Abstract
A disturbance in eating behavior is the defining characteristic of the clinical eating disorders, Anorexia Nervosa, Bulimia Nervosa, and Binge Eating Disorder. Surprisingly little research has been devoted to assessing objectively the nature of the eating disturbances in these disorders, to elucidating what factors contribute to the development and persistence of these disturbances, or to describing how they change with treatment. This review, which is based on a Mars lecture delivered at the 2010 meeting of the Society for the Study of Ingestive Behavior, reviews objective information about the nature of the disturbances of eating behavior in eating disorders. These data suggest that more detailed knowledge of eating behavior is an essential component of a full understanding of eating disorders and may provide a foundation for studies of pathophysiology and for the development of new treatment methods.
Keywords: Anorexia Nervosa, Bulimia Nervosa, Binge Eating Disorder, eating behavior
Introduction
This review is based on a Mars lecture given at the 2011 meeting of the Society for the Study of Ingestive Behavior. The focus of the lecture was on the relevance of research on eating behavior to our understanding of the “classic” eating disorders, Anorexia Nervosa, Bulimia Nervosa, and Binge Eating Disorder. This paper will briefly review work on Bulimia Nervosa and Binge Eating Disorder, and will focus more on recent work on the study of Anorexia Nervosa. As did the lecture, the paper will be based primarily on work conducted at the Eating Disorders Research Unit at New York State Psychiatric Institute, Columbia University Medical Center.
Bulimia Nervosa
The salient feature of Bulimia Nervosa is the occurrence of recurrent episodes of binge eating accompanied by inappropriate behavior to avoid weight gain, typically self-induced vomiting. The current DSM-IV diagnostic criteria also require that both the binge eating and the inappropriate compensatory behavior occur at least twice a week for three months [1]. Individuals with Bulimia Nervosa are typically women of normal weight in their teens or early 20s who are very concerned about their shape and weight.
When Bulimia Nervosa first came to prominence in the early 1980s, much was unclear about the nature of this disorder. A fundamental question was whether patients’ reports of the consumption of very large amounts of food in short periods of time were accurate, or, rather, were a reflection of their anxiety about the consumption of what were, in fact, only modest amounts of food.
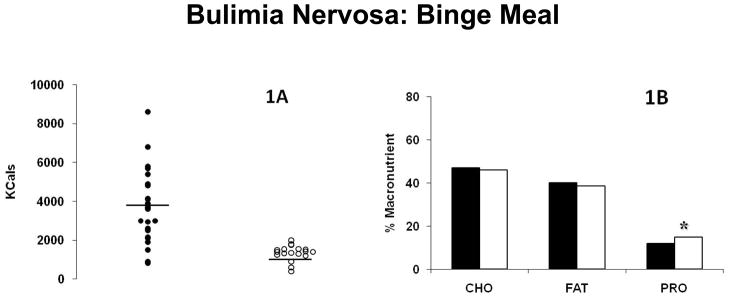
Our group, in close elaboration with that of Harry Kissileff, PhD, embarked on a series of studies aimed at the objective assessment of the eating behavior of individuals with Bulimia Nervosa [2]. Our initial studies were quite straightforward. We provided patients with a multi-item array of foods, and simply asked them to engage in binge eating of the type that they engaged in outside the laboratory. They were provided access to a bathroom if they wished to purge. While not all individuals were able to do so, a sufficient number were able to comply with the request to binge eat to permit the measurement of their eating behavior. Under these conditions, individuals with Bulimia Nervosa consumed substantially larger amounts of food, almost 4000 Kcals, than did control subjects given the identical instructions, who consumed just over 1000 Kcals (Figure 1A). In addition, the types of foods chosen by individuals with Bulimia Nervosa did not support the then-popular notion that this disorder was characterized by “carbohydrate craving.” Both patient and control groups selected meals with macronutrient compositions similar to that of the average American diet, with approximately 50% of calories from carbohydrates, 40% from fat, and 10% from protein (Figure 1B).
