100%-199% of FPL; middle income defined as 200%-399% of FPL; high income defined as ≥ 400% of FPL.
How do burdens vary among patients with cancer by insurance status?
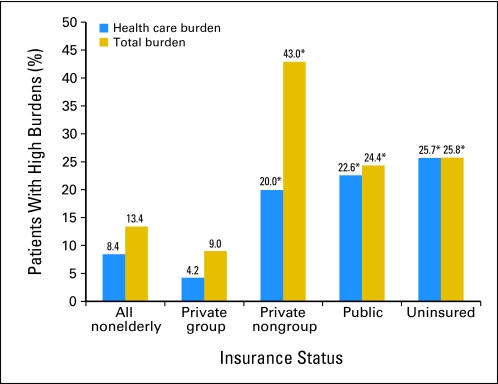
Among nonelderly adult patients with cancer, 78% (n = 4.5 million) had private group coverage, 5% (n = 270,000) had private nongroup coverage, 11% (n = 657,000) had public coverage, and 6% (n = 376,000) were uninsured. Figure 3 shows the prevalence of high health care and high total burdens by insurance status among patients with cancer. Focusing on health care burdens, we see that the uninsured were most likely to have high burdens (25.7%). However, in terms of total burdens, those with private nongroup insurance were most likely to have high burdens (43.0%), followed by the uninsured (25.8%), those with public insurance (24.4%), and those with private group insurance (9.0%).
Fig 3.
Prevalence of high out-of-pocket burdens among nonelderly adults receiving treatment for cancer by insurance status. Calculations using the Medical Expenditure Panel Survey–Household Component, 2001 to 2008. Health care burden includes out-of-pocket expenditures on health insurance premiums and health care services for all family members. (*) Difference from the reference category (private group) is significant at the 1% level.
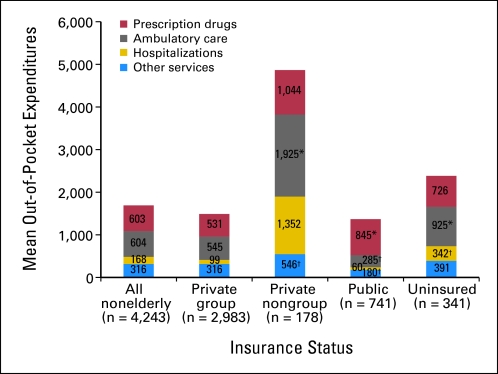
What services account for the largest share of out-of-pocket expenditures among patients with cancer?
Among all nonelderly patients with cancer, prescription drugs and ambulatory care services each accounted for 36%, hospitalizations accounted for 10%, and other services accounted for 19% of out-of-pocket expenditures. Compared with those with private group insurance, those with private nongroup coverage had significantly higher expenditures for ambulatory care and other services, those with public insurance had significantly higher expenditures for prescription drugs but lower expenditures for ambulatory care and other services, and the uninsured had significantly higher expenditures for ambulatory care and hospitalizations (Fig 4).
Fig 4.
Mean out-of-pocket expenditures by service type among nonelderly adults receiving treatment for cancer by insurance status. Calculations using the Medical Expenditure Panel Survey–Household Component, 2001 to 2008. Health care burden includes out-of-pocket expenditures on health insurance premiums and health care services for all family members. (*) Difference from the reference category (private group) is significant at the 5% level. (†) Difference from the reference category (private group) is significant at the 1% level.
Extensions and Sensitivity Tests
How do burdens change when we use after-tax income and expenditures?
Using after-tax income has two effects on burdens: first, health care expenses greater than 7.5% of adjusted gross income are tax deductible, lowering the after-tax burden of expenditures above the threshold, and second, after-tax income is significantly lower among the working age population, reducing the denominator of the burden measure. In our sample for 2004, mean pretax income was $79,908, whereas mean after-tax income was $62,026. Using the pretax method, 14.6% of patients with cancer had high burdens, whereas 16.5% had high burdens using the after-tax method. Thus, prevalence of high burdens among patients with cancer was 1.9 percentage points higher when using the after-tax method.
