Abstract
Segregation studies suggest that the health of blacks in the United States is poorer in majority-black compared with mixed-race neighborhoods. However, segregation studies have not examined black immigrants, who may benefit from social support and country-of-origin foods in black immigrant areas. The authors used 1995–2003 New York City birth records and a spatial measure of ethnic density to conduct a cross-sectional investigation of the risks of preterm birth for African-, Caribbean-, and US-born non-Hispanic black women associated with neighborhood-level African-, Caribbean-, and US-born non-Hispanic black density, respectively. Preterm birth risk differences were computed from logistic model coefficients, comparing neighborhoods in the 90th percentile of ethnic density with those in the 10th percentile. African black preterm birth risks increased with African density, especially in more deprived neighborhoods, where the risk difference was 6.1 per 1,000 (95% confidence interval: 1.9, 10.2). There was little evidence of an ethnic density effect among non-Hispanic black Caribbeans. Among US-born non-Hispanic blacks, an increase in preterm birth risk associated with US-born black density was observed in more deprived neighborhoods only (risk difference = 12.5, 95% confidence interval: 6.6, 18.4). Ethnic density seems to be more strongly associated with preterm birth for US-born non-Hispanic blacks than for non-Hispanic black immigrants.
Keywords: continental population groups, emigrants and immigrants, premature birth, residence characteristics, social environment
Investigations into the health effects of residential segregation and neighborhood ethnic density in the United States have focused primarily on the black population, seeking to explain ethnic disparities in a variety of health outcomes (1–3). These studies have generally found higher neighborhood proportions of black residents to be associated with poorer health in the black population (4–23). Segregation and ethnic density studies to date have typically treated black Americans as a homogeneous group, despite recent immigration from Africa and the Caribbean that makes the black population increasingly diverse (24), and despite the fact that, like foreign-born Hispanics (25), black immigrants appear to have better health outcomes than their US-born counterparts (26–33).
This limited attention to black immigrant neighborhoods represents an important gap in the literature, because ethnic density may be central to the immigrant health advantage; for example, positive immigrant health outcomes are often attributed to healthful country-of-origin foods (34), which are likely to be more accessible in immigrant areas, and to social support (35), which may be facilitated by close residential proximity to those with shared language and cultural affiliations. More broadly, it has been argued that ethnic density protects individuals belonging to minority or nondominant groups from a sense of cultural isolation (36) and low social status (37). Health benefits of ethnic density have been observed in European (36, 38, 39) and Hispanic (40–43) immigrant populations in the United States.
We sought to determine whether non-Hispanic black African and Caribbean immigrants respond to ethnic density similarly to US-born blacks, who experience increased risks associated with own-group density, or whether they resemble European and Hispanic immigrants, who appear to benefit from immigrant enclaves. We used geocoded 1995–2003 New York City birth records, which provide sufficient power to examine immigrant birth outcomes, and a census-based spatial measure of ethnic and immigrant density to estimate the association between African-, Caribbean-, and US-born black density in the maternal neighborhood and, respectively, African-, Caribbean-, and US-born black women's risk of giving birth preterm. We considered preterm birth because it is the leading contributor to the black-white disparity in infant mortality in the United States (1, 44), and it seems to be sensitive to material and psychosocial factors that may be influenced by ethnic density (45–50).
MATERIALS AND METHODS
Data sources and management
New York City birth records from January 1, 1995, through December 31, 2003, geocoded to the census tract level, were provided by the New York City Department of Health and Mental Hygiene. Use of the data for this study was approved by the University of North Carolina at Chapel Hill Institutional Review Board. Of 925,277 singleton births to New York City residents with complete census tract, gestational age, maternal ethnicity, and maternal country-of birth data (87.8% of all 1995–2003 records), we identified 254,928 non-Hispanic black mothers. We did not include black Hispanic women in this analysis because nearly 40% of Hispanics report a racial identity of “other” on the census (51), limiting our ability to accurately estimate black Hispanic neighborhood density.
Over half (n = 141,969) of the non-Hispanic black mothers were US-born. Among the foreign-born, we identified 21,088 African and 74,718 Caribbean immigrants, defined as women born in countries in the United Nations–defined African and Caribbean regions, respectively (52) (Web Table 1; this information is described in the first of 6 supplementary tables referred to as “Web Table” in the text and posted on the Journal’s Web site (http://aje.oupjournals.org/)). We included an additional 12,308 women born in Guyana, Suriname, or French Guiana—3 non-Spanish-speaking countries on the Caribbean coast of South America—in the Caribbean group, bringing the total number of Caribbeans to 87,026; we also conducted a sensitivity analysis by excluding the South American women. We excluded births to non-Hispanic black immigrants who were not African or Caribbean (n = 4,845).
The New York City Department of Health and Mental Hygiene assigned 1990 tract numbers to births occurring in 1995–1999 and 2000 tract numbers to births occurring in 2000–2003. Between the 2 censuses, the US Census Bureau split some 1990 census tracts to create two 2000 census tracts and merged some 1990 tract pairs to create single 2000 tracts (53). To create consistent tract numbers over time, we gave 1990 tracts that were merged in 2000 their corresponding 2000 tract numbers. Likewise, we gave 2000 tracts that had split from 1990 tracts their “parent” 1990 tract numbers.
To estimate ethnic and immigrant density, we downloaded tract-level African-, Caribbean-, and US-born non-Hispanic black population counts from Summary File 4 of the 2000 US Census. Summary File 4 provides data on 2,105 New York City census tracts, excluding 111 with fewer than 100 people in any ethnic group or fewer than 50 unweighted sample cases (54). Births occurring in these 111 tracts were excluded from our analysis (<1% in each group), leaving 21,064 black African births in 1,452 tracts, 86,961 black Caribbean births in 1,797 tracts, and 141,760 black American births in 1,885 tracts. The Census Bureau also suppresses population counts for African-, Caribbean-, and US-born non-Hispanic blacks in census tracts with large total populations but fewer than 100 non-Hispanic black residents (54), resulting in missing exposure data for 8.1% of African births, 5.8% of Caribbean births, and 6.5% of births to US-born black women. Suppressed black population counts in these tracts were assumed to be trivial relative to the total population of the tract and were set to zero; a supplemental analysis was conducted with these tracts excluded to assess the extent to which they influenced the findings.