Figure 1.
Kilocalorie content (1A) and macronutrient composition (1B) of binge meals of patients with Bulimia Nervosa. In 1A, filled circles are from patient meals and open circles are from control meals. In 1B, filled columns indicate means of patient meals and open columns indicate means of control meals. Adapted from [2].
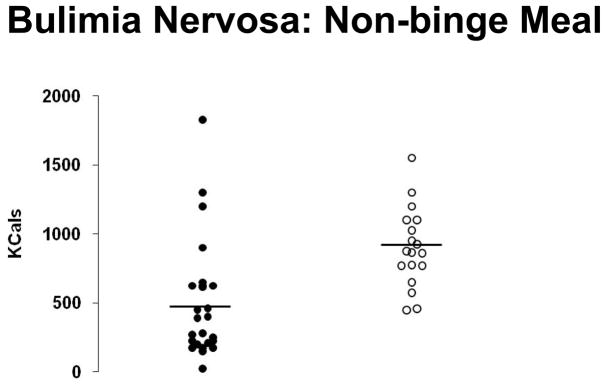
We also asked both patients and controls to consume a non-binge meal, that is, an amount of food that they could eat comfortably without the need to purge afterwards. Under these conditions, patients with Bulimia Nervosa consumed significantly fewer calories than controls (Figure 2). These results indicated that the abnormalities in eating behavior in Bulimia Nervosa were not confined to episodes of binge eating, and were consistent with clinical reports that, when not binge eating, individuals with Bulimia Nervosa markedly restrict their food intake, leading to a vicious cycle of binge eating followed by food restriction in an attempt to compensate which then leads to increased appetite, setting the stage for another episode of binge eating. The laboratory documentation of this pattern provides a foundation for a major component of cognitive-behavioral therapy (CBT), the most effective psychological treatment for Bulimia Nervosa [3]. Specifically, one of the important first steps in CBT is to encourage patients to consume more during non-binge meals to interrupt the restrict-binge-restrict cycle.
Figure 2.
Kilocalorie content of non-binge meals of patients with Bulimia Nervosa. Filled circles are from patient meals and open circles are from control meals. Adapted from [2].
These initial studies of Bulimia Nervosa were important in several regards. Critically, they demonstrated that disturbances in eating behavior could be examined objectively in a laboratory setting, thereby avoiding the necessity of relying solely on self-report data which are notoriously inaccurate. (At the same time, it cannot be automatically assumed that the behavior of subjects in laboratory is identical to their behavior outside such settings.) The results buttressed important clinical observations regarding key characteristics of the disorder, for example, that binge eating episodes were, in fact, objectively large, and that, as just noted, individuals with Bulimia Nervosa tend to restrict their food intake when not binge eating.
A crucial finding about the eating behavior of individuals with Bulimia Nervosa during binge episodes was that the salient disturbance was in the control of the amount consumed, rather than the consumption of a specific food or macronutrient. Combined with the extensive literature on the controls of food intake in animals, this observation laid the foundation for substantial work over the last 20 years by the Columbia group and others on the development of satiety in Bulimia Nervosa [4], on post-prandial disturbances in CCK release [5–8], and on gastric and autonomic functioning [9, 10]. While this work has been highly informative, it has not yet succeeded in definitively answering the critical question of whether individuals with Bulimia Nervosa have a disturbance in satiety that sets the stage for binge eating, or whether, because of emotional or cognitive difficulties, normal signals of satiety are overridden by individuals with the disorder [11].
