Abstract
This study was designed to evaluate the efficacy of the HealthWise South Africa HIV and substance abuse prevention program at impacting adolescents’ polydrug use and sexual risk behaviors. HealthWise is a school-based intervention designed to promote social-emotional skills, increase knowledge and refusal skills relevant to substance use and sexual behaviors, and encourage healthy free time activities. Four intervention schools in one township near Cape Town, South Africa were matched to five comparison schools (N = 4040). The sample included equal numbers of male and female participants (Mean age = 14.0). Multiple regression was used to assess the impact of HealthWise on the outcomes of interest. Findings suggest that among virgins at baseline (beginning of eighth grade) who had sex by Wave 5 (beginning of 10th grade), HealthWise youth were less likely than comparison youth to engage in two or more risk behaviors at last sex. Additionally, HealthWise was effective at slowing the onset of frequent polydrug use among non-users at baseline and slowing the increase in this outcome among all participants. Program effects were not found for lifetime sexual activity, condomless sex refusal and past-month polydrug use. These findings suggest that HealthWise is a promising approach to HIV and substance abuse prevention.
Introduction
HIV/AIDS and substance use are two significant threats to South African adolescents’ health. Among youth ages 15–19 years, approximately 3% of males and 7% of females are HIV positive; among youth ages 20–24 years, the prevalence increases dramatically to 5% of males and 20% of females [1]. Although substance use generally receives less publicity, a recent survey found that over 25% of ninth graders had used alcohol and/or cigarettes in the past-month and 21% of males and 7% of females had used marijuana [2]. These findings have important implications not only for later substance abuse [3, 4] but also for HIV transmission given that use of substances such as alcohol and marijuana may precede sexual risk behavior [5, 6]. Taken together, these findings indicate that there is an urgent need for comprehensive interventions aimed at promoting health and reducing sexual risk behaviors and substance use among South African youth.
The HealthWise program [7–9] was developed to meet this need. HealthWise was inspired by Botvin’s LifeSkills Training [10], Caldwell’s TimeWise: Taking Charge of Leisure [11] and best practices in sexual risk prevention. Theories that guided the development of the intervention include selective optimization with compensation [12, 13], Self-Determination Theory [14, 15] and Social Cognitive Theory [16]. HealthWise was designed based on the premise that increasing basic life skills, increasing knowledge of the risks of substance use and sexual behaviors and the skills needed to resist substance use and sex and providing and promoting healthy free time experiences will decrease substance use and sexual risk behaviors among youth. Therefore, HealthWise incorporates lessons aimed at developing social-emotional skills such as decision-making and stress and anger management, promoting prosocial attitudes, increasing knowledge and skills in regard to substance use and sex and encouraging engagement in personally meaningful healthy free time experiences (see Caldwell et al. [7] for a detailed description of HealthWise). Each of the 12 eighth grade lessons and 6 ninth grade booster lessons are delivered by teachers over two to three regularly scheduled class periods. In addition to the school-based curriculum, two Youth Development Specialists coordinate utilization of school and community resources and opportunities. Beginning in 2003, three subsequent cohorts of youth were involved in the HealthWise efficacy trial. Each cohort was followed for at least five waves of data collection. The results for Cohort 1 are promising [8, 17]. Relative to the comparison group of adolescents in comparable schools who received the government-mandated Life Orientation curriculum, the HealthWise group had smaller increases in recent alcohol and cigarette use, including heavy use, although the in some cases HealthWise impacted males and females differently. Female HealthWise participants were more likely to be non-smokers relative to the comparison group and male HealthWise participants were more likely to quit smoking [18]. No significant differences were found between the treatment and comparison group in regard to marijuana use.
The Cohort 1 results also suggest that HealthWise had positive effects on condom self-efficacy, knowledge of how to properly use a condom and knowledge of condom availability [8, 17]. No significant effects were found, however, in regard to sexual onset or past-month sexual activity and consistent use of condoms among sexually active youth. Although HealthWise has been implemented in a primarily Colored (mixed race of African, Asian and European descent) township, funding has been received to expand the implementation across different regions of South Africa with diverse populations.
In this study, we extend our evaluation of HealthWise by examining combined effects for Cohorts 1 and 2. Given the potential for cohort differences due to factors such as implementer familiarity with the intervention and participant characteristics, we tested for cohort differences in all analyses. Additionally, we expanded our analyses to also examine impacts on youth at highest risk of poor outcomes: polydrug users (lifetime, past-month and frequent) and those who engaged in high-risk behaviors at last sex (not using a condom, using alcohol or marijuana prior to sex and having sex with strangers). In congruence with Botvin and colleagues’ inclusion of alcohol, tobacco and marijuana in their definition of polydrug use [10, 19], we define polydrug use as use of two or more of these three substances. We also examined lifetime sexual activity and refusal to have sex due to the absence of condoms. As the HealthWise curriculum specifically focuses on each of these outcomes, we hypothesized that they would be more favorable for the HealthWise group relative to the comparison group. Given gender differences in our findings for Cohort 1, we also examined gender differences in this study.
