Abstract
The aim of this study is to examine existing research on social cognitive factors that may, in part, mediate the relationship between socioeconomic status (SES) and coronary heart disease (CHD). We focus on how social status is ‘carried’ in the mental systems of individuals, and how these systems differentially affect CHD risk and associated behaviors. To this end, literatures documenting the association of various social cognitive factors (e.g., social comparison, perceived discrimination, and self-efficacy) with cardiovascular disease are reviewed as are literatures regarding the relationship of these factors to SES. Possible mechanisms through which social cognitions may affect health are addressed. In addition, directions for future research are discussed, and a model identifying the possible associations between social cognitive factors, SES, and coronary disease is provided.
Introduction
There is a well-established relationship between socioeconomic status (SES) and health in industrialized nations, with individuals lower in SES experiencing higher rates of morbidity and mortality than higher-SES individuals. This relationship is particularly evident in the case of coronary heart disease (CHD), the progressive narrowing of the coronary vessels manifested by angina pectoris (chest pain), myocardial infarction (MI), and coronary death (AHA, 2009). Despite the overall decline in CHD mortality over the past 30 years, CHD is the leading cause of death in the United States (CDC, 2009). Recent advancements in cardiovascular health have primarily benefitted wealthier, better-educated individuals, while progress among those of lower socioeconomic standing continues to lag (Cooper, Cutler, Desvigne-Nickens, et al., 2000; NHLBI, 1995). Variation in SES demonstrates a consistent, inverse relationship with CHD morbidity (Diez-Roux, Nieto, Tyroler, Crum, & Szklo, 1995; Rose & Marmot, 1981) and mortality (Keil, Sutherland, Knapp, & Tyroler, 1992; Seigel et al., 1987) and with CHD risk factors such as cigarette smoking (Zang & Wynder, 1998), obesity (Sobal & Stunkard, 1989) and physical inactivity (Evenson et al., 2002).
Despite this robust association, the underlying mechanisms by which social inequalities impair cardiovascular health are not well understood. These associations span multiple levels of SES and are not explained by poverty alone, illiteracy, or lack of health care resources (Adler et al., 1994), findings which have prompted researchers to identify other possible mechanisms for the SES–CHD gradient. Examinations of individual psychological attributes in relation to social health disparities have focused primarily on the influence of negative emotions (Gallo & Matthews, 2003).
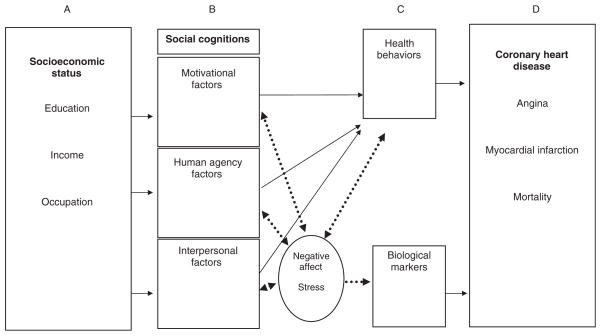
Here, we attempt to broaden the discussion of SES influences on health by suggesting a causal role for social psychological factors in the relationship between SES and CHD (see Figure 1) – particularly those related to self-perception and social perception. For example, living and working in lower SES environments may contribute to diminished self-esteem, lower sense of control, and a reduced orientation toward mastery and efficacy (Amato & Zuo, 1992; Baum, Garofalo, & Yali, 1999; McLoyd, 1998; Pearlin, Menaghan, Lieberman, & Mullan, 1981). Lower childhood SES has been associated with development of a pessimistic explanatory style (Finkelstein, Kubzansky, Capitman, & Goodman, 2007), suggesting that cognitive patterns linked to social origins may be carried throughout the life course. Accumulating evidence suggests that the influence of social standing upon these processes may impact behavioral and physiological mechanisms that, in turn, could affect cardiovascular health (Lynch, Davey Smith, Kaplan, & House, 2000; Taylor, Repetti, & Seeman, 1997).
Figure 1.
Model of social cognitive pathways through which socioeconomic status influences coronary heart disease.
Social Psychological Factors: Terminology
The field of social psychology has long been interested in how people perceive themselves, other individuals, and their social environments. Relevant terms include self-perception, social perception, social cognition, and interpersonal perception. For heuristic use, we refer here to ‘social cognitions’ as the constellation of beliefs and perceptions people hold for and about themselves and the world around them (e.g., self-efficacy, attitudes, and stereotype threat) as well as about other people in particular (e.g., norm perception, social comparison). In this study, we consider how these perceptions are related to SES and coronary disease, and more importantly, whether social cognitions could operate as mechanisms through which lower SES increases the CHD risk; i.e., whether they might mediate this association (Baron & Kenny, 1986). The factors of interest in this study are grouped according to conceptual similarity. As outlined by Moskowitz’s (2005) ‘interaction sequence’, when individuals’ negotiate the social environment, they do so through a prism of beliefs and perceptions regarding their reasons for achieving certain goals (motivations), a sense of efficacy in regard to navigating the environment, and an interpretation of the social interactions they encounter. In this study, we have adapted this ‘grouping’ of social cognitions to examine how individuals’ might negotiate the health-related sphere of their environment; specifically, how one’s motivations, one’s sense of efficacy, and one’s interpretation of social relationships might influence cardiovascular health.
