Abstract
Randomized controlled trial of 511 eligible women treated for diabetes, hypertension, infertility, or osteoporosis on an out-patient basis to test the hypothesis that those randomized to a brief intervention (BI) will drink less than those in the control condition 12 months later. A secondary goal was to identify the characteristics associated with changes in drinking outcome. All 511 completed the initial Alcohol Assessment and 96% completed the 12-month follow up interview. Those receiving the BI also had 3 and 6 month interviews. Four outcomes were assessed: 1) mean drinks per drinking day, 2) percent drinking days, 3) binge episodes defined as 4 or more drinks per occasion, and 4) weeks of drinking exceeding NIAAA sensible drinking limits. Overall, there were no differences in drinking outcome by treatment group. Characteristics associated with changes in drinking, however, were identified to provide possible direction for future investigation.
Keywords: Women, Alcohol, Brief Intervention, Health problems
1.0 Introduction
A significant number of American women may be problem drinkers, as 13% of those who drink will have more than 7 drinks per week (National Institute on Alcohol Abuse and Alcoholism, 2007). Although women have had lower rates of alcohol use disorders than men, the gender gap for drinking problems is narrowing (Hasin et al., 2007, Keyes et al., 2008). Women are more vulnerable to the negative medical consequences of alcohol because of metabolic differences, but they are less likely to be identified and treated for risky drinking (Baraona et al., 2001, Brienza & Stein, 2002).
One possible explanation for the difficulty in the identification and treatment of risky drinking in women is the complicated relationship between alcohol consumption and health, depending on which aspect of health is being studied. For example, a J-shaped curve has been reported for alcohol and cardiovascular disease, where light to moderate drinkers (1 drink per day by women) have less risk than abstainers, and heavy drinkers are at the highest risk (O'Keffe, Bybee, & Lavie, 2007). A U-shaped relationship, on the other hand, has been reported between alcohol and type 2 diabetes, whereby moderate but not heavy alcohol consumption is associated with reduced risk (Koppes, et al., 2005). Yet, the prospective Women's Health Study of nearly 40,000 female health professionals found that daily consumption of 10 g/day of alcohol (.75 to 1 drink) was significantly associated with a 9 percent increase in risk of invasive breast cancer, and the risk increased with more alcohol use (Zhang et al., 2007). These examples illustrate the challenges women and their healthcare providers face in understanding the true consequences of risky drinking.
Screening and brief intervention (SBI) has been developed to improve the identification and modification of risky drinking in medical settings. Although SBI for risky drinking has been ranked among the top ten most valuable clinical preventive services, it has been offered to less than half of all drinkers (Kuehn, 2008; Maciosek et al., 2006; US Preventive Services Task Force, 2004). Moreover, female risky drinkers were among the least likely to receive a brief intervention in a program involving 84 general practitioners in Great Britain (Kaner et al., 2001). A recent meta-analysis concluded that while brief interventions lowered alcohol consumption overall, the effect was clear in men, but not in women (Kaner et al., 2007). One explanation is that few women participated in past research.
The primary purpose of this study is to assess the efficacy of SBI in a sample of 511 risky drinking women with medical diagnoses potentially exacerbated by risky drinking. The women were not seeking treatment of their alcohol use, rather, they were receiving outpatient care for hypertension (e.g., 3 to 8% of high blood pressure is directly attributable to alcohol in women), diabetes (e.g., alcohol suppresses hepatic gluconeogenesis leading to hypoglycemia), infertility (e.g., heavy alcohol use is a modifiable risk factor associated with decreased fecundity), and osteoporosis (e.g., heavy drinking compromises bone health by decreasing bone density). (American Diabetes Association, 2010; Anderson, Nisenblat, & Norman, 2010; Berg et al., 2008; Homan et al., 2007; Klatsky et al., 2007; O'Keefe et al., 2007). We hypothesized that these women would be motivated to reduce their alcohol consumption because of their medical problems and that women randomized to the brief intervention condition would drink less than those in the control condition. The secondary purpose of the study was to identify, if possible, the characteristics of women for whom the BI was most effective.
2.0 Methods
This study was reviewed and approved by the Partners Institutional Review Board (2004-p-000687). A federal Certificate of Confidentiality was obtained (Number AA-30-2005).
2.1 Screening, Enrollment, and Randomization
2.1.1 Screening
All potential participants completed the initial screening measure, the Women's Health Habits Survey. This Survey contained questions about usual quantity and frequency of alcohol intake, stress, weight, sleep, and other health habits, and the T-ACE. The T-ACE is a 4 item alcohol screen based on the CAGE, with good to excellent results in identifying risky drinking by women who were pregnant, seeking gynecologic care, aged 60 and older, and among primary care patients (Gupman et al., 2002; McQuade at al., 2000; Sokol et al., 1989; Stevenson & Masters, 2005). The T-ACE substitutes a question about Tolerance to alcohol for the Guilt question (Sokol, Martier, and Ager, 1989).
The Women's Health Habits Survey was made available to potential participants in one of two ways. The first way was for women receiving outpatient treatment at the Brigham and Women's Hospital (BWH) diabetes, hypertension, osteoporosis, or infertility clinics. These women were sent letters (signed by their physicians and the first author) that described the study and included the Women's Health Habits Survey. Those interested in learning more returned the Survey in a business reply envelope. This group was the BWH sample. The second way involved women who responded to study advertisements on the subway, newspapers, and online. These women were sent the Women's Health Habits Survey and asked to return the completed Survey as well. This second group was the non-BWH sample.
2.1.2 Eligibility and Enrollment
Using a scripted interview, Research Assistants assessed the women who returned the screening Survey for eligibility criteria for the randomized trial. The women were contacted at a time scheduled to ensure their privacy. They were asked about meeting eligibility criteria which included having: 1) confirmed hypertension, diabetes, osteoporosis, or infertility, 2) sufficient command of English to complete study measures and interviews, 3) not currently receiving treatment for alcohol or drug use disorders, 4) not currently pregnant or nursing, 5) T-ACE alcohol screen positive and/or 6) typically consumed more than seven drinks a week or more than two drinks at a time (National Institute on Alcohol Abuse and Alcoholism, NIAAA, sensible drinking limits for women modified to reflect the medical status of the women). For healthy women without health conditions exacerbated by alcohol, the NIAAA has defined risky drinking to be more than 7 drinks per week and more than 3 drinks per day (National Institute on Alcohol Abuse and Alcoholism, 2007).