What is the prevalence of high burdens among cancer survivors who are not actively receiving treatment for cancer?
First, we verified that the prevalence of high total burdens among patients with cancer receiving treatment in MEPS and in the NHIS-MEPS linked sample were consistent: 13.4% (SE, 0.7%) in MEPS and 13.3% (SE, 0.9%) in the NHIS-MEPS linked sample. Figure 5 shows that the prevalence of high total burdens was 11.5% (SE, 0.9%) among cancer survivors not actively receiving treatment for cancer, 13.3% (SE, 0.9%) among cancer survivors receiving treatment, and 6.7% (SE, 0.2%) among those without cancer. Thus, for the nonelderly population overall, the prevalence of high burdens was not significantly different among cancer survivors receiving and not receiving treatment for cancer. Controlling for insurance status, we found that among those with private group coverage, the prevalence of high burdens was higher among cancer survivors receiving treatment compared with those not receiving treatment. We found no difference in the prevalence of burdens between cancer survivors receiving and not receiving treatment among the uninsured and those with public coverage. We could not examine the variation among those with private nongroup coverage because of sample-size limitations.
Fig 5.
Prevalence of high total burdens among cancer survivors receiving and not receiving treatment for cancer. Calculations using the National Health Interview Survey–Medical Expenditure Panel Survey linked sample, 2001 to 2008. Total burden includes out-of-pocket expenditures on health insurance premiums and health care services for all family members. Sample size was too small to make reliable estimates for cancer survivors with private nongroup insurance who were not receiving treatment. (*) Difference from the reference category (cancer survivor receiving treatment) is significant at the 5% level. (†) Difference from the reference category (cancer survivor receiving treatment) is significant at the 1% level.
DISCUSSION
We found that nonelderly adults with cancer were significantly more likely to have high out-of-pocket burdens compared with other chronically ill and well patients: 13.4% of nonelderly adults with cancer had high total burdens, in contrast to 9.7% of those with other chronic conditions and 4.4% of those without chronic conditions. Among patients with cancer, the following were associated with higher out-of-pocket burdens: private nongroup insurance, age 55 to 64 years, non-Hispanic black, never married or widowed, one child or no children, unemployed, lower income, lower education level, living in nonmetropolitan statistical areas, and having other chronic conditions. Furthermore, we found that even when not actively receiving treatment for cancer, expenditures among cancer survivors were higher than those among similar individuals without cancer.
In the near future, for nonelderly adults with cancer, the temporary national high-risk pool and state-based health insurance exchanges are likely to lower out-of-pocket burdens, especially among the currently uninsured and those with nongroup private insurance. There are some limitations to our study. First, note that our goal was to examine the prevalence of high burdens among persons with cancer. It is beyond the scope of this study, nor did we attempt, to disentangle the multiple potential causal relationships between cancer and burdens, such as loss of employment and reduced income caused by illness. Second, our burden measure was based on income and did not capture any medical debt or depletion of savings because of cancer treatment. Third, we could not examine the variation in burdens by cancer site and treatment type because of sample-size limitations or by stage of illness, which is not reported in MEPS.
Despite these limitations, MEPS is an ideal source for analyzing out-of-pocket burdens, because it includes all payers and components of expenditures, unlike claims data, which only include covered services. The National Cancer Institute, American Cancer Society, National Center for Chronic Disease Prevention and Health Promotion of the Centers for Disease Control, and Office of Behavioral and Social Science Research of the National Institutes of Health are jointly funding a cancer supplement to MEPS for the panel starting in 2011. This cancer supplement will enable researchers to examine medical expenditures among patients with cancer in more detail.
In conclusion, high out-of-pocket burdens may affect treatment choice and deter patients from getting care. We believe that our findings on the prevalence and sociodemographics associated with high burdens will be helpful for patients with cancer. Furthermore, although a detailed patient-physician discussion of insurance status and costs may not be feasible, we believe that an awareness of out-of-pocket burdens is also useful for clinical oncologists.