Thus, the categories used throughout the article are as follows: Motivational factors are reasons to undergo improved health practices or forgo detrimental ones and include attitudes and health beliefs regarding a particular health behavior, as well as intentions to perform the behavior. (These factors are related to volitional behavior and, by definition, are addressed only within the ‘Behaviors’ section of the manuscript.) Human Agency factors refer to a sense of capacity to influence the environment, either in relation to a particular health behavior or in reference to negotiation of the broader social environment, and include perceived control, self-efficacy, and attribution. Further, social interactions and the ensuing interpretations of these interactions can serve both as facilitators and impediments of health practices and of psychological processes that may affect health, and the salient Interpersonal Factors examined here include social norms, perceived discrimination, stereotype threat, and social comparison.
Organization of the Article
In the following sections, evidence relating social cognitions to (i) coronary disease outcomes, (ii) biological risk markers, and (iii) CHD-related risk behaviors is reviewed. In each section, evidence linking SES to the specific social cognitive factors of interest in that section (Columns A and B, Figure 1) is presented. Next, studies relating those factors to coronary disease outcomes, biological risk markers, or behaviors are discussed (Columns B and C/D, Figure 1).
Social Cognitions and Coronary Disease Outcomes
Substantial evidence links socioeconomic position with coronary morbidity and mortality (Diez-Roux et al., 1995; Keil et al., 1992; Rose & Marmot, 1981; Seigel et al., 1987). This section reviews research linking social cognitions with specific coronary disease outcomes (i.e., angina, MI, and coronary mortality), a body of work which has focused primarily on human agency factors. The theoretical basis for, and evidence supporting, a relation between SES and human agency is discussed first. Next, the evidence documenting positive associations between agentic factors and CHD is reviewed. Finally, the three studies that have examined SES, social cognitions, and CHD outcomes within a single model are presented and are summarized in Table 1.
Table 1.
Studies examining social cognitive variables in relation to socioeconomic status (SES) and coronary heart disease (CHD) outcomes
| SC variable | Author/date | Subjects | SES outcome | CHD outcome | Results |
|---|---|---|---|---|---|
| Human agency | |||||
| Control Pearlin and Schooler’s mastery scale and measure of ‘general’ self-efficacy (When trying to learn new things I usually give up if I’m not initially successful) |
Bosma et al. (2005) | 3888 older adults from GLAS study (Netherlands) Prospective (5 year f/u) cohort study |
SES index of combined education, occupation, and income | Acute MI | HRs for MI in medium/low SES groups decreased by 4% when contr. for classic risk fx, 30% for low general control beliefs (SES effects on AMI lost significance) |
| Control | Marmot et al. (1997) | Whitehall II cohort | Civil service grade | Adult mortality | Higher childhood SES = higher levels of perceived control in adulthood, perceived control sig. mediated association of SES w/later mortality |
| Control | Chandola et al. (2004) | Whitehall II phases 3–5, 7470 males and females | Civil service grade ‘Household position’ = presence of financial problems, difficulty paying bills, etc. | Fatal CHD, non-fatal MI | Low control at home predicted CHD among women but not men. Women – low SES predicted CHD (HR = 2.7). HR significantly reduced after adjusting for control (HR = 2.5) and risk fx |
MI, myocardial infarction.
Self-efficacy and control
Marxist theories of social class and alienated labor have focused on how the nature of work affects self-efficacy (Gecas, 1989), suggesting that prolonged lack of control is inherent to lower social status (Mirowsky & Ross, 1983). Education (Aalto et al., 2007; Cohen, Kaplan, & Salonen, 1999), income (Cohen et al., 1999; Lachman & Weaver, 1998), and occupation (Bosma, Schrijvers, & Mackenbach, 1999; Chandola, Kuper, Singh-Manoux, Bartley, & Marmot, 2004; Marmot, Bosma, Hemingway, Brunner, & Stansfield, 1997) are related to mastery and personal control as are measures combining socioeconomic indices (Bosma et al., 1999, 2005; Marmot et al., 1997). SES has generally shown positive relations with self-efficacy (Ribisl, Winkleby, Fortmann, & Flora, 1998; Winkleby, Flora, & Kraemer, 1994) and self-esteem (Twenge & Campbell, 2002). According to the ‘job strain’ model of psychosocial work characteristics (Karasek, 1979), coronary risk is heightened by the distress resulting from an imbalance between workers’ low control and high conflicting task demands. Lack of occupational control has been consistently associated with CHD risk (see reviews by Hemingway & Marmot, 1998 and Schnall & Landsbergis, 1994), and higher control outside the workplace has been linked to lower incidence of CHD (Bosma et al., 2005).