Finally, potential participants agreed to study terms, which included: 1) confirmation of their medical diagnosis by their physician, 2) completion of Assessment and follow-up interviews for which they would receive $50.00 each, and 3) randomization to treatment condition. Participants would only learn of their treatment assignment at the conclusion of the Assessment interview.
2.1.3 Randomization
Participants were randomized by computer-generated assignment to either an active control or treatment condition. The active control condition (AC) consisted of the Assessment Interview with a single 12-month interview to obtain follow-up data. No other interviews were planned for this group because of their therapeutic potential. The treatment condition (BI) included the same Assessment Interview, Brief Intervention, and interviews at 3, 6, and 12 months to obtain follow-up data. The Brief Intervention with additional follow-up interviews is similar to the schedule of suggested clinician contacts outlined in Helping Patients Who Drink Too Much (National Institute on Alcohol Abuse and Alcoholism, 2007).
2.2 Assessment Interview
Upon confirmation of their medical diagnosis, eligible participants were scheduled for their Assessment Interview that took place in the outpatient research offices at the Brigham and Women's Hospital. Participants were only informed of their treatment assignment at the conclusion of the Assessment Interview.
The Assessment Interview was administered by the Research Assistants and required up to 1 hour to complete. Measures included: 1) the alcohol and drug abuse modules from the Structured Clinical Interview for DSM-IV (SCID), to obtain current and lifetime alcohol and drug disorder diagnoses (First et al., 2002); 2) the alcohol timeline followback (TLFB), to obtain estimates of daily drinking for the 6 months prior to study enrollment (Sobell & Sobell, 1992); and the 3) MOS 36-Item Short Form Health Survey (SF-36), to assess general health status, among others (Ware & Shelbourne, 1992).
2.3 Brief Intervention
Those randomized to the treatment arm received the Brief Intervention (BI) shortly after the Assessment Interview in the outpatient research offices of the Brigham and Women's Hospital. The BI was intentionally scheduled on the same day as the Assessment, whenever possible, to minimize subject inconvenience. Hence, it was necessary for study staff to be aware of the treatment assignment to facilitate scheduling.
The BI was given by the first author or other physicians she trained. It was based on Personal Steps to a Healthy Choice: A Woman's Guide and Helping Patients Who Drink Too Much, both published by NIH (National Institute of Alcohol Abuse and Alcoholism, 2007; National Institute of Health, 2000). Physician preparation included review of the aforementioned materials as well as appropriate chapters from Motivational Interviewing (Miller and Rollnick, 1991), observation of a brief intervention and then practice with mock patients, after which time feedback was given. Physicians' brief interventions with study patients were initially observed by the PI, with feedback given. In addition, brief interventions were audiotaped according to a pre-set schedule (the first several given by each physician and then a random selection of 1-2 each per week thereafter). The audiotapes were reviewed and rated by the PI and another physician using the Yale Adherence and Competence Scale for Motivational Interviewing (YACS II, Nuro et al., 2005). Again, feedback was given and no physician rated his/her own sessions.
The study BI required about 30 minutes to complete, a time frame similar to other studies that either used a 30 minute single session physician encounter, or two fifteen minute physician encounters (Saitz et al., 2007). The BI included the standard 4 components:
Assessment and Feedback, which summarized the individual's drinking patterns compared to national averages and offered standardized information on the health consequences of drinking on her medical problem (e.g., heavy alcohol use increases the risk of hypertension, is significantly and positively related to fasting blood glucose, is associated with increases in infertility due to ovulatory factors, and may compromise bone health).
Goal setting and contracting, which asked for the participant's drinking goal (e.g., cut down or abstain) and important reasons for modifying drinking behavior.
Behavioral modification, during which time participants were asked to identify the circumstances they would be at increased risk for drinking and to develop alternative behaviors.
Written materials, participants were given their own copy of Personal Steps, annotated with their personal information.
2.4 Follow-Up Interviews
Follow-up interviews were administered by the Research Assistants at prescribed intervals. The follow-up interviews either took place in the outpatient research offices at the Brigham and Women's Hospital or over the phone at times scheduled to ensure the privacy and convenience of the participant.
The BI group had 3 and 6 month follow-up interviews which included the Alcohol Timeline Follow back to obtain information on alcohol use in the previous 90 days, and two other measures. The two supplementary measures were the Medication Adherence Scale (4-items about medication compliance; Brooks et al., 1994) and the Perceived Stress Scale (14-items about situations which participants considered to be stressful; Cohen et al., 1983) and are not the focus of the current report.
All participants were interviewed 12 months after enrollment. They completed a TLFB to provide information about alcohol use since their last study contact. For the AC group, the TLFB would cover the prior 12 month period. For the BI group, the TLFB would cover the prior 6 month period (if the 3 and 6 month follow-up interviews were completed as scheduled), or the entire 12 month period since enrollment (if necessary).
2.5 Data Analysis
All analyses used the SAS statistical package (version 9.1). Simple descriptive statistics were calculated and are reported as percentages, means, and standard deviations (SD), as appropriate. The demographic and clinical characteristics of the participants (BWH versus non-BWH and treatment versus active control) were compared using t-tests for continuous variables and chi-square tests for categorical variables.
Comparisons of the participants' drinking using four outcome measures were planned using Intention to Treat Analysis. The 20 (4%) participants who did not complete the study had their last available drinking data carried forward and are considered “treatment failures.” The four outcome measures were: 1) drinks per drinking day (D/DD), 2) percent drinking days (% DD), 3) number of binge episodes, with binges defined as 4 or more drinks per occasion, and 4) number of weeks exceeding NIAAA sensible drinking limits (weeks > SDL). Drinking for the six-month period prior to study enrollment would be compared to establish baseline, pre-study patterns of consumption. While data about alcohol use in the first six months after study enrollment would be available, information about this period of use for the BI group would be based on a shorter time of recall than for the AC group (which had a 12 month interview only). Hence, the most comparable drinking data for both groups would be the information gathered at the 12-month interview for the preceding 6 months and is the basis of the multivariate analysis.
