Abstract
Epidemiologic studies seldom include wealth as a component of socioeconomic status. The authors investigated the associations between wealth and 2 broad outcome measures: mortality and self-rated general health status. Data from the longitudinal Panel Study of Income Dynamics, collected in a US population between 1984 and 2005, were used to fit marginal structural models and to estimate relative and absolute measures of effect. Wealth was specified as a 6-category variable: those with ≤0 wealth and quintiles of positive wealth. There were a 16%–44% higher risk and 6–18 excess cases of poor/fair health (per 1,000 persons) among the less wealthy relative to the wealthiest quintile. Less wealthy men, women, and whites had higher risk of poor/fair health relative to their wealthy counterparts. The overall wealth–mortality association revealed a 62% increased risk and 4 excess deaths (per 1,000 persons) among the least wealthy. Less wealthy women had between a 24% and a 90% higher risk of death, and the least wealthy men had 6 excess deaths compared with the wealthiest quintile. Overall, there was a strong inverse association between wealth and poor health status and between wealth and mortality.
Keywords: health status, inverse probability weighting, marginal structural model, mortality, socioeconomic status, wealth
The goal of this study was to explore the association between an uncommonly used measure of socioeconomic status (wealth) and 2 health outcomes (self-rated health status (SRH) and mortality). Wealth, the stockpile of resources amassed over the lifetime, differs from income, which is the flow of resources into the household (1).
Previous studies have found a consistent causal association between wealth and mortality: As wealth increases, mortality declines (2–7). The previous literature on the causal direction between wealth and SRH (and other health outcomes), however, is mixed. Although several studies have found that less wealth results in poorer health (8–16), others have found a more compelling argument for the effects working in the other direction, with poor health resulting in a decline in wealth (17–20). There is also some speculation that the wealth–morbidity association may be attributable to an unmeasured confounder. Although our study cannot address all potential sources of bias, it does better enable us to manage concerns expressed in prior studies. First, our use of marginal structural models produces improved estimates by better managing time-varying confounding. In addition, we provide both relative and absolute measures of effect and a longer follow-up time than other studies. Given these methodological improvements, we hope to more effectively address the question: Do the wealthy have a health advantage?
MATERIALS AND METHODS
We used data from the Panel Study of Income Dynamics, an ongoing longitudinal study of the US population that began in 1968. The design and content of the Panel Study have been previously described (21). Data for this study came from 7 waves of the Panel Study: 1984, 1989, 1994, 1999, 2001, 2003, and 2005. Health questions were asked only of the head of household and his/her partner.
Measures
The health outcomes examined in this study were SRH and mortality. The SRH variable was derived from the standard question, “Would you say your health in general is excellent, very good, good, fair, or poor?” In keeping with several other papers on wealth and health, it was dichotomized as excellent, very good, or good (coded as 0) versus fair or poor (coded as 1). Deaths were verified by using the National Death Index. However, the mortality status of respondents who were lost to follow-up was not matched to the National Death Index; thus, their vital status is unknown (22). The maximum follow-up time for mortality was 21 years (1984–2005) with a median of 17 years.
Family wealth in the Panel Study of Income Dynamics is well-measured and consistent with that from other studies (23). It was defined as total net worth, which includes the value of one's primary home, farm, or business assets, checking or savings accounts, vehicles, second homes, stocks, and bonds minus any debt. Wealth was adjusted for inflation by using the 2001 consumer price index and specified as a 6-category variable, where category 1 included all those that had ≤0 wealth, and categories 2–6 were quintiles of positive wealth. Wealth quintiles were based on the distribution of wealth for each survey year. In the final models, wealth was specified as 5 indicator terms to avoid making any assumptions about linearity. The referent group was the highest wealth quintile. For stratified models, wealth categories were redefined for only the population of interest; for example, the model for women defined wealth categories only among women. Models using alternative specifications of wealth are available in Web Tables 1–3, which are available on the Journal’s Web site (http://aje.oxfordjournals.org/).
Income, marital status, region of residence, education, age, race, sex, and time were included as covariates for both outcomes. Income was specified as a continuous poverty/income ratio using the annual poverty thresholds from the Census Bureau that accounts for household size (24). Marital status was categorized as married (referent group), never married or divorced, separated, or widowed and specified as indicator terms. The 3 indicator variables for region classified state of residence as Northeast, Midwest, or South; West was the referent group. Education was specified as 2 indicator variables (less than high school and high school degree), and greater than high school was the referent group. Age was specified as a continuous centered variable for both outcomes. An indicator variable for race included all nonwhite participants, which in the Panel Study of Income Dynamics consists mostly of African Americans, and the referent group was non-Hispanic white. Time was specified as a continuous variable and a cubic spline with knots at the 5th, 27.5th, 50th, 72.5th, and 95th percentiles. The mortality model also included baseline (and time-varying) SRH as a dichotomized covariate. Given the heterogeneity in wealth distribution by race and gender (1), we included race- and gender-stratified models for both mortality and SRH.
Statistical analysis
Adjusted associations were estimated by using both absolute (risk differences) and relative (risk ratio) measures of effect for the total population and by gender and race separately. For SRH, a binomial marginal structural model yielded adjusted risk ratios directly. For mortality, a cumulative incidence model, fitted with a logistic marginal structural model, was used to ascertain risk of death. Results from a Cox model were similar to those from the cumulative incidence model. Marginal structural models are effective in controlling for time-varying confounders; these are covariates that act as both confounders and mediators simultaneously (25). Risk differences were calculated by taking the differences between predicted probabilities estimated from a logistic marginal structural model. The delta method was used to estimate the variances for risk differences (26) via the marginal effects postestimation procedures available in STATA, version 10, software (27). Risk differences were calculated by holding all covariates at their mean values, which correspond to standardization of the effect estimates to the covariate distribution in the total study population (28).
