Abstract
Background
A debilitating anemia associated with low serum iron often accompanies inflammatory bowel disease (IBD). Increased production of the iron regulatory hormone hepcidin is implicated in its pathogenesis and may also contribute to the inflammatory process itself. Hepcidin expression is dependent on bone morphogenetic proteins (BMPs) like BMP6, but the mechanisms that increase hepcidin levels during intestinal inflammation are not clear. Here, we test the hypothesis that inhibiting hepcidin expression may have beneficial effects in IBD, and also shed light on the mechanism of colitis-induced hepcidin up-regulation.
Methods
Mice with T cell transfer colitis were treated with vehicle or one of three anti-BMP reagents – HJV.Fc, a recombinant protein that prevents binding of BMPs to their receptor, LDN-193189, a small molecule inhibitor of BMP signal transduction, and an anti-BMP6 antibody. The effects of these reagents on colitis severity, liver hepcidin mRNA and serum iron were determined. The mechanism of hepcidin up-regulation was investigated by examining BMP6 expression and activity and the effects of IL-6 deficiency.
Results
All the anti-BMP reagents inhibited hepcidin expression and increased serum iron levels in the colitic mice. They also produced modest reductions in colon inflammatory cytokine expression. Although hepcidin up-regulation during colitis was dependent on BMP6, it was not associated with increased BMP6 expression or activity. IL-6 was required for increased hepcidin expression during colitis.
Conclusions
Inhibiting hepcidin expression may help to correct the anemia of IBD and may also attenuate intestinal inflammation. The mechanism of colitis-induced hepcidin up-regulation involves both BMP6 and IL-6.
Keywords: Inflammation, iron, bone morphogenetic protein, hepcidin
INTRODUCTION
Inflammatory bowel disease (IBD) can be complicated by the development of an iron deficiency anemia that is only partly explained by intestinal blood loss. This so-called anemia of chronic disease (ACD) is seen in association with other inflammatory conditions, is often refractory to oral iron supplementation, and may require treatment with parenteral iron or erythropoietin (1). Understanding ACD pathogenesis has been of considerable interest to clinicians and basic researchers, especially since it can have a significant impact on quality of life. Recent elucidation of the mechanisms that regulate iron metabolism have shed light on the condition, and have revealed an important role for hepcidin, an iron regulating hormone secreted by hepatocytes (2,3).
Hepcidin controls the amount of iron entering the circulation by binding and down-regulating ferroportin, a plasma membrane transporter that pumps iron out of phagocytes and duodenal enterocytes, the sites where iron is recycled from aged red blood cells and absorbed from the diet, respectively (2,4). Hepcidin expression is regulated transcriptionally in response to changing serum iron levels. Elevated serum iron promotes hepcidin expression, leading to down-regulation of ferroportin and decreased entry of iron into the circulation. Conversely, low serum iron leads to reduced hepcidin expression, elevated ferroportin and increased movement of iron into the circulation. A key molecule involved in sensing serum iron and regulating hepcidin expression appropriately is HFE, an atypical class I major histocompatibility protein expressed on the hepatocyte surface (5-7). The HFE-hepcidin-ferroportin axis functions as a central mechanism for maintenance of iron homeostasis. Mutations in the HFE gene are associated with the most common inherited iron overload disorder in humans, type I hereditary hemochromatosis (5,8). Recent work has shown that hepcidin transcription depends on functional interactions between signals induced by HFE and those activated by bone morphogenetic proteins (BMPs) such as BMPs 2, 4 and 6 (9-12). The binding of these BMPs to their receptor and the co-receptor hemojuvelin (HJV) expressed on hepatocytes initiates a cascade of events, including the phosphorylation of the receptor SMADs 1, 5 and 8, that culminate in the transcriptional up-regulation of the hepcidin gene. Of the various BMPs, BMP6 appears to be the most functionally relevant regulator of hepcidin in vivo: its expression is modulated by circulating iron levels and its absence in mice leads to marked iron overload (13-15).
In addition to iron status, inflammatory cytokines can also influence transcription of the hepcidin gene. Interleukin-6 (IL-6) has been shown to increase hepcidin expression in vitro and in vivo, and IL-6-induced hepcidin up-regulation has been proposed to play an important role in the pathogenesis of ACD (16-18). The properties of hepcidin are consistent with this role. The decrease in ferroportin expression that results from elevated hepcidin levels would block entry of iron into the circulation, with consequent impairment of erythropoiesis (3,16). Furthermore, since intestinal absorption of iron is inhibited by the hepcidin-mediated down-regulation of ferroportin on enterocytes, the anemia would be resistant to oral iron supplementation. Although the importance of IL-6 in inducing hepcidin expression has been demonstrated in tissue culture experiments and in relatively simple in vivo models of inflammation such as the injection of lipopolysaccharide (LPS) or turpentine (16-18), the mechanisms that up-regulate hepcidin in more clinically relevant situations, including IBD, are yet to be worked out.