Binge Eating Disorder
Although Binge Eating Disorder was described in 1959 [12], it came to prominence in 1994 when the fourth edition of the Diagnostic and Statistical Manual of the American Psychiatric Association (DSM-IV) was under development [1]. While Binge Eating Disorder was not formally recognized in DSM-IV, criteria were provided in an appendix for further study. The provision of these criteria has spurred substantial research interest in Binge Eating Disorder, and it is currently recommended for inclusion in DSM-5. The hallmark feature of Binge Eating Disorder is the occurrence of recurrent episodes of binge eating in the absence of the inappropriate compensatory behavior characteristic of individuals with Bulimia Nervosa. In contrast to those with Bulimia Nervosa, individuals with Binge Eating Disorder tend to be overweight or obese and middle-aged.
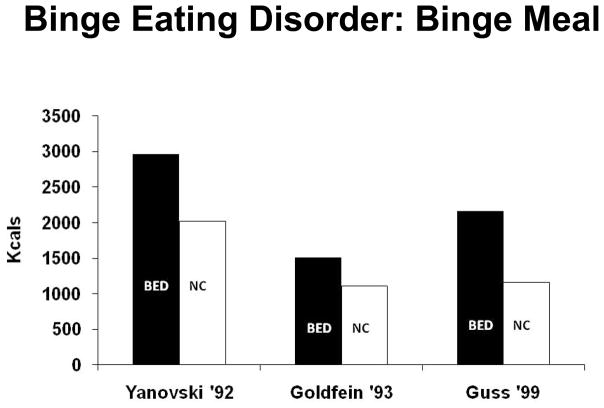
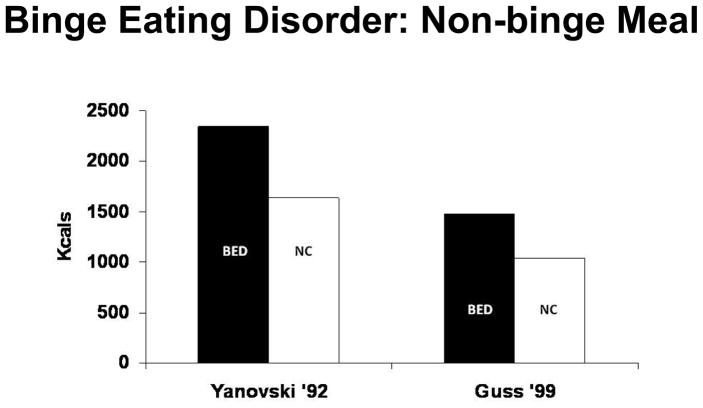
A modest amount of research has focused on characterizing the eating behavior of individuals with Binge Eating Disorder. Using techniques similar to those developed to examine Bulimia Nervosa, several studies documented that individuals with Binge Eating Disorder, compared to individuals of similar age and body weight, consume significantly more food in a laboratory setting when asked to binge eat (Figure 3) [13]. However in contrast to individuals with Bulimia Nervosa, who undereat when asked not to binge eat in a laboratory meal, individuals with Binge Eating Disorder consume more than comparable controls even when not asked to binge eat. (Figure 4)
Figure 3.
Average kilocalorie content of binge meals of patients with Binge Eating Disorder (BED) and controls (NC) from three studies. Filled columns indicate means of patient meals and open columns indicate means of control meals.
Figure 4.
Average kilocalorie content of non-binge meals of patients with Binge Eating Disorder (BED) and controls (NC) from two studies. Filled columns indicate means of patient meals and open columns indicate means of control meals.
These findings are both reassuring and perplexing. As in the case of Bulimia Nervosa, it is reassuring that individuals with Binge Eating Disorder, at least in the laboratory setting, exhibit eating behavior that is distinctly abnormal. This well-replicated observation suggests that the core abnormality of Binge Eating Disorder is a disturbance in eating behavior, not in the perception of what is eaten. What is perplexing is the observation that individuals with Binge Eating Disorder consume more than controls during both binge and non-binge meals. If the laboratory meal data were representative of meals outside the laboratory, one would expect individuals with Binge Eating Disorder to be gaining weight much more rapidly than comparable controls. The limited data available do not support this. Of course, it is conceivable that individuals with Binge Eating Disorder eat larger but fewer meals than controls or that they have elevated levels of energy expenditure, but there are no solid data to support these hypotheses.