The use of survey weights when analyzing data from the Panel Study of Income Dynamics produces nationally representative estimates. However, survey weights were not used in the current analysis, because we are interested in a substantive hypothesis rather than population representative prevalence estimates; thus, parameters estimated in our models have in-sample interpretations and are not applicable to the broader US population. Furthermore, survey weights from the Panel Study of Income Dynamics account for attrition. We calculated a censoring weight (discussed below) that serves a similar purpose.
The time-varying confounders for SRH were income and marital status; for mortality, SRH was also included. The main exposure, wealth, was time varying. Sex, race, age, education, and region were ascertained at baseline and treated as time invariant. Baseline values for all time-varying confounders were also included in the final marginal structural model. In SRH models, starting values from Poisson regression were used if binomial models did not converge (29).
In households where both the head of household and partner were present, there was clustering by household. Furthermore, there was 1 observation per time point per person, resulting in additional clustering by individual. We adjusted the variances for clustering at the highest level of aggregation, the household, which produced valid estimates by accounting for both sources of dependence (30, 31). For the SRH analysis, individuals who reported poor SRH at baseline were excluded, and only the first incidence of poor or fair SRH was modeled. Participants entered the study between 1984 and 2003 as long as they participated in more than 1 year of data collection. Those with only 1 wave of data collection were excluded, because they did not accrue person-time.
Inverse probability weights
Inverse probability weights control for time-varying confounding by creating a so-called pseudopopulation (25). Inverse probability weights were estimated from predicted probabilities obtained from logistic and multinomial models. Logistic models were used to obtain censoring weights, where the outcome of interest was whether or not an individual was lost to follow-up at that time point. Multinomial (i.e., proportional odds) models were used to obtain treatment weights; the 6-category wealth variable was the outcome. Multiplying the treatment and censoring weights resulted in the final inverse probability weight. In the weighting model, continuous variables, income and age (centered on the mean), were specified flexibly; age was specified as a linear term, squared term, and 2 quadratic splines, and income was specified as linear, squared, and cubic terms. Because these are stabilized inverse probability weight, the numerator of the weight contains all baseline covariates, while the denominator contains baseline and time-varying confounders. Several weighting models were tested, and the best one was chosen depending on the distribution of the inverse probability weight. Desirable properties for the inverse probability weight are a mean close to 1 and a small range (25, 32).
Very large values of the stabilized weight or means far from 1 indicated a possible violation of the positivity assumption or a misspecified weighting model. One strategy used to deal with extreme weights is to truncate or trim the weights (32). Depending on the model, 2% or 3% of the inverse probability weight was trimmed at each end. However, 5% of the inverse probability weight was trimmed in the mortality and SRH model for men. Trimming the weights resulted in means close to 1 and a much narrower range of values; however, it also resulted in less control for known confounders.
RESULTS
There were 26,615 persons that were either heads of household or partners for at least 1 wave between 1984 and 2005 in the Panel Study of Income Dynamics. The mortality analysis used this full sample. After excluding 2,419 participants with fair or poor health status at baseline and 8,451 with 1 wave of data collection, the final sample size for the SRH analysis was 15,745. Overall, there were 2,162 deaths (8.12%), and the prevalence of poor or fair health status was 16.4% at baseline. The age range for the full sample at baseline was 18–95 years of age.
Table 1 provides demographic characteristics overall and by quintiles of wealth for the full study population. After adjustment for inflation, the median wealth at baseline was approximately $17,925, but the mean wealth was close to $101,600, indicating the highly skewed nature of household wealth. The percentage in the poorest wealth category was higher for women compared with men (about 57.6% vs. 42.4%). As wealth increased, however, the male/female gap declined and was nearly eliminated at the highest quintile of wealth. In the wealthiest quintile, the proportion of white respondents to nonwhites was 6 times as high, while in the poorest wealth category the gap was reduced to about 1.5 times as high. Older, more educated, and higher income individuals had much more wealth than their younger, less educated, and lower income counterparts. For these 3 characteristics, there was a steady trend (Ptrend < 0.0001). Among the highest quintile of wealth, there were far more married persons (84.8%) compared with the never married (5.4%) or widowed, divorced, or separated (9.8%). In the crude analysis, the percentage of persons reporting poor SRH declined as wealth increased, but the percentage of deaths increased with greater wealth (because of increasing age). All bivariate analyses presented in Table 1 had P < 0.001.
Table 1.