For each of our 4 outcome measures, we compared drinking at baseline between the two arms, as well as drinking at 12 months between the two arms, using a 2-sample t-test. We then calculated the change in each of our 4 outcomes by subtracting the 12-month assessment measure from the baseline assessment measure. These changes were compared between the two arms using a 2-sample t-test.
Finally, in order to adjust for confounding due to any patient demographic or clinical characteristics which were not fully balanced by randomization, we constructed linear regression models for each of our 4 outcome measures at 12 months. In the initial model, our primary predictor was Brief Intervention, while the adjustment covariates included all of the patient demographic and clinical variables that we considered to be potentially related to drinking behavior, including the drinking measures at baseline. The included covariates are all of those measures shown in Table 1 except for BMI, and these are summarized again in Table 4. We also constructed a second set of models based on our prior study where we found that the impact of the Brief Intervention was related to the degree of drinking at baseline (Chang et al., 2005). For these models, we included all of the independent variables mentioned above, plus the interaction term between baseline drinking and the Brief Intervention.
Table 1. Participants by Out-Patient Practice.
| BWH (n=363) | Non-BWH (n=148) | p-Value | |
|---|---|---|---|
| Mean age, (SD) year | 44.1 (13.2) | 47.5 (14.4) | 0.01 |
| Race, % | <.0001 | ||
| Asian | 2 | 2 | |
| Pacific Islander | 1 | 0 | |
| Black | 14 | 41 | |
| White | 83 | 57 | |
| Hispanic, % | 6 | 4 | 0.57 |
| Marital Status, % | <.0001 | ||
| Married | 63 | 29 | |
| Widowed | 3 | 3 | |
| Divorced | 11 | 21 | |
| Separated | 1 | 2 | |
| Never married | 22 | 45 | |
| Education, % | <.0001 | ||
| < BA, including HS | 32 | 52 | |
| 4 year college | 30 | 22 | |
| Any graduate/professional school | 38 | 26 | |
| Employed, % | 72 | 52 | <.0001 |
| Children, % | 45 | 57 | 0.01 |
| Mean BMI (SD) | 26.3 (7.0) | 29.6 (8.1) | <.0001 |
| SF-36, Mean (SD) | |||
| PCS1 | 50.9 (10.0) | 48.1 (9.2) | .005 |
| MCS2 | 45.8 (10.8) | 46 (10.6) | 0.91 |
| Medical Diagnosis, % | <.0001 | ||
| Hypertension | 22 | 54 | |
| Diabetes | 15 | 30 | |
| Osteoporosis | 20 | 12 | |
| Infertility | 43 | 4 | |
| Randomized to BI, % | 51 | 44 | 0.16 |
| Drinking at Enrollment Mean (SD) | |||
| Drinks/drinking day | 2.1 (1.2) | 2.3 (1.8) | 0.10 |
| % drinking days | 24 (27) | 22 (25) | 0.35 |
| No. of binges | 5.5 (17.6) | 9.2 (26.5) | 0.12 |
| Weeks > SDL | 3.9 (7.5) | 3.7 (7.4) | 0.78 |
Physical Component Summary Scale
Mental Health Component Summary Scale
Table 4. Changes in Alcohol Outcome Measures Between Study Arms.
| Changes within Arms | Difference in Changes Between Arms | |||||
|---|---|---|---|---|---|---|
| Mean Change (SD) | Mean Change (SD) | Mean Difference (95% CI) | Mean Difference (95% CI) | |||
| Active Control | Brief Intervention | Unadjusted | P-value | Adjusted* | P-value | |
| Drinks/drinking day change | -.31 (1.4) | -.18 (1.4) | -.13 (-.38, .11) | .28 | -.06 (0.3, .18) | .63 |
| % Drinking days change | -1.3 (1.7) | -4.3 (.21) | 3.0 (-.3, 6.0) | .07 | 3.0 (-.1, 6.0) | .07 |
| Binge change | -1.9 (13.9) | -1.4 (24.3) | -.50 (-3.9, 2.9) | .78 | -2.2 (-4.9, .54) | .11 |
| Sensible drinking weeks change | -.71 (5.8) | -.75 (5.8) | 0.04 (-.97, 1.1) | .84 | 0.27 (-1.2, .65) | .57 |
Models were adjusted for each respective baseline drinking measure, disease (diabetes, infertility, or osteoporosis versus hypertension), age, married versus not, race (any minority versus Caucasian), Hispanic versus non-Hispanic, education, children, employment status, MCS score, PCS score, lifetime substance use disorder diagnoses (alcohol, cocaine, marijuana, opiates, polysubstance)
3.0 Results
3.1 Overall Results
511 of 3115 (16.4%) women assessed for eligibility were enrolled. Among the 2504 (80.3%) not enrolled, 678 (27%) provided only an incomplete initial screen. The remaining 1826 (73%) did not meet inclusion criteria. Most (83%, n=1517) were alcohol screen negative and drank within the NIAAA sensible drinking limits. Among the 309 alcohol screen positive women, 130 (42%) were unavailable, 92 (30%) did not have one of the study diseases confirmed, 41 (13%) were pregnant, 17 (6%) declined to authorize medical records release, 13 (4%) consumed no alcohol in the past 6 months, 6 (2%) were in alcohol treatment, and the remaining 10 (3%) were excluded for other reasons. The study began in February 2005 and ended in May 2009.
