Abstract
Background
Reports of false beliefs may be a unique feature of behavioral variant frontotemporal dementia (bvFTD) but the nature of these experiences is unclear.
Objective
To report a case of pathologically verified Pick disease in a patient presenting with prominent and recurrent fantasies.
Methods
We describe the clinical, neuroradiologic, and neuropathologic findings of a 53-year-old woman presenting with fantasies and meeting Clinical Consensus Criteria for bvFTD.
Results
Early in her course, she reported interactions with different actors, having torrid affairs with them, and other related fantasies. When confronted with her false beliefs, she admitted that these relationships were imaginary. Autopsy revealed Pick disease with τ-immunoreactive Pick bodies in the frontal and temporal cortices, and in the hippocampi.
Conclusions
Fantastic thinking, or vividly experienced imagination, may be a manifestation of bvFTD that is distinct from delusions and confabulations and could be the source of previously reported delusions and confabulations in bvFTD.
Keywords: frontotemporal dementia, Pick disease, confabulations, delusions, fantasy
Behavioral variant frontotemporal dementia (bvFTD) is a clinical syndrome characterized by a gradual and progressive change in personality or behavior, including apathy, disinhibition, loss of social graces, repetitive or compulsive behaviors, and dietary or oral behavioral changes.1 bvFTD is associated with τ-negative, ubiquitin-positive/TDP-43 or FUS inclusions, or τ-positive inclusions, like Pick bodies. The presence of Pick bodies, or intraneuronal argyrophilic-staining inclusions, is the pathologic hallmark of Pick disease, and accounts for 16% to 42% of bvFTD cases.2
Psychotic symptoms, such as hallucinations or delusions, are unusual in bvFTD but can occur.3–5 There is debate as to whether false beliefs reported among bvFTD patients are phenomenologically distinct from content-specific delusions, such as those seen in Alzheimer disease (AD). Here, we report a patient with pathologically verified Pick disease and prominent fantastic thinking. We conclude that, rather than delusions or confabulations, bvFTD patients may vividly experience imagination and make-believe.
CASE REPORT
A 53-year-old woman presented with a 5-year to 6-year history of personality and behavioral changes (Fig. 1). She initially appeared disengaged with decreased appetite, and was treated for depression with little response. Soon after, the patient began to have daydreams about having relationships with famous actors. She typically reported that she was either friendly with or married to these celebrities, and at least once mentioned having children with George Clooney. She spent significant amounts of time conversing with her imaginary husbands. When asked about her real husband, she replied that in her imaginary world, he had gotten lost while hiking, and so she was free to have these other relationships. However, when pressed on the nature of these relationships, she submitted that they were not real and that she was married to her husband. Regarding her behavior, she stated that “thinking (was) as good as doing.” These fantastic relationships remained present throughout the course of her illness.
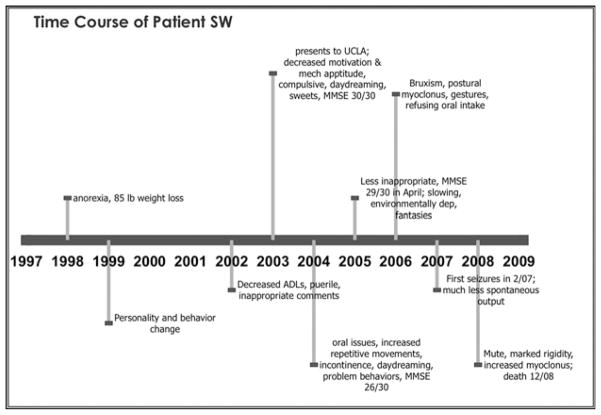
FIGURE 1.
Time course of patient’s disease progression.