Area-level covariates were obtained from Summary File 3 of the 2000 US Census.
Variables and variable construction
We defined the outcome, preterm birth, as a live singleton birth with a clinical estimate of gestational age of more than 20 but less than 37 weeks (55). The clinical estimate of gestational age has been found to be more accurate than estimates based on the last menstrual period alone (56, 57).
We defined the exposure, neighborhood immigrant or ethnic density (subsequently referred to as “ethnic density”), as the percentage of the population in an African-, Caribbean-, or US-born non-Hispanic black woman's area of residence that was non-Hispanic black and born in Africa, the Caribbean, or the United States, respectively. Following Reardon and Firebaugh (58) and Reardon et al. (59), we assumed that the areas nearest a woman's residence contributed most to her experience of neighborhood-level ethnic density. We allowed the influence of populations farther away to decrease in proportion to distance. Because they were the smallest unit available in the birth records, we used census tracts to locate women geographically; New York City census tracts are small, with a median area of 0.18 km2, providing fairly precise locations. We estimated the distance from each woman's residence to other populations by computing distances between geographically weighted census tract centers (centroids) (60) with ArcView GIS software (ESRI, Redlands, California).
We calculated the proximity-weighted ethnic density (58) experienced by a woman M residing in census tract J (ΠJM) by multiplying the number of people sharing her ethnic identity in each census tract K (xKM) by a weight (pJK) that represents the proximity of tracts J and K. We summed these weighted ethnic populations and divided them by total census tract populations (xK) that were weighted in the same way. Doing so produced a “percentage,” as shown below:
 |
The proximity weight (pJK) allows census tract K’s influence to decay in an approximately Gaussian manner with its distance from census tract J (61):
where is the distance between census tracts J and K. Note that if J = K, then dJK = 0 and = 1; that is, a census tract’s own ethnic composition has maximal influence on its estimated ethnic density. Because we were not using continuous values of but instead using between-tract distances, not all possible values of were used to compute the exposure. The variable r is the distance from census tract J beyond which there is no influence on J’s estimated ethnic density. The value of the radius is chosen based on the total area thought to influence those living in census tract J. Lee et al. (61) suggest a radius of 500 m to approximate neighborhoods accessible by foot, which we considered appropriate for a dense urban area such as New York City. Supplemental analyses with other suggested radii (1,000 m, 2,000 m, 4,000 m) produced similar ethnic density–preterm birth results but decreased precision of the estimates. This measure is discussed further elsewhere (Mason et al., “Ethnic Density and Preterm Birth Across Seven Ethnic Groups in New York City,” unpublished manuscript).
We included the following individual-level covariates in adjusted models because they are associated with preterm birth, vary by ethnicity and nativity, and/or are markers of socioeconomic status (62): maternal age (indicators for <20, 20–34, and ≥35 years), education taking age into account (indicators for <12 years and age <20 years, <12 years and age ≥20 years, 12 years, 13–15 years, and ≥16 years), parity (indicators for 1, 2–5, and ≥6 previous births), tobacco use (smoker or nonsmoker), prepregnancy weight (indicators for <125, 125–150, and >150 pounds (1 pound = 0.45 kg)), and payment type (indicators for private insurance, Medicaid, or out-of-pocket (self-pay)).
We included residential stability and neighborhood deprivation as contextual-level covariates. We defined residential stability as the percentage of the neighborhood population residing in the same house from 1995 to 2000. Neighborhood deprivation was represented by using a standardized index arising from 17 tract-level census variables (Web Table 2) that were summarized by using principal components analysis, as described by Messer et al. (63). This index enabled us to account for correlated dimensions of neighborhood deprivation in adjusted models. Both residential stability and the component variables of the neighborhood deprivation index were proximity weighted in the same manner as ethnic density. We dichotomized residential stability and the neighborhood deprivation index at the birth records median; models adjusted for continuous versions of these variables produced similar estimates.
Data analysis
We modeled the relation between proximity-weighted ethnic density and preterm birth using logistic regression with Stata 10 software (Stata Corporation, College Station, Texas), with the Huber-White “sandwich” variance estimator to account for clustering at the census tract level (64), producing “population-averaged” estimates of effect (65). For comparison, we ran random-intercept models, and these “cluster-specific” results were nearly identical to the population-averaged estimates. In this paper, we present the results from population-averaged models because they estimate an average effect for the whole population rather than for a single census tract and are thus more appropriate for public health inference (66).
We computed risk differences (RDs) from the model coefficients, using intercept and variable coefficients to back-calculate from odds to risks (67). RDs provide an estimate of the number of preterm births attributable to (or prevented by) the exposure (assuming the modeled associations are valid and causal) and thus have a more direct public health interpretation than do odds ratios.
We ran separate sets of models for African-, Caribbean-, and American-born non-Hispanic black women. In all models, we included ethnic density as a continuous variable because the log odds of preterm birth was roughly linearly related to ethnic density among Africans and Caribbeans; a squared term in the US-born model accommodated a curvilinear ethnic density–preterm birth association.
First, we estimated crude associations by regressing the log odds of preterm birth among African-, Caribbean-, and US-born non-Hispanic black women on African, Caribbean, and American black densities, respectively. Second, we included individual- and contextual-level covariates. Third, we ran reduced models without prepregnancy weight because, for 7.3% of births to Caribbean women, 10.3% of births to African women, and 7.9% of births to US-born black women, data on this variable were missing. We conducted a change-in-estimate analysis, and we considered omission of prepregnancy weight worthwhile for the increase in precision and generalizability if the estimated RD changed by less than 2 preterm births per 1,000 births. Fourth, we stratified models by neighborhood deprivation because the association between ethnic density and preterm birth may depend on the resource environment also present (67, 68). Here, we present stratified results unadjusted for continuous neighborhood deprivation index because adjusting for this index within each stratum produced similar, but less precise results.