We have shown recently that besides acting as a key regulator of iron homeostasis, hepcidin may also contribute to the pathogenesis of inflammatory states. In Hfe knock-out mice, a model of human type I hemochromatosis (19), we found that abnormally low expression of hepcidin was associated with attenuated Salmonella enterocolitis in vivo and reduced LPS-induced production of inflammatory cytokines by peritoneal macrophages in vitro (20,21). The decrease in cytokine production by the mutant macrophages was caused by the low intracellular iron in these cells, which in turn was the result of elevated ferroportin expression secondary to the impaired hepcidin expression in the mice (20). In keeping with these observations, treatment of Hfe-deficient and wild-type macrophages with either hepcidin or ferrous sulfate enhanced their expression of inflammatory cytokines in response to LPS stimulation (21). Based on the data, we proposed that hepcidin might contribute to the development of a positive feedback loop in which inflammatory cytokines induce hepcidin up-regulation, the hepcidin down-regulates ferroportin, and the consequent increase in intracellular iron in macrophages promotes the production of inflammatory cytokines (21,22). We suggested that blocking hepcidin expression could represent a way to interrupt this vicious cycle and thereby correct the dysregulated iron metabolism associated with inflammatory states such as IBD and also have beneficial effects on maladaptive inflammation. We obtained preliminary support for this idea by using broad-spectrum inhibitors of BMPs in the Salmonella enterocolitis and piroxicam/IL-10 knock-out colitis models (21). In the present work, we investigated the effects of these inhibitors, as well as a more selective strategy of BMP6 neutralization, in T cell transfer colitis, which is generally considered to be the mouse model of intestinal inflammation most similar to human IBD (23). We also carried out studies to elucidate the mechanism by which hepcidin is up-regulated during colitis.
MATERIALS AND METHODS
Ethical considerations
All animal experiments were approved by the Sub-committee on Research Animal Care of Massachusetts General Hospital.
Induction of T cell transfer colitis
We used a version of the T cell transfer colitis model based on previously published protocols (23). In brief, naïve CD4+CD25− T cells were purified from the spleens of 6-8 week old wild-type C57BL/6 male mice (Jackson Laboratory, Bar Harbor, ME) using a magnetic sorting-based purification kit as per the manufacturer's directions (Miltenyi Biotec, Auburn, CA). The isolated cells were suspended in PBS and injected intraperitoneally into 6-8 week old, male, lymphocyte-deficient recipient mice (C57BL/6 background), so that each mouse received 1-2 million cells. Depending on availability, we used either RAG1 or RAG2 knock-out mice as recipients, the former being from a breeding colony at Massachusetts General Hospital and the latter from Taconic (Hudson, NY). All recipient mice were of the same genotype in any given experiment. The clinical status and body weight of the animals were monitored over the succeeding 6-8 weeks.
Treatment of mice
Treatment with inhibitors of BMP-dependent hepcidin expression was initiated 6 weeks after transfer of T cells. Three different treatment protocols were used, with all therapeutic reagents being administered intraperitoneally: (a) purified recombinant HJV.Fc fusion protein, prepared as described previously (9,10), 15 mg/kg body weight per dose, 3 doses per week for 2 weeks, (b) the small organic compound LDN-193189 (synthesized at the Vanderbilt Institute of Chemical Biology), a dorsomorphin analog (21,24), 3 mg/kg body weight, 2 doses per day for 1 week, (c) a neutralizing anti-BMP6 antibody (R&D Systems, Minneapolis, MN) (13), 10 mg/kg body weight, 3 doses per week for 2 weeks. Control mice were injected at the same times with an equivalent volume of vehicle (2% 2-hydroxypropyl-β-cyclodextrin in the case of LDN-193189 and PBS in the case of the HJV.Fc and anti-BMP6). The animals were euthanized by carbon dioxide asphyxia at the end of the treatment period.
Analysis of hepcidin and BMP6 expression
At necropsy, a piece of liver was excised and total RNA prepared using Trizol reagent as directed by the manufacturer (Invitrogen, Carlsbad, CA). Quantitative RT-PCR was carried out as previously described (20,21) with primers specific for hepcidin and BMP6. Relative expression was calculated using the 2−ΔΔCt method with normalization to GAPDH. We have published the primer sequences for hepcidin and GAPDH earlier (20,21). The primers used to amplify BMP6 mRNA were 5′ATGGCAGGACTGGATCATTGC3′ and 5′CCATCACAGTAGTTGGCAGCG3′ (25).
Evaluation of colitis
At necropsy, the colon was excised and its length measured. Segments of the proximal, middle and distal colon were processed for hematoxylin/eosin staining and histopathological analysis, and for measurement of cytokine mRNA levels by quantitative RT-PCR, all as previously described (20,21). The colon histopathology was assigned an inflammation score (21) by an observer who was unaware of treatment status. The primers used for amplification of IL-17 transcripts were 5′CCACGTCACCCTGGACTCTC3′ and 5′CTCCGCATTGACACAGCG3′ (26). Relative expression was calculated using the 2−ΔΔCt method with normalization to GAPDH.
Analysis of serum iron concentration
Serum iron concentrations were measured as described previously (10) using a colorimetric assay from Thermo Scientific (West Palm Beach, FL).
Treatment with dextran sulfate sodium (DSS)
Mice were given 2.5% DSS (molecular weight 36,000-50,000, MP Biomedicals, Solon, OH) in drinking water ad libitum and were euthanized 48 hours after start of treatment. In these experiments, the mice were injected with anti-BMP6 or vehicle as described above, with the first dose being given just prior to start of DSS and a second dose 6 hours before euthanasia. In the experiments examining IL-6 expression, the period of DSS treatment was extended to 7 days for some of the mice.