Unweighted Demographic Characteristics of the Study Population at Baseline, Panel Study of Income Dynamics, United States, 1984–2005a
| Overall (N = 26,615) | ≤0 wealth (n = 4,642) | Quintile 1 (n = 4,883) | Quintile 2 (n = 4,377) | Quintile 3 (n = 3,412) | Quintile 4 (n = 3,007) | Quintile 5 (n = 2,896) | |
| Sex, % | |||||||
| Male | 46.8 | 42.4 | 47.9 | 48.6 | 48.0 | 48.3 | 48.8 |
| Female | 53.2 | 57.6 | 52.1 | 51.5 | 52.0 | 51.7 | 51.2 |
| Race. % | |||||||
| White | 51.7 | 38.6 | 47.1 | 57.6 | 63.8 | 75.0 | 86.3 |
| Nonwhite | 48.3 | 61.4 | 52.9 | 42.4 | 36.2 | 25.0 | 13.7 |
| Education, % | |||||||
| Less than high school | 25.3 | 30.3 | 27.8 | 19.3 | 22.5 | 17.3 | 12.5 |
| High school graduate | 39.0 | 36.7 | 45.0 | 40.9 | 39.5 | 38.6 | 36.7 |
| Greater than high school | 35.8 | 33.0 | 27.2 | 39.8 | 38.0 | 44.0 | 50.8 |
| Marital status, % | |||||||
| Never married | 21.9 | 43.2 | 33.1 | 21.1 | 12.3 | 8.6 | 5.4 |
| Married | 62.8 | 37.6 | 49.6 | 65.5 | 74.3 | 79.9 | 84.8 |
| Widowed, divorced, or separated | 15.4 | 19.2 | 17.3 | 13.4 | 13.4 | 11.5 | 9.8 |
| Mean age, years (SD) | 37.0 (15.1) | 31.4 (12.6) | 30.9 (12.4) | 33.1 (12.6) | 37.4 (14.1) | 41.8 (14.6) | 48.1 (15.1) |
| Mean income, dollars (SD) | 33,848 (37,208) | 20,690 (24,289) | 22,915 (19,609) | 32,581 (27,342) | 37,192 (26,295) | 44,797 (33,188) | 61,894 (75,873) |
| Median wealth, dollars (25%, 75%) | 17,925 (1,219, 78,925) | −7,607 (−5, 950, 0) | 3,687 (1,315, 5,713) | 19,521 (13,125, 25,411) | 52,903 (41,825, 62,471) | 118,455 (93,450, 138,066) | 605,641 (222,440, 528,163) |
| Health outcomes, % | |||||||
| Prevalence of poor healthb | 16.4 | 19.8 | 14.2 | 11.9 | 14.0 | 12.6 | 12.1 |
| Risk of deathc | 8.1 | 5.7 | 5.4 | 6.2 | 7.9 | 10.6 | 17.7 |
Abbreviation: SD, standard deviation.
Total sample size for bivariate analysis is 23,217. This is the full sample of all heads and partners minus those who are missing wealth data at their baseline visit.
Prevalence of poor health status at baseline visit by wealth quintile at baseline visit.
Risk of death over entire follow-up period by wealth quintile at baseline visit.
Wealth and SRH
As seen in Table 2, there was a strong association between SRH and wealth on both the relative and absolute scales. In the fully adjusted binomial model, as wealth increased the risk of poor SRH declined. Those with ≤0 wealth and those in quintile 1 had a higher risk of poor SRH relative to the wealthiest quintile (risk ratio (RR) = 1.42, 95% confidence interval (CI): 1.17, 1.74 and RR = 1.44, 95% CI: 1.21, 1.72), respectively. Those in quintiles 2–4 also had an elevated risk of poor health (RR = 1.19, 95% CI: 1.00, 1.42; RR = 1.20, 95% CI: 1.02, 1.41; and RR = 1.16, 95% CI: 1.00, 1.36, respectively) relative to the wealthiest quintile.
Table 2.
Risk Ratios and 95% Confidence Intervals for the Association Between Wealth and Poor/Fair Self-rated Health and Wealth and Mortality for the Total Population, Panel Study of Income Dynamics, United States, 1984–2005
| SRH (n = 14,533) |
Mortality (n = 21,479) |
|||
| RR | 95% CI | RR | 95% CI | |
| ≤0 wealth | 1.42 | 1.17, 1.74 | 1.62 | 1.29, 2.05 |
| Quintile 1 | 1.44 | 1.21, 1.72 | 1.29 | 1.03, 1.62 |
| Quintile 2 | 1.19 | 1.00, 1.42 | 1.31 | 1.05, 1.64 |
| Quintile 3 | 1.20 | 1.02, 1.41 | 1.26 | 1.03, 1.55 |
| Quintile 4 | 1.16 | 1.00, 1.36 | 1.17 | 0.97, 1.41 |
| Quintile 5 | 1.00 | Referent | 1.00 | Referent |
Abbreviations: CI, confidence interval; RR, risk ratio; SRH, self-rated health.
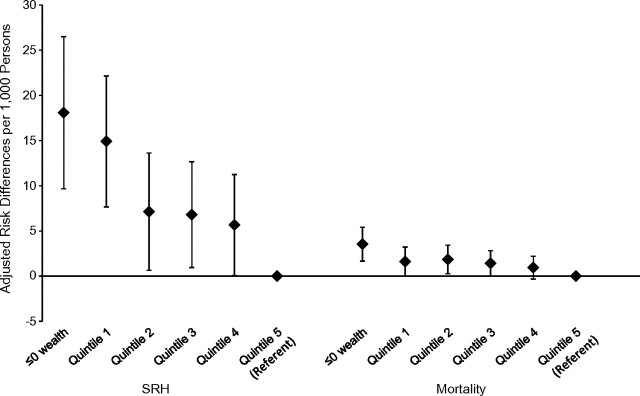
Risk differences were expressed as the number of excess cases of poor health attributable to having lower wealth instead of high wealth (quintile 5) per 1,000 persons from 1984 to 2005 (Figure 1). After adjustment for covariates, among those with ≤0 wealth, there were 18 (95% CI: 10, 26) excess cases, in quintile 1 there were 15 (95% CI: 8, 22), and in quintile 2 there were 7 (95% CI: 1, 14). Quintiles 3 and 4 had 7 (95% CI: 1, 13) and 6 (95% CI: 0, 11) excess cases of poor health, respectively.
Figure 1.
Risk differences and 95% confidence intervals per 1,000 persons for poor/fair self-rated health and mortality by wealth quintile for the total population, Panel Study on Income Dynamics, United States, 1984–2005. Both models were adjusted for baseline covariates and time-varying income and marital status. The mortality model was also adjusted for time-varying self-rated health (SRH).