In contrast, having a stronger belief in personal control has also been related to greater coronary atherosclerosis in adults undergoing angiography (Seeman, 1991). This finding may reflect participants’ unrealistic expectations of control (Taylor & Seeman, 1999) or hostile tendencies, which are associated with increased coronary risk (Barefoot, Dahlstrom, & Williams, 1983; Dembroski, MacDougall, Costa, & Grandits, 1989). The locus of control (LOC) construct has yielded inconsistent results when examining recovery from coronary events. In one investigation, patients recovering from acute MI who were classified as having an internal control locus demonstrated better prognoses than those reporting external control perceptions (Cromwell, Butterfield, Brayfield, & Curry, 1977), while Flowers (1994) found no such association for cardiac patients.
Attributions
Attributional or explanatory style (Abramson, Seligman, & Teasdale, 1978) adds to the LOC concept of internality–externality by including the dimensions of stability–instability and globality–specificity (i.e. whether attributions are maintained across time/in varied situations). Considering the imbalance between resources and demands in low-SES environments, pessimistic attributions (tendencies toward expecting negative outcomes for future events) may be activated more frequently and with greater magnitude in lower-SES individuals (Grewen et al., 2000). Kohn and Schooler (1982) report positive associations between SES and optimism, while Taylor and Seeman (1999) show negative outcome expectations (pessimism) to relate to low SES. Low occupational status is correlated with ‘fatalistic’ causal perceptions (i.e., emphasis of environmental rather than personal causation of behavior) (Wheaton, 1980). Optimism covaries positively with educational attainment (Giltay, Geleijnse, Zitman, Hoekstra, & Schouten, 2004; Radcliffe & Klein, 2002), whereas pessimistic explanatory style is inversely related to education (Kubzansky, Sparrow, Vokonas, & Kawachi, 2001).
In regard to CHD, Kubzansky et al. (2001) demonstrated that veterans’ optimistic explanatory style predicted lower risk of angina, nonfatal MI, and fatal CHD. In two separate studies of older Dutch persons, optimism was found to have a protective effect against CHD mortality (Giltay, Kamphuis, Kalmijn, Zitman, & Kromhout, 2006; Giltay et al., 2004).
Mediating social cognitions
The three studies investigating social cognitions as mediators between SES and CHD outcomes have focused on perceived control (Table 1). In one analysis of 5-year CHD incidence from the Whitehall II study of British civil servants, Marmot et al. (1997) examined the contribution of control perceptions to disease risk. Compared with those in the highest occupational grade, those in the lowest grade had significantly higher age-adjusted odds ratio of developing new CHD, and adjustment for perceived control provided the largest contribution to reducing the odds ratios for newly reported CHD in the lowest grade. Results from a second Whitehall II study indicated that low control at home predicted CHD among women, but not among men. Furthermore, adjustment for control accounted for a significant portion of the relation between household social position and women’s CHD risk (Chandola et al., 2004). In a third, population-based prospective investigation, incident heart disease (acute MI) at 5 years was recorded in middle- and older-aged participants without baseline heart disease. As expected, low SES predicted higher risk of CHD (Bosma et al., 2005), and adjustment for control beliefs and coronary risk factors (e.g. smoking, hypertension) showed control to account for substantially greater variance in coronary risk (30%) than did traditional risk factors (4%).
In sum, human agency factors such as self-efficacy, control beliefs, and attributional style have been related both to coronary disease outcomes and to indices of socioeconomic position. Further, perceived control appears to play a mediational role in the relation between SES and CHD. Conceivably, coronary risk in lower SES individuals may be heightened, in part, by the inherent distress of having relatively little control over demanding social and economic environments.
Social Cognitions and Biological Risk Markers
In addition to coronary disease morbidity and mortality, several ‘preclinical’ indicators of CHD have been related to socioeconomic position. Exaggerated cardiovascular reactivity, defined as physiologic responses to a psychological or physical stressor (Manuck, Kasprowicz, Monroe, Larkin, & Kaplan, 1989), has been implicated in the development of hypertension (Treiber et al., 2003), and research demonstrates inverse relationships between SES and both blood pressure (Sorel, Ragland, Syme, & Davis, 1992; Vargas, Ingram, & Gillum, 2000) and cardiovascular reactivity (Gump, Matthews, & Räikkönen, 1999; Lynch, Everson, Kaplan, Salonen, & Salonen, 1998). Significant inverse relations between SES and triglycerides (Brunner et al., 1997), plasma glucose concentrations (Brunner et al., 1997; Ko et al., 2001), and the metabolic syndrome (Brunner et al., 1997; Lawlor, Ebrahim, & Davey Smith, 2002; Park et al., 2003) have also been documented. As described previously (see ‘CHD Outcomes’ section), evidence supports an association between social standing and self-efficacy. Similarly, SES has been associated with interpersonal social cognitive factors which, in turn, are related to several biological markers of coronary risk. These relationships are discussed later, as are the three studies that have examined SES, social cognitions, and preclinical disease markers within a single model (summarized in Table 2).