Immunoblotting
Fragments of liver were homogenized in radioimmunoprecipitation assay (RIPA) buffer containing a cocktail of protease and phosphatase inhibitors, separated by polyacrylamide gel electrophoresis and transferred to nitrocellulose membranes, all as described earlier (27). The membranes were blocked and probed with antibodies to phospho-SMAD1/5/8 and total SMAD1 (Cell Signaling Technology, Danvers, MA). After developing the blots with the appropriate fluorescently labeled secondary antibody reagents, they were visualized using the Li-Cor Odyssey infrared imaging system (Li-Cor Biotechnology, Lincoln, NE). The intensities of the phospho-SMAD bands were quantified and normalized to the corresponding total SMAD1 bands.
Statistical analysis
The means and standard deviations of the results from multiple animals are shown. The student's t test was used to determine significance, with a p value of < 0.05 being considered significant.
RESULTS
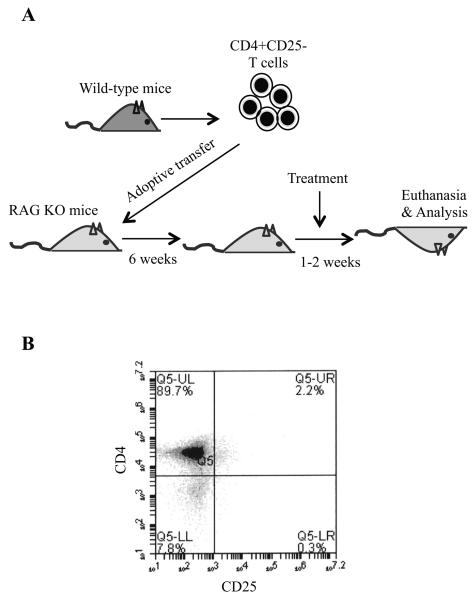
The experimental scheme used in our studies is illustrated in Figure 1A. Using the magnetic sorting protocol, we obtained 80-90% pure CD4+CD25− naïve T cells for injection into RAG-deficient recipients (Figure 1B). Initial experiments revealed that changes in body weight were not a reliable indicator of colitis, so we chose 6 weeks after T cell transfer, when most animals had developed appreciable intestinal inflammation, as the standard time to initiate treatment. None of the treatments used altered body weight, or the gross appearance, histopathology or tissue inflammation score of the colon, so these results will not be presented.
Figure 1.
The T cell transfer colitis model used in the study. A, CD4+CD25− naïve T cells were isolated from wild-type mice and injected into RAG-deficient animals. Six weeks after the T cell transfer, the mice were treated as described in the text and euthanized for analysis. B, Representative flow cytometry profile of purified CD4+CD25− T cells.
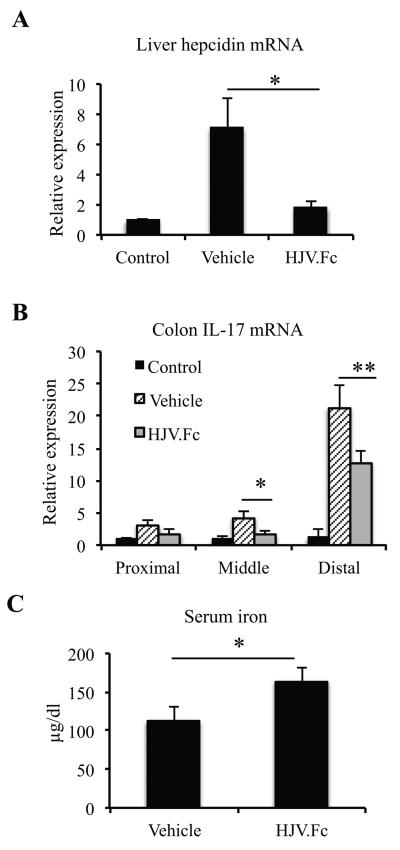
RAG-deficient mice that received naïve T cells and that were treated with vehicle expressed significantly higher levels of hepcidin in the liver than control animals that did not receive T cells (Figure 2A). This up-regulation corresponded to increased colonic levels of the inflammatory cytokines IL-17 (Figure 2B) and IL-6 (not shown), indicative of colitis. Treatment of the colitic mice for 2 weeks with HJV.Fc, a soluble form of the BMP co-receptor HJV that blocks binding of BMPs 2, 4 and 6 to their receptor (9,10), successfully inhibited hepcidin up-regulation (Figure 2A), and also significantly decreased IL-17 mRNA levels in the middle and distal segments of the colon (Figure 2B). The HJV.Fc treatment also significantly elevated serum iron concentrations (Figure 2C).
Figure 2.
Results of HJV.Fc treatment of mice with T cell transfer colitis. A, Liver hepcidin mRNA levels in mice treated with vehicle or HJV.Fc, expressed relative to the mean level in control mice that did not receive T cells. *p = 0.037, n = 3 mice per group. B, Colon IL-17 mRNA levels in the proximal, middle and distal regions of the colon of mice treated with vehicle or HJV.Fc, expressed relative to the mean level in control mice that did not receive T cells. *p = 0.024, **p = 0.035, n = 3 mice per group. C, Serum iron concentrations in mice treated with vehicle or HJV.Fc. *p = 0.02, n = 3 mice per group.