We calculated preterm birth RDs for a change from the 10th to the 90th percentiles of ethnic density for each group. The 10th and 90th percentiles of African density corresponded to 0.2% and 7.0% African, respectively; that is, 10% of black African births occurred in neighborhoods that were between 0% and 0.2% African, whereas 90% occurred in neighborhoods that were between 0% and 7.0% African (Web Figure 1a; this is the first of 2 supplementary figures also posted on the Journal’s Web site (http://aje.oupjournals.org/)). The 10th and 90th percentiles were 2.3% and 39.5%, respectively, for Caribbean density (Web Figure 1b) and 13.0% and 70.1%, respectively, for US-born density (Web Figure 1c). For the Caribbeans and US-born (the 2 higher-density groups), we also estimated RDs for an absolute change from 2% to 40% ethnic density.
RESULTS
Approximately 80% of the African births were to women originating from The Gambia, Ghana, Guinea, Ivory Coast, Mali, Nigeria, or Senegal. Forty percent of Caribbean births were to Jamaican women, 21% were to Haitian women, and 18% were to women from Trinidad.
African-born black women had low rates of preterm birth (7.5%) relative to Caribbean-born (9.9%) and US-born (11.9%) blacks. African mothers were least likely to report smoking during pregnancy (Table 1), but they were also least likely to have private health insurance. Caribbean mothers were most likely to have received at least a high school education and to live in a wealthier neighborhood, and they were less likely than US-born black mothers to have smoked during pregnancy.
Table 1.
Characteristics of African-, Caribbean-, and US-Born Non-Hispanic Black Mothers, New York City Birth Records, 1995–2003
| Characteristic | African-born |
Caribbean-born |
US-born |
||||||
| No. | % | % PTB | No. | % | % PTB | No. | % | % PTB | |
| Age, years | |||||||||
| <20 | 522 | 2 | 8 | 4,772 | 5 | 10 | 21,939 | 15 | 11 |
| 20–34 | 15,771 | 75 | 7 | 60,951 | 70 | 9 | 101,579 | 72 | 11 |
| ≥35 | 4,771 | 23 | 9 | 21,238 | 24 | 12 | 18,242 | 13 | 16 |
| Maternal education, years | |||||||||
| <12, age <20 years | 358 | 2 | 8 | 2,704 | 3 | 10 | 14,781 | 11 | 11 |
| <12, age ≥20 years | 5,729 | 28 | 7 | 12,776 | 15 | 10 | 26,709 | 19 | 14 |
| 12 | 7,297 | 35 | 8 | 35,916 | 42 | 10 | 47,669 | 34 | 12 |
| 13–15 | 3,382 | 16 | 8 | 21,846 | 25 | 10 | 36,772 | 26 | 11 |
| ≥16 | 3,796 | 18 | 7 | 12,452 | 15 | 10 | 14,089 | 10 | 10 |
| Previous births | |||||||||
| 1 | 7,336 | 35 | 8 | 36,115 | 42 | 10 | 61,404 | 43 | 11 |
| 2–5 | 13,506 | 64 | 7 | 50,036 | 58 | 10 | 77,010 | 54 | 12 |
| ≥6 | 222 | 1 | 8 | 810 | 1 | 13 | 3,336 | 2 | 19 |
| Prepregnancy weight, poundsab | |||||||||
| <125 | 2,693 | 14 | 8 | 15,518 | 19 | 10 | 25,314 | 19 | 14 |
| 125–150 | 8,077 | 43 | 7 | 31,042 | 39 | 10 | 45,132 | 35 | 11 |
| >150 | 8,109 | 43 | 8 | 34,065 | 42 | 10 | 60,104 | 46 | 10 |
| Tobacco use | |||||||||
| Nonsmoker | 20,930 | 100 | 7 | 85,581 | 99 | 10 | 127,319 | 90 | 11 |
| Smoker | 62 | 0 | 18 | 866 | 1 | 14 | 127,319 | 10 | 19 |
| Payment for delivery | |||||||||
| Private insurance | 4,891 | 24 | 8 | 30,289 | 36 | 10 | 48,872 | 35 | 10 |
| Medicaid | 14,859 | 71 | 7 | 50,553 | 60 | 10 | 86,077 | 62 | 13 |
| Self-pay | 1,045 | 5 | 11 | 3,266 | 4 | 15 | 4,472 | 3 | 18 |
| Residential stability | |||||||||
| Less stable | 11,322 | 54 | 7 | 35,503 | 41 | 10 | 52,321 | 37 | 12 |
| More stable | 9,742 | 46 | 8 | 51,458 | 59 | 10 | 89,439 | 63 | 12 |
| Neighborhood deprivation | |||||||||
| Less deprived | 6,074 | 29 | 8 | 42,396 | 49 | 10 | 41,654 | 29 | 10 |
| More deprived | 14,988 | 71 | 7 | 44,564 | 51 | 10 | 100,103 | 71 | 12 |
| Continuous neighborhood deprivationc (median, 10th, 90th percentile) | 0.63 | 0.29 | 1.58 | 0.31 | −0.26 | 0.77 | 0.76 | −0.28 | 1.63 |
Abbreviation: PTB, preterm birth.
One pound = 0.45 kg.
All variables were missing for less than 4% of observations, except prepregnancy weight (records missing for 10.4% of African-, 7.3% of Caribbean-, and 7.9% of US-born).
The neighborhood deprivation index was derived by using principal components analysis from 17 census variables and was standardized to a mean of 0 and a standard deviation of 1, with more positive numbers corresponding to greater deprivation.
Crude model results indicated that African-, Caribbean-, and US-born black densities were all associated with increased risks of preterm birth. US black density was associated with a greater increase in risk (RD = 12.5 per 1,000, 95% confidence interval (CI): 7.4, 17.6) than African (RD = 4.8 per 1,000, 95% CI: 1.0, 8.5) or Caribbean (RD = 4.3 per 1,000, 95% CI: −1.1, 9.7) densities (Table 2).