Table 2.
Studies examining social cognitive variables in relation to socioeconomic status (SES) and coronary heart disease-related biological risk markers
| SC variable | Author/date | Subjects | SES outcome | Biological marker | Results |
|---|---|---|---|---|---|
| Human agency | |||||
| Attributional style measured by ASQ | Grewen et al. (2000) | 37 postmenopausal females (39–64 years) No HRT |
Composite of income, educ, and race to create ‘social disadvantage’ score | Blood pressure | Mean comparisons – low SES/high pessimism women = higher SBP |
| Interpersonal | |||||
| Threat perception Controlling for anger did not account sig for SES effects on SBP reactivity |
Chen and Matthews (2001) | 201 (50% AA/50%CA) children (8–10 years) and adolescents (15–17 years) Prospective study – lab sessions 3 years apart |
Family SES, paternal SES (Hollingshead) (subst maternal SES if no father in home) | CV reactivity (BP, HR, cardiac output, total peripheral resistance) Time 1 CVR controlled for at Time 2 |
Low SES assoc. w/higher TPR reactivity and > perceptions of hostile intent. Cog bias mediated relationship in low SES AAs |
| Threat perception | Chen et al. (2004) | 47 AA and 53 CA male and female adolescents Interviews and lab stressors + BP/HR measured (cross sectional) |
Family SES, paternal SES (Hollingshead) | CV reactivity (BP, HR) | Lower SES assoc. w/> threat appraisals to neutral events, which mediated associations w/DBP and HR 2 tests of mediation |
Self-efficacy
Cardiovascular reactivity is inversely related to subjects’ task-specific self-efficacy (Bandura, Reese, & Adams, 1982). Autonomic nervous system (ANS) activation plays an influential role in the pathophysiology of cardiovascular disease (Corti et al., 2000), and catecholamine reactivity (a measure of ANS activation) has been inversely related to performance self-efficacy on stressful tasks (Bandura, Taylor, Williams, Mefford, & Barchas, 1985; Gerin, Litt, Deich, & Pickering, 1996; Wright & Dismukes, 1995).
Social comparison
When asked to compare themselves with others in a society, individuals of lower occupational status, less education, and lower incomes rank themselves as lower in social standing (Adler, Epel, Castellazzo, & Ickovics, 2000; Gianaros et al., 2007; Singh-Manoux et al., 2005), and a frequently cited correlate of low SES is the distress or demoralization stemming from this form of ‘upward’ social comparison (Wilkinson, 1999). Consistent with this, adverse cardiovascular responses, including increased ventricular contractility and vasoconstriction, have been related to engagement in upward social comparison (Mendes, Blascovich, Major, & Seery, 2001). Evidence of socioeconomic variation in health outcomes even among those who are not materially disadvantaged has prompted the examination of relative social standing in SES-related variability in disease risk (Marmot & Wilkinson, 1999; Wilkinson, 1999). One measure of perceived social ranking, termed subjective SES, asks individuals to engage in a form of social comparison by indicating their standing in relation to others on a visual ‘ladder’ of ascending SES (Adler et al., 2000). People reporting lower subjective SES exhibit several physiological risk factors for CHD, including higher central adiposity (Adler et al., 2000), higher BMI (Goodman et al., 2001, 2003), a more pronounced rise in morning cortisol (Wright & Steptoe, 2005), greater adrenocortical responses to stress (Adler et al., 2000), and higher basal heart rate (Adler et al., 2000).
Stereotype threat and perceived discrimination
Steele and colleagues (Steele & Aronson, 1995; Steele, Spencer, & Aronson, 2002) have demonstrated the concept of stereotype threat, or the fear that one’s behavior will confirm the existing stereotype of one’s identified group. Although most research on stereotyping has examined categories based on racial categorization, class-based stereotypes have been documented (Feldman & Hilterman, 1974; Weeks & Lupfer, 2004). Because students from lower SES families generally perform worse on tests of intellectual ability (Neisser et al., 1996), the concept of stereotype threat has been proposed to contribute to differences in scholastic achievement between high- and low-SES individuals. After inducing stereotype threat for low SES (by citing poor performance in low SES students on standardized tests), Croizet and Claire (1998) found that SES was inversely related to performance when a test was presented as a measure of verbal ability, despite equal performance between groups when no mention of intellectual function was included. Similarly, another sample of lower-income students performed worse than their high-SES counterparts on an academic test when an SES-based stereotype threat was activated (Harrison, Stevens, Monty, & Coakley, 2006.
The activation of stereotype threat may heighten stress in stereotyped group members, bringing about alterations in neurobiological systems. Although no studies have yet investigated physiological correlates of stereotype threat in reference to SES, African Americans under stereotype threat have been found to exhibit larger blood pressure increases during academic tests (Blascovich, Spencer, Quinn, & Steele, 2001).