Method
Data collection
HealthWise was implemented in Mitchell’s Plain, an under-resourced township near Cape Town, South Africa that was developed during Apartheid. Of the 25 schools in the area, six were deemed ineligible to participate due to perceived organizational incapacity. Of the 19 remaining schools, four were randomly selected to participate and receive both the pilot and finalized version of the HealthWise curriculum and five schools were selected to serve as the comparison group (four were matched to the treatment schools and one was selected as a back-up). The comparison schools were matched to the treatment schools based on the proportion of Afrikaans-taught classrooms, socioeconomic status and other demographic variables. All nine schools agreed to participate. Students in the comparison schools received the governmentally mandated Life Orientation curriculum, which differ substantially between schools and overlap minimally with HealthWise content [9].
Trained research staff administered questionnaires using personal digital assistants to youth who provided assent and had received parental consent to participate. Data were collected at the beginning and end of each school year, starting in the eighth grade. Data from Waves 1 (beginning of eighth grade) and 5 (beginning of 10th grade) were utilized in this study. The study protocol was approved by The Pennsylvania State University and Stellenbosch University IRBs. Cohort 1 data collection began in 2004 and Cohort 2 data collection began 1 year later in 2005.
Participants
Participants included 4040 youth (53% in Cohort 1 and 47% in Cohort 2; 38% treatment group and 62% comparison and 50% male). The mean age of participants at baseline was 14.0 (SD = 0.84). The majority of participants (88%) identified themselves as Colored, followed by Black (8%), White (3%) and Indian/Other (1%).
Measures
Lifetime polydrug use
Lifetime alcohol, tobacco and marijuana use were assessed with the questions ‘How many drinks of alcohol (including beer and wine) have you had in your entire life?’ (0 = none, 1 = part or all of 1 drink and 2 = more than 1 drink), ‘How many cigarettes have you smoked in your entire life?’ (0 = none, or a few puffs of 1 cigarette and 1= more than 1 cigarette) and ‘How many times have you used dagga [marijuana] in your entire life’ (0 = never, 1 = once and 2 = 2 or more times), respectively. Youth who indicated that they had not used any of the three substances (i.e. had scores of 0 on all three questions) were coded as 0 on the lifetime polydrug use scale. Youth who indicated that they had used one substance were coded as 1, those who had used 2 substances were coded as 2 and those who had used all three substances were coded as 3.
Past-month polydrug use
Youth who responded that they had used a particular substance in their lifetime were then asked about past-month use of that substance. Past-month alcohol, tobacco and marijuana use were assessed with the questions ‘During the past 4 weeks did you use alcohol (including beer and wine)?’, ‘During the past 4 weeks did you smoke cigarettes?’ and ‘During the past 4 weeks did you use dagga?’ (0 = no and 1 = yes), respectively.
Youth who indicated that they had not used any of the three substances in the past-month (or their lifetime) were coded as 0 on the past-month polydrug use scale. Youth who indicated that they had used one substance were coded as 1, those who had used 2 substances were coded as 2 and those who had used all three substances were coded as 3.
Frequent polydrug use
Youth who indicated past-month use of a particular substance also were asked about their frequency of use. Alcohol, tobacco and marijuana use were assessed with the questions ‘During the past 4 weeks how many alcoholic drinks did you have?’ (1 = 1 or less, 2 = 2–3 and 3 = 4 or more), ‘During the past 4 weeks how many cigarettes did you smoke?’ (1 = 1 or less, 2 = 2–9 and 3 = 10 or more) and ‘During the past 4 weeks how many times did you use dagga?’ (1 = 1 time, 2 = 2–3 times and 3 = 4 or more times).
Youth who reported (i) no lifetime use of a given substance or (ii) no past-month use of a given substance were coded as 0 on the frequent use variable for that substance. Additionally, for each of the three substances, youth were coded as 0 if their responses were less than 3 and coded as 1 if their responses equaled 3. Scores for the three substances were summed (0 = frequent use of no substances, 1= frequent use of 1 substance, 2 = frequent use of 2 substances and 3 = frequent use of 3 substances).
Lifetime sexual activity
Lifetime sexual activity was assessed with the question ‘Have you ever had sex? This means intimate contact with someone during which the penis enters the vagina (female private parts)’ (0 = no and 1 = yes).
Condomless sex refusal
All youth, regardless of their sexual status, were asked about condomless sex refusal with the question ‘Have you ever refused to have sex because you or your partner did not have a condom?’ (0 = no and 1 = yes).