Another reason for concern about the nature of the disturbance in eating behavior in Binge Eating Disorder emerges from treatment studies. A range of psychological and pharmacological interventions has been shown to be effective in reducing binge eating in Binge Eating Disorder [14]. Yet, remarkably, there is no systematic relationship between change in binge eating behavior and change in weight. In some studies, for example, psychological interventions led to a virtual cessation of binge eating, yet weight remained stable [15]. While other explanations are possible, such as a redistribution of calories among meals as binge eating ceases, it is also conceivable that treatment for Binge Eating Disorder, rather than changing the behavior itself, alters the level of distress about eating behavior and, therefore, whether an episode of eating is viewed as a binge. This is a fundamental question about the nature of Binge Eating Disorder: to what degree is the fundamental problem an objective disturbance in eating behavior and to what degree is it an altered perception of eating behavior that is within normal limits in our current environment? It is difficult to know how this critical question can be resolved until methods are developed to assess eating behavior accurately on an ambulatory basis.
Anorexia Nervosa
Anorexia Nervosa is the “oldest” eating disorder having been clearly recognized in the 19th century [16]. The salient features of Anorexia Nervosa are a relentless pursuit of thinness through dieting and exercise associated with intense fear of gaining weight or becoming fat despite the achievement of a significantly low body weight. The disorder primarily affects girls and young women and can be life-threatening, with a mortality rate as high as that of any psychiatric disorder.
Characteristic Eating Behavior
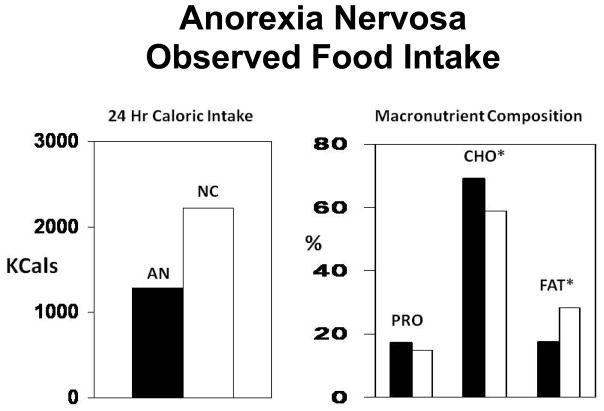
The eating behavior of individuals with Anorexia Nervosa has received surprisingly little attention, perhaps because of the challenge of studying a behavior that affected individuals avoid engaging in. Clinical descriptions are very consistent, noting a strong aversion to the consumption of foods viewed as fattening. A few studies have examined eating behavior in Anorexia Nervosa in a laboratory setting. For example, Hadigan et al. [17] documented that, when allowed to choose their own menus, individuals with Anorexia Nervosa, while on a clinical research unit, consumed far fewer calories than controls, especially by reducing calories from fat (Figure 5)
Figure 5.
Average kilocalorie and macronutrient composition of observed meals of patients with Anorexia Nervosa (AN) and controls (NC). Data from [17].
Change with Treatment
Having developed methods to examine the eating behavior of individuals with Bulimia Nervosa and Binge Eating Disorder, our group more recently became interested in applying such methods to the study of individuals with Anorexia Nervosa. An initial question was how eating behavior changed during treatment.
