Abstract
Objectives. Metformin is the preferred oral antidiabetic agent for type 2 diabetes. Lactic acidosis is described as a rare complication, usually during an acute kidney injury (AKI). Material and Methods. We conducted a prospective observational study of metformin-associated AKI cases during four years. 29 cases were identified. Previous renal function, clinical data, and outcomes were recorded. Results. An episode of acute gastroenteritis precipitated the event in 26 cases. Three developed a septic shock. Three patients died, the only related factor being liver dysfunction. More severe metabolic acidosis hyperkalemia and anemia were associated with higher probabilities of RRT requirement. We could not find any relationship between previous renal dysfunction and the outcome of the AKI. Conclusions. AKI associated to an episode of volume depletion due to gastrointestinal losses is a serious complication in type 2 diabetic patients on metformin. Previous renal dysfunction (mild-to-moderate CKD) has no influence on the severity or outcome.
1. Introduction
Metformin is the only biguanide extensively used these days, and has become the first-line oral drug in type 2 diabetes [1]. Metformin-associated lactic acidosis has not been thoroughly characterized. Meta-analyses and large studies have been unable to establish an epidemiological association, probably due to its low incidence rate. However, most cases have been reported associated with an episode of acute kidney injury (AKI), predominantly in intensive care units [2–4]. Usual treatment includes correction of acidosis and hyperkalemia using bicarbonate solutions, as well as renal replacement therapies (RRT) [5].
Some coexisting conditions have been classically defined as contraindications for the use of metformin [6]. The reason for including chronic kidney disease (CKD) probably arises from the fact that most cases of lactic acidosis were described in association with an AKI episode derived from hypovolemia secondary to gastrointestinal losses. Experimental studies and several series of cases show that adverse outcomes seem more related to hepatic dysfunction than to renal impairment [2, 3, 7]. The pharmacological effect of metformin, as well as the onset of lactic acidosis, could be mediated in part through a self-limiting inhibition of the respiratory chain that restrains hepatic gluconeogenesis while increasing glucose utilization in peripheral tissues [8, 9].
This study describes the features of the AKI related to metformin use to determine the prognostic influence of previous CKD, in an attempt to find if there is real evidence to further consider renal impairment as a contraindication for metformin prescription.
2. Material and Methods
2.1. Study Design
The study was developed at the Hospital General Universitario Gregorio Marañón, in Madrid, between 2006 and 2010. We recorded all patients with AKI meeting RIFLE criteria for renal injury or failure. Patients were included whenever they followed daily treatment with metformin and had biochemical data of metabolic acidosis.
Clinical data were collected. Renal function was evaluated (before—at least three months earlier and while in a healthy state—, baseline and during followup). Serum creatinine and estimated glomerular filtration rate (eGFR) as calculated with the MDRD-4-IMDS equation were recorded. Patients were stratified according to the NKF-KDOQI criteria for CKD stages according to their previous serum creatinine: normal eGFR (over 60 mL/min/1.73 m2) and CKD (below 60), and those with CKD in stages 3a (eGFR between 45 and 59 mL/min) and 3b (between 30 and 44).
2.2. Objectives
Our primary goal was to evaluate RRT requirements in a crude, unadjusted analysis, stratified by previous renal function. Secondary endpoints included renal function at hospital discharge and three months later, and all-cause mortality.
2.3. Statistical Analysis
All statistical analyses were performed with SPSS, version 15.0.1 (SPSS Inc, Chicago, IL). Categorical data were compared using the Chi-square test, and continuous variables by means of a Student's t-test. Association between basal characteristics and potential prognostic factors was assessed in univariate analyses. Statistical significance was defined as a two-tailed P < 0.05.