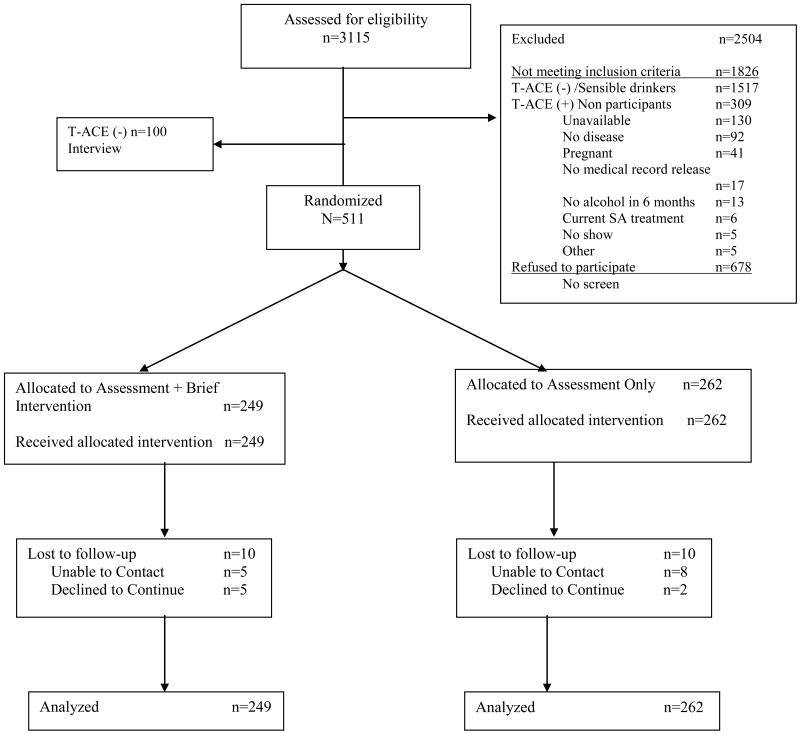
Four hundred ninety one of the 511 women (96%) completed the 12-month interviews. Ten women were lost to follow-up and ten withdrew. There were no statistically significant differences between these 20 women and the 491 who completed the study in terms of baseline alcohol consumption on any of the four alcohol endpoints, and demographic or clinical characteristics. Figure 1 summarizes the study flow.
Figure 1. Study Flowchart.
3.1.1 BWH and non-BWH Participants
Seventy-one percent of the 511 eligible enrolled women received outpatient medical care at the BWH clinics (n=348, these women received letters from their physicians and the PI). The remaining 148 (29%) received outpatient medical care elsewhere in the Boston area (and responded to study advertisements). Compared to the BWH clinical sample, the non-BWH women were older (mean age of 47.5 versus 44.1 years, p=.01); more likely to be black (41% versus 14%, p<.0001); more likely to be never married (45% versus 22%, p<.0001), and to have less than a 4 year college education (52% versus 32%, p<.0001). In addition, the non-BWH women were more likely to have children (57% versus 45%, p=.01) and to be cigarette smokers (20% versus 11%, p=.01). The non-BWH women were heavier (mean BMI 29.6 versus 26.3, p<.0001); and had a somewhat lower Physical Component Scale Summary (mean 48.1 versus 50.9, p=.005). The non-BWH group were significantly more likely to have hypertension or diabetes, and few had osteoporosis or infertility (p<.0001). However, there were no differences between the BWH and non-BWH women on any of the four measures of baseline alcohol consumption at enrollment. The non-BWH women accounted for 32% of those in the Active Control group and 26% of those in the BI group (p=.16). Table 1 summarizes the comparison between the BWH and non-BWH women at enrollment, or the women who received letters from the physicians or those who responded to study advertisements, respectively.
3.1.2 Treatment and Active Control Group Participants
Women randomized to each of the two treatment groups were similar in terms of mean age, marital status, racial and ethnic background, educational attainment, children at home, and employment. Whereas half the women in both groups had hypertension or diabetes, a higher proportion of women with infertility was found in the AC group and a higher proportion of women with osteoporosis was found in the BI group, but these differences were not statistically significant (p=.08). In the event that the women had more than one medical diagnosis by history (e.g., hypertension and osteoporosis), the disease under active treatment (e.g., hypertension) was the basis of disease classification. Seventy women (14%) had more than one medical diagnosis by history. The groups did not differ in their overall Physical Component Summary Scale Score (mean, 50.1 (SD=9.8)) and Mental Health Component Summary Scale Score (mean, 45.9 (SD=10.7)).
The groups were also similar in terms of lifetime and current substance use disorders. Lifetime alcohol use disorders were the most prevalent (43%), followed by marijuana (13%), and cocaine (7%). Lifetime disorders involving sedatives (2%), stimulants (2%), and hallucinogens (1.6%) were infrequent and equally distributed between the two groups. More women in the BI group, however, had lifetime opiate diagnoses compared to the AC group (p=.02). More women in the BI group satisfied criteria for current alcohol use disorders (p=.06); however the groups had similar infrequent rates of current marijuana, cocaine, and other substance use disorders. Table2 summarizes the comparison of participant characteristics by treatment groups.
Table 2. Demographic and Clinical Characteristics of Participants.
| Variable | Brief Intervention n=249 |
Active Control N=262 |
p-value |
|---|---|---|---|
| Mean age (SD), years | 46.1 (13.3) | 44.2 (13.9) | 0.12 |
| Marital Status, % | |||
| Married | 54 | 52 | 0.60 |
| Race/Ethnic Background, % | |||
| Black | 23 | 21 | 0.21 |
| White | 73 | 78 | |
| Other | 4 | 1 | |
| Hispanic | 5 | 5 | 0.73 |
| Disease, % | |||
| Hypertension | 31 | 32 | 0.07 |
| Diabetes | 21 | 18 | |
| Osteoporosis | 21 | 14 | |
| Infertility | 27 | 36 | |
| SF-36 | |||
| Physical component summary | 50.0 (9.9) | 50.2 (9.8) | 0.77 |
| Mental health component summary | 46.2 (10.5) | 45.6 (10.5) | 0.54 |
| Education, % | |||
| < BA, including High School | 40 | 36 | 0.44 |
| 4 year College graduate | 28 | 26 | |
| Any graduate/professional school | 32 | 38 | |
| Children, % | 49 | 47 | 0.61 |
| Employed, % | 63 | 70 | 0.09 |
| Lifetime Substance Use Disorders, % | |||
| Alcohol | 40 | 45 | 0.27 |
| Marijuana | 13 | 13 | 0.97 |
| Cocaine | 7 | 7 | 0.87 |
| Opiates | 3 | 0.4 | 0.02 |
| Other (sedatives, stimulants, hallucinogens) | 5 | 5 | 0.90 |
| Current Substance Use Disorders, % | |||
| Alcohol | 12 | 7 | .06 |
| Marijuana | 3 | 2 | .71 |
| Cocaine | 2 | 1 | .27 |
| Opiates | 0 | 0 | -- |
| Other (sedatives, stimulants, hallucinogens) | 1 | 1 | 1 |
3.2.1 Changes in Alcohol Consumption Between Treatment Groups
Four alcohol endpoints were defined: drinks per drinking day (D/DD), percent drinking days (%DD), number of binge episodes (defined as 4 or more drinks per event) and number of weeks when NIAAA sensible drinking limits were exceeded (>SDL). For the 6-month period prior to study enrollment, the AC and BI groups had similar patterns. Both groups averaged more than 2 D/DD, and had approximately one binge episode per month and 4 weeks that exceeded NIAAA sensible drinking limits for women. The BI group had more % DD than the AC group prior to enrollment (p=.053). In the 6 to 12 month period after study enrollment, there were no significant differences between treatment groups on any of the four drinking outcomes, all of which showed modest declines. Table 3 summarizes the pattern of alcohol use before and after study enrollment.