Table 2.
Preterm Birth Risk Differences for African-, Caribbean-, and US-Born Non-Hispanic Black Women Associated With Neighborhoods in the 90th Percentile of Ethnic/Immigrant Density Compared With 10th-Percentile Neighborhoods, New York City, 1995–2003
| Immigrant/Ethnic Group | Model |
|||||||
| Crude |
Adjusted |
Stratified: Less Deprived Neighborhoods |
Stratified: More Deprived Neighborhoods |
|||||
| RD | 95% CI | RDa | 95% CI | RDa | 95% CI | RDa | 95% CI | |
| African-born | 4.8 | 1.0, 8.5 | 4.8 | 2.1, 7.4 | 2.8 | −1.4, 7.0 | 6.1 | 1.9, 10.2 |
| Caribbean-born | 4.3 | −1.1, 9.7 | 1.5 | −3.2, 6.3 | −1.5 | −8.6, 5.5 | 4.4 | −1.6, 10.4 |
| US-born | 12.5 | 7.4, 17.6 | 8.1 | 3.3, 12.8 | −4.0 | −12.1, 4.2 | 12.5 | 6.6, 18.4 |
Abbreviations: CI, confidence interval; RD, risk difference.
Adjusted and stratified risk differences were calculated for women aged 20–34 years who were high school educated, had 2–5 previous livebirths, were nonsmokers, were receiving Medicaid assistance, and resided in a more stable neighborhood. Adjusted risk differences were calculated for more deprived neighborhoods.
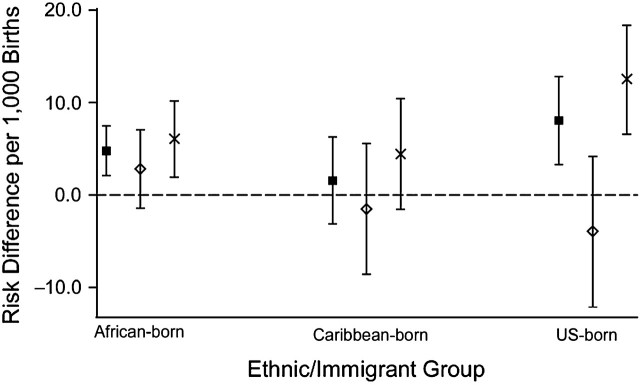
Adjustment for individual- and area-level covariates did not change the African estimate (RD = 4.8 per 1,000, 95% CI: 2.1, 7.4), but it moved the Caribbean- and US-born estimates toward the null (Caribbean RD = 1.5 per 1,000, 95% CI: −3.2, 6.3; US-born RD = 8.1 per 1,000, 95% CI: 3.3, 12.8) (Table 2, Figure 1). These RDs correspond to risk ratios of 1.08 (95% CI: 1.03, 1.13), 1.04 (95% CI: 0.97, 1.13), and 1.11 (95% CI: 1.03, 1.19) for African-, Caribbean-, and US-born non-Hispanic blacks, respectively. Final estimates were not adjusted for prepregnancy weight because its exclusion changed the RDs by less than 2 per 1,000 (refer to Web Table 3 for fully adjusted estimates).
Figure 1.
Preterm birth risk differences for African-, Caribbean-, and US-born non-Hispanic black women associated with the 90th versus the 10th percentile of ethnic/immigrant density in all New York City neighborhoods combined ( ), less deprived neighborhoods (
), less deprived neighborhoods ( ), and more deprived neighborhoods (
), and more deprived neighborhoods ( ), 1995–2003.
), 1995–2003.
The RDs estimated in less deprived neighborhoods were lower than the estimates in more deprived neighborhoods for all 3 groups (Figure 1, Table 2). Among Africans, the difference in RDs across strata was small. The difference in the RDs across strata was larger for Caribbean women, but the confidence intervals were wide and overlapping. Among US-born blacks, the effect modification was clearer: the RD in wealthier neighborhoods was −4.0 per 1,000 (95% CI: −12.1, 4.2); in poorer neighborhoods, it was 12.5 per 1,000 (95% CI: 6.6, 18.4).
Black immigrant enclaves tend to be located near US-born black populations (69), so we reran African and Caribbean models adjusting for US-born black density. Results for Africans moved toward the null; for Caribbeans, controlling for US-born black density moved estimates away from the null, but the confidence intervals widened considerably (Web Table 4).
We conducted several additional sensitivity analyses to assess the influence of certain variable and population specifications (Web Table 4; Web Figure 2). First, we excluded census tracts in which ethnic population counts were suppressed (and assumed to be zero in the main analyses). Second, we restricted the analyses to primiparous women to eliminate the influence of repeat births to the same women, which could not be otherwise accounted for. Third, we used linked hospital discharge data to identify and exclude medically indicated preterm births. Finally, we excluded women from French Guiana, Guyana, and Suriname from the Caribbean models. The findings remained largely unchanged in all supplemental analyses.
For better comparability between immigrant and US-born ethnic density effects, we calculated RDs for an absolute change from 2% to 40% own-group density for Caribbean- and US-born women (Web Table 5). African ethnic density levels were not high enough to include in this subanalysis. Adjusted RDs for US-born women (10.8 per 1,000, 95% CI: 4.5, 17.1) were substantially higher than RDs for the same contrast among Caribbean-born women (RD = 1.5, 95% CI: −3.4, 6.3), corresponding to risk ratios of 1.10 (95% CI: 1.04, 1.17) and 1.02 (95% CI: 0.96, 1.08) for US- and Caribbean-born non-Hispanic black women, respectively.
To assess the potential impact of gestation length misclassification on our results, we reran models with low-birth-weight (<2,500 g) preterm births, which are unlikely to be misclassified. Results were similar, except that African RDs were higher in less deprived neighborhoods and lower in more deprived neighborhoods.