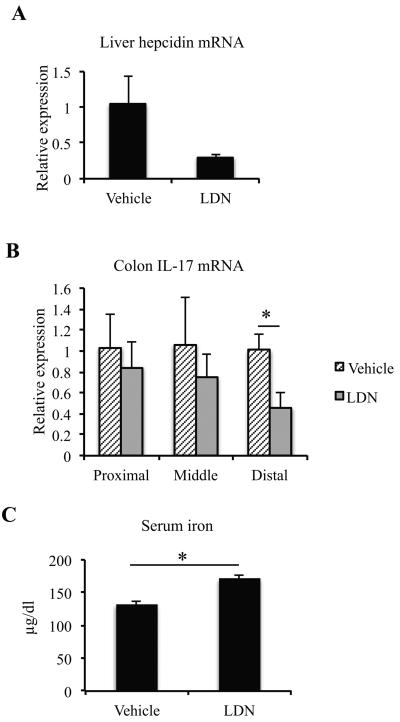
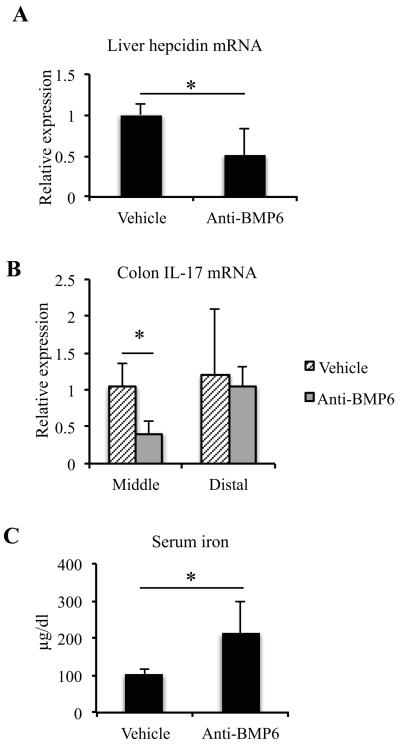
We repeated the experiment with 2 other inhibitors of BMP-induced hepcidin expression – the small organic compound and dorsomorphin analog LDN-193189, which blocks intracellular signaling pathways activated by BMPs (24), and an antibody that specifically neutralizes BMP6. Because of the twice-daily dosing required for LDN-193189, we limited its use to 1 week of treatment, whereas the anti-BMP6 antibody was used for 2 weeks. The results are shown in Figures 3 and 4. Each of the 2 reagents inhibited hepcidin expression in the mice with T cell transfer colitis (Figures 3A and 4A) and increased serum iron concentrations (Figures 3C and 4C). They also had modest and variable effects on the severity of intestinal inflammation, as indicated by decreases in tissue IL-17 mRNA levels (Figures 3B and 4B). Even though these experiments indicated a clear requirement for BMPs, and for BMP6 in particular, for the up-regulation of hepcidin associated with intestinal inflammation, there was no increase in BMP6 expression in the animals with T cell transfer colitis (Figure 5).
Figure 3.
Results of LDN-193189 treatment of mice with T cell transfer colitis. A, Liver hepcidin mRNA levels in mice treated with vehicle or LDN-193189, expressed relative to the mean level in vehicle-treated mice. The p value for the difference between the groups was 0.074, n = 3 mice in the vehicle-treated group, 5 in the LDN-193189 group. B, Colon IL-17 mRNA levels in the proximal, middle and distal regions of the colon of mice treated with vehicle or LDN-19189, expressed relative to the mean level in the vehicle-treated group. *p = 0.006, n = 3 mice in the vehicle-treated group, 5 in the LDN-193189 group. C, Serum iron concentrations in mice treated with vehicle or LDN-193189. *p < 0.0001, n = 3 mice in the vehicle-treated group, 5 in the LDN-193189 group.
Figure 4.
Results of anti-BMP6 treatment of mice with T cell transfer colitis. A, Liver hepcidin mRNA levels in mice treated with vehicle or anti-BMP6, expressed relative to the mean level in vehicle-treated mice. *p = 0.047, n = 4 mice in the vehicle-treated group, 5 in the anti-BMP6 group. B, Colon IL-17 mRNA levels in the middle and distal regions of the colon of mice treated with vehicle or anti-BMP6, expressed relative to the mean level in the vehicle-treated group. *p = 0.021, n = 4 mice in the vehicle-treated group, 5 in the anti-BMP6 group. C, Serum iron concentrations in mice treated with vehicle or anti-BMP6. *p = 0.043, n = 4 mice in the vehicle-treated group, 5 in the anti-BMP6 group.
Figure 5.
Liver BMP6 mRNA levels in mice that did not receive T cells (control) or in mice that received T cells and were treated with vehicle, expressed relative to the mean level in the control group. n = 3 mice per group.