Stratified models for SRH revealed a similar pattern (Table 3). Among men and whites, the least wealthy had a higher risk of poor health on the risk ratio and risk difference scales (for men, RR = 1.41, 95% CI: 1.02, 1.96, risk difference (RD) = 21, 95% CI: 9, 33; for whites, RR = 1.89, 95% CI: 1.47, 2.44, RD = 22, 95% CI: 11, 33) compared with the wealthier quintiles. Among women, those with ≤0 wealth had a similarly elevated risk of poor health as those in quintile 1 (RR = 1.73, 95% CI: 1.33, 2.25 and RR = 1.82, 95% CI: 1.43, 2.31, respectively). The binomial model for nonwhites showed a near-null association for the poorest wealth quintiles and suggested a protective effect for the wealthier quintiles (although confidence intervals included 1).
Table 3.
Risk Ratios, Risk Differences,a and 95% Confidence Intervals for the Association Between Poor/Fair Self-rated Health and Wealth by Gender and Race, Panel Study of Income Dynamics, United States, 1984–2005b
| Menc (n = 6,801) |
Womend (n = 7,732) |
Whitee (n = 9,206) |
Nonwhitef (n = 5,586) |
|||||
| RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | |
| ≤0 wealth | 1.41 | 1.02, 1.96 | 1.73 | 1.33, 2.25 | 1.89 | 1.47, 2.44 | 0.97 | 0.75, 1.25 |
| Quintile 1 | 1.38 | 1.09, 1.75 | 1.82 | 1.43, 2.31 | 1.63 | 1.29, 2.06 | 0.97 | 0.76, 1.24 |
| Quintile 2 | 1.25 | 0.99, 1.58 | 1.47 | 1.16, 1.87 | 1.33 | 1.07, 1.65 | 0.86 | 0.67, 1.10 |
| Quintile 3 | 1.13 | 0.91, 1.41 | 1.55 | 1.23, 1.95 | 1.14 | 0.93, 1.41 | 0.85 | 0.66, 1.08 |
| Quintile 4 | 1.12 | 0.90, 1.38 | 1.26 | 1.01, 1.56 | 1.03 | 0.84, 1.26 | 0.85 | 0.67, 1.08 |
| Quintile 5 | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| RD |
95% CI |
RD |
95% CI |
RD |
95% CI |
RD |
95% CI |
|
| ≤0 wealth | 21 | 9, 33 | 25 | 14, 37 | 22 | 11, 33 | 2 | −14, 18 |
| Quintile 1 | 14 | 4, 24 | 25 | 15, 35 | 17 | 9, 25 | 0 | −15, 15 |
| Quintile 2 | 11 | 2, 20 | 15 | 6, 23 | 10 | 3, 16 | −8 | −22, 6 |
| Quintile 3 | 5 | −3, 13 | 17 | 9, 26 | 5 | −1, 10 | −7 | −21, 7 |
| Quintile 4 | 5 | −3, 12 | 8 | 1, 15 | 1 | −4, 6 | −8 | −22, 6 |
| Quintile 5 | Referent | Referent | Referent | Referent | ||||
Abbreviations: CI, confidence interval; Q, quintile; RD, risk difference; RR, risk ratio.
Per 1,000 persons.
All models adjusted for baseline covariates and time-varying income and marital status.
Unweighted cutpoints for wealth quintiles that correspond to the wealth distribution among men: Q1 ($1–$12,902); Q2 ($12,903–$44,515); Q3 ($44,516–$104,860); Q4 ($104,861–$262,122); Q5 (≥$262,123). The average debt for the male population was $15,845.
Unweighted cutpoints for wealth quintiles that correspond to the wealth distribution among women: Q1 ($1–$10,557); Q2 ($10,558–$39,160); Q3 ($39,161–$94,369); Q4 ($94,370–$238,810); Q5 (≥$238,811). The average debt for the female population was $14,037.
Unweighted cutpoints for wealth quintiles that correspond to the wealth distribution among whites: Q1 ($1–$20,762); Q2 ($20,763–$67,303); Q3 ($67,304–$149,573); Q4 ($149,574–$334,019); Q5 (≥$334,020). The average debt for the white population was $18,288.
Unweighted cutpoints for wealth quintiles that correspond to the wealth distribution among nonwhites: Q1 ($1–$5,047); Q2 ($5,048–$18,730); Q3 ($18,731–$44,531); Q4 ($44,532–$98,336); Q5 (≥$98,337). The average debt for the nonwhite population was $10,774.
Wealth and mortality
In the mortality analysis, on both the relative and absolute scales, there was an increased risk of death among less wealthy groups. As seen in Table 2, those with ≤0 wealth had a 62% higher risk of death compared with the wealthiest group (95% CI: 1.29, 2.05). Low-wealth quintiles 1 and 2 had similarly elevated risks of death of 29% (95% CI: 1.03, 1.62) and 31% (95% CI: 1.05, 1.64), respectively, while the risk of death fell for those in quintiles 3 (RR = 1.26, 95% CI: 1.03, 1.55) and 4 (RR = 1.17, 95% CI: 0.97, 1.41), respectively. On the absolute scale (Figure 1), this represented an excess of 4 (95% CI: 2, 5) deaths among the least wealthy, an excess of 2 (95% CI: 0, 3) deaths among quintiles 1 and 2, and an excess of 1 (95% CI: 0, 3 and 95% CI: 0, 2, respectively) death among those in quintiles 3 and 4 per 1,000 persons.