Finally, to explore ethnic density effects by country of origin, we reran models for the 2 most prevalent African subgroups (Nigerians and Ghanaians) and Caribbean subgroups (Jamaicans and Haitians). The results indicated some differences in the ethnic density response by country of birth (Web Table 6), with Nigerians appearing to benefit from ethnic density in wealthier neighborhoods, but the results were too imprecise to provide strong support for heterogeneity across subgroups.
DISCUSSION
In this study, we found residence near high proportions of their own ethnic group to be associated with an increase in preterm birth risk for non-Hispanic black African-, Caribbean-, and US-born women, especially in more deprived neighborhoods. RDs for both relative (10th to 90th percentile) and absolute (2% to 40%) increases in ethnic density suggest that preterm birth is associated more strongly with residence in ethnically dense poor neighborhoods for US-born non-Hispanic blacks than it is for Caribbean-born non-Hispanic blacks. The same pattern was observed when we used risk ratios, indicating that the results are not dependent on scale choice. Lack of variability in African density hindered comparison of African effects with the other groups.
The distinctive results among US-born women suggest that US-born black neighborhoods, compared with black Caribbean immigrant enclaves, have a different balance of burdens and resources. Sociologists have, for example, documented ethnically based systems of resource sharing in Caribbean immigrant enclaves (69) that may counteract broader material deprivation. Ethnographic work also suggests that black immigrants perceive fewer race-based barriers to success (70) and less racism (71) than their US-born counterparts, and, similar to many immigrant groups (24), black immigrants may view their neighborhoods as a temporary step toward assimilation with whites. For US-born blacks, with accumulated experiences of race-based limitations to geographic and economic mobility (70), residence in black neighborhoods may be associated with hopelessness, depression, or other psychological determinants of physical well-being.
Contrary to theories suggesting that immigrant enclaves are health promoting (36, 37) and in contrast to the findings for Hispanics (40–43, 72–74), we did not find reduced preterm birth risks in black immigrant enclaves. Black immigrant areas, especially poor ones, may have negative characteristics that outweigh the potential benefits of cultural or ethnic cohesiveness; Hispanic cultures may, alternatively, be uniquely health protective.
Interpretation of our estimated ethnic density–preterm birth association for Africans is hindered by low African density. The most-African neighborhoods were only 7% African, a level that may not meaningfully influence the social environment, and the ethnic density–preterm birth association we measured may be a result of other neighborhood characteristics that covary with the presence of African immigrants. It is also possible, however, that segregation of Africans occurs on a smaller scale than we were able to measure (e.g., along a single street or block face). In this case, our larger-scale measure may be a diluted, but meaningful marker of African enclaves.
A major limitation of our data was lack of information on mothers’ assimilation. Highly assimilated foreign-born women may differ little from the US-born in their response to ethnic density, and their inclusion with the African and Caribbean immigrants may have prevented us from detecting protective immigrant enclave effects in the less-assimilated. We also lacked information on the timing of mothers’ residence in their neighborhoods and thus could not take into account length of neighborhood exposure, which likely differs for immigrants and the US-born. Finally, we did not have the power to obtain informative effect estimates for ethnic density based on a single country of origin, which would more closely approximate shared language and culture.
This analysis is, to our knowledge, the first to investigate health outcomes in black immigrant neighborhoods, despite recent interest in the health effects of residential segregation (75). One study found a null association between Caribbean-born non-Hispanic black body mass index and residence in foreign-born or linguistically isolated neighborhoods in New York City (76). However, the study's reliance on the percentage of all foreign-born individuals to define immigrant enclaves likely limited its ability to detect effects specific to Caribbean neighborhoods. In addition to its substantive contribution, our study used a spatial measure of ethnic density to avoid “aspatial” measures’ potential mischaracterization of geographic population distributions (77). Our results suggest that the association between ethnic density and poor birth outcomes among non-Hispanic black Caribbean immigrants is small compared with the association among US-born blacks. Similar negative responses to ethnic density may, however, emerge among black immigrants as they accumulate experiences of racial oppression (70). Further studies of black immigrants using detailed assimilation measures may help to explain the erosion of immigrant health associated with time in the United States and point to contextual and psychosocial sources of the health disadvantage experienced by the US-born black population.
Supplementary Material
Acknowledgments
Author affiliations: Department of Epidemiology, University of North Carolina, Chapel Hill, North Carolina (Susan M. Mason, Jay S. Kaufman); Carolina Population Center, University of North Carolina, Chapel Hill, North Carolina (Susan M. Mason, Jay S. Kaufman, Michael E. Emch); Department of Epidemiology, Biostatistics, and Occupational Health, McGill University, Montreal, Quebec, Canada (Jay S. Kaufman); Department of Geography, University of North Carolina, Chapel Hill, North Carolina (Michael E. Emch); Department of Maternal and Child Health, University of North Carolina, Chapel Hill, North Carolina (Vijaya K. Hogan); and Department of Community and Preventive Medicine, Mount Sinai School of Medicine, New York, New York (David A. Savitz).
This work was supported by Centers for Disease Control and Prevention Public Health Research Dissertation Grant 1R36DP001849-01.
The authors thank Dr. Julie Daniels for her contributions to the conception of this study and Dr. Teresa Janevic for her help with the neighborhood deprivation index.
This paper was awarded the 2010 Lilienfeld Student Prize by the Society for Epidemiologic Research.
Conflict of interest: none declared.