3. Results
Twenty-nine patients were included, thirteen men and sixteen women, with a mean age of 72.00 ± 8.78 years (Table 1). The daily metformin dose was 1700 to 2550 mg. Baseline mean serum creatinine concentration was 105.20 ± 29.17 μmol/L: seventeen patients (59%) had baseline stage 3 CKD (28% stage 3a and 31% stage 3b). Twenty-six patients were admitted into the emergency unit with volume depletion in the context of gastrointestinal losses, most of them 24 to 72 hours after the beginning of the symptoms. The remaining three had a septic shock. The mean laboratory values at the time of admission are summarized in Table 1.
Table 1.
Clinical and analytical characteristics of the patients.
| Patients classified according to renal function | ||||
|---|---|---|---|---|
| All patients n = 29 |
eGFR > 60 mL/min* n = 12 |
eGFR < 60 mL/min* n = 17 |
P† | |
| Age Gender (M/F) (%) |
72 ± 8.78 44.8/55.2 |
70.33 ± 5.74 50/50 |
73.18 ± 10.42 41.2/58.8 |
0.40 0.64 |
| Coexisting conditions (%): | ||||
| (i) Hypertension | 100 | 100 | 100 | — |
| (ii) Chronic heart disease | 38 | 25 | 53 | 0.13 |
| (iii) Cerebrovascular disease | 31 | 25 | 35 | 0.56 |
| (iv) Cancer | 24 | 33 | 18 | 0.33 |
| (v) Liver disease | 10 | 8 | 12 | 0.77 |
| (vi) Peripheral vasculopathy | 10 | 0 | 18 | 0.12 |
| (vii) Chronic respiratory disease | 3 | 8 | 0 | 0.23 |
| Other treatments (%): Antihypertensive drugs: ‡ |
||||
| (i) RAAS blockers | 86 | 91.7 | 82.4 | 0.47 |
| (a) of which ACE inhibitors | 59 | |||
| (b) of which ARB | 24 | |||
| (c) of which dual block | 3 | |||
| (ii) Diuretics | 55 | 50 | 58.8 | 0.64 |
| Other antidiabetic agents: | ||||
| (i) Other oral antidiabetic drugs | 41 | 33.3 | 47.1 | 0.46 |
| (ii) Insulin | 21 | 33.3 | 17.6 | 0.33 |
| Laboratory values at diagnosis: | ||||
| (i) Creatinine (μmol/L) | 599.35 ± 299.68 | 675.38 ± 302.33 | 544.55 ± 295.26 | 0.25 |
| (ii) eGFR (mL/min/1.73 m2) | 10.47 ± 7.94 | 8.73 ± 6.98 | 11.69 ± 8.55 | 0.33 |
| (iii) Urea (mmol/L) | 58.01 ± 20.75 | 58.52 ± 24.73 | 57.65 ± 18.23 | 0.91 |
| (iv) pH | 7.12 ± 0.19 | 7.12 ± 0.18 | 7.12 ± 0.20 | 0.96 |
| (v) Lactate (mmol/L) | 9.05 ± 4.99 | 8.92 ± 5.02 | 9.07 ± 5.16 | 0.94 |
| (vi) Bicarbonate (mmol/L) | 11.14 ± 7.23 | 10.84 ± 7.51 | 11.35 ± 7.25 | 0.86 |
| (vii) Anion gap | 29.03 ± 10.23 | 28.58 ± 12.51 | 28.94 ± 9.62 | 0.93 |
| (viii) Sodium (mmol/L) | 134.17 ± 7.09 | 135.42 ± 5.25 | 133.29 ± 8.20 | 0.44 |
| (ix) Chloride (mmol/L) | 94.24 ± 8.64 | 96 ± 7.82 | 93 ± 9.20 | 0.37 |
| (x) Potassium (mmol/L) | 5.65 ± 1.36 | 6.01 ± 1.09 | 5.40 ± 1.50 | 0.24 |
| (xi) Phosphate (mmol/L) | 2.48 ± 1.40 | 2.63 ± 1.89 | 2.37 ± 0.92 | 0.63 |
| (xii) Hemoglobin (g/L) | 117.7 ± 22.4 | 111.4 ± 17.1 | 122.1 ± 25.0 | 0.21 |
| (xiii) Total serum proteins (g/L) | 66.9 ± 12.4 | 68.3 ± 10.9 | 66.0 ± 13.5 | 0.64 |
| (xiv) Albumin (g/L) | 32.8 ± 5.1 | 32.9 ± 5.3 | 32.8 ± 5.2 | 0.96 |
| Blood pressure at diagnosis (mm Hg): | ||||