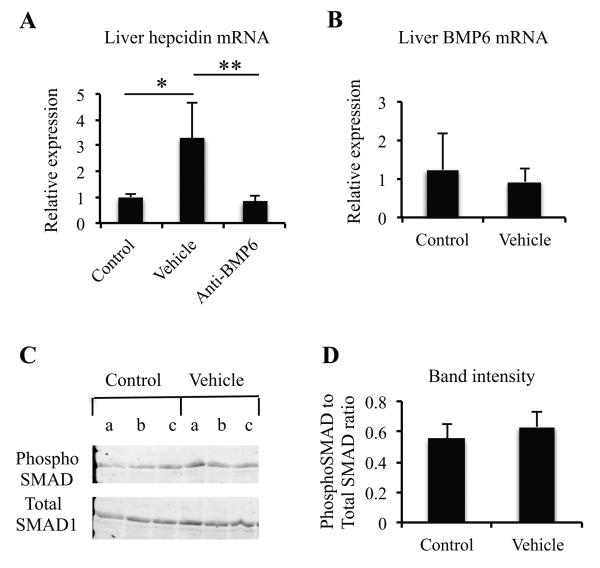
To gain mechanistic insight into the role played by BMP6 in intestinal inflammation-induced hepcidin up-regulation, we turned to the DSS colitis model. We found that hepcidin expression was significantly increased 48 hours after starting DSS, and that the up-regulation was inhibited by treatment with the BMP6 neutralizing antibody (Figure 6A). However, there was no change in BMP6 mRNA levels associated with the DSS-induced hepcidin up-regulation (Figure 6B). BMP2 and BMP4 levels were also not affected by the DSS treatment (data not shown). Furthermore, we could not detect evidence of activation of BMP-dependent signaling in the liver as assayed by immunoblotting with an antibody specific for the phosphorylated forms of SMADs 1, 5 and 8 (Figures 6C and 6D) (28). Thus, the BMP6-dependent increase in hepcidin expression associated with colitis occurred without overt indications of an increase in BMP6 expression or activity.
Figure 6.
Hepcidin and BMP6 in DSS colitis. A, Liver hepcidin mRNA levels in mice treated with vehicle or anti-BMP6, expressed relative to the mean level in control mice that did not receive DSS. *p = 0.02, **p = 0.015, n = 4 mice in the control group, 5 in the vehicle-treated group and 3 in the anti-BMP6 group. B, Liver BMP6 mRNA levels in mice that did not receive DSS (control) or in mice that received DSS and were treated with vehicle, expressed relative to the mean level in the control group. n = 4 mice in the control group, 5 in the vehicle-treated group. C, Results of anti-phospho-SMAD1/5/8 and anti-SMAD1 immunoblotting of liver homogenates from mice that did not receive DSS (control) or vehicle-treated mice that received DSS. Each lane corresponds to an individual mouse. D, Quantitation of band intensities. The intensities of the phospho-SMAD1/5/8 and total SMAD1 bands from the blot in C were quantified and expressed as a ratio (3 mice per group).
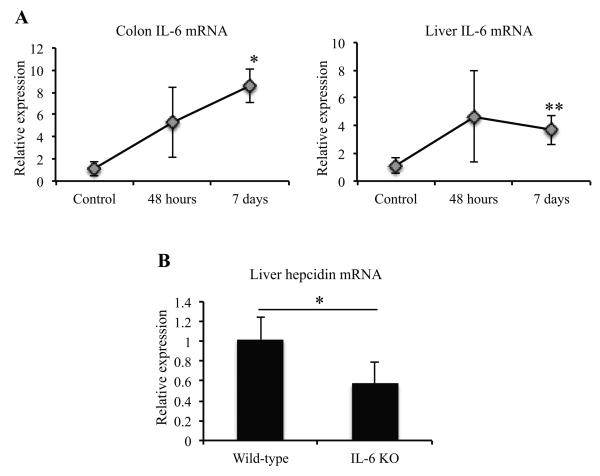
Since IL-6 has been implicated in up-regulation of hepcidin in LPS- and turpentine-induced models of inflammation (16-18), we examined expression of this cytokine in the colon and liver and found an increase in both tissues by 48 hours after starting DSS, and a more significant elevation at the end of 1 week (Figure 7A). Consistent with the functional importance of this observation, the DSS-induced increase in hepcidin expression was significantly reduced in IL-6 knock-out animals (Figure 7B). Our results suggest that IL-6 is an important inducer of hepcidin up-regulation in the context of intestinal inflammation.
Figure 7.
The role of IL-6 in hepcidin up-regulation during DSS colitis. A, IL-6 mRNA levels in the colon and liver following DSS treatment for 48 hours or 7 days, expressed relative to the mean level in control mice that did not receive DSS. *p = 0.006, **p = 0.031, n = 3 mice per group. B, Liver hepcidin mRNA levels in wild-type and IL-6 knock-out (KO) mice 48 hours after starting DSS, expressed relative to the mean level in the wild-type. *p = 0.019, n = 4 wild-type mice, 6 IL-6 knock-out mice.
DISCUSSION
The results reported here make several important points relevant to the pathogenesis and treatment of IBD, especially in relation to the dysregulated iron metabolism and ACD that is often associated with this condition (1). Firstly, they demonstrate that intestinal inflammation in T cell transfer colitis and in DSS-induced colitis is associated with a significant increase in hepcidin expression in the liver. This finding is consistent with earlier work from our laboratory, which showed a similar up-regulation of hepcidin in piroxicam/IL-10 knock-out colitis, as well as in Salmonella-induced enterocolitis (21). Thus, multiple forms of intestinal inflammation, including that occurring in 3 different mouse models of IBD, lead to the induction of hepcidin expression. Hepcidin up-regulation has also been observed in at least some, although not all, studies of human IBD. Semrin et al found in an analysis of pediatric Crohn's disease that urinary hepcidin levels were elevated in individuals with active inflammation (29). In contrast, a study of adult patients with ulcerative colitis or Crohn's disease found decreased serum levels of hepcidin (30). The variable results suggest that hepcidin up-regulation in human IBD is likely to be influenced by factors such as age, type of disease and disease activity, and that further investigation of these issues is required.