Risk at last sex
Youth who indicated that they had engaged in lifetime sexual activity were asked several questions about their last sexual encounter. Four of these questions were used in order to create the risk at last sex scale: ‘The last time you had sex, did you or your partner use a condom?’ (0 = no and 1 = yes), ‘The last time you had sex, did you drink alcohol?’ (0 = no and 1 = yes), ‘The last time you had sex did you smoke dagga [marijuana]?’ (0 = no and 1 = yes) and ‘Thinking about the last time you had sex, how would you describe your relationship with that person?’ (0 = just met them that day, 1 = I’ve known them for a while and 2 = serious dating partner). The last question was recoded to indicate having sex with a stranger (I’ve known them for a while and serious dating partner responses = 0 and just met them that day = 1). Given the importance of condom use to the prevention of negative sexual consequences such as sexually transmitted infections, condom use was weighted more heavily than the other three risk behaviors. Thus, youth who indicated condom use at last sex were coded as 0; those who did not use condoms at last sex were coded as 1 if they did not engage in the other three risk behaviors, as 2 if they engaged in one other risk behavior, as 3 if they engaged in two other risk behaviors and as 4 if they engaged in three other risk behaviors. This risk index was analyzed as a continuous variable.
Missing data
Approximately 10% of the sample was lost to attrition at each wave (NTime 1 = 4040; NTime 5 = 2613). Similar to other longitudinal intervention studies, relative to youth who remained in the study at Wave 5, youth who dropped out of the study by Wave 5 were more likely to report risk behaviors at baseline (lifetime, recent and heavy polydrug use; lifetime sexual activity and risk at last sex). Due to the significant level of attrition, we utilized multiple imputation [20, 21] in order to obtain accurate parameter estimates. Each imputed dataset included the substance use and sexual behavior variables at each of the first five time points, as well as gender and dummy codes for race at baseline. We imputed data sets separately by treatment group. Given that only adolescents who had sex were asked follow-up questions about sexual risk behaviors, it was not practical to use multiple imputation to account for missing data in the follow-up questions. Thus, raw data were used to calculate the risk at last sex scale.
Analytic strategy
We utilized linear and logistic regression models to test the impact of HealthWise on the outcomes of interest, as well as cohort and gender differences in these impacts. Main effects were tested first, followed by two-way interactions (gender by treatment, gender by cohort and cohort by treatment) and three-way interactions (gender by treatment by cohort). Given known racial differences in the outcomes of interest [8, 22], we controlled for race in all analyses. Due to research suggesting that Black South African youth are at higher risk compared with youth of other races [22], race was dummy coded with Black youth as the reference group.
We conducted two sets of analyses for each outcome. In the first set of analyses, we examined data for all participants and controlled for baseline scores on the variables of interest. In the second set of analyses, we examined these relationships for youth who had not engaged in the outcome of interest at baseline (e.g. had a score of 0 on the lifetime polydrug use scale at baseline).
Results
Descriptive statistics
Baseline descriptive statistics for the independent and dependent variables are presented in Table I. The HealthWise group had a significantly higher percentage of Black youth relative to the comparison group. There were not any significant differences in terms of lifetime or past-month polydrug use or the number of risk behaviors at last sex. HealthWise youth were more likely to be sexually active relative to the comparison group. Additionally, HealthWise females were less likely to report that they refused sex due to not having condoms, and HealthWise males were more likely to report frequent polydrug use relative to the comparison group.
Table I.
Descriptive statistics at baseline by treatment status and gender
| Male |
Female |
|||||
| Variable | Comparison N = 1274 | HealthWise N =758 | χ2 | Comparison N = 1228 | HealthWise N = 780 | χ2 |
| Race | 22.75*** | 66.57*** | ||||
| Colored | 89 | 84 | 91 | 81 | ||
| Black | 6 | 12 | 5 | 15 | ||
| White | 4 | 3 | 3 | 3 | ||
| Indian | <1 | <1 | <1 | <1 | ||
| Other | <1 | <1 | <1 | <1 | ||
| Lifetime polydrug use | 1.04 | 5.13 | ||||
| 0 Substances | 41 | 39 | 50 | 50 | ||
| 1 Substance | 32 | 33 | 27 | 30 | ||
| 2 Substances | 21 | 23 | 20 | 16 | ||
| 3 Substances | 6 | 5 | 3 | 4 | ||
| Past-month polydrug use | 7.57 | 4.63 | ||||
| 0 Substances | 69 | 63 | 71 | 72 | ||
| 1 Substance | 20 | 25 | 19 | 21 | ||
| 2 Substances | 8 | 9 | 8 | 6 | ||
| 3 Substances | 3 | 3 | 2 | 1 | ||
| Frequent polydrug use | 8.41* | 1.16 | ||||
| 0 Substances | 85 | 81 | 86 | 86 | ||
| 1 Substance | 10 | 13 | 10 | 10 | ||
| 2 Substances | 4 | 5 | 3 | 3 | ||
| 3 Substances | 1 | 1 | 1 | 1 | ||
| Lifetime sexual activity | 16 | 22 | 9.27*** | 4 | 7 | 10.93*** |
| Condomless sex refusal | 40 | 43 | 1.40 | 41 | 36 | 3.84* |
| Risk behaviors at last sexual encountera | 3.68 | 3.24 | ||||
| 0 Risk behaviors | 59 | 64 | 58 | 54 | ||
| 1 Risk behavior | 23 | 15 | 16 | 29 | ||
| 2 Risk behaviors | 18 | 21 | 26 | 17 | ||
| 3 Risk behaviors | 0 | 0 | 0 | 0 | ||
| 4 Risk behaviors | 0 | 0 | 0 | 0 | ||
Among sexually active participants. ***P < 0.001, * P < 0.05.