| (i) Systolic | 119.31 ± 37.31 | 121.33 ± 42.84 | 117.88 ± 34.20 | 0.81 |
| (ii) Diastolic | 63.00 ± 19.50 | 62.09 ± 21.17 | 63.59 ± 18.98 | 0.85 |
| (iii) Mean | 81.41 ± 24.41 | 80.97 ± 28.44 | 81.69 ± 22.36 | 0.94 |
| Endpoints: | ||||
| (i) RRT requirement (%) | 30 | 91.7 | 47.1 | 0.013 |
| (ii) Creatinine at discharge (μmol/L) | 138.79 ± 42.43 | 123.76 ± 28.29 | 150.28 ± 48.62 | 0.09 |
| (iii) eGFR at discharge (mL/min/1.73 m2)* | 42.72 ± 12.60 | 46.50 ± 13.03 | 39.95 ± 11.95 | 0.20 |
| (iv) Creatinine 3 months after discharge (μmol/L) | 106.96 ± 38.01 | 99.01 ± 32.71 | 111.38 ± 40.66 | 0.47 |
| (v) eGFR 3 months after discharge (mL/min/1.732)* | 63.82 ± 28.60 | 65.59 ± 22.43 | 62.73 ± 32.65 | 0.83 |
Mean ± standard deviation for quantitative variables; percentages for qualitative variables. *Estimated glomerular filtration rate (eGFR) calculated according to the MDRD-4-IMDS equation. †Significant P values between groups highlighted in bold. ‡RAAS: renin-angiotensin-aldosterone system; ACE: angiotensin-converting enzyme; ARB: aldosterone-receptor blockers.
Nine patients (30%) were treated with intravenous fluids, including administration of bicarbonate, and medical management of hyperkalemia. The other twenty also required RRT: eleven (55%) with continuous techniques and nine with intermittent hemodialysis. Fifteen patients (51.7%) required ICU admission.
Patients with lower plasma pH, higher level of potassium, lower serum proteins, and lower hemoglobin concentration had a higher probability of requiring RRT (Table 2). We detected no cases of lactic acidosis related to long-term metformin use without a concomitant AKI. Previous renal dysfunction had no influence on the outcome: a worse chronic kidney disease stage did not imply a higher risk of needing dialysis. In fact, 91.7% of the patients with a previous eGFR over 60 mL/min/1.73 m2 needed RRT, yet only 47.1% of the patients with CKD did (P = 0.013). This significant difference could also be seen in the subgroups analysis (Figure 1).
Table 2.
Prognostic factors for renal replacement therapy requirement.
| RRT required | RRT not required | P* | |
|---|---|---|---|
| Hemoglobin (g/L) | 109.9 ± 16.8 | 134.7 ± 24.6 | 0.002 |
| Potassium (mmol/L) | 6.03 ± 1.11 | 4.81 ± 1.55 | 0.015 |
| pH | 7.06 ± 0.19 | 7.24 ± 0.09 | 0.023 |
| Serum proteins (g/L) | 63.3 ± 12.2 | 73.2 ± 10.5 | 0.041 |
| Creatinine (μmol/L) | 666.54 ± 309.40 | 449.07 ± 221.88 | 0.07 |
| Bicarbonate (mmol/L) | 9.51 ± 6.98 | 14.56 ± 6.35 | 0.08 |
| Lactate (mmol/L) | 9.54 ± 5.29 | 7.97 ± 4.32 | 0.44 |
| Anion gap | 29.75 ± 11.21 | 27.44 ± 7.99 | 0.59 |
| Systolic blood pressure (mmHg) | 121.26 ± 43.30 | 115.60 ± 23.65 | 0.71 |
| Diastolic blood pressure (mmHg) | 63.37 ± 20.32 | 62.22 ± 18.77 | 0.89 |
| Mean blood pressure (mmHg) | 82.67 ± 27.35 | 78.74 ± 17.82 | 0.70 |
*Significant P values between groups highlighted in bold.