Approximately 4 years before presenting to the Frontotemporal Dementia Clinic at the University of California, Los Angeles, the patient became even more withdrawn from social interactions and activities. She demonstrated decreased motivation to perform daily household tasks, where previously she had been quite meticulous (eg, vacuuming the house every day). One year before presentation, she began to have more difficulty performing instrumental activities of daily living and experienced a decline in self-care. In particular, she began to struggle with simple tasks such as turning on the shower or putting a key in the car ignition. She began to make inappropriate comments or ask silly questions to strangers, and her behavior was puerile. She was more impulsive and she developed an increasing appetite for sweets. She exhibited compulsive and repetitive behaviors: counting, avoiding stepping on cracks on sidewalks, picking at her fingers, pinching her lip, rubbing her right knee or right face, and swaying back and forth when standing. Around the time of initial presentation, the patient’s eldest daughter, who was brain damaged from a near-drowning accident at the age of 5 years, had recently been placed into a nursing home. Though our patient had been her daughter’s primary caregiver, she seemed oblivious to this event.
On initial examination, the patient exhibited a fixed smile and frequent staring. She scored a 30/30 on the Mini-Mental State Examination. Further neurobehavioral assessment showed decreased reverse digit span, decreased phonemic and categorical verbal fluency, poor verbal recall but intact verbal recognition memory, intact visuoconstructional ability, and decreased performance on go-no-go, antisaccade, and judgment testing.
Magnetic resonance imaging revealed global cerebral atrophy, which was particularly pronounced in the frontal lobes. Single photon emission computed tomography imaging revealed hypoperfusion that was most prominent in the right anterior prefrontal, lateral, and orbitofrontal lobes, the right anterior portion of the interhemispheric fissure, the right anterior temporal lobe, and the anterior portion of the cingulate gyrus. Hypoperfusion was present to a lesser degree in the left cerebral hemisphere (Fig. 2A). Taken together, her clinical presentation and neuroimaging findings were consistent with a diagnosis of bvFTD.
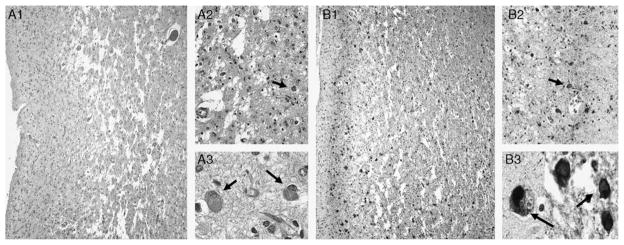
FIGURE 2.
A, Axial SPECT scan showing frontal and temporal hypoperfusion, right greater than left. B, Brain at autopsy showing marked atrophy of the frontal and anterior temporal lobes. C, Coronal section showing temporal lobe atrophy with relative sparing of bilateral hippocampi. SPECT indicates single photon emission computed tomography.
One year after initial presentation, she began to exhibit increasingly inappropriate behaviors. In particular, she would confront young strangers and ask them about their sexual orientation, or she would directly ask smokers why they did not quit smoking. Her imaginary world became more involved, and she started imagining sexual acts with movie stars. She told her family that she was thinking about becoming gay. Despite being treated with sertraline, her repetitive acts, such as counting, disrupted her daily routine. She was started on a low dose of quetiapine and became somewhat less impulsive and compulsive.
The patient’s fantastic thinking continued to focus on celebrities. Two years after presentation, she reported active fantasies about Kevin Costner, and made comments about this relationship in public. She was still engaging in repetitive acts, and was becoming more environmentally dependent and distractible. By 2.5 years after presentation, she was very compliant and displayed fewer behavioral problems although she continued to make inappropriate comments regarding the sexual orientation of women strangers she saw in public. She developed bruxism. Three years after initial presentation, the patient began to make obscene gestures to passersby when riding in the car and started to refuse liquids. She still had vivid fantasies, claiming that she was married to George Clooney and had had 2 children with him.
Soon after, the patient began to deteriorate. She developed postural myoclonus and was started on clonazepam. Almost 4 years after initial presentation, she had 2 seizures, and was started on levetiracetam. Her disinhibited behaviors decreased and she was increasingly less responsive to questions. She developed a visual grasp, increased neck tone, and poor balance. Soon after, the patient became mute and refused to open her mouth for food or liquids. She followed commands intermittently and displayed motor impersistence. Her myoclonus had increased, and she had become increasingly rigid, especially in the axial plane. She could still walk, though with a list and very poor balance. The patient died 6 months later, 11 years from the onset of her illness.