Supplementary Material
Footnotes
The views expressed in this article are those of the authors, and no official endorsement by the US Department of Health and Human Services or Agency for Healthcare Research and Quality is intended or should be inferred.
Authors' disclosures of potential conflicts of interest and author contributions are found at the end of this article.
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The author(s) indicated no potential conflicts of interest.
AUTHOR CONTRIBUTIONS
Conception and design: Didem S.M. Bernard
Administrative support: Stacy L. Farr
Collection and assembly of data: All authors
Data analysis and interpretation: All authors
Manuscript writing: All authors
Final approval of manuscript: All authors
REFERENCES
- 1.National Cancer Institute. Cancer Trends Progress Report: 2007 Update. http://progressreport.cancer.gov.
- 2.Dinan MA, Curtis LH, Hammill BG, et al. Changes in the use and costs of diagnostic imaging among Medicare beneficiaries with cancer, 1999-2006. JAMA. 2010;303:1625–1631. doi: 10.1001/jama.2010.460. [DOI] [PubMed] [Google Scholar]
- 3.Meropol NJ, Schrag D, Smith TJ, et al. American Society of Clinical Oncology guidance statement: The cost of cancer care. J Clin Oncol. 2009;27:3868–3874. doi: 10.1200/JCO.2009.23.1183. [DOI] [PubMed] [Google Scholar]
- 4.Tangaka FK, Trogdon JG, Richardson LC, et al. Cancer treatment cost in the United States: Has the burden shifted over time. Cancer. 2010;116:3477–3484. doi: 10.1002/cncr.25150. [DOI] [PubMed] [Google Scholar]
- 5.Elkin EB, Bach PB. Cancer's next frontier: Addressing high and increasing costs. JAMA. 2010;303:1085–1087. doi: 10.1001/jama.2010.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Howard DH, Molinari NA, Thorpe KE. National estimates of medical costs incurred by nonelderly cancer patients. Cancer. 2004;100:883–891. doi: 10.1002/cncr.20063. [DOI] [PubMed] [Google Scholar]
- 7.Warren JL, Yabroff KR, Meekins A, et al. Evaluation of trends in the cost of initial cancer treatment. J Natl Cancer Inst. 2008;100:888–897. doi: 10.1093/jnci/djn175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yabroff KR, Joan LW, Banthin JS, et al. Comparison of approaches for estimating prevalence costs of care for cancer patients? What is the impact of data source. Med Care. 2009;47(suppl 1):S64–S67. doi: 10.1097/MLR.0b013e3181a23e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Short PF, Moran JR, Punekar R. Medical expenditures of adult cancer survivors aged <65 years in the United States. Cancer. doi: 10.1002/cncr.25835. [epub ahead of print on December 23, 2010] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weaver KE, Roland JH, Bellizzi KM, et al. Forgoing medical care because of cost: Assessing disparities in healthcare access among cancer survivors living in the United States. Cancer. 2010;116:3493–3504. doi: 10.1002/cncr.25209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.The Kaiser Family Foundation. USA Today/Kaiser Family Foundation/Harvard School of Public Health National Survey of Households Affected by Cancer. http://www.kff.org/kaiserpolls/pomr112006pkg.cfm.