Another consequence of social class stereotyping may be the perception of SES-related discrimination. However, despite documented negative beliefs relevant to social standing, such as perceptions of low-SES individuals as being lazy (Leahy, 1981), dishonest (Desmond, Price, & Eoff, 1989), and uninterested in education (Bullock, 1999), few investigations have included a measure of mistreatment on the basis of income level. In one study, low-SES patients reported higher rates of being discriminated against by health care providers, an effect that was independent of subjects’ race (Trivedi & Ayanian, 2006). Although several investigations among the US African American population document links between self-reported experiences of discrimination and elevated blood pressure (see review by Brondolo, Rieppi, Kelly, & Gerin, 2003), no studies of class-based discrimination have included a measure of CHD-related risk.
Mediating social cognitions
A small number of investigations have addressed the influence of socioeconomic position on biological markers of coronary disease risk via interpersonal social cognitions (Table 2). Although they did not explicitly examine the mediational role of pessimism in the SES–CHD relationship, Grewen et al. (2000) showed that low-SES/high-pessimism women had significantly higher systolic blood pressure than women in three other groups (high SES/low pessimism, high SES/high pessimism, and low SES/low pessimism), demonstrating that the combination of lower social status and negative expectations regarding future events may enhance CHD risk. More direct evidence comes from two studies that tested cognitive appraisal biases among adolescents of diverse socioeconomic position (Chen, Langer, Raphaelson, & Matthews, 2004; Chen & Matthews, 2001). In these investigations, lower-SES participants displayed greater perceptions of hostile intent and threat appraisals to neutral events, and these cognitions mediated associations between social standing and total peripheral resistance, heart rate, and diastolic blood pressure reactivity in the lower-SES individuals. The authors concluded that, although SES contributed only a small portion of the variance in cardiovascular reactivity, cognitive appraisal biases explained a substantial portion of SES effects.
Altogether, these results suggest that individuals’ cognitions regarding their social environment may influence coronary disease risk, perhaps through stress-related physiological responses (see Figure 1). Several social cognitive factors, including self-efficacy, social comparison processes, and perceived discrimination, have been related to measures of social status. Similarly, these factors have been related to various ‘preclinical’ indicators of CHD, such as higher blood pressure, heart rate, and central adiposity. In addition, preliminary evidence demonstrates a mediational role for cognitions (specifically cognitive appraisal biases) in the association between SES and CHD risk indicators.
Social Cognitions and CHD-related Behaviors
Consistent evidence links physical inactivity, poor diet, and smoking with CHD (American Heart Association, 2009; Wannamethee, Whincup, Shaper, & Walker, 1996), behaviors which have also been associated with social standing. The prevalence of cigarette smoking increases at successively lower levels of SES (Zang & Wynder, 1998), and direct associations have been found between physical activity levels and SES (Ford et al., 1991; Evenson et al., 2002). This section reviews research linking SES, social cognitions, and CHD-related behaviors (see Figure 1). This body of work has focused largely on motivational factors; thus, the theoretical basis for, and evidence supporting, a relation between SES and motivational factors is discussed first. Next, evidence documenting associations between social cognition and behavior is reviewed. Finally, the nine studies that have examined SES, social cognitions, and CHD-related behavior within a single study are presented and summarized in Table 3.
Table 3.
Studies examining social cognitive variables in relation to socioeconomic status (SES) and coronary heart disease (CHD)-related health behaviors
| SC variable | Author/date | Subjects | SES outcome | Behavior | Results |
|---|---|---|---|---|---|
| Motivational | |||||
| Attitudes (‘important to me’) | Steptoe and Wardle (1999) | 374 females, 290 males Postal survey, South London |
Education (low vs. high) | Dietary intake | Controlling for dietary attitudes reduced effect of higher education on better dietary habits to non-significance |
| Attitudes | Wardle and Griffith (2001) | 1894 males and female participants Omnibus survey, Great Britain |
Civil Service Grade | Weight control practices | Higher SES = more concerned about weight– led to weight control, perhaps leading to lower BMIs |
| Attitudes | Seccareccia et al. (1991) | 6074 Italian males 46 y.o. Postal survey |
Occupation | Smoking, physical activity, diet, blood pressure and cholesterol checks | Highest of 3 SES groups held most favorable health attitudes, smoked less, reported most leisure PA, and had BP and cholesterol checks most frequently |