Table 3. Summary of Alcohol Consumption Before and After Enrollment.
| 6 months Before Enrollment | Brief Intervention, n=249 | Active Control, n=262 | p-value |
|---|---|---|---|
| Drinks/Drinking Days | 2.1 (1.4) | 2.2 (1.5) | 0.72 |
| % Drinking Days | 26% | 21% | 0.053 |
| Binge Episodes | 7.4 (24) | 5.7 (17) | 0.37 |
| Weeks > SDL | 4.2 (7.9) | 3.5 (7.1) | 0.26 |
| 6-12 months After Enrollment | Brief Intervention, n=239 | Active Control, n=252 | p-value |
| Drinks/Drinking Days | 2.0 (2.0) | 1.9 (1.6) | 0.60 |
| % Drinking Days | 22% | 20% | 0.52 |
| Binge Episodes | 6.0 (21) | 3.8 (13) | 0.17 |
| Weeks > SDL | 3.5 (7.5) | 2.8 (6.7) | 0.27 |
3.2.2 Changes in Measures of Drinking Outcome: Multivariate Analysis Results
Table 4 summarizes the unadjusted and adjusted changes in drinking outcomes between groups from pre-enrollment and 6 to 12 months afterward. A trend whereby the BI group had more improvement on % DD was identified (effect =.03, SE= .016, p=.07). Otherwise, there were no between group differences. The effects of specific covariates on the outcome measures are discussed subsequently.
3.2.2.1 Drinks per Drinking Day
In our multivariate model, we found a significant interaction between the initial number of D/DD and the treatment arm (interaction effect=-.29, SE=.09, p=.001). In this model the BI had the greatest effect on women with lower initial D/DD (effect=.56, SE=.22, p=.01). Three additional covariates had a significant effect in the multivariate model of change in D/DD. Two were associated with reduced number of D/DD: infertility compared to the hypertension reference group (effect=.43, SE=.21, p=.04; multigroup test across medical conditions, p=.27) and initial D/DD (effect=.45, SE=.06, p<.0001). Hispanic background was associated with a negative effect on D/DD improvement (effect=-.95, SE=-.29, p=.001).
3.2.2.2 Percent Drinking Days
Only two covariates had a statistically significant effect in the multivariate model of change in percent drinking days: the initial % DD (effect=.27, SE=.03, p<.0001) and infertility diagnosis compared to the hypertension reference group (effect=.06, SE=.03, p=.03; multigroup test across medical conditions, p=.008).
3.2.2.3 Binge Episodes
Several variables had significant effects on changes in binges. Covariates that had a positive effect on reduction of binges were the participant's age (effect=.14, SE=.07, p=.03), infertility diagnosis compared to the hypertension reference group (effect=5.60, SE=2.34, p=.02; multigroup test across medical conditions, p=.23), and initial number of binges (effect=.72, SE=.03, p<.0001). In contrast, the following covariates had a negative effect on binge reduction: lifetime alcohol use disorders (effect=-3.38, SE=1.47, p=.02), lifetime cocaine use disorders (effect=-8.30, SE=3.01, p=.01), and BI (effect=-2.68, SE=1.37, p=.05).
3.2.2.4 Weeks Exceeding Sensible Drinking Limits (> SDL)
Two covariates associated with reduced number of weeks exceeding SDL were: the initial number of weeks exceeding SDL (effect=.39, SE=.033), p<.001) and infertility diagnosis compared to the hypertension reference group (effect=3.05, SE=.85, p<.001; multigroup test across medical conditions, p=.003).
4.0 Discussion
The main finding of this randomized trial comparing brief intervention to active control is that there were no differences in subsequent alcohol use one year after enrollment. With a 96% follow-up rate, this study of 511 non-treatment seeking women with medical problems exacerbated by risky drinking is directly responsive to the stated need for more brief intervention trials focusing on women (Kaner et al., 2007). Two trends among the women receiving the brief intervention were noted; they had greater reductions in percent drinking days but little change in the number of binge episodes.
Study results update those reported in the seminal WHO cross- national trial of brief interventions that included 299 women who demonstrated significant reductions in drinking intensity of approximately 10% in treatment and control groups (WHO Brief Intervention Study Group, 1996). Similarly, studies including heavy drinking women attending general practices in Finland and the United Kingdom found that reductions in drinking did not differ between the control and brief intervention groups (Aalto et al., 2000; Scott & Anderson, 1990). In contrast, 205 women of child bearing age enrolled in Project TrEAT had greater reductions in alcohol consumption after two fifteen minute physician-delivered counseling visits that were still evident at four-year follow-up (Manwell et al., 2000).
Possible explanations for study findings include reactivity to assessment and the presence of medical conditions. For example, a study of 102 women with alcohol use disorders found that 44% were abstinent after assessment but before the first session of treatment (Epstein et al., 2005). Likewise, others have reported reactivity to assessment activities in samples of women drinkers (Worden et al., 2008). Hence, all women in the study may have changed some aspects of their drinking behavior as result of the assessment interview. The linkage of alcohol use to health problems may be especially compelling to women, who have been described to be very responsive to medically oriented approaches, and to evaluations and interventions in medical settings (Kauffman et al., 1997; Weisner & Schmidt, 1992). Some types of medical conditions in particular, may serve to motivate changes in drinking. For example, we found that women with infertility problems had the greatest reductions in alcohol consumption, regardless of group assignment. It might be speculated that women in treatment for infertility had the greatest, immediate motivation for any behavior modification that would improve their chances for pregnancy. The potential adverse consequences of chronic diseases such as hypertension, diabetes, or osteoporosis may occur in the more distant future.