Our findings also indicate that elevated hepcidin contributes to 2 aspects of the disease process in T cell transfer colitis, viz., the dysregulated iron metabolism and the inflammation. Blocking hepcidin expression with 3 different inhibitors led in all cases to a significant elevation of serum iron levels, confirming and extending similar observations that we made earlier in the Salmonella enterocolitis and piroxicam/IL-10 knock-out colitis models (21). This outcome fits with the known role of hepcidin as an inhibitor of ferroportin-mediated iron export from phagocytes and enterocytes (2-4), and is in keeping with results from one study of human IBD that showed that patients with active Crohn's disease had impaired oral absorption of iron (29). Taken together, the data suggest that elevated hepcidin is likely to be a significant factor in the pathogenesis of ACD in IBD. Blocking hepcidin expression also attenuated the severity of intestinal inflammation in our experiments, at least to the extent of reducing tissue inflammatory cytokine expression. The effect on inflammation was not as pronounced as in our earlier work with the Salmonella enterocolitis and piroxicam/IL-10 knock-out colitis models (21). The difference may reflect the fact that those models are driven mainly by innate immune mechanisms, whereas T cell transfer colitis is mediated by adaptive immunity (23,31-33). This issue could be especially relevant since the effects of hepcidin on the immune response appear to be mediated mainly by macrophages (21). Another factor that could contribute to the variable effects of inhibiting hepcidin expression on inflammation is the recent observation that hepcidin may down-regulate inflammatory cytokine production under some circumstances. Studies by De Domenico et al showed that the binding of hepcidin to ferroportin can activate a signaling cascade, involving the Jak2 kinase and the STAT3 transcription factor, which suppresses LPS-induced expression of a number of cytokines (34). Thus, the hepcidin-ferroportin interaction may influence macrophage cytokine expression negatively via Jak2/STAT3 signaling, as shown by the experiments of De Domenico et al, or positively via an increase in intracellular iron, as indicated by our studies, and the net outcome of blocking hepcidin expression on the inflammatory response may depend on which of these effects predominates.
In addition to demonstrating the important role played by hepcidin in colitis, our experiments have provided insight into the mechanisms that induce hepcidin during intestinal inflammation. The results indicate that of the several BMPs that have been implicated as regulators of hepcidin expression (9,10,13), BMP6 clearly plays an essential role in the context of the colitis models used here since neutralization of this molecule alone significantly reduced hepcidin levels. Interestingly, intestinal inflammation was not associated with increases in liver BMP6 mRNA levels or BMP6-dependent signaling activity in our studies. These results suggest that even though BMP6 was required for normal expression of hepcidin, the actual stimulus for colitis-induced hepcidin up-regulation involved another factor. Our findings point to increased production of IL-6 by the liver and other tissues during colitis as being one such factor. The data suggest a mechanism in which signals activated by increased IL-6 expression interact with constitutive signals provided by basal levels of BMP6 to promote hepcidin transcription. The combination of the 2 sets of signals determines the amount of hepcidin expressed and blocking either leads to lowering of hepcidin production. This explanation is consistent with earlier observations showing that an intact BMP-SMAD pathway is required for IL-6-induced hepcidin up-regulation and that signals activated by BMPs and IL-6 probably interact at the level of the hepcidin promoter (10,24,35,36). Moreover, BMP6-deficient mice have abnormally low basal hepcidin production, and although they up-regulate expression following LPS exposure, the final level achieved is significantly lower than wild-type animals (14). On the other hand, IL-6 knock-out mice have normal basal hepcidin levels but fail to up-regulate expression following LPS stimulation (16).
The data presented here, along with our earlier findings (21), demonstrate that lowering abnormally elevated levels of hepcidin has a beneficial effect on serum iron in multiple models of colitis, probably as a result of increased ferroportin-mediated release of iron into the circulation. Thus, inhibiting hepcidin expression or function in inflammatory conditions such as IBD is likely to be helpful in correcting the associated anemia by facilitating the absorption and recycling of iron. This approach could represent a novel therapeutic strategy for the ACD associated with chronic inflammation, one that our results suggest may have the added benefit of helping to attenuate the inflammatory process itself. Treatment of ACD based on hepcidin modulation could be especially relevant to IBD since the oral administration of iron in this condition may exacerbate the intestinal inflammation (1,37-41). Further investigation of these ideas is clearly indicated.
ACKNOWLEDGMENTS
We are grateful to the Chemical Synthesis Core, Vanderbilt Institute of Chemical Biology for synthesizing the LDN-193189, and to Dr. Hai Ning Shi, Massachusetts General Hospital, for advice on some of the experiments.
Sources of support: This work was supported by grants from the Broad Medical Research Program (IBD-0253) and the National Institutes of Health (R56 AI089700) to BJC, and by an unrestricted educational grant from Wyeth Nutrition to LW.
Footnotes
CONFLICT OF INTEREST
HYL and JLB have ownership interest in Ferrumax Pharmaceuticals, which has licensed technology from Massachusetts General Hospital based on their work. A patent application entitled “Methods and Composition to Regulate Iron Metabolism” has been submitted by Massachusetts General Hospital.