- 12.Neumann PJ, Palmer JA, Nadler E, et al. Cancer therapy costs influence treatment: A national survey of oncologists. Health Aff (Millwood) 2010;29:196–202. doi: 10.1377/hlthaff.2009.0077. [DOI] [PubMed] [Google Scholar]
- 13.Ward E, Halpern M, Schrag N, et al. Association of insurance with cancer care utilization and outcomes. CA Cancer J Clin. 2008;58:9–31. doi: 10.3322/CA.2007.0011. [DOI] [PubMed] [Google Scholar]
- 14.Thorpe KE, Howard DH. Health insurance and spending among cancer patients. Health Aff (Millwood) 2003;W3(suppl):189–198. doi: 10.1377/hlthaff.w3.189. [DOI] [PubMed] [Google Scholar]
- 15.Bernard DM, Banthin JS, Encinosa WE. Wealth, income, and the affordability of health insurance. Health Aff (Millwood) 2009;28:887–896. doi: 10.1377/hlthaff.28.3.887. [DOI] [PubMed] [Google Scholar]
- 16.Covinsky KE, Goldman L, Cook EF, et al. The impact of serious illness on patients' families: SUPPORT investigators—Study to understand prognoses and preferences for outcomes and risks of treatment. JAMA. 1994;272:1839–1844. doi: 10.1001/jama.272.23.1839. [DOI] [PubMed] [Google Scholar]
- 17.Lauzier S, Maunsell E, Drolet M, et al. Wage losses in the year after breast cancer: Extent and determinants among Canadian women. J Natl Cancer Inst. 2008;100:321–332. doi: 10.1093/jnci/djn028. [DOI] [PubMed] [Google Scholar]
- 18.Syse A, Tretli S, Kravdal O. The impact of cancer on spouses' labor earnings. Cancer. 2009;115(suppl):4350–4361. doi: 10.1002/cncr.24582. [DOI] [PubMed] [Google Scholar]
- 19.Arozullah AM, Calhoun AE, Wolf M, et al. The financial burden of cancer: Estimates from a study of insured women with breast cancer. J Support Oncol. 2004;2:271–278. [PubMed] [Google Scholar]
- 20.Cohen S. Sample Design of the 1997 Medical Expenditure Panel Survey Household Component: Methodology Report 11. Rockville, MD, Agency for Healthcare Research and Quality Pub. No. 01-0001, 2000.
- 21.Bernard DM, Banthin JS, Encinosa WE. Health care expenditure burdens among adults with diabetes in 2001. Med Care. 2006;44:210–215. doi: 10.1097/01.mlr.0000199729.25503.60. [DOI] [PubMed] [Google Scholar]
- 22.Selden TM, Banthin JS. Health care expenditure burdens among elderly adults: 1987 and 1996. Med Care. 2003;41(suppl):III13–III23. doi: 10.1097/01.MLR.0000076051.76245.19. [DOI] [PubMed] [Google Scholar]
- 23.Banthin JS, Bernard DM. Changes in financial burdens for health care: National estimates for the population younger than 65 years, 1996 to 2003. JAMA. 2006;296:2712–2719. doi: 10.1001/jama.296.22.2712. [DOI] [PubMed] [Google Scholar]
- 24.Banthin JS, Cunningham P, Bernard DM. Financial burden of health care, 2001-2004. Health Aff (Millwood) 2008;27:188–195. doi: 10.1377/hlthaff.27.1.188. [DOI] [PubMed] [Google Scholar]
- 25.Bernard DM, Banthin JS. Medicare Part D and health care expenditure burdens among the elderly: 2005 and 2007. Rockville, MD, Agency for Healthcare Research and Quality Working Paper, 2010.
- 26.Goldman DP, Smith JP. Methodological biases in estimating the burden of out-of-pocket expenses. Health Serv Res. 2001;35:1357–1365. discussion, 1365-1370. [PMC free article] [PubMed] [Google Scholar]
- 27.Agency for Healthcare Research and Quality. HCUP Clinical Classification Software: Healthcare Cost and Utilization Project (HCUP)—January 2011. Rockville, MD, Agency for Healthcare Research and Quality, 2011. www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp.
- 28.Healthcare Cost and Utilization Project. Chronic Condition Indicator for ICD-9-CM. http://www.hcup-us.ahrq.gov/toolssoftware/chronic/chronic.jsp.
- 29.Bernard DM, Banthin JB. Premiums in the Individual Health Insurance Market for Policyholders Under Age 65: 2002 and 2005. http://www.meps.ahrq.gov/mepsweb/data_files/publications/st202/stat202.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.