The length of the brief intervention and length of follow-up afterwards are also important to take into account when comparing outcomes. Most reports indicate little additional benefit from longer brief interventions, with the median time being about 25 minutes (Kaner et al., 2007; Wutzke et al., 2006). Hence, it is possible that the study BI did not confer more therapeutic benefit after the hour-long assessment when drinking behaviors were assessed one year later; differences between the two groups might have been apparent if comparisons were made at other times. Results from other research groups vary from confirmation of the short term effects of brief interventions which disappeared by 12 months (Cunningham et al., 2010; Vasilaki et al., 2006; Wutzke et al., 2002), to sustained reductions in alcohol use in other circumstances (Manwell et al., 2000).
Finally, regression to the mean, which should have been equated across conditions within the limits of randomization and follow-up rates, needs to be considered in the context of these other explanations for study findings (Finney, 2007). Participants in both the treatment and control groups may have reported reductions as part of a natural downward trend (Cunningham, 2006). Furthermore, BI participants had higher but non-significant rates of current alcohol use disorders and percent drinking days at enrollment; which could bias the results to the null.
Some potential study limitations are noted. Women who were particularly motivated in managing their health habits may have enrolled in this study which required the return of a screening questionnaire, subsequent phone screen, and then study appointments. Although the study physicians were carefully trained and monitored, it is possible that the manner in which the brief interventions was given was not sufficiently persuasive. Indeed, the participants' own physicians might have been more influential in achieving behavior change if they gave the BI instead. Moreover, it is not known whether the participants discussed their alcohol use with their own doctors as result of their participation in the study. Their doctors might have then offered advice about drinking, which could have reflected any number of possibilities, including abstinence, reduction, or no change. Participants and study staff could not be blinded to treatment group assignment, similar to other studies taking place in medical settings (Saitz et al., 2007).
Other possible limitations include the reliance on self-reports of alcohol use. While the TLFB is considered reliable and valid over different lengths of recall, use of “real-time” assessments may have yielded different results. There were no contingencies regarding alcohol use, however there is experimental evidence that being screened and monitored for drinking behavior can lead to reduced self-reported hazardous drinking (McCambridge & Day, 2007). Such reductions may be real, or may reflect socially desirable responding in order to avoid making a negative impression (Welte & Russell 1993). A differential effect of recall bias may have been manifest within the BI and AC groups. It has been further suggested that “impression managers” are sensitive to their audience and may adjust their accounts accordingly (Davis et al., 2010). Follow-up interviews were conducted either in person or over the phone in similar proportions in both groups; available evidence indicates that an interviewer's physical presence may not be an important factor as a contributor to misreporting (Tourangeau & Yan, 2007). It is unlikely that the Research Assistants were perceived as intimidating, authority figures, despite their professional demeanor. Thus, while the potential limitations of self-report methods of drinking are acknowledged and likely equally applicable to both the treatment and active control groups, they still have been the major source about human drinking behavior in most studies because they are practical -- inexpensive, non-invasive, and acceptable to participants (Del Boca & Darkes, 2002).
Several strengths to the study might be mentioned. The sample consisted of a large and diverse group of 511 women. The 96% follow-up rate was high. The medical problems experienced by the women are common, exacerbated by risky drinking, and were confirmed by their physicians. The women were recruited from outpatient medical clinics at the study hospital and elsewhere in the contiguous area, which increases generalizability. Since most physicians have been reluctant to offer brief interventions themselves, one possible solution has been to delegate that work to “others” (Kuehn, 2008). This study used a collaborative model between physicians and other clinicians willing to screen, assess, and intervene. The physicians who offered the brief interventions were well trained in the method, having received periodic feedback since their patient sessions were taped and rated.
Some study observations may be helpful when considering future brief interventions for women. The BI was most helpful for women with fewer drinks per drinking day at the start of the study, and associated with a significantly greater reduction in mean percent drinking days. The BI was less helpful in reducing drinks per drinking day among Hispanic women and it did not moderate binge drinking. Lifetime history of both alcohol and cocaine use disorders had significant negative effects on the reduction of binge drinking. Infertility was the medical diagnosis associated with the greatest improvement in drinking overall, regardless of treatment group assignment. Thus, it appears that future efforts might focus on developing more effective means to modify binge drinking and identifying why the BI was less helpful among Hispanic women and women with chronic medical problems such as hypertension, diabetes, or osteoporosis. The impact of the BI might be enhanced if there were a linkage with a personal physician who could follow-up with the patient afterwards.
As the gender gap in alcohol use, abuse, and dependence in the United States narrows, and the frequency of at-risk and binge drinking among middle-aged and elderly adults increases, effective approaches to risky drinking women are more necessary than ever (Blazer & Wu, 2009). Since it is unlikely that treatments such as brief interventions can be beneficial to all, it is desirable to know for whom they will be beneficial, and perhaps even why. Results from this study contribute to the growing body of knowledge about brief interventions by its focus on 511 risky drinking women with medical diagnoses seen in outpatient clinical settings and its findings that improvements in treatment are needed.
Acknowledgments
Kari Braaten, MD, MPH, Jeremy Barowsky, MD, and Jason Caplan, MD gave brief interventions to study participants. Dr. Braaten also reviewed brief intervention study tapes for treatment fidelity.
This study was supported by grants from the NIAAA and the Office of Research on Women's Health (R01 AA 014678 and K24 AA 00289, both GC).
Footnotes
Preliminary results were presented at the 162nd Annual Meeting of the American Psychiatric Association, San Francisco, CA, 18 May, 2009.
The authors have no financial or personal conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aalto M, Saksanen R, Laine P, Forrstrom R, Raikaa M, Kiviluoto M, Seppa K, Sillanaukee P. Brief intervention for female heavy drinkers in routine general practice: a 3year randomized, controlled study. Alcoholism: Clinical and Experimental Research. 2000;24:1680–1686. [PubMed] [Google Scholar]
- American Diabetes Association. Alcohol. [Accessed: 08-25-2010]; http: www.diabetes.org/food-and-fitness/food/what-can-i-eat/alcohol.