Figure 1.
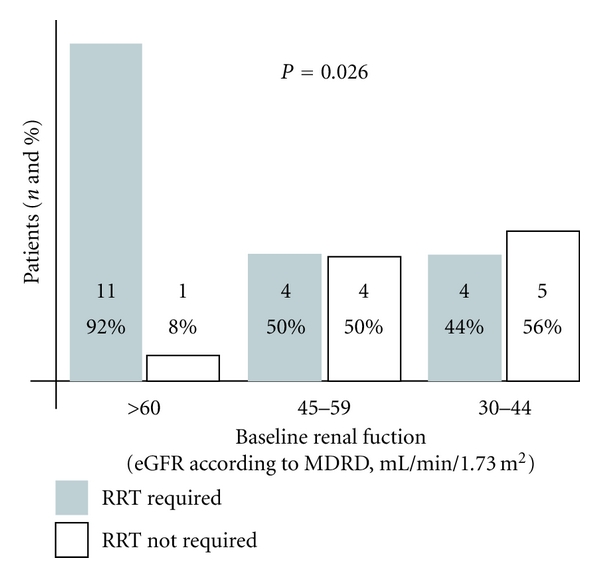
Influence of previous renal function on renal replacement therapy requirement during the acute kidney injury episode. Number and percentage of patients that required renal replacement therapies in relation with previous renal function. ∗Previous renal function expressed as estimated glomerular filtration rate in mL/min/1.73 m2 calculated according to the MDRD-4-IMDS formula.
Three patients died: one, secondarily to refractory septic shock, and two cirrhotic patients developed concomitant liver failure. The average in-hospital length of stay was 15.66 ± 11.02 days. Renal function prognosis was good: the mean creatinine at hospital discharge was 138.79 ± 42.43 μmol/L. Three months after discharge, the mean creatinine was 106.96 ± 38.01 μmol/L.
4. Discussion
In our study, mild-to-moderate CKD is not associated with the risk of developing the AKI episode. CKD is neither associated with a more severe acidosis nor does it imply a higher morbimortality. In contrast, in our study, the group of patients with moderate CKD has lower RRT requirements, as a proof of a less severe episode. This fact cannot be explained by means of a more profound hypotension or a higher rate of SRAA blockers use. Because of that, we consider it safe that this group of patients could continue with metformin treatment.
Volume depletion and hypoperfusion appear more important in the severity of metformin-related metabolic acidosis when associated with an AKI. Thus, patients undergoing any risk situation for volume depletion would benefit from a temporary interruption in their metformin treatment. This is a regular practice for radiological studies with iodated contrasts, as part of nephrotoxicity prophylaxis. It could also become a good practice for primary care physicians to advice patients on metformin to temporarily interrupt this treatment whenever they develop any other potential danger, particularly diarrhea or vomiting. We believe that this simple practice would lower the rate of this complication of metformin.
Previous renal dysfunction has been described as a potential risk factor of metformin-associated lactic acidosis and most guidelines support CKD as a contraindication. While CKD stages 4-5 (eGFR below 30) are accepted as an absolute contraindication, the information about moderate CKD (eGFR between 30 and 59) is more controversial [10]. It is established as an absolute contraindication in the technical information of the drug, but other guidelines of scientific societies, such as the American Diabetes Association, permit its use in patients with an eGFR > 30 mL/min [1].
Recent studies point out liver disease as more important risk and prognostic factors. Peters et al. [4] and Seidowsky et al. [3] find prothrombin time and prothrombin activity respectively as the only analytical factors related to a higher mortality. Furthermore, experimental studies highlight the importance of the biochemical pathways affected by this drug, mainly glycolysis activation and inhibition of gluconeogenesis and mitochondrial respiratory chain complex 1, both in liver cells [7–9]. The fact that two of our three deaths were due to hepatic failure supports this idea.