The stratified analysis in Table 4 showed that women in the least wealthy group had an increased risk of 90% relative to that for the wealthiest women (95% CI: 1.32, 2.72), while women in quintile 4 still had a 24% increased risk of death (95% CI: 0.92, 1.67). The models for men, whites, and nonwhites revealed an increased risk of death among the lowest wealth quintile (RR = 1.66, 95% CI: 1.22, 2.27, RR = 1.78, 95% CI: 1.26, 2.53, RR = 1.49, 95% CI: 1.03, 2.15, respectively), with a declining risk among higher wealth quintiles. There was an excess of 6 deaths among men, 4 among whites and nonwhites, and 3 among women in the least wealthy group (95% CI: 1, 10 for men; 95% CI: 1, 6 for whites; 95% CI: 1, 8 for nonwhites, and 95% CI: 1, 5 for women, respectively). Trend tests in both the SRH and mortality models showed a significant dose response except in models limited to nonwhites. Group or chunk tests for wealth were significant for all models. Refer to Web Table 4 for trend and group test results.
Table 4.
Risk Ratios, Risk Differences,a and 95% Confidence Intervals for the Association Between Mortality and Wealth by Gender and Race, Panel Study of Income Dynamics, United States, 1984–2005b
| Menc (n = 9,870) |
Womend (n = 11,040) |
Whitee (n = 12,327) |
Nonwhitef (n = 8,576) |
|||||
| RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | |
| ≤0 wealth | 1.66 | 1.22, 2.27 | 1.90 | 1.32, 2.72 | 1.78 | 1.26, 2.53 | 1.49 | 1.03, 2.15 |
| Quintile 1 | 1.27 | 0.94, 1.72 | 1.56 | 1.10, 2.21 | 1.42 | 1.06, 1.90 | 1.19 | 0.80, 1.77 |
| Quintile 2 | 1.21 | 0.90, 1.63 | 1.71 | 1.21, 2.43 | 1.23 | 0.91, 1.66 | 1.03 | 0.67, 1.58 |
| Quintile 3 | 1.13 | 0.87, 1.47 | 1.64 | 1.18, 2.27 | 1.21 | 0.93, 1.57 | 1.49 | 1.02, 2.18 |
| Quintile 4 | 1.11 | 0.86, 1.44 | 1.24 | 0.92, 1.67 | 1.05 | 0.82, 1.35 | 1.40 | 0.95, 2.05 |
| Quintile 5 | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| RD |
95% CI |
RD |
95% CI |
RD |
95% CI |
RD |
95% CI |
|
| ≤0 wealth | 6 | 1, 10 | 3 | 1, 5 | 4 | 1, 6 | 4 | 1, 8 |
| Quintile 1 | 3 | −1, 6 | 2 | 0.4, 4 | 2 | 0.2, 4 | 2 | −2, 5 |
| Quintile 2 | 2 | −2, 5 | 3 | 1, 4 | 1 | −1, 3 | 0.3 | −3, 4 |
| Quintile 3 | 1 | −3, 4 | 2 | 1, 4 | 1 | −0.4, 3 | 4 | 0.3, 8 |
| Quintile 4 | 0.4 | −3, 3 | 1 | −0.3, 2 | 0.3 | −1, 2 | 3 | −0.4, 7 |
| Quintile 5 | Referent | Referent | Referent | Referent | ||||
Abbreviations: CI, confidence interval; Q, quintile; RD, risk difference; RR, risk ratio.
Per 1,000 persons.
All models adjusted for baseline covariates and time-varying income, marital status, and general health status.
Unweighted cutpoints for wealth quintiles that correspond to the wealth distribution among men: Q1 ($1–$12,902); Q2 ($12,903–$44,515); Q3 ($44,516–$104,860); Q4 ($104,861–$262,122); Q5 (≥$262,123). The average debt for the male population was $15,845.
Unweighted cutpoints for wealth quintiles that correspond to the wealth distribution among women: Q1 ($1–$10,557); Q2 ($10,558–$39,160); Q3 ($39,161–$94,369); Q4 ($94,370–$238,810); Q5 (≥$238,811). The average debt for the female population was $14,037.
Unweighted cutpoints for wealth quintiles that correspond to the wealth distribution among whites: Q1 ($1–$20,762); Q2 ($20,763–$67,303); Q3 ($67,304–$149,573); Q4 ($149,574–$334,019); Q5 (≥$334,020). The average debt for the white population was $18,288.
Unweighted cutpoints for wealth quintiles that correspond to the wealth distribution among nonwhites: Q1 ($1–$5,047); Q2 ($5,048–$18,730); Q3 ($18,731–$44,531); Q4 ($44,532–$98,336); Q5 (≥$98,337). The average debt for the nonwhite population was $10,774.
DISCUSSION
As hypothesized, in our study wealthier individuals reported being healthier and had lower mortality. We also hypothesized that the effects would be stronger for women and nonwhites. Stratified SRH and mortality models revealed that wealthier men, women, and whites reported better health and lower mortality, but this was not the case for nonwhites (as evidenced by results from trend tests) on both the absolute and relative scales. We did, however, see larger magnitudes in the point estimates for women relative to men.
Our findings for nonwhites are likely because of the limited distribution of wealth among minorities. The unweighted data in Table 3 show that some of the wealthiest nonwhites would only correspond to quintile 3 among whites. This lack of variability in wealth among nonwhites makes it difficult to detect an association between wealth and health among this subgroup. Others have suggested that, because of racism and discrimination, high socioeconomic status does not afford the same health benefits among minorities as it does for whites, another possible explanation for our results (33). Our findings for gender, however, are consistent with those from prior research (34). We found that there were more cases of poor health among women compared with men (higher morbidity), but for the poorest men (those with ≤0 wealth), the burden of mortality was higher (higher mortality).