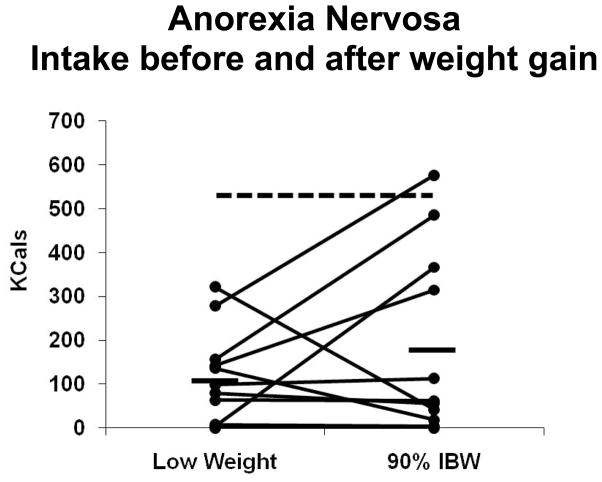
Most individuals with Anorexia Nervosa can be successfully helped to gain weight in structured treatment programs such as day hospitals and inpatient facilities. Treatment on our inpatient research unit typically lasts 2 to 3 months during which time patients gain substantial weight and show significant improvement on most psychological measures. By the end of their hospital stay, patients' daily food intake routinely exceeds 3000 kcals, and it is apparent that, in this structured and supervised setting, eating behavior has changed dramatically. Sysko et al. [18] attempted to assess changes in unsupervised eating behavior by asking individuals hospitalized on the unit to consume their lunch from an opaque container containing a strawberry yogurt shake beverage with which they were unfamiliar. Individuals were studied on two occasions, at the beginning and near the end of their hospital stays. In the first meal, patients consumed about 100 kcals on average, substantially less than mean of over 500 kcals consumed by control subjects. The average patient intake during the second meal increased slightly but not significantly, and remained under 200 kcals (Figure 6).
Figure 6.
Kilocalorie intake of 12 patients with Anorexia Nervosa from a single-item lunch meal before and after weight gain. Dashed line indicates average intake of control group. Data from [18].
Mayer et al. [19] recently replicated and extended these findings. Patients were again asked to consume lunch meals near the beginning and at the end of their hospital stays, but, in this experiment, they were free to choose their lunch from a multi-item array. In the first meal, the average patient intake was 364 kcals, which increased significantly to 516 kcals at the second meal. However, intake on both occasions was significantly less than that of controls, who consumed over 750 kcals. The average percent of calories derived from fat in the patient meals also increased, from approximately 20 to 25%. However, it remained substantially below that of the controls, who derived approximately 40% of their calories from fat. Mayer et al. also found that the dietary energy density (kcals per gram of food consumed) and the diet variety score (the number of different foods consumed) did not change between the first and second meals, and were significantly lower than those of controls.
These findings indicate that, despite substantial weight gain and improvement in many psychological characteristics and despite dramatic increases in food intake during supervised meals, the “spontaneous” eating behavior of individuals with Anorexia Nervosa remains quite abnormal following intensive and lengthy care.
Clinical Significance
Several studies suggest that the lack of greater change in eating behavior during treatment for Anorexia Nervosa has substantial clinical significance. Schebendach et al. [20] examined the relationship between eating behavior immediately prior to hospital discharge and outcome over the next year. Eating behavior was assessed from four-day food records obtained immediately prior to hospital discharge, and outcomes were categorized according to the Morgan-Russell scale, a standard measure used to assess individuals with Anorexia Nervosa. Twenty-nine of 41 patients were judged to have fair or better outcomes versus 12 who were categorized as having done poorly. Analysis of the diet records found that the two groups reported similar total caloric intakes prior to discharge of about 2300 kcal per day. However, the poor outcome group reported obtaining a lower fraction of calories from fat (21 ± 3.8% versus 25 ± 5.1%, p = 0.01) and a lower diet variety score (12.8 ± 2.4 versus 11.1 ± 1.6 foods/day, p = 0.01).