REFERENCES
- 1.Stein J, Hartmann F, Dignass AU. Diagnosis and management of iron deficiency anemia in patients with IBD. Nat Rev Gastroenterol Hepatol. 2010;7:599–610. doi: 10.1038/nrgastro.2010.151. [DOI] [PubMed] [Google Scholar]
- 2.Hentze MW, Muckenthaler MU, Galy B, et al. Two to tango: regulation of mammalian iron metabolism. Cell. 2010;142:24–38. doi: 10.1016/j.cell.2010.06.028. [DOI] [PubMed] [Google Scholar]
- 3.Ganz T, Nemeth E. Iron sequestration and anemia of inflammation. Semin Hematol. 2009;46:387–393. doi: 10.1053/j.seminhematol.2009.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nemeth E, Tuttle MS, Powelson J, et al. Hepcidin regulates cellular iron efflux by binding to ferroportin and inducing its internalization. Science. 2004;306:2090–2093. doi: 10.1126/science.1104742. [DOI] [PubMed] [Google Scholar]
- 5.Feder JN, Gnirke A, Thomas W, et al. A novel MHC class I-like gene is mutated in patients with hereditary haemochromatosis. Nat Genet. 1996;13:399–408. doi: 10.1038/ng0896-399. [DOI] [PubMed] [Google Scholar]
- 6.Schmidt PJ, Toran PT, Giannetti AM, et al. The transferrin receptor modulates Hfe-dependent regulation of hepcidin expression. Cell Metab. 2008;7:205–214. doi: 10.1016/j.cmet.2007.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gao J, Chen J, Kramer M, et al. Interaction of the hereditary hemochromatosis protein HFE with transferrin receptor 2 is required for transferrin-induced hepcidin expression. Cell Metab. 2009;9:217–227. doi: 10.1016/j.cmet.2009.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pietrangelo A. Hereditary hemochromatosis: pathogenesis, diagnosis and treatment. Gastroenterology. 2010;139:393–408. doi: 10.1053/j.gastro.2010.06.013. [DOI] [PubMed] [Google Scholar]
- 9.Babitt JL, Huang FW, Wrighting DM, et al. Bone morphogenetic protein signaling by hemojuvelin regulates hepcidin expression. Nat Genet. 2006;38:531–539. doi: 10.1038/ng1777. [DOI] [PubMed] [Google Scholar]
- 10.Babitt JL, Huang FW, Xia Y, et al. Modulation of bone morphogenetic protein signaling in vivo regulates systemic iron balance. J Clin Invest. 2007;117:1933–1939. doi: 10.1172/JCI31342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Corradini E, Garuti C, Montosi G, et al. Bone morphogenetic protein signaling is impaired in an HFE knock-out mouse model of hemochromatosis. Gastroenterology. 2009;137:1489–1497. doi: 10.1053/j.gastro.2009.06.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ryan JD, Ryan E, Fabre A, et al. Defective bone morphogenetic protein signaling underlies hepcidin deficiency in HFE hereditary hemochromatosis. Hepatology. 2010;52:1266–1273. doi: 10.1002/hep.23814. [DOI] [PubMed] [Google Scholar]
- 13.Andriopoulos B, Jr, Corradini E, Xia Y, et al. BMP6 is a key endogenous regulator of hepcidin expression and iron metabolism. Nat Genet. 2009;41:482–487. doi: 10.1038/ng.335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Meynard D, Kautz L, Darnaud V, et al. Lack of the bone morphogenetic protein BMP6 induces massive iron overload. Nat Genet. 2009;41:478–481. doi: 10.1038/ng.320. [DOI] [PubMed] [Google Scholar]
- 15.Corradini E, Schmidt PJ, Meynard D, et al. BMP6 treatment compensates for the molecular defect and ameliorates hemochromatosis in Hfe knock-out mice. Gastroenterology. 2010;139:1721–1729. doi: 10.1053/j.gastro.2010.07.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nemeth E, Rivera S, Gabayan V, et al. IL-6 mediates hypoferremia of inflammation by inducing synthesis of the iron regulatory hormone hepcidin. J Clin Invest. 2004;113:1271–1276. doi: 10.1172/JCI20945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee P, Peng H, Gelbart T, et al. Regulation of hepcidin transcription by interleukin-1 and interleukin-6. Proc Natl Acad Sci USA. 2005;102:1906–1910. doi: 10.1073/pnas.0409808102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wrighting DM, Andrews NC. Interleukin-6 induces hepcidin expression through STAT3. Blood. 2006;108:3204–3209. doi: 10.1182/blood-2006-06-027631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhou XY, Tomatsu S, Flemin RE, et al. HFE gene knock-out produces a mouse model of hereditary hemochromatosis. Proc Natl Acad Sci USA. 1998;95:2492–2497. doi: 10.1073/pnas.95.5.2492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang L, Johnson EE, Shi HN, et al. Attenuated inflammatory responses in hemachromatosis reveal a role for iron in the regulation of macrophage cytokine translation. J Immunol. 2008;181:2723–2731. doi: 10.4049/jimmunol.181.4.2723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang L, Harrington L, Trebicka E, et al. Selective modulation of TLR4-activated inflammatory responses by altered iron homeostasis. J Clin Invest. 2009;119:3322–3328. doi: 10.1172/JCI39939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cherayil BJ. Cross-talk between iron homeostasis and intestinal inflammation. Gut Microbes. 