- Anderson K, Nisenblat V, Norman R. Lifestyle factors in people seeking infertility treatment – a review. Australian and New Zealand Journal of Obstetrics and Gynecology. 2010;50:8–20. doi: 10.1111/j.1479-828X.2009.01119.x. [DOI] [PubMed] [Google Scholar]
- Baraona E, Abittan CS, Dohmen K, Moretti M, Pozzato G, Chayes ZW, Schaefer C, Lieber CS. Gender differences in pharmacokinetics of alcohol. Alcoholism: Clinical and Experimental Research. 2001;25:502–507. [PubMed] [Google Scholar]
- Berg KM, Kunins HV, Jackson JL, Nahvi S, Chaudury A, Harris KA, Malik K, Arnsten JH. Association between alcohol consumption and both osteoporotic fracture and bone density. American Journal of Medicine. 2008;121:406–418. doi: 10.1016/j.amjmed.2007.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blazer DG, Wu LT. The epidemiology of at-risk and binge drinking among middle-aged and elderly community adults: national survey on drug use and health. American Journal of Psychiatry. 2009;166:1162–1169. doi: 10.1176/appi.ajp.2009.09010016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brienza RS, Stein MD. Alcohol use disorders in primary care: do gender specific differences exist? Journal of General Internal Medicine. 2002;17:387–397. doi: 10.1046/j.1525-1497.2002.10617.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks CM, Richards JM, Kohler CL, Soong SJ, Martin B, Windsor RA, Bailey WC. Assessing adherence to asthma medication and inhaler regimens: A psychometric analysis of adult self-report scales. Medical Care. 1994;32:298–907. doi: 10.1097/00005650-199403000-00008. [DOI] [PubMed] [Google Scholar]
- Chang G, McNamara TK, Orav EJ, Koby D, Lavigne A, Ludman B, Vincitorio NA, Wilkins-Haug L. Brief intervention for prenatal alcohol use: a randomized trial. Obstetrics and Gynecology. 2005;105:991–8. doi: 10.1097/01.AOG.0000157109.05453.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Karmarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24:385–396. [PubMed] [Google Scholar]
- Cunningham JA. Regression to the mean: what does it mean? Alcohol and Alcoholism. 2006;41:580. doi: 10.1093/alcalc/agl039. [DOI] [PubMed] [Google Scholar]
- Cunningham JA, Wild TC, Cordingly J, Van Mierlo T, Humphreys K. Twelve-month follow-up results from a randomized controlled trial of a brief personalized feedback intervention for problem drinkers. Alcohol and Alcoholism. 2010;45:258–262. doi: 10.1093/alcalc/agq009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis CG, Thanke J, Vilhena N. Social desirability biases in self-reported alcohol consumption and harms. Addictive Behaviors. 2010;35:302–311. doi: 10.1016/j.addbeh.2009.11.001. [DOI] [PubMed] [Google Scholar]
- Del Boca FK, Darkes J. The validity of self-reports of alcohol consumption: state of the science and challenges for research. Addiction. 2003;98(Suppl 2):1–12. doi: 10.1046/j.1359-6357.2003.00586.x. [DOI] [PubMed] [Google Scholar]
- Epstein EE, Drapkin ML, Yusko DA, Cook SM, McCrady BS, Jensen NK. Is alcohol assessment therapeutic? Pretreatment change in drinking among alcohol-dependent women. Journal of Studies on Alcohol. 2005;66:369–378. doi: 10.15288/jsa.2005.66.369. [DOI] [PubMed] [Google Scholar]
- Finney JW. Regression to the mean in substance use disorder treatment research. Addiction. 2007;103:42–52. doi: 10.1111/j.1360-0443.2007.02032.x. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV TR Axis I Disorders – Non-Patient Edition (SCID-I/NP 11/2002 Revision) Biometrics Research Department, New York State Psychiatric Institute; New York: 2002. [Google Scholar]
- Gupman AE, Svikis D, McCaul ME, Anderson J, Santora PB. Detection of alcohol and drug problems in an urban gynecology clinic. Journal of Reproductive Medicine. 2002;47:404–410. [PubMed] [Google Scholar]
- Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States. Archives of General Psychiatry. 2007;64:830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- Homan GF, Davies M, Norman R. The impact of lifestyle factors on reproductive performance in the general population and those undergoing infertility treatment: a review. Human Reproductive Update. 2007;13:209–223. doi: 10.1093/humupd/dml056. [DOI] [PubMed] [Google Scholar]
- Kaner EF, Dickinson HO, Beyer EF, Schlesinger C, Heather N, Saunders JB, Burnand B, Pienaar ED. Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database of Systematic Reviews. 2007;(2) doi: 10.1002/14651858.CD004148.pub. Art No. CD 004148. [DOI] [PubMed] [Google Scholar]
- Kaner EFS, Heather N, Brodie J, Lock CA, McAvoy BR. Patient and practitioner characteristics predict brief alcohol intervention in primary care. British Journal of General Practice. 2001;51:822–827. [PMC free article] [PubMed] [Google Scholar]
- Karjane NW, Stovall DW, Berger NG, Svikis DS. Alcohol abuse risk factors and psychiatric disorders in pregnant women with a history of infertility. Journal of Women's Health. 2008;17:1623–7. doi: 10.1089/jwh.2007.0651. [DOI] [PubMed] [Google Scholar]
- Kauffman SE, Silver P, Poulin J. Gender differences in attitudes toward alcohol, tobacco, and other drugs. Social Work. 1997;42:231–241. doi: 10.1093/sw/42.3.231. [DOI] [PubMed] [Google Scholar]
- Keyes KM, Brant DF, Hasin DF. Evidence for a closing gender gap in alcohol use, abuse, and dependence in the United States population. Drug and Alcohol Dependence. 2008;93:21–29. doi: 10.1016/j.drugalcdep.2007.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klatsky AL, Gunderson EP, Kipp H, Udaltsova N, Friedman GD. Higher prevalence of systemic hypertension among moderate alcohol drinkers: an exploration of the role of underreporting. Journal of Studies on Alcohol. 2006;67:421–438. doi: 10.15288/jsa.2006.67.421. [DOI] [PubMed] [Google Scholar]
- Koppes LLJ, Dekker JM, Hendriks HFJ, Bouter LM, Heine RJ. Moderate alcohol consumption lowers the risk of type 2 diabetes. Diabetes Care. 2005;28:719–725. doi: 10.2337/diacare.28.3.719. [DOI] [PubMed] [Google Scholar]