Additional, albeit circumstantial, evidence regarding the importance of eating behavior in avoiding relapse after initial treatment for Anorexia Nervosa derives from an analysis of factors predicting successful weight maintenance following weight restoration in a hospital-based program. In collaboration with the University of Toronto, the Columbia group found that the antidepressant fluoxetine had no impact in reducing the rate of relapse in the year following successful acute treatment [21]. Subsequent analysis of a wide range of clinical, psychological, and behavioral features found that only two were significant predictors of successful weight maintenance during the 6 to 12 months following hospital discharge [22]. The two features were both weight related: BMI at the time of discharge and rate of weight loss in the first month following discharge. Since all patients entering the study had reached a normal BMI during hospital treatment, the difference in BMI at the time of hospital discharge between the success and failure groups was very small (20.5 ± 0.52 kg/m2 versus 20.1 ± 0.44 kg/m2), and presumably reflects greater caloric consumption in the success group in the days prior to discharge. While changes in weight reflect not only caloric intake but also energy expenditure, we hypothesize that it is those individuals who leave the supervised setting of the hospital with the ability to consume a varied diet with higher caloric density fare best. These data suggest that the outcome of treatment for Anorexia Nervosa may be improved through increased focus on improving patients’ narrow range of food choices and their persistent avoidance of fat.
Factors Possibly Affecting
Eating Behavior In experienced and structured treatment settings, the eating behavior of individuals with Anorexia Nervosa can largely be normalized as long as the behavior is closely monitored. The results just reviewed suggest that, once such structure is withdrawn, characteristic abnormalities in eating behavior are likely to recur and increase the probability of relapse. However, this emphasis on eating behavior in Anorexia Nervosa does not imply that Anorexia Nervosa can be understood solely in behavioral terms. A range of biological, psychological, and environmental influences undoubtedly contributes to the development of Anorexia Nervosa. However, given the key role of disturbances in eating behavior in the perpetuation of the disorder, the identification of factors proximally related to these behavioral disturbances is potentially of substantially importance. Pre-meal anxiety is a possible candidate.
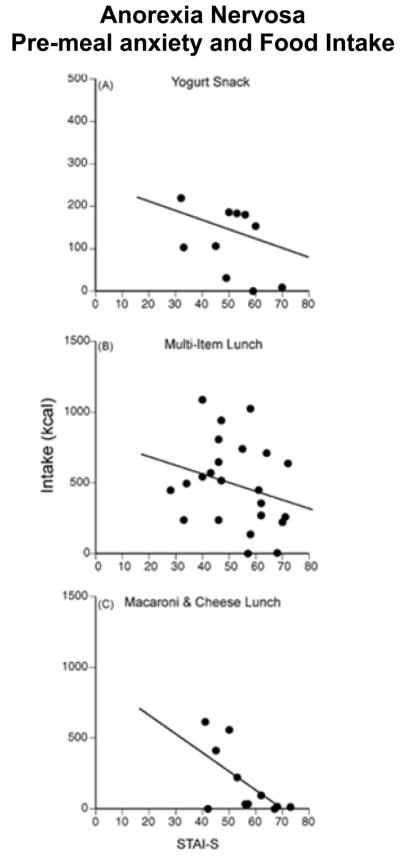
It has long been recognized that a range of anxiety disturbances are associated with Anorexia Nervosa. For example, a significant fraction of individuals with Anorexia Nervosa also meets criteria for Obsessive-Compulsive Disorder. Recent preliminary data from our group suggest that the level of anxiety immediately prior to a meal is inversely related to the amount consumed (Figure 7) [23]. If confirmed by further studies, these results may suggest a path for new treatment strategies. For example, exposure and response prevention paradigms have documented utility in the treatment of Obsessive-Compulsive Disorder and might usefully be extended to the treatment of Anorexia Nervosa [24].
Figure 7.
Pre-meal anxiety and kilocalorie intake across three laboratory test meals in individuals with Anorexia Nervosa. Pre-meal anxiety was measured by Spielberger State-Trait Inventory, State version (STAI-S).From [23].