4.1. Study Limitations
In spite of being one of the largest series describing metformin-related AKI, our sample is still comprised of a low number of patients. A larger series could give more data on mortality predictive factors. Also, a controlled study comparing the outcomes of medical treatment versus RRT would shed light on the best therapeutic approach.
5. Conclusion
In our study, stage 3 chronic kidney disease is not associated with a higher risk for dialysis-dependent acute kidney injury in patients who develop lactic acidosis while taking metformin, and it seems not to influence prognosis. Thus, metformin appears to be safe in this group of patients.
Acknowledgments
The authors wish to thank all the staff members and nurses of the nephrology department at their Institution for their invaluable contribution to the publication of this paper as a result of their outstanding daily bedside work. Part of this paper was presented at the 40th congress of the Spanish Society of Nephrology. The authors declare no competing interests.
References
- 1.Nathan DM, Buse JB, Davidson MB, et al. Medical management of hyperglycaemia in type 2 diabetes mellitus: a consensus algorithm for the initiation and adjustment of therapy : aonsensus statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetologia. 2009;52(1):17–30. doi: 10.1007/s00125-008-1157-y. [DOI] [PubMed] [Google Scholar]
- 2.Salpeter SR, Greyber E, Pasternak GA, Salpeter EE. Risk of fatal and nonfatal lactic acidosis with metformin use in type 2 diabetes mellitus. Cochrane Database of Systematic Reviews. 2005;(4) doi: 10.1002/14651858.CD002967.pub4. Article ID CD002967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Seidowsky A, Nseir S, Houdret N, Fourrier F. Metformin-associated lactic acidosis: a prognostic and therapeutic study. Critical Care Medicine. 2009;37(7):2191–2196. doi: 10.1097/CCM.0b013e3181a02490. [DOI] [PubMed] [Google Scholar]
- 4.Peters N, Jay N, Barraud D, et al. Metformin-associated lactic acidosis in an intensive care unit. Critical Care. 2008;12(6, article no. R149) doi: 10.1186/cc7137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Heaney D, Majid A, Junor B. Bicarbonate haemodialysis as a treatment of metformin overdose. Nephrology Dialysis Transplantation. 1997;12(5):1046–1047. doi: 10.1093/ndt/12.5.1046. [DOI] [PubMed] [Google Scholar]
- 6.Jones GC, Macklin JP, Alexander WD. Contraindications to the use of metformin. British Medical Journal. 2003;326(7379):4–5. doi: 10.1136/bmj.326.7379.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stumvoll M, Nurjhan N, Perriello G, Dailey G, Gerich JE. Metabolic effects of metformin in non-insulin-dependent diabetes mellitus. The New England Journal of Medicine. 1995;333(9):550–554. doi: 10.1056/NEJM199508313330903. [DOI] [PubMed] [Google Scholar]
- 8.Owen MR, Doran E, Halestrap AP. Evidence that metformin exerts its anti-diabetic effects through inhibition of complex 1 of the mitochondrial respiratory chain. Biochemical Journal. 2000;348(3):607–614. [PMC free article] [PubMed] [Google Scholar]
- 9.Dykens JA, Jamieson J, Marroquin L, Nadanaciva S, Billis PA, Will Y. Biguanide-induced mitocondrial dysfunction yields increased lactate production and cytotoxicity of aerobically-poised HepG2 cells and human hepatocytes in vitro. Toxicology and Applied Pharmacology. 2008;233(2):203–210. doi: 10.1016/j.taap.2008.08.013. [DOI] [PubMed] [Google Scholar]
- 10.K/DOQI Workgroup. K/DOQI clinical practice guidelines for cardiovascular disease in dialysis patients. American Journal of Kidney Diseases. 2005;45(4, supplement 3):S1–153. [PubMed] [Google Scholar]