- Kuehn BM. Despite benefit, physicians slow to offer brief advice on harmful alcohol use. JAMA. 2008;299:751–753. doi: 10.1001/jama.299.7.751. [DOI] [PubMed] [Google Scholar]
- Maciosek MV, Coffield AB, Edwards NM, Flottemesch TH, Goodman MJ, Solberg LI. Priorities among effective clinical preventive services. Results of a systematic review and analysis. American Journal of Preventive Medicine. 2006;31:52–61. doi: 10.1016/j.amepre.2006.03.012. [DOI] [PubMed] [Google Scholar]
- Manwell LB, Fleming MF, Mundt MP, Stauffacher EA, Barry KL. Treatment of problem alcohol use in women of childbearing age: Results of a brief intervention trial. Alcoholism: Clinical and Experimental Research. 2000;24:1517–1524. [PubMed] [Google Scholar]
- McCambridge J, Day M. Randomized controlled trial of the effects of completing alcohol use disorders identification test questionnaire on self-reported hazardous drinking. Addiction. 2007;103:241–248. doi: 10.1111/j.1360-0443.2007.02080.x. [DOI] [PubMed] [Google Scholar]
- McQuade WH, Levy SM, Yanek LR, Davis SW, Liepman MR. Detecting symptoms of alcohol abuse in primary care settings. Archives of Family Medicine. 2000:814–21. doi: 10.1001/archfami.9.9.814. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational Interviewing. New York: The Guilford Press; 1991. [Google Scholar]
- Moyer A, Finney JW, Swearingen CE, Vergun P. Brief interventions for alcohol problems: a meta-analytic review of controlled investigations in treatment-seeking and non-treatment-seeking populations. Addiction. 2002;97:279–292. doi: 10.1046/j.1360-0443.2002.00018.x. [DOI] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. Helping patients who drink too much A clinician's guide. 2007. NIH Publication No. 07-3769, Revised January 2007. [Google Scholar]
- National Institutes of Health. Personal Steps to A Healthy Choice: A Woman's Guide. 2000. NIH Publication No. 00-4370. [Google Scholar]
- Nuro KF, Maccarelli L, Baker SM, Martino S, Rounsaville BJ, Carroll KM. Yale Adherence and Competence Scale (YACS II) Guidelines, Second Edition. West Haven, CT: Yale University Psychotherapy Development Center Training; 2005. (7). [Google Scholar]
- O'Keefe JH, Bybee KA, Lavie CJ. Alcohol and cardiovascular health. Journal of the American College of Cardiology. 2007;11:1009–14. doi: 10.1016/j.jacc.2007.04.089. [DOI] [PubMed] [Google Scholar]
- Saitz R, Palfai TP, Cheng DM, Horton NJ, Freedner N, Dukes K, Kraemer KL, Roberts MS, Guerriero RT, Samet JH. Brief intervention for medical inpatients with unhealthy alcohol use. Annals of Internal Medicine. 2007;146:167–776. doi: 10.7326/0003-4819-146-3-200702060-00005. [DOI] [PubMed] [Google Scholar]
- Scott E, Anderson P. Randomized controlled trial of general practitioner intervention in women with excessive alcohol consumption. Drug and Alcohol Review. 1990;10:313–321. doi: 10.1080/09595239100185371. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline Followback: A technique for assessing self-reported ethanol consumption. In: Allen J, Litten RZ, editors. Measuring alcohol consumption: psychosocial and biological methods. Totowa, NJ: Humana Press; 1992. pp. 41–72. [Google Scholar]
- Sokol RJ, Martier SS, Ager JW. The T-ACE questions: practical prenatal detection of risk-drinking. American Journal of Obstetrics and Gynecology. 1989;160:863–71. doi: 10.1016/0002-9378(89)90302-5. [DOI] [PubMed] [Google Scholar]
- Stevenson JS, Masters JA. Predictors of alcohol use misuse and abuse in older women. Journal of Nursing Scholarship. 2005;37:329–35. doi: 10.1111/j.1547-5069.2005.00057.x. [DOI] [PubMed] [Google Scholar]
- Tourangeau R, Yan T. Sensitive questions in surveys. Psychological Bulletin. 2007;133:859–883. doi: 10.1037/0033-2909.133.5.859. [DOI] [PubMed] [Google Scholar]
- Vasilaki EI, Hosier SG, Cox WM. The efficacy of motivational interviewing as a brief intervention for excessive drinking: A meta-analytic review. Alcohol and Alcoholism. 2006;41:328–335. doi: 10.1093/alcalc/agl016. [DOI] [PubMed] [Google Scholar]
- Ware JE, Sherbourne CD. The MOS-36 Item Short Form Health Status Survey (SF-36). I. Conceptual framework and item selection. Medical Care. 1992;30:MS253–MS265. [PubMed] [Google Scholar]
- Weisner C, Schmidt L. Gender disparities in treatment for alcohol problems. JAMA. 1992;268:1872–1876. [PubMed] [Google Scholar]
- Welte JW, Russell M. Influence of socially desirable responding in a study of stress and substance abuse. Alcoholism: Clinical and Experimental Research. 1993;17:758–761. doi: 10.1111/j.1530-0277.1993.tb00836.x. [DOI] [PubMed] [Google Scholar]
- US Preventive Services Task Force. Screening and behavioral counseling interventions in primary care to reduce alcohol misuse: A recommendation statement. Annals of Internal Medicine. 2004;140:554–556. doi: 10.7326/0003-4819-140-7-200404060-00016. [DOI] [PubMed] [Google Scholar]
- WHO Brief Intervention Study Group. A cross-national trial of brief interventions with heavy drinkers. American Journal of Public Health. 1996;86:948–955. doi: 10.2105/ajph.86.7.948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Worden BL, McCrady BS, Epstein EE. Assessment reactivity to follow-up in a study of women's treatment for alcohol dependence. Addictive Behaviors. 2008;33:831–5. doi: 10.1016/j.addbeh.2007.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wutzke SE, Conigrave KM, Saunders JB, Hall WD. The long-term effectiveness of brief interventions for unsafe alcohol consumption: a 10 year follow-up. Addiction. 2002;97:665–675. doi: 10.1046/j.1360-0443.2002.00080.x. [DOI] [PubMed] [Google Scholar]
- Zhang SM, Lee IM, Manson JE, Cook NR, Willett WD, Buring JE. Alcohol consumption and breast cancer risk in the women's health study. American Journal of Epidemiology. 2007;165:667–676. doi: 10.1093/aje/kwk054. [DOI] [PubMed] [Google Scholar]