Conclusion
Disturbances in eating behavior are defining characteristics of the clinical eating disorders Anorexia Nervosa, Bulimia Nervosa, and Binge Eating Disorder. This review documents that these disturbances can be studied objectively and that such studies yield reproducible results that are clearly linked to clinical phenomena. Direct examination of eating behavior provides a potential method for identifying psychobiological factors that contribute to the perpetuation of these disturbances. Given the extensive literature on the controls of eating behavior in animals, such studies also provide an obvious basis for translational work. Finally, recent work on Anorexia Nervosa suggests that the persistence of characteristic abnormalities in eating behavior sets the stage for the perpetuation of this serious illness. Therefore, increased understanding of the psychological and biological factors that underlie these behavioral disturbances may provide a useful way of enhancing both our understanding of and our ability to treat this challenging illness.
Acknowledgments
Harry Kissileff PhD, Michael Devlin MD, Ellen Zimmerli PhD and the staff of the Eating Disorders Research Unit and the New York State Psychiatric Institute made major contributions to the conduct of the work described.
References
- 1.American Psychiatric Association. Task Force on DSM-IV. Diagnostic and statistical manual of mental disorders : DSM-IV. 4. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 2.Walsh BT, Hadigan CM, Kissileff HR, Lachaussee JL. Bulimia Nervosa: A Syndrome of Feast and Famine. In: Anderson GH, Kennedy SH, editors. The Biology of Feast and Famine: Relevance to Eating Disorders. San Diego: Academic Press, Inc; 1992. pp. 1–20. [Google Scholar]
- 3.Wilson GT, Grilo CM, Vitousek KM. Psychological treatment of eating disorders. Am Psychol. 2007;62:199–216. doi: 10.1037/0003-066X.62.3.199. [DOI] [PubMed] [Google Scholar]
- 4.Kissileff H, Wentzlaff T, Guss J, Walsh B, Devlin M, Thornton J. A direct measure of satiety disturbance in patients with bulimia nervosa. Physiology & behavior. 1996;60:1077–85. doi: 10.1016/0031-9384(96)00086-8. [DOI] [PubMed] [Google Scholar]
- 5.Devlin MJ, Walsh BT, Guss JL, Kissileff H, Liddle R, Petkova E. Postprandial cholecystokinin release and gastric emptying in patients with bulimia nervosa. American Journal of Clinical Nutrition. 1997;65:114. doi: 10.1093/ajcn/65.1.114. [DOI] [PubMed] [Google Scholar]
- 6.Geracioti TD, Jr, Liddle RA. Impaired cholecystokinin secretion in bulimia nervosa. New England Journal of Medicine. 1988;319:683–8. doi: 10.1056/NEJM198809153191105. [DOI] [PubMed] [Google Scholar]
- 7.Keel PK, Wolfe BE, Liddle RA, De Young KP, Jimerson DC. Clinical features and physiological response to a test meal in purging disorder and bulimia nervosa. Archives of general psychiatry. 2007;64:1058. doi: 10.1001/archpsyc.64.9.1058. [DOI] [PubMed] [Google Scholar]
- 8.Pirke KM, Kellner MB, Frieß E, Krieg JC, Fichter MM. Satiety and cholecystokinin. International Journal of Eating Disorders. 1994;15:63–9. doi: 10.1002/1098-108x(199401)15:1<63::aid-eat2260150108>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 9.Faris PL, Kim SW, Meller WH, Goodale RL, Oakman SA, Hofbauer RD, et al. Effect of decreasing afferent vagal activity with ondansetron on symptoms of bulimia nervosa: a randomised, double-blind trial. The Lancet. 2000;355:792–7. doi: 10.1016/S0140-6736(99)09062-5. [DOI] [PubMed] [Google Scholar]
- 10.Geliebter A, Melton P, McCray RS, Gallagher DR, Gage D, Hashim SA. Gastric capacity, gastric emptying, and test-meal intake in normal and bulimic women. American Journal of Clinical Nutrition. 1992;56:656. doi: 10.1093/ajcn/56.4.656. [DOI] [PubMed] [Google Scholar]