Autopsy revealed the presence of Pick disease. On gross examination, the 1040 g (unfixed weight) brain demonstrated diffuse cerebral cortical atrophy in the frontal and temporal lobes, with a slight left hemisphere predominance and relative sparing of the parietal and occipital cortices (Figs. 2B, C). Microscopic examination included routine hematoxylin and eosin staining and immunohistochemistry incorporating primary antibodies to β-amyloid 1 to 40 and 1 to 42, τ, and α-synuclein. There was severe neuronal loss, gliosis, and spongiosis of the deep cortical layers of the bilateral frontal and temporal lobes, which was more pronounced on the right (Fig. 3A). There was also moderate neuronal loss and gliosis of the striatum and substantia nigra. Cortical tissue from the parietal and occipital lobes was relatively less affected. Immunostaining revealed abundant τ-positive Pick bodies within the remaining neurons in the frontal and temporal cortices, and the pyramidal and granule neurons within the hippocampus. Rare Pick bodies were also seen in the parietal and occipital cortex and striatum (Fig. 3B).
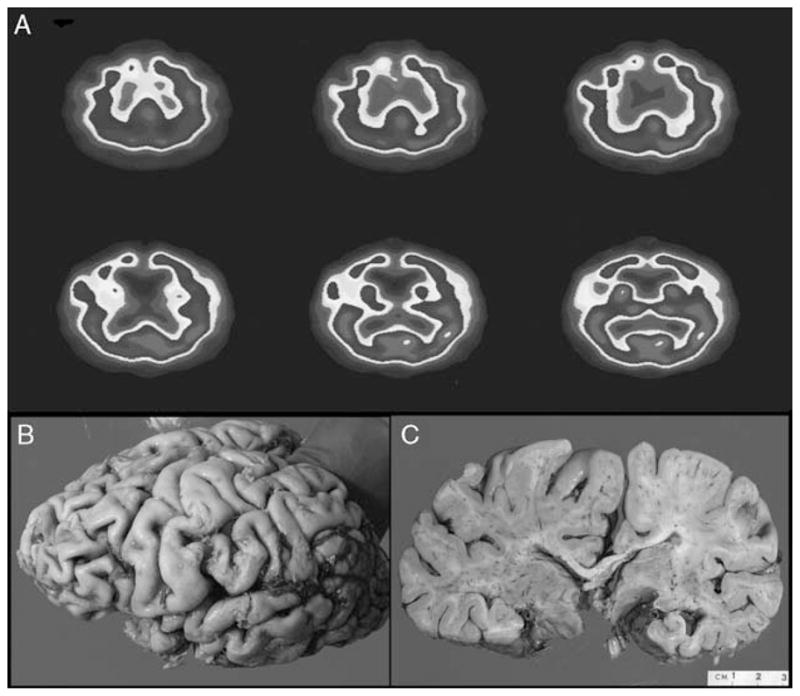
FIGURE 3.
Histologic sections. A, H&E staining. A1, Frontal cortex demonstrating spongiosis of the deep cortical layers (40 ×). A2, Highlights marked gliosis, neuron loss and Pick bodies (arrow) (400 ×). A3, Details of Pick bodies (arrows) (1000 ×). B1 and B2, τ-immunostaining of corresponding sections of frontal cortex showing abundant τ-immunoreactive residual neurons and Pick bodies (arrow) (40 × and 400 × , respectively). B3, τ-immunoreactive Pick bodies (arrows) (1000 ×). H&E indicates hematoxylin and eosin.
DISCUSSION
Our patient presented with fantastic thinking as an early and persistent feature of her illness. Fantastic thinking is the product of creative imagination, unrestricted by reality, and is usually understood to be untrue by the inventor.
Psychotic symptoms, such as delusions and hallucinations, are uncommon features in bvFTD.3 However, there have been several recent reports documenting delusional thinking or confabulations among bvFTD patients.4–7 A delusion is “a false belief based on an incorrect inference about external reality that is firmly sustained despite what almost everyone else believes and despite what constitutes incontrovertible and obvious proof or evidence to the contrary.”8 DeClarembault syndrome is a delusional disorder in which a woman believes that a man of higher social status is passionately in love with her. Our patient’s presentation resembles a “reverse” DeClarembault syndrome, however, she was not delusional regarding the nature of the relationships she claimed to have with celebrities. When questioned about these relationships, our patient repeatedly stated that she knew these relationships were “in her head” and not real.