Polydrug use
We present results for lifetime, past-month and frequent polydrug use for all participants (users and non-users) and then for non-users at baseline. Models with two-way interactions are presented in Table II; no three-way interactions were significant. In the analysis of all participants, there were not significant gender, cohort or treatment main effects for lifetime polydrug use. There was, however, a significant gender by treatment interaction (β = −0.15, SE = 0.07, P < 0.05), so we ran the main effects models separately for males and females. In order to better understand these findings, we used χ2 tests to examine the statistically significant differences in the number of substances used within gender (P < 0.001 for all comparisons). HealthWise males were slightly more likely to use two or more substances at baseline (34 versus 31%), but the percentage increase of substance use from baseline to Wave 5 (29%) was equal to the increase of the comparison group, indicating there was no effect of HealthWise on male polydrug use. On the other hand, at baseline HealthWise females were slightly less likely (23%) to use two or more substances than comparison females (25%). By Wave 5, the HealthWise females had a smaller increase (32%) in substance use than the comparison females (36%). This finding suggests that HealthWise had a positive effect by reducing the rate of increase in lifetime polydrug use among females.
Table II.
Regression models predicting lifetime, past-month and frequent polydrug use
| Lifetime polydrug use (all participants) | Lifetime polydrug use (non-users at baseline) | Past-month polydrug use (all participants) | Past-month polydrug use (non-users at baseline) | Frequent polydrug use (all participants) | Frequent polydrug use (non-users at baseline) | |
| β(SE) | β(SE) | β(SE) | β(SE) | β(SE) | β(SE) | |
| Intercept | 0.90 (0.08)*** | 0.92 (0.13)*** | 0.29 (0.05)*** | 0.21 (0.07)** | 0.24 (0.05)*** | 0.17 (0.06)** |
| Baseline use | 0.47 (0.02)*** | — | 0.33 (0.02)*** | — | 0.38 (0.03)*** | — |
| Race: Black versus White | 0.22 (0.13) | 0.34 (0.20) | 0.15 (0.09) | 0.17 (0.12) | 0.14 (0.08) | 0.12 (0.10) |
| Race: Black versus Colored | 0.43 (0.07)*** | 0.32 (0.10)** | 0.25 (0.05)*** | 0.20 (0.06)** | 0.23 (0.05)*** | 0.12 (0.05)* |
| Race: Black versus Other | 0.00 (0.22) | 0.17 (0.32) | 0.09 (0.14) | 0.15 (0.18) | −0.10 (0.13) | −0.07 (0.15) |
| Gender | 0.09 (0.05) | 0.04 (0.09) | −0.04 (0.03) | −0.03 (0.03) | −0.02 (0.04) | −0.02 (0.05) |
| Cohort | 0.00 (0.05) | −0.01 (0.10) | −0.00 (0.02) | 0.00 (0.03) | −0.04 (0.04) | −0.07 (0.05) |
| Treatment | 0.06 (0.06) | 0.19 (0.11) | −0.01 (0.02) | −0.01 (0.03) | −0.11 (0.04)* | −0.09 (0.05) |
| Gender by treatment | −0.15 (0.07)* | −0.23 (0.12)* | — | — | 0.00 (0.05) | 0.01 (0.06) |
| Cohort by treatment | −0.03 (0.07) | −0.01 (0.11) | — | — | 0.09 (0.05) | 0.12 (0.06)* |
| Cohort by gender | 0.02 (0.07) | 0.01 (0.11) | — | — | 0.01 (0.05) | 0.01 (0.06) |
***P < 0.001, **P < 0.01, *P < 0.05.
Similarly, among non-users at baseline, there were no significant gender, cohort, or treatment main effects for lifetime polydrug use but there was a significant gender by treatment interaction (β = −0.23, SE = 0.12, P < 0.05). In order to better understand this interaction, we ran the main effects model separately for males and females and used χ2 tests to examine the statistically significant differences in the number of substances used within gender (P < 0.001 for all comparisons). At Wave 5, HealthWise males had a slightly higher prevalence of using one (32 versus 30%), two (24 versus 23%) and three (20 versus 16%) substances relative to comparison males, whereas HealthWise females had a slightly lower prevalence of using two or more substances relative to comparison females (36 versus 40%).