- 11.Zimmerli EJ, Devlin MJ, Kissileff HR, Walsh BT. The development of satiation in bulimia nervosa. Physiology & behavior. 2010;100:346–9. doi: 10.1016/j.physbeh.2010.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stunkard AJ. Eating patterns and obesity. Psychiatric Quarterly. 1959;33:284–95. doi: 10.1007/BF01575455. [DOI] [PubMed] [Google Scholar]
- 13.Walsh BT, Boudreau G. Laboratory studies of binge eating disorder. International Journal of Eating Disorders. 2003;34:S30–S8. doi: 10.1002/eat.10203. [DOI] [PubMed] [Google Scholar]
- 14.Brownley KA, Berkman ND, Sedway JA, Lohr KN, Bulik CM. Binge eating disorder treatment: a systematic review of randomized controlled trials. International Journal of Eating Disorders. 2007;40:337–48. doi: 10.1002/eat.20370. [DOI] [PubMed] [Google Scholar]
- 15.Wilfley DE, Welch RR, Stein RI, Spurrell EB, Cohen LR, Saelens BE, et al. A randomized comparison of group cognitive-behavioral therapy and group interpersonal psychotherapy for the treatment of overweight individuals with binge-eating disorder. Archives of general psychiatry. 2002;59:713. doi: 10.1001/archpsyc.59.8.713. [DOI] [PubMed] [Google Scholar]
- 16.Silverman JA. Charcot's comments on the therapeutic role of isolation in the treatment of anorexia nervosa. International Journal of Eating Disorders. 1997;21:295–8. doi: 10.1002/(sici)1098-108x(199704)21:3<295::aid-eat10>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 17.Hadigan CM, Anderson EJ, Miller KK, Hubbard JL, Herzog DB, Klibanski A, et al. Assessment of macronutrient and micronutrient intake in women with anorexia nervosa. International Journal of Eating Disorders. 2000;28:284–92. doi: 10.1002/1098-108x(200011)28:3<284::aid-eat5>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 18.Sysko R, Walsh BT, Schebendach J, Wilson GT. Eating behavior among women with anorexia nervosa. American Journal of Clinical Nutrition. 2005;82:296. doi: 10.1093/ajcn.82.2.296. [DOI] [PubMed] [Google Scholar]
- 19.Mayer LES, Schebendach J, Bodell LP, Shingleton RM, Walsh BT. Eating behavior in anorexia nervosa: before and after treatment. International Journal of Eating Disorders. doi: 10.1002/eat.20924. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schebendach JE, Mayer LES, Devlin MJ, Attia E, Contento IR, Wolf RL, et al. Dietary energy density and diet variety as predictors of outcome in anorexia nervosa. American Journal of Clinical Nutrition. 2008;87:810. doi: 10.1093/ajcn/87.4.810. [DOI] [PubMed] [Google Scholar]
- 21.Walsh BT, Kaplan AS, Attia E, Olmsted M, Parides M, Carter JC, et al. Fluoxetine after weight restoration in anorexia nervosa: a randomized controlled trial. Jama. 2006;295:2605–12. doi: 10.1001/jama.295.22.2605. [DOI] [PubMed] [Google Scholar]
- 22.Kaplan A, Walsh B, Olmsted M, Attia E, Carter J, Devlin M, et al. The slippery slope: prediction of successful weight maintenance in anorexia nervosa. Psychological medicine. 2009;39:1037–45. doi: 10.1017/S003329170800442X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Steinglass JE, Sysko R, Mayer L, Berner LA, Schebendach J, Wang Y, et al. Pre- meal anxiety and food intake in Anorexia Nervosa. Appetite. 2010 doi: 10.1016/j.appet.2010.05.090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Steinglass JE, Sysko R, Glasofer D, Albano AM, Simpson HB, Walsh BT. Rationale for the application of exposure and response prevention to the treatment of anorexia nervosa. International Journal of Eating Disorders. 2011;44:134–41. doi: 10.1002/eat.20784. [DOI] [PMC free article] [PubMed] [Google Scholar]