Glossary
Abbreviations
- CI
confidence interval
- RD
risk difference
References
- 1.Fiscella K. Racial disparity in infant and maternal mortality: confluence of infection, and microvascular dysfunction. Matern Child Health J. 2004;8(2):45–54. doi: 10.1023/b:maci.0000025726.53515.65. [DOI] [PubMed] [Google Scholar]
- 2.Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep. 2001;116(5):404–416. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Acevedo-Garcia D, Lochner KA, Osypuk TL, et al. Future directions in residential segregation and health research: a multilevel approach. Am J Public Health. 2003;93(2):215–221. doi: 10.2105/ajph.93.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Laveist TA. Linking residential segregation to the infant-mortality race disparity in US cities. Sociol Soc Res. 1989;73(2):90–94. [Google Scholar]
- 5.Laveist TA. Segregation, poverty, and empowerment: health consequences for African Americans. Milbank Q. 1993;71(1):41–64. [PubMed] [Google Scholar]
- 6.Peterson RD, Krivo LJ. Racial segregation, the concentration of disadvantage, and black and white homicide victimization. Sociol Forum. 1999;14(3):465–493. [Google Scholar]
- 7.Acevedo-Garcia D. Zip code-level risk factors for tuberculosis: neighborhood environment and residential segregation in New Jersey, 1985–1992. Am J Public Health. 2001;91(5):734–741. doi: 10.2105/ajph.91.5.734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chang VW. Racial residential segregation and weight status among US adults. Soc Sci Med. 2006;63(5):1289–1303. doi: 10.1016/j.socscimed.2006.03.049. [DOI] [PubMed] [Google Scholar]
- 9.Collins CA, Williams DR. Segregation and mortality: the deadly effects of racism? Sociol Forum. 1999;14(3):495–523. [Google Scholar]
- 10.Cooper RS, Kennelly JF, Durazo-Arvizu R, et al. Relationship between premature mortality and socioeconomic factors in black and white populations of US metropolitan areas. Public Health Rep. 2001;116(5):464–473. doi: 10.1093/phr/116.5.464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grady SC. Racial disparities in low birthweight and the contribution of residential segregation: a multilevel analysis. Soc Sci Med. 2006;63(12):3013–3029. doi: 10.1016/j.socscimed.2006.08.017. [DOI] [PubMed] [Google Scholar]
- 12.Hart KD, Kunitz SJ, Sell RR, et al. Metropolitan governance, residential segregation, and mortality among African Americans. Am J Public Health. 1998;88(3):434–438. doi: 10.2105/ajph.88.3.434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.LeClere FB, Rogers RG, Peters KD. Ethnicity and mortality in the United States: individual and community correlates. Soc Forces. 1997;76(1):169–198. [Google Scholar]
- 14.Polednak AP. Poverty, residential segregation, and black/white mortality ratios in urban areas. J Health Care Poor Underserved. 1993;4(4):363–373. doi: 10.1353/hpu.2010.0094. [DOI] [PubMed] [Google Scholar]
- 15.Yankauer A. The relationship of fetal and infant mortality to residential segregation: an inquiry into social epidemiology. Am Soc Rev. 1950;15(5):644–648. [Google Scholar]
- 16.Guest AM, Almgren G, Hussey JM. The ecology of race and socioeconomic distress: infant and working-age mortality in Chicago. Demography. 1998;35(1):23–34. [PubMed] [Google Scholar]
- 17.Polednak AP. Trends in US urban black infant mortality, by degree of residential segregation. Am J Public Health. 1996;86(5):723–726. doi: 10.2105/ajph.86.5.723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Polednak AP. Black-white differences in infant mortality in 38 standard metropolitan statistical areas. Am J Public Health. 1991;81(11):1480–1482. doi: 10.2105/ajph.81.11.1480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ellen IG. Is segregation bad for your health? The case of low birth weight. Brookings-Wharton Papers Urban Affairs. 2000:203–229. [Google Scholar]
- 20.Morello-Frosch R, Jesdale BM. Separate and unequal: residential segregation and estimated cancer risks associated with ambient air toxics in U.S. metropolitan areas. Environ Health Perspect. 2006;114(3):386–393. doi: 10.1289/ehp.8500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Subramanian SV, Acevedo-Garcia D, Osypuk TL. Racial residential segregation and geographic heterogeneity in black/white disparity in poor self-rated health in the US: a multilevel statistical analysis. Soc Sci Med. 2005;60(8):1667–1679. doi: 10.1016/j.socscimed.2004.08.040. [DOI] [PubMed] [Google Scholar]
- 22.White K, Borrell LN. Racial/ethnic neighborhood concentration and self-reported health in New York City. Ethn Dis. 2006;16(4):900–908. [PubMed] [Google Scholar]
- 23.Zenk SN, Schulz AJ, Israel BA, et al. Neighborhood racial composition, neighborhood poverty, and the spatial accessibility of supermarkets in metropolitan Detroit. Am J Public Health. 2005;95(4):660–667. doi: 10.2105/AJPH.2004.042150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Iceland J, Scopilliti M. Immigrant residential segregation in U.S. metropolitan areas, 1990–2000. Demography. 2008;45(1):79–94. doi: 10.1353/dem.2008.0009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Acevedo-Garcia D, Soobader MJ, Berkman LF. The differential effect of foreign-born status on low birth weight by race/ethnicity and education. Pediatrics. 2005;115(1):e20–e30. doi: 10.1542/peds.2004-1306. doi:10.1542/peds.2004-1306. [DOI] [PubMed] [Google Scholar]
- 26.David RJ, Collins JW., Jr Differing birth weight among infants of U.S.-born blacks, African-born blacks, and U.S.-born whites. N Engl J Med. 1997;337(17):1209–1214. doi: 10.1056/NEJM199710233371706. [DOI] [PubMed] [Google Scholar]
- 27.Venters H, Gany F. African immigrant health [published online ahead of print April 4, 2009] J Immigr Minor Health. doi: 10.1007/s10903-009-9243-x. (doi:10.1007/s10903-009-9243-x) [DOI] [PubMed] [Google Scholar]