Results of the main effects models for past-month polydrug use are presented in Table II. There were no significant main effects or interactions for gender, cohort or treatment in the analysis of all participants or the analysis of non-users at baseline.
There were no significant gender or cohort main effects for frequent polydrug use but there was a significant treatment main effect (all participants: β = −0.11, SE = 0.04, P < 0.05; non-users: β = −0.09, SE = 0.05, P < 0.05). In the analysis of all participants, frequent polydrug use was significantly lower among the HealthWise group. In the analysis of non-users at baseline, the HealthWise group had a significantly lower onset of frequent polydrug use than the comparison group (P < 0.10). Additionally, among non-users, there was a significant cohort by treatment interaction (β = 0.12, SE = 0.06, P < 0.05).
In order to better understand these findings, we used χ2 tests to examine the statistically significant differences in the number of substances used frequently within cohort (P < 0.001 for all comparisons). For Cohort 1, the onset of frequent use of two or more substances from baseline to Wave 5 was twice as high for the comparison group (6%) relative to the HealthWise group (3%). For Cohort 2, the onset of frequent use of two or more substances from baseline to Wave 5 was similar for HealthWise and comparison youth (5 versus 4%).
Sexual risk behaviors
Three types of sexual behaviors were examined in this study: lifetime sexual activity, condomless sex refusal and risk at last sex. These behaviors were examined for all participants (virgins and non-virgins at baseline) and then for virgins only at baseline.
Results of the main effects models for the sexual behavior variables are presented in Table III; there were not any significant interactions. There were no significant treatment effects for lifetime sexual activity but there were some gender and cohort differences. In both the analysis of all participants and the model with virgins at baseline, females were less likely to report lifetime sexual activity compared with males. In addition, youth in Cohort 1 were less likely to report lifetime sexual activity than youth in Cohort 2.
Table III.
Regression models predicting lifetime sexual activity, condomless sex refusal and risk behaviors at last sexual encounter
| Lifetime sexual activity (all participants) | Lifetime sexual activity (virgins at baseline) | Condomless sex refusal (all participants) | Condomless sex refusal (virgins at baseline) | Risk behavior at last sexual encounter (all participants) | Risk behaviors at last sexual encounter (virgins at baseline) | ||
| β(SE) | β(SE) | β(SE) | β(SE) | β(SE) | β(SE) | ||
| Intercept | 0.01 (0.17) | −0.05 (0.18) | −0.13 (0.18) | 0.06 (0.19) | 0.52 (0.35) | 0.59 (0.17)*** | |
| Baseline value | 1.22 (0.14)*** | — | 0.78 (0.08)*** | — | −0.12 (0.13) | — | |
| Race: Black versus White | −0.88 (0.28)*** | −0.78 (0.31)* | 0.22 (0.25) | 0.23 (0.30) | −0.47 (0.57) | 0.22 (0.29) | |
| Race: Black versus Colored | −0.92 (0.16)*** | −0.90 (0.16) | −0.19 (0.16) | −0.07 (0.17) | 0.03 (0.22) | 0.00 (0.12) | |
| Race: Black versus Other | −0.28 (0.48) | −0.40 (0.55) | −0.60 (0.48) | −0.62 (0.49) | 1.77 (1.00) | −0.40 (0.47) | |
| Gender | −0.75 (0.09)*** | −0.75 (0.10)*** | 0.04 (0.07) | 0.03 (0.07) | 0.13 (0.26) | 0.07 (0.08) | |
| Cohort | 0.16 (0.08)* | 0.20 (0.09)* | −0.05 (0.07) | −0.06 (0.08) | 0.04 (0.18) | −0.09 (0.08) | |
| Treatment | 0.02 (0.08) | 0.07 (0.09) | −0.06 (0.08) | 0.01 (0.08) | 0.09 (0.19) | −0.16 (0.08)* | |
***P < 0.001, *P < 0.05.
There were no gender, cohort or treatment effects in the analysis of condomless sex refusal. This was true for the analysis with all participants and the analysis with virgins at baseline.