2010;1:65–69. doi: 10.4161/gmic.1.1.10863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ostanin DV, Bao J, Koboziev I, et al. T cell transfer model of chronic colitis: concepts, considerations, and tricks of the trade. Am J Physiol Gastrointest Liver Physiol. 2009;296:G135–G146. doi: 10.1152/ajpgi.90462.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yu PB, Hong CC, Sachidanandan C, et al. Dorsomorphin inhibits BMP signals required for embryogenesis and iron metabolism. Nat Chem Biol. 2008;4:33–41. doi: 10.1038/nchembio.2007.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kautz L, Meynard D, Monnier A, et al. Iron regulates phosphorylation of Smad1/5/8 and gene expression of BMP6, Smad7, Id1 and Atoh8 in the mouse liver. Blood. 2008;112:1503–1509. doi: 10.1182/blood-2008-03-143354. [DOI] [PubMed] [Google Scholar]
- 26.Khader SA, Pearl JE, Sakamoto K, et al. IL-23 compensates for the absence of IL-12p70 and is essential for the IL-17 response during tuberculosis but is dispensable for protection and antigen-specific IFN-gamma responses if IL-12p70 is available. J Immunol. 2005;175:788–795. doi: 10.4049/jimmunol.175.2.788. [DOI] [PubMed] [Google Scholar]
- 27.Li Q, Cherayil BJ. Role of Toll-like receptor 4 in macrophage activation and tolerance during Salmonella enterica serovar Typhimurium infection. Infect Immun. 2003;71:4873–4882. doi: 10.1128/IAI.71.9.4873-4882.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Miyazono K, Kamiya Y, Morikawa M. Bone morphogenetic protein receptors and signal transduction. J Biochem. 2010;147:35–51. doi: 10.1093/jb/mvp148. [DOI] [PubMed] [Google Scholar]
- 29.Semrin G, Fishman DS, Bousvaros A, et al. Impaired intestinal iron absorption in Crohn's disease correlates with disease activity and markers of inflammation. Inflamm Bowel Dis. 2006;12:1101–1106. doi: 10.1097/01.mib.0000235097.86360.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Arnold J, Sangwaiya A, Bhatkal B, et al. Hepcidin and inflammatory bowel disease: dual role in host defence and iron homeostasis. Eur J Gastroenterol Hepatol. 2009;21:335–339. doi: 10.1097/MEG.0b013e32830e2885. [DOI] [PubMed] [Google Scholar]
- 31.Hapfelmeier S, Hardt WD. A mouse model for S. typhimurium-induced enterocolitis. Trends Microbiol. 2005;13:497–503. doi: 10.1016/j.tim.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 32.Berg DJ, Zhang J, Weinstock JV, et al. Rapid development of colitis in NSAID-treated IL-10-deficient mice. Gastroenterology. 2002;123:1527–1542. doi: 10.1053/gast.2002.1231527. [DOI] [PubMed] [Google Scholar]
- 33.Hale LP, Gottfried MR, Swidsinski A. Piroxicam treatment of IL-10-deficient mice enhances colonic epithelial apoptosis and mucosal exposure to intestinal bacteria. Inflamm Bowel Dis. 2005;11:1060–1069. doi: 10.1097/01.mib.0000187582.90423.bc. [DOI] [PubMed] [Google Scholar]
- 34.De Domenico I, Zhang TY, Koening CL, et al. Hepcidin mediates transcriptional changes that modulate acute cytokine-induced inflammatory responses in mice. J Clin Invest. 2010;120:2395–2405. doi: 10.1172/JCI42011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wang RH, Li C, Xu X, et al. A role of SMAD4 in iron metabolism through the positive regulation of hepcidin expression. Cell Metab. 2005;2:399–409. doi: 10.1016/j.cmet.2005.10.010. [DOI] [PubMed] [Google Scholar]
- 36.Verga Falzacappa MV, Casanovas G, Hentze MW, et al. A bone morphogenetic protein (BMP)-responsive element in the hepcidin promoter controls HFE2-mediated hepatic hepcidin expression and its response to IL-6 in cultured cells. J Mol Med. 2008;86:531–540. doi: 10.1007/s00109-008-0313-7. [DOI] [PubMed] [Google Scholar]
- 37.Oldenburg B, van Berge Henegouwen GP, Rennick D, et al. Iron supplementation affects the production of pro-inflammatory cytokines in IL-10-deficient mice. Eur J Clin Invest. 2000;30:505–510. doi: 10.1046/j.1365-2362.2000.00650.x. [DOI] [PubMed] [Google Scholar]
- 38.Carrier J, Aghdassi E, Cullen J, et al. Iron supplementation increases disease activity and vitamin E ameliorates the effect in rats with dextran sulfate sodium-induced colitis. J Nutr. 2002;132:3146–3150. doi: 10.1093/jn/131.10.3146. [DOI] [PubMed] [Google Scholar]
- 39.Erichsen K, Hausken T, Ulvik RJ, et al. Ferrous fumarate deteriorated plasma antioxidant status in patients with Crohn's disease. Scand J Gastroenterol. 2003;38:543–548. doi: 10.1080/00365520310000771. [DOI] [PubMed] [Google Scholar]
- 40.Uritski R, Barshack I, Bilkis I, et al. Dietary iron affects inflammatory status in a rat model of colitis. J Nutr. 2004;134:2251–2255. doi: 10.1093/jn/134.9.2251. [DOI] [PubMed] [Google Scholar]
- 41.Seril DN, Liao J, West AB, et al. High-iron diet: foe or feat in ulcerative colitis and ulcerative colitis-associated carcinogenesis. J Clin Gastroenterol. 2006;40:391–397. doi: 10.1097/00004836-200605000-00006. [DOI] [PubMed] [Google Scholar]