| Intentions (‘motivation to change’) | Ribisl et al. (1998) | 243 Hispanic, 1786 white males (25–64 years) Stanford Five City Project, cross sectional survey |
Education | Framingham risk score (combination of age, cig/day, total cholesterol, SBP, BMI) | Lower Ed = lower change intentions, higher CVD risk Did not test for mediation |
| Human agency | |||||
| Self-efficacy | Winkleby et al. (1994) | 221 females/190 males (25–74 years) Stanford Five City Project Baseline + prospective 6 year follow up survey |
Education | Framingham risk score (combination of age, cig/day, total cholesterol, SBP, BMI) | Low SES group = lowest self-efficacy scores, lowest CHD change scores – not a mediation model |
| Self-efficacy | Ribisl et al. (1998) | 243 Hispanic, 1786 White males (25–64 years) Stanford Five City Project, cross sectional survey |
Education | Framingham risk score (combination of age, cig/day, total cholesterol, SBP, BMI) | Lower Ed = lower Self-efficacy, and higher CVD risk, but did not test for mediation |
| Self-efficacy | Manfredi et al. (2007) | 644 female smokers Path analysis examining mediators of education-smoking behavior |
Education | Smoking | Self-efficacy did not directly influence quit attempts in low SES women |
| Interpersonal | |||||
| Social norms | Manfredi et al. (1992) | 256 female smokers (18–39 years) Evaluation of a smoking cessation intervention, baseline telephone interviews |
Education | Smoking cessation | Higher ed. predictive of living in ‘cessation supporting environments’ w/fewer smokers |
| Social norms | Manfredi et al. (2007) | 644 female smokers Path analysis examining mediators of education-smoking behavior |
Education | Smoking | Social pressure to quit mediated effects of education on attempts to quit |
Motivational factors
Many standard predictors of health behaviors in models like the Theory of Planned Behavior (Ajzen, 1991), which aims to explain and predict a variety of voluntary behaviors, characterize motivations for adopting health behaviors. Attitudes (positive or negative evaluations) toward healthy behavior predict consumption of low-fat food (Armitage & Conner, 2001; Paisley & Sparks, 1998), physical activity (Courneya, Friedenreich, Arthur, & Bobick, 1999; Trafimow & Trafimow, 1998), and smoking behavior (Morrison, Gillmore, Simpson, & Wells, 1996; Norman, Conner, & Bell, 1999). Attitudes may be determined, in part, by beliefs regarding the consequences of a behavior, termed outcome expectancies. Direct relations between outcome expectancies and exercise behavior have been found in many (though not all) studies (e.g., Dzewaltowski, Noble, & Shaw, 1990; Resnick, Orwig, Magaziner, & Wynne, 2002; Rovniak, Anderson, Winett, & Stephens, 2002). Beliefs regarding how lifestyle habits affect health, combined with attitudes toward health behaviors, motivate individuals to implement changes. Behavioral intentions indicate the degree to which one has formulated conscious plans to perform a behavior (Warshaw & Davis, 1985). Evidence supports an association between intention and actual performance of physical activity (Hausenblas, Carron, & Mack, 1997) and smoking (Hanson, 1999; O’Callaghan, Callan, & Baglioni, 1999).
Participants with fewer years of education report less favorable attitudes toward engagement in healthy behavior (Winkleby et al., 1994), and education is positively associated with intention to reduce CHD risk (Ribisl et al., 1998). Wardle, Waller, and Rapoport (2001), Wardle and Steptoe (2003) report more positive attitudes toward maintaining a healthy weight in British civil servants of higher occupational grade and found that lower grade predicted less ‘health consciousness’ and less concern for the future. Manfredi, Lacey, Warnecke, and Buis (1992) examined female smokers’ beliefs about the health risks of smoking, and found that low-SES women are less concerned about smoking-related risks (i.e. cancer, heart disease) than higher-SES women.
Human agency
As described previously (see ‘CHD Outcomes’ section), evidence supports an association between social standing and human agency factors, and a similar relationship has been documented for these factors and specific health behaviors. For example, internal LOC was related to the performance of a higher number of health behaviors in a sample of over 11,000 adults (Norman, Bennett, Smith, & Murphy, 1998) and has been associated with higher physical activity (Sonstroem & Walker, 1973) and a healthier diet (Bennett, Moore, Smith, Murphy, & Smith, 1995). Some evidence suggests that ‘internals’ are more likely to reduce (Best & Steffy, 1971) or stop smoking (James, Woodruff, & Werner, 1965), whereas other research shows no relationship between LOC and cessation (Brod & Hall, 1984; Carlisle-Frank, 1991). Low self-efficacy ratings predict smoking initiation (Conrad et al., 1992), while high self-efficacy is related to smoking cessation (Barrios & Niehaus, 1985; Carey, Snel, Carey, & Richards, 1989; Coletti, Supnick, & Payne, 1985; Mudde, de Vries, & Dolders, 1995).