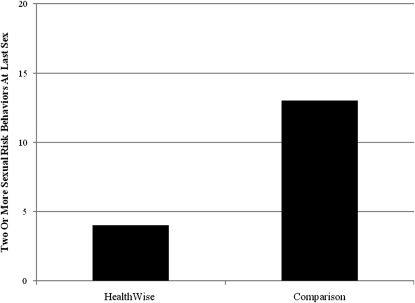
There was no significant treatment effect for risk at last sex in the analysis of all participants. Among virgins at baseline, there was a significant treatment effect in the expected direction for risk at last sex (β = −0.16, SE = 0.08, P < 0.05). In order to better understand these findings, we used χ2 analysis in order to understand group differences in the number of sexual risk behaviors. Of virgins at baseline who became sexually active by Wave 5, the HealthWise and comparison groups had the same prevalence of condom use at last sex at Wave 5 (72%). Among youth who did not use a condom, however, comparison youth were three times more likely to also engage in at least one other risk behavior at last sex (see Fig. 1). Although the same pattern held true for the combined sample of virgins and non-virgins, the results did not reach statistical significance.
Fig. 1.
Percentage of virgins at baseline who became sexually active by Wave 5 and engaged in two or more risk behaviors at last sex.
Discussion
Emerging research suggests that HealthWise is a promising HIV and substance abuse preventive intervention for South African youth [8, 17]. The purpose of this study was to extend the evaluation of HealthWise by examining gender and cohort differences in treatment effects of HealthWise on two outcomes at Wave 5 (post-test): polydrug use and sexual risk behaviors. Although the findings are modest and include some gender differences, results suggest that HealthWise was effective at reducing the behaviors associated with some of the poorest outcomes: frequent polydrug use and engaging in two or more sexual risk behaviors at last sex. A detailed discussion of the results follows.
Polydrug use
Youth who engage in frequent use of multiple substances are at increased risk of physical and psychological harm compared with non-users and light users. Therefore, one of the most promising findings in this study was that the HealthWise curriculum was effective at slowing both the onset of frequent polydrug use among non-users at baseline and the increase in this outcome among the whole sample. There was an indication that HealthWise was more effective at slowing the onset among baseline non-users in Cohort 1 than Cohort 2. This was the only cohort difference found in this study, which suggests that the impact of HealthWise was generally consistent across cohorts.
There were gender differences in regard to lifetime polydrug use. We ran the analyses separately for males and females and examined differences in the number of substances used in order to better understand these findings. For females, the effects were in the expected direction. For males, however, our interpretation of the significant interaction indicates no program effect on this lifetime outcome. The effect of HealthWise on frequent use, we believe, is more important than lifetime use given that lifetime use for some may have occurred prior to exposure to the program and may involve low levels of experimentation (as included in our definition of this variable). Given that there were gender differences in the impact of the intervention on substance use in this study and past HealthWise studies [8, 18], additional research clearly is needed to better understand the reasons for these differences, as well as ways to strengthen intervention impacts on substance use for both genders.
Sexual behavior
Given the tremendous need for effective HIV prevention programs in South Africa and internationally, the findings regarding the impact of HealthWise on risk behaviors at last sex are potentially important. Among virgins at baseline who became sexually active by Wave 5, nearly three-fourths of HealthWise and comparison youth reported condom use at their last sexual encounter. The high prevalence of condom use and lack of treatment effect on this outcome could be attributable to the fact that public health campaigns that emphasize condom use already are prevalent across South Africa [23]. Future research is needed to better understand the characteristics of the youth in this township area who do not report using condoms in order to design preventive interventions that effectively target this group. Research also is needed that explores the consistency of youths’ condom use over time, as well as the efficacy of preventive interventions at increasing consistent condom use.
Among those who did not use a condom, comparison youth were significantly more likely to also engage in at least one other risk behavior such as substance use or having sex with an unfamiliar partner compared with HealthWise youth. Although the findings for the analysis that combined virgins and non-virgins at baseline were not statistically significant, the same pattern held true.
These findings are consistent with past research on school-based HIV prevention programs [24] in that they highlight the need to target not only condom use but also other social and contextual factors in preventive interventions. Female adolescents in particular may have more control over factors such as alcohol and marijuana use and choice of partner than actual condom use, so reducing these risk behaviors represents an important step in the right direction. General concepts integrated into HealthWise such as healthy decision-making, as well as specific lessons on condom use, substance avoidance, negotiating risky situations and avoiding sex with new partners likely resulted in this finding. Future analyses will examine the specific mediators of the effects of HealthWise on sexual risk behaviors. These results, along with those from other intervention trials [24], indicate that prevention programs that spend the majority of time emphasizing condom use at the expense of discussing relational, contextual and structural variables may not be enough to make significant impacts on the HIV epidemic above and beyond those that have already been seen.