- 28.Miranda J, Siddique J, Belin TR, et al. Depression prevalence in disadvantaged young black women—African and Caribbean immigrants compared to US-born African Americans. Soc Psychiatry Psychiatr Epidemiol. 2005;40(4):253–258. doi: 10.1007/s00127-005-0879-0. [DOI] [PubMed] [Google Scholar]
- 29.Williams DR, Haile R, González HM, et al. The mental health of Black Caribbean immigrants: results from the National Survey of American Life. Am J Public Health. 2007;97(1):52–59. doi: 10.2105/AJPH.2006.088211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Singh GK, Kogan MD, Yu SM. Disparities in obesity and overweight prevalence among US immigrant children and adolescents by generational status. J Community Health. 2009;34(4):271–281. doi: 10.1007/s10900-009-9148-6. [DOI] [PubMed] [Google Scholar]
- 31.Breslau J, Borges G, Hagar Y, et al. Immigration to the USA and risk for mood and anxiety disorders: variation by origin and age at immigration. Psychol Med. 2009;39(7):1117–1127. doi: 10.1017/S0033291708004698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fang J, Madhavan S, Alderman MH. Low birth weight: race and maternal nativity—impact of community income. Pediatrics. 1999;103(1):E5. doi: 10.1542/peds.103.1.e5. (doi:10.1542/peds.2004-1627) [DOI] [PubMed] [Google Scholar]
- 33.Stein CR, Savitz DA, Janevic T, et al. Maternal ethnic ancestry and adverse perinatal outcomes in New York City. Am J Obstet Gynecol. 2009;201(6) doi: 10.1016/j.ajog.2009.06.047. 584.e1–584.e9. (doi:10.1016/j.ajog.2009.06.047) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cobas JA, Balcazar H, Benin MB, et al. Acculturation and low-birthweight infants among Latino women: a reanalysis of HHANES data with structural equation models. Am J Public Health. 1996;86(3):394–396. doi: 10.2105/ajph.86.3.394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.James SA. Racial and ethnic differences in infant mortality and low birth weight. A psychosocial critique. Ann Epidemiol. 1993;3(2):130–136. doi: 10.1016/1047-2797(93)90125-n. [DOI] [PubMed] [Google Scholar]
- 36.Halpern D. Minorities and mental health. Soc Sci Med. 1993;36(5):597–607. doi: 10.1016/0277-9536(93)90056-a. [DOI] [PubMed] [Google Scholar]
- 37.Pickett KE, Wilkinson RG. People like us: ethnic group density effects on health. Ethn Health. 2008;13(4):321–334. doi: 10.1080/13557850701882928. [DOI] [PubMed] [Google Scholar]
- 38.Muhlin GL. Mental hospitalization of the foreign-born and the role of cultural isolation. Int J Soc Psychiatry. 1979;25(4):258–266. doi: 10.1177/002076407902500405. [DOI] [PubMed] [Google Scholar]
- 39.Mintz N, Schwartz DT. Urban ecology and psychosis: community factors in the incidence of schizophrenia and manic-depression among Italians in greater Boston. Int J Soc Psychiatry. 1964;10:101–118. doi: 10.1177/002076406401000202. [DOI] [PubMed] [Google Scholar]
- 40.Eschbach K, Mahnken JD, Goodwin JS. Neighborhood composition and incidence of cancer among Hispanics in the United States. Cancer. 2005;103(5):1036–1044. doi: 10.1002/cncr.20885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Eschbach K, Ostir GV, Patel KV, et al. Neighborhood context and mortality among older Mexican Americans: is there a barrio advantage? Am J Public Health. 2004;94(10):1807–1812. doi: 10.2105/ajph.94.10.1807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ostir GV, Eschbach K, Markides KS, et al. Neighbourhood composition and depressive symptoms among older Mexican Americans. J Epidemiol Community Health. 2003;57(12):987–992. doi: 10.1136/jech.57.12.987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Patel KV, Eschbach K, Rudkin LL, et al. Neighborhood context and self-rated health in older Mexican Americans. Ann Epidemiol. 2003;13(9):620–628. doi: 10.1016/S1047-2797(03)00060-7. [DOI] [PubMed] [Google Scholar]
- 44.Hogue CJ, Hargraves MA. Preterm birth in the African-American community. Semin Perinatol. 1995;19(4):255–262. doi: 10.1016/s0146-0005(05)80039-4. [DOI] [PubMed] [Google Scholar]
- 45.Dole N, Savitz DA, Siega-Riz AM, et al. Psychosocial factors and preterm birth among African American and White women in central North Carolina. Am J Public Health. 2004;94(8):1358–1365. doi: 10.2105/ajph.94.8.1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lu MC, Chen B. Racial and ethnic disparities in preterm birth: the role of stressful life events. Am J Obstet Gynecol. 2004;191(3):691–699. doi: 10.1016/j.ajog.2004.04.018. [DOI] [PubMed] [Google Scholar]
- 47.Collins JW, Jr, David RJ, Symons R, et al. Low-income African-American mothers’ perception of exposure to racial discrimination and infant birth weight. Epidemiology. 2000;11(3):337–339. doi: 10.1097/00001648-200005000-00019. [DOI] [PubMed] [Google Scholar]
- 48.Rosenberg L, Palmer JR, Wise LA, et al. Perceptions of racial discrimination and the risk of preterm birth. Epidemiology. 2002;13(6):646–652. doi: 10.1097/00001648-200211000-00008. [DOI] [PubMed] [Google Scholar]
- 49.Rini CK, Dunkel-Schetter C, Wadhwa PD, et al. Psychological adaptation and birth outcomes: the role of personal resources, stress, and sociocultural context in pregnancy. Health Psychol. 1999;18(4):333–345. doi: 10.1037//0278-6133.18.4.333. [DOI] [PubMed] [Google Scholar]
- 50.Messer LC, Kaufman JS, Dole N, et al. Neighborhood crime, deprivation, and preterm birth. Ann Epidemiol. 2006;16(6):455–462. doi: 10.1016/j.annepidem.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 51.Census 2000 Brief: Overview of Race and Hispanic Origin. 10. Washington, DC: US Census Bureau; 2001. ( http://www.census.gov/prod/2001pubs/c2kbr01-1.pdf). (Accessed August 9, 2010) [Google Scholar]