Higher self-efficacy is also associated with successful weight loss attempts (Chambliss & Murray, 1979; Weinberg, Hughes, Critelli, England, & Jackson, 1984) weight loss maintenance (Blair, Booth, Lewis, & Wainwright, 1989), and initiation and maintenance of exercise programs (e.g., Brawley & Rogers, 1993; Dzewaltowski et al., 1990; McAuley & Courneya, 1993; Poag-DuCharme & Brawley, 1993). Higher self-efficacy scores are associated with better self monitoring of blood glucose, better diet, and higher physical activity in patients with diabetes (Sarkar, Fisher, & Schillinger, 2006), and some (though not all) self-efficacy interventions have been shown to enhance diabetes management (Corbett, 1999). The single study relating coronary risk behavior and attributional style showed that internal explanatory style for negative events (i.e. ‘self-blame’) predicted a lapse in dietary restriction during weight loss attempts (Ogden & Wardle, 1990).
Interpersonal factors
Subjective norms are a subset of beliefs indicative of the desire to comply with social norms, either to avoid rejection and criticism or to receive gratification from others. Social norms are thought to provide a context in which an individual makes health-relevant decisions (Emmons, Barbeau, Gutheil, Stryker, & Stoddard, 2007). Christakis and Fowler’s (2007) examination of social influences on obesity found that a person’s chances of becoming obese increased significantly if one had an obese friend, sibling, or spouse, regardless of geographic separation. The authors suggest that having obese social contacts may change a person’s tolerance for becoming obese and may, in turn, influence his or her adoption of specific consumption or activity patterns. Thus, although the strength of social norms has not been explicitly examined in relation to SES, the accepted behavioral norms of one’s home, workplace, or community (i.e., indices of socioeconomic position) will likely influence individual health behavior. In adolescent boys (Trost, Pate, Ward, Saunders, & Riner, 1999) and college students (Okun et al., 2003), ratings of significant others’ value of physical activity are positively associated with participants’ own activity levels, and seeing physically active community members is related to exercise among African American women (Ainsworth et al., 2003; King et al., 2000). Emmons et al. (2007) found that those whose family and friends ate more fruit and vegetables and exercised daily demonstrated more favorable dietary and physical activity scores.
Perception of the favorability of other people’s behavior also appears to influence one’s own actions. The Prototype/Willingness Model for risk behavior (Gibbons & Gerrard, 1995) assumes that people maintain images of the type of person who engages in a particular behavior, with more favorable images (smokers are rebellious and cool) resulting in increased willingness to engage in the behavior. The model has been effective in predicting willingness to engage in smoking behavior; as participants’ ratings of the ‘typical smoker’ image became more favorable, smoking behavior increased, and vice-versa (Thornton, Gibbons, & Gerrard, 2002). Because smoking is substantially more common in low-SES individuals (Zang & Wynder, 1998), more frequent exposure to smokers within one’s social network may play a role in increasing the favorability of smokers’ images in low-SES environments.
Social comparisons play an influential role in how people judge their own disease risk (Klein & Weinstein, 1997), and comparisons with ‘the average person’ have been associated with behavioral intentions (Klein, 2002). Because higher education has been associated with better CHD-related knowledge (Gans, Assmann, Sallar, & Lasater, 1999), higher-SES individuals may be more accurate judges of CHD risk than those of lower-social status. Higher perceived risk has been related to both desire to engage in CHD risk reducing behaviors and actual dietary and smoking behavior change (Silagy, Muir, Coulter, Thorogood, & Roe, 1993; Winkleby et al., 1994). The related phenomenon of unrealistic optimism (optimistic bias) is the belief that one is at less risk for negative health events than are others. Smokers, for instance, report a belief that the risk of smoking-related diseases applies more to other smokers than to themselves (Weinstein, 1998), and optimistically biased individuals exhibit higher rates of smoking (Strecher, Kreuter, & Kobrin, 1995). The one study that examined risk perception in the context of cardiovascular disease found that unrealistically optimistic individuals exhibited higher systolic blood pressure and higher serum cholesterol (Radcliffe & Klein, 2002).
Mediating social cognitions
Despite numerous investigations linking social cognitive factors with health behavior, only nine studies were found which included measures of both socioeconomic position and CHD-related health behaviors along with relevant social cognitions (Table 3). Steptoe and Wardle (1999) examined relations of educational attainment and attitudes toward dietary habits in a cross-sectional population survey. After dividing the sample into low-and high-SES groups, adjustment for attitudes toward food in a logistic regression analysis reduced the odds ratio for having a high-fiber diet to nonsignificance, suggesting that educational influences on diet are largely accounted for by attitudes. Consistent with data showing that people of lower SES, despite generally higher body mass, tend to be more satisfied with their body size than people of higher SES (Lynch et al., 2007; McLaren & Kuh, 2004; Wardle et al., 2001), Wardle and Griffith’s (2001) British survey of weight attitudes found that those with higher civil service grades held stronger weight concerns (despite having lower body mass than those in lower social classes) and were more likely to participate in weight control practices. Another survey of health practices in a group of over 6000 Italian men showed that, along with holding more favorable attitudes, the highest SES groups smoked less, reported more physical activity, and attended blood pressure and cholesterol screenings more frequently than those in lower occupational grades (Seccareccia, Menotti, & Prati, 1991). Similarly, Ribisl et al. (1998) showed an inverse association between education and cardiovascular risk scores, while intention to alter risk was directly related to educational attainment.