It is important to note that there were no treatment effects for lifetime sexual activity and condomless sex refusal. As part of reducing sexual risk, both of these are desirable goals. Among those who have never had sex, one of our objectives was to delay the onset of sexual activity. Among those who had already experienced sex, HealthWise aimed to promote the acceptability of ceasing sexual activity, especially if neither partner had a condom. Moving forward, our goal is to explore ways to modify the HealthWise curriculum in order to have broader impacts on sexual health. The fact that there were no treatment effects for lifetime sexual activity, but that there were treatment effects for risk behaviors at last sex among virgins at baseline suggests that with this population in particular, comprehensive sex education programs may have a greater public health impact than abstinence education curricula. Thus, we plan to maintain the comprehensive nature of HealthWise, yet modify it in appropriate ways in order to meet the needs of youth most at-risk of negative outcomes (e.g. youth who are already sexually active). Possible modifications include focusing more attention on the relational aspects of sexual behavior (e.g. partner and peer pressure), as well the individual, social and environmental factors that influence behavioral choices such as condom use.
As a whole, the mixed findings concerning the efficacy of HealthWise at changing sexual behaviors point to a need for additional research. To that end, we currently are in the process of expanding the implementation of HealthWise to all schools in the Southern Metro School District (one of the Cape Town school districts). The main purpose of this new trial will be to investigate three key independent variables hypothesized to influence implementation fidelity. The first two independent variables, teacher training and support, focus on how to prepare teachers and monitor their delivery of a prevention program with fidelity. The third independent variable, enhancement of school environment, concerns development of a school climate that supports the successful delivery of a prevention program. We will also evaluate the effectiveness of HealthWise on the student outcomes of interest.
The results shown here need to be understood in the general context of school-based prevention programs in South Africa. There have been very few longitudinal studies that have been rigorously evaluated. Of those, only one had an effect on behavior and that was only at a 6-month follow-up [25]. The effects of HealthWise, while modest, have both a longer follow-up period and apply to multiple risk behaviors, indicating that HealthWise may be a promising program.
Limitations and conclusions
It is important to consider several limitations when interpreting the results of this study. Most importantly, the fact that the data were collected in one under-resourced region of South Africa and included primarily Colored adolescents suggests that these findings may not generalize to South African adolescents of different races, with different economic circumstances or in different regions.
There were also limitations related to data collection. As all data were collected via self-report, adolescents may have distorted their true substance use and/or sexual activity based on perceived social expectations or fear of punishment. This, however, is true of all studies of this type. It is important to note that the surveys were not administered by teachers and participants were assured of the confidentiality of their responses in order to minimize this risk.
Additionally, there was a high rate of participant attrition by Wave 5. While the general consensus is that the missing data imputation procedures used here are the most precise way to handle attrition, we did perform separate analysis on dropouts. As with most longitudinal studies of adolescents, the results indicated that those at highest risk at baseline were more likely to drop out over the course of this study.
Despite these limitations, this study presents an important contribution to the health education literature as it furthers understanding of the efficacy of HIV and substance abuse prevention programs among South African youth, one of the populations most affected by the HIV/AIDS epidemic. These findings suggest that HealthWise has modest but important impacts on some of the highest risk substance use and sexual behaviors. Additionally, this study calls attention to the need to consider cohort and gender differences when evaluating the long-term efficacy of prevention and health promotion programs.
Funding
National Institutes of Health (R01 DA01749 to E.S., F31 DA024535 to M.T.).
Conflict of interest statement
None declared.
Acknowledgments
The authors would like to thank Dr Lori-Ann Palen for providing statistical consultation on the project. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Drug Abuse or the National Institutes of Health.