- 52.United Nations Statistics Division. Country or area & region codes: composition of regions. New York, NY: United Nations Statistics Division; (African countries: http://unstats.un.org/unsd/methods/m49/m49regin.htm#africa) (Caribbean countries: http://unstats.un.org/unsd/methods/m49/m49regin.htm#americas). (Accessed August 9, 2010) [Google Scholar]
- 53.Table G-1: New York City 1990 Census Tracts With Boundary/Number Changes for 2000 Census. New York, NY: New York City Department of City Planning; 2001. ( http://home2.nyc.gov/html/dcp/pdf/census/g1.pdf). (Accessed August 9, 2010) [Google Scholar]
- 54.US Census Bureau. Technical documentation. Washington, DC: US Census Bureau; 2000. Summary File 4: 2000 Census of Population and Housing. chapter 5, page 1. ( http://www.census.gov/prod/cen2000/doc/sf4.pdf). (Accessed August 9, 2010) [Google Scholar]
- 55.Berkowitz GS, Papiernik E. Epidemiology of preterm birth. Epidemiol Rev. 1993;15(2):414–443. doi: 10.1093/oxfordjournals.epirev.a036128. [DOI] [PubMed] [Google Scholar]
- 56.Ananth CV. Menstrual versus clinical estimate of gestational age dating in the United States: temporal trends and variability in indices of perinatal outcomes. Paediatr Perinat Epidemiol. 2007;21(suppl 2):22–30. doi: 10.1111/j.1365-3016.2007.00858.x. [DOI] [PubMed] [Google Scholar]
- 57.Joseph KS, Huang L, Liu S, et al. Reconciling the high rates of preterm and postterm birth in the United States. Obstet Gynecol. 2007;109(4):813–822. doi: 10.1097/01.AOG.0000255661.13792.c1. [DOI] [PubMed] [Google Scholar]
- 58.Reardon SF, Firebaugh G. Response: segregation and social distance: a generalized approach to segregation measurement. Sociol Methodol. 2002;32:85–101. [Google Scholar]
- 59.Reardon SF, Matthews SA, O'Sullivan D, et al. The geographic scale of metropolitan racial segregation. Demography. 2008;45(3):489–514. doi: 10.1353/dem.0.0019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Jenness Enterprises. Flagstaff, AZ: Jenness Enterprises; 2006. Polygon center of mass. ( http://www.jennessent.com/arcview/centermass.htm). (Accessed August 9, 2010) [Google Scholar]
- 61.Lee BA, Reardon SF, Firebaugh G, et al. Beyond the census tract: patterns and determinants of racial residential segregation at multiple scales. Am Sociol Rev. 2006;73(5):766–791. doi: 10.1177/000312240807300504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Behrman RE, Butler AS. Preterm Birth: Causes, Consequences, and Prevention. Washington, DC: National Academies Press; 2007. [PubMed] [Google Scholar]
- 63.Messer LC, Laraia BA, Kaufman JS, et al. The development of a standardized neighborhood deprivation index. J Urban Health. 2006;83(6):1041–1062. doi: 10.1007/s11524-006-9094-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Williams RL. A note on robust variance estimation for cluster-correlated data. Biometrics. 2000;56(2):645–646. doi: 10.1111/j.0006-341x.2000.00645.x. [DOI] [PubMed] [Google Scholar]
- 65.Kaufman JS. Re: “Appropriate assessment of neighborhood effects on individual health: integrating random and fixed effects in multilevel logistic regression” [letter] Am J Epidemiol. 2005;162(6):602–603. doi: 10.1093/aje/kwi251. [DOI] [PubMed] [Google Scholar]
- 66.Hubbard AE, Ahern J, Fleischer NL, et al. To GEE or not to GEE: comparing population average and mixed models for estimating the associations between neighborhood risk factors and health. Epidemiology. 2010;21(4):467–474. doi: 10.1097/EDE.0b013e3181caeb90. [DOI] [PubMed] [Google Scholar]
- 67.Austin PC. Absolute risk reductions, relative risks, relative risk reductions, and numbers needed to treat can be obtained from a logistic regression model. J Clin Epidemiol. 2010;63(1):2–6. doi: 10.1016/j.jclinepi.2008.11.004. [DOI] [PubMed] [Google Scholar]
- 68.Pickett KE, Collins JW, Jr, Masi CM, et al. The effects of racial density and income incongruity on pregnancy outcomes. Soc Sci Med. 2005;60(10):2229–2238. doi: 10.1016/j.socscimed.2004.10.023. [DOI] [PubMed] [Google Scholar]
- 69.Crowder KD. Residential segregation of West Indians in the New York/New Jersey metropolitan area: the roles of race and ethnicity. Int Migr Rev. 1999;33(1):79–113. [PubMed] [Google Scholar]
- 70.Benson JE. Exploring the racial identities of black immigrants in the United States. Sociol Forum. 2006;21(2):219–247. [Google Scholar]
- 71.Dominguez TP, Strong EF, Krieger N, et al. Differences in the self-reported racism experiences of US-born and foreign-born Black pregnant women. Soc Sci Med. 2009;69(2):258–265. doi: 10.1016/j.socscimed.2009.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Inagami S, Borrell LN, Wong MD, et al. Residential segregation and Latino, black and white mortality in New York City. J Urban Health. 2006;83(3):406–420. doi: 10.1007/s11524-006-9035-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Jenny AM, Schoendorf KC, Parker JD. The association between community context and mortality among Mexican-American infants. Ethn Dis. 2001;11(4):722–731. [PubMed] [Google Scholar]
- 74.Reyes-Ortiz CA, Ju H, Eschbach K, et al. Neighbourhood ethnic composition and diet among Mexican-Americans. Public Health Nutr. 2009;12(2):2293–2301. doi: 10.1017/S1368980009005047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kramer MR, Hogue CR. Is segregation bad for your health? Epidemiol Rev. 2009;31:178–194. doi: 10.1093/epirev/mxp001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Park Y, Neckerman KM, Quinn J, et al. Place of birth, duration of residence, neighborhood immigrant composition and body mass index in New York City. Int J Behav Nutr Phys Act. 2008;5:19. doi: 10.1186/1479-5868-5-19. doi:10.1186/1479-5868-5-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Reardon SF, O'Sullivan D. Measures of spatial segregation. Sociol Methodol. 2004;34:121–162. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.