Several mechanisms have been proposed for how low socioeconomic status impacts health outcomes. The less wealthy may be more subject to poor physical and social environments, which can encourage health-damaging exposures (35). In addition, the lack of a safety net associated with having little or no wealth can cause chronic stress among the poor, which in turn can trigger a series of biologic events, through central nervous system activation of autonomic, neuroendocrine, and immune responses resulting in poor health (36).
Previous studies on wealth and mortality (2–7) and on wealth and SRH (13, 14) found results similar to ours. There were, however, 2 US studies that found no association between wealth and mortality and several econometric analyses that found little support for the conclusion that low levels of wealth were associated with poor health (17–20). Instead, these papers suggested the opposite, that poor health caused declines in wealth (17, 18, 20). One study suggested that an important mediator, baseline health status, was the main driver of mortality, and socioeconomic status was less relevant among an elderly cohort (37), while other studies used short follow-up periods to assess the question of reverse causation (17–20, 38). A serious change in health status is likely to have an immediate effect on a household's financial well being, evidenced by the fact that most personal bankruptcies were caused by illness of a family member (in 2007 over 60%) (39). Therefore, a longer follow-up period may be needed to see the effects of low wealth on poor health.
By using longitudinal data with an extensive follow-up and a method that controls for time-varying confounding, we presented estimates that corroborate the hypothesis that low levels of wealth are associated with poor health perceived health status. Other studies with long follow-up times further corroborated our results (13).
Limitations of our study included selection bias caused by the exclusion of baseline cases in the SRH analysis. Those in poor health were more likely to be older and less wealthy. Thus, our effect estimates may be biased downward toward the null and may underestimate the true effect (40). In addition, baseline cases of poor SRH were excluded from the analysis to improve inference; however, given measurement error, the subjective nature of SRH, and the lack of SRH data prior to 1984, we were unable to create a truly “disease-free” cohort. Therefore, the possibility for reverse causation still exists.
Another limitation in the mortality analysis was the relatively high level of attrition in the Panel Study of Income Dynamics (about 3% per year, cumulatively about 50% since the inception of the study) (41). Respondents who were lost to follow-up were included in the analysis and censored at their last time point; however, their mortality status remained unknown. Differential mortality between censored and uncensored respondents (e.g., censored individuals had higher mortality rates and were less wealthy) would result in bias toward the null and an underestimation of the real mortality risk. In an intensive follow-up effort, the Panel Study of Income Dynamics found that up to 14% of censored participants could be deceased, thus potentially introducing bias from uncounted deaths (22).
Regardless of the close conceptual association between income and wealth, we believed that adjusting for income was necessary in order to understand the true effect of wealth on these health outcomes. Empirically, there is a moderate correlation between income and wealth in the Panel Study of Income Dynamics (on average, r = 0.41), which has been noted elsewhere (1). In sensitivity analysis, SRH models that excluded both baseline and time-varying income revealed risk ratios of a substantially larger magnitude, suggesting that income attenuated the effect of wealth on SRH. Thus, at the very least, our results provide conservative estimates of the wealth-health association.
Finally, some have questioned the usefulness of SRH as a health outcome for assessing social inequalities (42–44) and for etiologic research (45). The use of SRH in our study, however, may be more justified because of the well-measured wealth variable (which many other health studies lack) coupled with limited health information in the Panel Study of Income Dynamics.
There were several strengths to our study. First, as noted above, wealth data in the Panel Study were rigorously and comprehensively measured (23). Many epidemiologic studies measure wealth crudely, resulting in invalid or underestimated results (46). In addition, our extensive longitudinal data allowed us to explore the question of wealth and health from a life-course perspective. Many studies of wealth and health have used cross-sectional data, and several longitudinal studies had relatively short follow-up times. A related advantage was our use of the marginal structural model as the analytical technique. Comparing estimates from the marginal structural model with those from the traditional approach (refer to Web Table 5) indicated that traditional estimates for mortality were closer to the null, while estimates were similar for SRH. Therefore, it appears that time-varying confounding was stronger for mortality compared with the SRH models. The use of the marginal structural model presumes a manipulable exposure and a realistic intervention regime (47). Since wealth distributions are partly determined by government policies such as tax laws, this assumption of manipulability is reasonable. However, given that some unmeasured confounding is likely, wealth is not randomizable, the possibility for reverse causation still exists, and the causal interpretation of our estimates is limited. Nonetheless, we believe our study is an improvement over previous research.
In conclusion, after control for income and education, our study found a consistent gradient between wealth and health overall and among men, women, and whites. That is, wealth captures something different from income and education that should be independently evaluated not only to understand how socioeconomic status impacts health but also to determine how to prevent poor health.
Supplementary Material
Acknowledgments
Author affiliations: Department of Epidemiology, School of Public Health, University of Michigan, Ann Arbor, Michigan (Anjum Hajat); Department of Epidemiology, Biostatistics, and Occupational Health, McGill University, Montreal, Canada (Jay S. Kaufman); Department of Epidemiology, Gillings School of Global Public Health, University of North Carolina, Chapel Hill, North Carolina (Kathryn M. Rose, James C. Thomas); and Division of Social and Behavioural Health Sciences, Dalla Lana School of Public Health, University of Toronto, Toronto, Canada (Arjumand Siddiqi).
This work was supported by the Robert and Kristen Greczyn scholarship granted by the University of North Carolina School of Public Health, the Smith research grant awarded by the University of North Carolina Graduate School, and the US Public Health Service Traineeship awarded by the Health Resources and Services Administration all awarded to A. H.
The authors would like to thank Dr. Amar Hamoudi for his valuable comments on the manuscript. In addition, they would like to thank Dr. Daniel Westreich for expert assistance on fitting marginal structural models and Dr. Whitney Robinson for general methodological assistance. Finally, they would like to thank Dr. Ana Diez-Roux for her support of this work.