If not delusions, did our patient have confabulations? Confabulations are usually “a falsification of memory occurring in clear consciousness.”9 A suggested working definition is “false statements that are not made to deceive, are typically more coherent than thoughts produced during delirium, and do not reflect underlying psychopathology.”7 Momentary or provoked confabulations are false answers created to fill in gaps in memory often in response to questions, and tend to vary according to the context of the current setting. Fantastic or spontaneous confabulations are offered and elaborated upon without any provocation. They often have grandiose and wish-fulfilling characteristics, and remain relatively consistent regarding the nature of their content.10,11 The difference between fantastic confabulations and our patient’s fantastic thinking is that she knew her imagined relationships were not real, and she did not have significant day-to-day memory difficulties.
We propose that our patient’s report of false experiences does not meet the criteria for delusions or confabulations, and can best be characterized as “fantastic thinking.” Fantastic thinking is characterized by unfettered imaginations and wish-fulfillment that the patient experiences but knows are not real. A possible explanation for our patient’s fantastic thinking was that her feeling for reality was disturbed, although her actual understanding of reality was not. This is supported by recent work suggesting that the affective and cognitive components of theory of mind are dissociable.12 It is also possible that the patient’s divulgence of private thoughts could have been due to disinhibition or poor monitoring of her behavior in social situations. Alternatively, she may simply have been unconcerned that others might perceive her statements as bizarre.
Despite the phenomenologic distinctions between fantastic thinking, delusions, and confabulations, the underlying neurobiologic correlates for all 3 symptoms may overlap. Delusions have been associated with damage to the inferior frontal lobes, in particular the right hemisphere, the right dorsolateral prefrontal cortex and right inferior frontal pole, the right or bilateral caudate nuclei, and the left temporal lobe.13–15 Lesions causing confabulations also occur predominantly in the orbitofrontal and basal forebrain regions, as well as the amygdala, cingulate gyrus, dorsomedial nucleus of the thalamus, and medial hypothalamus.15
bvFTD is associated with bilateral atrophy of the frontal lobes, in particular, the medial frontal and anterior temporal lobes.2 The ventromedial frontal lobes play an important role in self-referential processes and affective theory of mind. They also integrate information from the insula and other areas to establish a general representation of self.12,16 It is reasonable, therefore, that bvFTD patients might develop fantastic thinking due to preferential involvement of the ventral and dorsomedial frontal lobes, which leads to an alteration of their subjective feeling of reality and their role of self within that reality. This altered feeling of reality can be separated from their intact understanding of reality, which is mediated by the dorsolateral frontal lobes.12 This interpretation is supported by single photon emission computed tomography imaging in our patient, which demonstrated greater hypoperfusion in anterior prefrontal and medial frontal areas relative to dorsolateral prefrontal areas. Her scan also showed more pronounced hypoperfusion on the right than on the left, which is consistent with previous work suggesting that the nondominant (right) frontal lobe may lead to a shift in long-held self-schemas.17 Additionally, it has also been well established that self-monitoring and inhibition is dependent upon intact right orbitofrontal cortex.16
In conclusion, this is a unique case of a pathologically verified Pick disease in a patient presenting with fantastic thinking as an early and primary manifestation of the illness. This case adds to the small but growing number of bvFTD patients presenting with this symptom, which is distinct from delusions and confabulations. This report underscores the importance of considering a diagnosis of bvFTD when prominent fantasies develop in mid-life.
Acknowledgments
Harry V. Vinters, MD is supported in part by the UCLA Alzheimer Disease Research Center grant P50AG16570 and the Daljit S. & Elaine Sarkaria Chair in Diagnostic Medicine.