References
- 1.Shisana O, Rehle T, Simbayi LC, et al. South African National Prevalence, Incidence, Behaviour, and Communication Survey 2008: A Turning Tide Among Teenagers? Cape Town, South Africa: HSRC Press; 2009. [Google Scholar]
- 2.Plüddemann A, Flisher AJ, Mathews C, et al. Adolescent methamphetamine use and sexual risk behaviour in secondary school students in Cape Town, South Africa. Drug Alcohol Rev. 2008;29:1–6. doi: 10.1080/09595230802245253. [DOI] [PubMed] [Google Scholar]
- 3.Pitkanen T, Lyyra A-L, Pulkkinen L. Age of onset of drinking and the use of alcohol in adulthood: a follow-up study from age 8-42 for females and males. Addiction. 2005;100:652–61. doi: 10.1111/j.1360-0443.2005.01053.x. [DOI] [PubMed] [Google Scholar]
- 4.Bonomo YA, Bowes G, Coffey C, et al. Teenage drinking and the onset of alcohol dependence: a cohort study over seven years. Addiction. 2004;99:1520–8. doi: 10.1111/j.1360-0443.2004.00846.x. [DOI] [PubMed] [Google Scholar]
- 5.Guo J, Chung I-J, Hill KG, et al. Developmental relationships between adolescent substance use and risky sexual behavior in young adulthood. J Adolesc Health. 2002;31:354–62. doi: 10.1016/s1054-139x(02)00402-0. [DOI] [PubMed] [Google Scholar]
- 6.Palen L, Smith EA, Flisher AJ, et al. Substance use and sexual risk behavior among South African eighth grade students. J Adolesc Health. 2006;39:761–3. doi: 10.1016/j.jadohealth.2006.04.016. [DOI] [PubMed] [Google Scholar]
- 7.Caldwell LL, Smith EA, Flisher AJ, et al. HealthWise South Africa: development of a life skills curriculum for young adults. World Leis. 2004;3:4–17. [Google Scholar]
- 8.Smith EA, Palen L-A, Caldwell LL, et al. Substance use and 2sexual risk prevention in Cape Town, South Africa: an evaluation of the HealthWise program. Prev Sci. 2008;9:311–21. doi: 10.1007/s11121-008-0103-z. [DOI] [PubMed] [Google Scholar]
- 9.Wegner L, Flisher AJ, Caldwell LL, et al. Healthwise South Africa: cultural adaptation of a school-based risk prevention programme. Health Educ Res. 2008;23:1085–96. doi: 10.1093/her/cym064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Botvin GJ, Griffin KW. Life skills training: empirical findings and future directions. J Prim Prev. 2004;25:211–32. [Google Scholar]
- 11.Caldwell LL. TimeWise: Taking Charge of Leisure Time. Scotts Valley, CA: ETR; 2004. [Google Scholar]
- 12.Baltes PB. On the incomplete architecture of human ontogeny: selection, optimization, and compensation as foundations of developmental theory. Am Psychol. 1997;52:366–80. doi: 10.1037//0003-066x.52.4.366. [DOI] [PubMed] [Google Scholar]
- 13.Lerner RM, Freund AM, De Stefanis I, et al. Understanding developmental regulation in adolescence: the use of the selection, optimization, and compensation model. Hum Dev. 2001;44:29–50. [Google Scholar]
- 14.Ryan RM, Deci EL. Self-Determination Theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000;55:68–78. doi: 10.1037//0003-066x.55.1.68. [DOI] [PubMed] [Google Scholar]
- 15.Ryan RM, Deci EL. Intrinsic and extrinsic motivations: classic definitions and new directions. Contemp Educ Psychol. 2000;25:54–67. doi: 10.1006/ceps.1999.1020. [DOI] [PubMed] [Google Scholar]
- 16.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice Hall; 1986. [Google Scholar]
- 17.Coffman DL, Smith EA, Caldwell LL. The Effects of the HealthWise Intervention on Condom Use Knowledge. Paper presented at the 16th Annual Meeting of the Society for Prevention Research, San Franscisco, CA: Society for Prevention Research, 2008. [Google Scholar]
- 18.Palen LA. Free Time Activities and Substance Abuse Among Adolescents in Cape Town, South Africa [Dissertation] University Park, PA: The Pennsylvania State University; 2008. [Google Scholar]
- 19.Botvin GJ, Griffin KW, Diaz T, et al. Drug abuse prevention among minority adolescents: posttest and one-year follow-up of a school-based preventive intervention. Prev Sci. 2001;2:1–13. doi: 10.1023/a:1010025311161. [DOI] [PubMed] [Google Scholar]
- 20.Schafer JL, Graham JW. Missing data: our view of the state of the art. Psychol Methods. 2002;7:147–77. [PubMed] [Google Scholar]
- 21.Graham JW, Cumsille PE, Elek-Fisk E. Methods for handling missing data. In: Schinka JA, Velicer WF, editors. Research Methods in Psychology. New York, NY: John Wiley & Sons; 2002. [Google Scholar]
- 22.Reddy SP, Panday S, Swart D, et al. Umthenthe Uhlaba Usamila—The South African Youth Risk Behaviour Survey 2002. Cape Town, South African: Medical Research Council; 2003. [Google Scholar]
- 23.Scott R, Harrison D. A Gauge of HIV Prevention in South Africa, 2009. Wierda Valley, Sandton: loveLife; 2009. [Google Scholar]
- 24.Harrison A, Newell M, Imrie J, et al. HIV prevention for South African youth: which Interventions work? A systematic review of current evidence. BMC Public Health. 2010;10:1–12. doi: 10.1186/1471-2458-10-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Harvey B, Stuart J, Swan T. Evaluation of a drama-in-education programme to increase AIDS awareness in South African high schools: a randomized community intervention trial. Int J STD AIDS. 2000;11:105–11. doi: 10.1177/095646240001100207. [DOI] [PubMed] [Google Scholar]