Conflict of interest: none declared.
Glossary
Abbreviations
- CI
confidence interval
- RD
risk difference
- RR
risk ratio
- SRH
self-rated health status
References
- 1.Keister LA. Wealth in America: Trends in Wealth Inequality. Cambridge, United Kingdom: Cambridge University Press; 2000. [Google Scholar]
- 2.Mare RD. Socioeconomic careers and differential mortality among older men in the United States. In: Vallin J, D'Souza S, Palloni A, editors. Measurement and Analysis of Mortality: New Approaches. New York, NY: Oxford University Press; 1990. pp. 362–387. [Google Scholar]
- 3.Menchik PL. Economic status as a determinant of mortality among black and white older men: does poverty kill? Popul Stud. 1993;47(3):427–436. [Google Scholar]
- 4.Bond Huie SA, Krueger PM, Rogers RG, et al. Wealth, race, and mortality. Soc Sci Q. 2003;84(3):667–684. [Google Scholar]
- 5.Attanasio OP, Hoynes HW. Differential mortality and wealth accumulation. J Hum Resour. 2000;35(1):1–29. [Google Scholar]
- 6.Cunningham WE, Hays RD, Duan N, et al. The effect of socioeconomic status on the survival of people receiving care for HIV infection in the United States. J Health Care Poor Underserved. 2005;16(4):655–676. doi: 10.1353/hpu.2005.0093. [DOI] [PubMed] [Google Scholar]
- 7.Daly MC, Duncan GJ, McDonough P, et al. Optimal indicators of socioeconomic status for health research. Am J Public Health. 2002;92(7):1151–1157. doi: 10.2105/ajph.92.7.1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mutchler JE, Burr JA. Racial differences in health and health care service utilization in later life: the effect of socioeconomic status. J Health Soc Behav. 1991;32(4):342–356. [PubMed] [Google Scholar]
- 9.Robert S, House JS. SES differentials in health by age and alternative indicators of SES. J Aging Health. 1996;8(3):359–388. doi: 10.1177/089826439600800304. [DOI] [PubMed] [Google Scholar]
- 10.Ostrove JM, Feldman P, Adler NE. Relations among socioeconomic status indicators and health for African-Americans and whites. J Health Psychol. 1999;4(4):451–463. doi: 10.1177/135910539900400401. [DOI] [PubMed] [Google Scholar]
- 11.Wenzlow AT, Mullahy J, Robert SA, et al. An Empirical Investigation of the Relationship Between Wealth and Health Using the Survey of Consumer Finances. Madison, WI: Institute for Research on Poverty; 2004. [Google Scholar]
- 12.Smith JP, Kington R. Race, socioeconomic status, and health in late life. In: Martin L, Solbo B, editors. Racial and Ethnic Differences in the Health of Older Americans. Washington, DC: National Academy Press; 1997. pp. 106–162. [Google Scholar]
- 13.Shuey KM, Willson AE. Cumulative disadvantage and black-white disparities in life-course health trajectories. Res Aging. 2008;30(2):200–225. [Google Scholar]
- 14.Rodriguez E, Allen JA, Frongillo EA, Jr, et al. Unemployment, depression, and health: a look at the African-American community. J Epidemiol Community Health. 1999;53(6):335–342. doi: 10.1136/jech.53.6.335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kennickell AB. What is the difference? Evidence on the distribution of wealth, health, life expectancy, and health insurance coverage. Stat Med. 2008;27(20):3927–3940. doi: 10.1002/sim.3375. [DOI] [PubMed] [Google Scholar]
- 16.Demakakos P, Nazroo J, Breeze E, et al. Socioeconomic status and health: the role of subjective social status. Soc Sci Med. 2008;67(2):330–340. doi: 10.1016/j.socscimed.2008.03.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Adams P, Hurd MD, McFadden D, et al. Healthy, wealthy, and wise? Tests for direct causal paths between health and socioeconomic status. J Econom. 2003;112(1):3–56. [Google Scholar]
- 18.Hurd M, Kapteyn A. Health, wealth, and the role of institutions. J Hum Resour. 2003;38(2):386–415. [Google Scholar]
- 19.Meer J, Miller DL, Rosen HS. Exploring the health-wealth nexus. J Health Econ. 2003;22(5):713–730. doi: 10.1016/S0167-6296(03)00059-6. [DOI] [PubMed] [Google Scholar]
- 20.Smith JP. Healthy bodies and thick wallets: the dual relation between health and economic status. J Econ Perspect. 1999;13(2):144–166. [PMC free article] [PubMed] [Google Scholar]
- 21.Panel Study of Income Dynamics. An overview of the Panel Study of Income Dynamics. Ann Arbor, MI: Panel Study of Income Dynamics; 2000. ( http://psidonline.isr.umich.edu/Guide/Overview.html). (Accessed September 7, 2010) [Google Scholar]
- 22.McGonagle K, Smith JP, Schoeni RF. The PSID Sample Leaver Tracking Project. Ann Arbor, MI: PSID Technical Paper Series; 2008. [Google Scholar]
- 23.Curtin R, Juster FT, Morgan J. Survey estimates of wealth: an assessment of quality. In: Lipsey RE, Tice HS, editors. The Measurement of Saving, Investment, and Wealth. Chicago, IL: University of Chicago Press; 1989. pp. 473–548. [Google Scholar]
- 24.Bureau of the Census, US Department of Commerce. Poverty thresholds by size of family and number of children. 1984–2005. Washington, DC: Bureau of the Census; 2010. ( http://www.census.gov/hhes/www/poverty/data/threshld/index.html). (Accessed September 7, 2010) [Google Scholar]