References
- 1.Neary D, Snowden JS, Gustafson L, et al. Frontotemporal lobar degeneration: a consensus on clinical diagnostic criteria. Neurology. 1998;51:1546–1554. doi: 10.1212/wnl.51.6.1546. [DOI] [PubMed] [Google Scholar]
- 2.Josephs KA. Frontotemporal dementia and related disorders: deciphering the enigma. Ann Neurol. 2008;64:4–14. doi: 10.1002/ana.21426. [DOI] [PubMed] [Google Scholar]
- 3.Mendez MF, Shapira JS, Woods RJ, et al. Psychotic symptoms in frontotemporal dementia: prevalence and review. Dement Geriatr Cogn Disord. 2008;25:206–211. doi: 10.1159/000113418. [DOI] [PubMed] [Google Scholar]
- 4.Tartaglia MC, Kertesz A, Ang LC. Delusions and hallucinations in frontotemporal dementia: a clinicopathologic case report. Cogn Behav Neurol. 2008;21:107–110. doi: 10.1097/WNN.0b013e3181799e19. [DOI] [PubMed] [Google Scholar]
- 5.Omar R, Sampson EL, Loy CT, et al. Delusions in frontotemporal lobar degeneration. J Neurol. 2009;256:600–607. doi: 10.1007/s00415-009-0128-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nedjam Z, Dalla Barba G, Pillon B. Confabulation in a patient with fronto-temporal dementia and a patient with Alzheimer’s disease. Cortex. 2000;36:561–577. doi: 10.1016/s0010-9452(08)70538-0. [DOI] [PubMed] [Google Scholar]
- 7.Nedjam Z, Devouche E, Dalla Barba G. Confabulation, but not executive dysfunction discriminate AD from frontotemporal dementia. Eur J Neurol. 2004;11:728–733. doi: 10.1111/j.1468-1331.2004.00981.x. [DOI] [PubMed] [Google Scholar]
- 8.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington DC: American Psychiatric Association; 1994. [Google Scholar]
- 9.Berlyne N. Confabulation. Br J Psychiatry. 1972;120:31–39. doi: 10.1192/bjp.120.554.31. [DOI] [PubMed] [Google Scholar]
- 10.Glowinski R, Payman V, Frencham K. Confabulation: a spontaneous and fantastic review. Aust N Z J Psychiatry. 2008;42:932–940. doi: 10.1080/00048670802415335. [DOI] [PubMed] [Google Scholar]
- 11.Gundogar D, Demirci S. Confabulation: a symptom which is intriguing but not adequately known. Turk Psikiyatri Derg. 2007;18:172–178. [PubMed] [Google Scholar]
- 12.Shamay-Tsoory SG, Aharon-Peretz J. Dissociable prefrontal networks for cognitive and affective theory of mind: a lesion study. Neuropsychologia. 2007;45:3054–3067. doi: 10.1016/j.neuropsychologia.2007.05.021. [DOI] [PubMed] [Google Scholar]
- 13.McMurtray AM, Sultzer DL, Monserratt L, et al. Content-specific delusions from right caudate lacunar stroke: association with prefrontal hypometabolism. J Neuropsychiatry Clin Neurosci. 2008;20:62–67. doi: 10.1176/jnp.2008.20.1.62. [DOI] [PubMed] [Google Scholar]
- 14.Trimble MR, Mendez MF, Cummings JL. Neuropsychiatric symptoms from the temporolimbic lobes. J Neuropsychiatry Clin Neurosci. 1997;9:429–438. doi: 10.1176/jnp.9.3.429. [DOI] [PubMed] [Google Scholar]
- 15.Sultzer DL, Brown CV, Mandelkern MA, et al. Delusional thoughts and regional frontal/temporal cortex metabolism in Alzheimer’s disease. Am J Psychiatry. 2003;160:341–349. doi: 10.1176/appi.ajp.160.2.341. [DOI] [PubMed] [Google Scholar]
- 16.Mendez MF, Lauterbach EC, Sampson SM. An evidence-based review of the psychopathology of frontotemporal dementia: a report of the ANPA Committee on Research. J Neuropsychiatry Clin Neurosci. 2008;20:130–149. doi: 10.1176/jnp.2008.20.2.130. [DOI] [PubMed] [Google Scholar]
- 17.Miller BL, Seeley WW, Mychack P, et al. Neuroanatomy of the self: evidence from patients with frontotemporal dementia. Neurology. 2001;57:817–821. doi: 10.1212/wnl.57.5.817. [DOI] [PubMed] [Google Scholar]