- 25.Robins JM, Hernán MA, Brumback B. Marginal structural models and causal inference in epidemiology. Epidemiology. 2000;11(5):550–560. doi: 10.1097/00001648-200009000-00011. [DOI] [PubMed] [Google Scholar]
- 26.Oehlert GW. A note on the delta method. Am Stat. 1992;46(1):27–29. [Google Scholar]
- 27.STATA statistical software: release 10. College Station, TX: StataCorp LP; 2007. [Google Scholar]
- 28.Localio AR, Margolis DJ, Berlin JA. Relative risks and confidence intervals were easily computed indirectly from multivariable logistic regression. J Clin Epidemiol. 2007;60(9):874–882. doi: 10.1016/j.jclinepi.2006.12.001. [DOI] [PubMed] [Google Scholar]
- 29.Spiegelman D, Hertzmark E. Easy SAS calculations for risk or prevalence ratios and differences [invited editorial note] Am J Epidemiol. 2005;162(3):199–200. doi: 10.1093/aje/kwi188. [DOI] [PubMed] [Google Scholar]
- 30.Miglioretti DL, Heagerty PJ. Marginal modeling of nonnested multilevel data using standard software. Am J Epidemiol. 2007;165(4):453–463. doi: 10.1093/aje/kwk020. [DOI] [PubMed] [Google Scholar]
- 31.Angeles G, Guilkey DK, Mroz TA. The impact of community-level variables on individual-level outcomes: theoretical results and applications. Sociol Methods Res. 2005;34(1):76–121. [Google Scholar]
- 32.Cole SR, Hernán MA. Constructing inverse probability weights for marginal structural models. Am J Epidemiol. 2008;168(6):656–664. doi: 10.1093/aje/kwn164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Williams DR. Race, socioeconomic status, and health. The added effects of racism and discrimination. Ann N Y Acad Sci. 1999;896(1):173–188. doi: 10.1111/j.1749-6632.1999.tb08114.x. [DOI] [PubMed] [Google Scholar]
- 34.Rieker PP, Bird CE. Rethinking gender differences in health: why we need to integrate social and biological perspectives. J Gerontol B Psychol Sci Soc Sci. 2005;60(special issue II):40–47. doi: 10.1093/geronb/60.special_issue_2.s40. [DOI] [PubMed] [Google Scholar]
- 35.Adler NE, Rehkopf DH. U.S. disparities in health: descriptions, causes, and mechanisms. Annu Rev Public Health. 2008;29(1):235–252. doi: 10.1146/annurev.publhealth.29.020907.090852. [DOI] [PubMed] [Google Scholar]
- 36.Steptoe A, Marmot M. The role of psychobiological pathways in socio-economic inequalities in cardiovascular disease risk. Eur Heart J. 2002;23(1):13–25. doi: 10.1053/euhj.2001.2611. [DOI] [PubMed] [Google Scholar]
- 37.Feinglass J, Lin S, Thompson J, et al. Baseline health, socioeconomic status, and 10-year mortality among older middle-aged Americans: findings from the Health and Retirement Study, 1992, 2002. J Gerontol B Psychol Sci Soc Sci. 2007;62(4):S209–S217. doi: 10.1093/geronb/62.4.s209. [DOI] [PubMed] [Google Scholar]
- 38.Wu S. The effects of health events on the economic status of married couples. J Hum Resour. 2003;38(1):219–230. [Google Scholar]
- 39.Himmelstein DU, Thorne D, Warren E, et al. Medical bankruptcy in the United States, 2007: results of a national study. Am J Med. 2009;122(8):741–746. doi: 10.1016/j.amjmed.2009.04.012. [DOI] [PubMed] [Google Scholar]
- 40.Flanders WD, Klein M. Properties of 2 counterfactual effect definitions of a point exposure. Epidemiology. 2007;18(4):453–460. doi: 10.1097/01.ede.0000261472.07150.4f. [DOI] [PubMed] [Google Scholar]
- 41.Fitzgerald J, Gottschalk P, Moffitt R. An analysis of sample attrition in panel data: the Michigan Panel Study of Income Dynamics. J Hum Resour. 1998;33(2):251–299. [Google Scholar]
- 42.Delpierre C, Lauwers-Cances V, Datta GD, et al. Using self-rated health for analysing social inequalities in health: a risk for underestimating the gap between socioeconomic groups? J Epidemiol Community Health. 2009;63(6):426–432. doi: 10.1136/jech.2008.080085. [DOI] [PubMed] [Google Scholar]
- 43.Dowd JB, Zajacova A. Does the predictive power of self-rated health for subsequent mortality risk vary by socioeconomic status in the US? Int J Epidemiol. 2007;36(6):1214–1221. doi: 10.1093/ije/dym214. [DOI] [PubMed] [Google Scholar]
- 44.Singh-Manoux A, Dugravot A, Shipley MJ, et al. The association between self-rated health and mortality in different socioeconomic groups in the GAZEL cohort study. Int J Epidemiol. 2007;36(6):1222–1228. doi: 10.1093/ije/dym170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jylhä M. What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Soc Sci Med. 2009;69(3):307–316. doi: 10.1016/j.socscimed.2009.05.013. [DOI] [PubMed] [Google Scholar]
- 46.Pollack CE, Chideya S, Cubbin C, et al. Should health studies measure wealth? A systematic review. Am J Prev Med. 2007;33(3):250–264. doi: 10.1016/j.amepre.2007.04.033. [DOI] [PubMed] [Google Scholar]
- 47.Levine B. Causal models. Epidemiology. 2009;20(6):931. doi: 10.1097/EDE.0b013e3181ba36f6. author reply 931–932. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.