Using data from the Stanford Five-City project, two studies examined self-efficacy in relation to coronary disease risk behavior scores, though neither directly tested for mediation. In the first, education was positively associated with self-efficacy scores and inversely related to change in CHD risk scores over 6 years (Winkleby et al., 1994). A later cross-sectional survey similarly documented low self-efficacy in those with less education, along with higher coronary risk scores (Ribisl et al., 1998). The one study to test for mediation of a health behavior via human agency factors showed that self-efficacy did not mediate the relation between smokers’ educational attainment and cessation attempts (Manfredi, Cho, Crittenden, & Dolecek, 2007). In the two studies exploring interpersonal factors, Manfredi et al. (1992, 2007) theorized that, because smoking is more prevalent in low-SES groups, it may be a valued part of lifestyle among low-SES individuals and that, owing to weaker ‘quitting’ norms, low-SES women may be less motivated to quit. Results supported the authors’ claim in both studies, showing that more highly educated women smokers lived in environments more supportive of quitting and this social pressure to quit mediated the effects of education on cessation.
Overall, substantial evidence demonstrates an association between social status and CHD-related behavioral risk factors such as physical inactivity, poor diet, and smoking. Moreover, these health-impairing practices have been related to social cognitions (primarily motivational factors), although data supporting a mediating role for these factors in the relationship between SES and CHD risk behavior is limited. Further research is needed in this area and may benefit from inclusion of more well-defined health behavioral outcomes, as well as from more standardized measures for motivational factors across studies.
Summary
Overall, the moderate but growing evidence base to date supports a role for social cognitions in the relationship between socioeconomic position and risk of CHD (Figure 1). Fifteen studies indirectly or directly addressed social cognitions as mediators of the SES-health gradient. Although the majority of studies examining links between both social status and social cognition with CHD and health-relevant behaviors were correlational in nature and did not explicitly test for mediation, those that did utilize more sophisticated analytical techniques demonstrated evidence for a causal role of social cognitive factors, specifically for control and threat perceptions, in the SES–CHD gradient. The fact that independent effects for these cognitive factors were shown after adjusting for behavioral risk factors (Bosma et al., 2005) further strengthens this assertion, given that behavior serves as a potentially key mediator of the SES–CHD relationship.
Despite evidence supporting a role for social cognitive factors in the development of coronary disease, several limitations were evident in this body of research. In the case of motivational factors, intention may be a useful predictor of future health behavior, but because studies often do not measure individuals’ intentions close in time to the observed behavior, the changing nature of intentions over time may limit predictive power (Sutton, 1998). Also, considering some individuals’ tendencies toward internal control beliefs in some circumstances (e.g., career goals) but externality regarding a target health behavior (e.g., weight management), a unidimensional and generalized scale of perceived control may fail to detect such distinctions (Carlisle-Frank, 1991).
Another potential limitation is the lack of standard self-efficacy measures, and the fact that many investigations employ study-specific self-efficacy questionnaires (Coletti et al., 1985; DiClemente, 1981; DiClemente, Fairhurst, & Piotrowski, 1995). Further, most investigations utilized questionnaires and survey techniques, and the primarily cross-sectional analyses prohibit causal inferences, both for the associated SES and CHD outcomes as well as for cognitive concepts and behavioral and physiological factors (Weinstein, Rothman, & Sutton, 1998). Results support continued exploration of the role of social cognitions in the SES–CHD relationship via prospective study designs, and novel concepts such as stereotype threat and cognitive biases bear much more investigation. Finally, inclusion of more well-defined health outcomes, particularly in the health behavior realm, is encouraged as a parallel to the growing sophistication of physiological measurement techniques (e.g. ambulatory blood pressure monitoring).
Future research on social cognitions that have not yet been applied to SES is encouraged. Possible directions include examinations of relationship perceptions (beliefs about marriage partner, which could be affected by SES and in turn affect behavior) and perceived norms about the value of good health vis-á-vis other goals. More comprehensive assessment of SES, either on an individual (wealth, subjective SES) or community level, is also essential. Also, considering that most investigations were conducted with ethnically and racially limited university populations, future studies should include more heterogenous samples and should specifically examine gender or racial differences. The association of social status with health appears to be particularly strong among African Americans and women, for whom the burden of discrimination may be more powerful (Adler et al., 1994), underscoring the importance of disentangling the multiple effects of social class, gender, and ethnicity.
Although the aim here has been to present evidence for a causal role of social cognitive factors in the SES–CHD relationship, alternate explanations for the sequential nature of these associations exist. Poorer cardiovascular health may influence social status via vascular impairments in higher-order brain function (Haley et al., 2007), which could, in turn, diminish opportunities for educational and occupational attainment. However, evidence for the ‘social drift’ hypothesis of the SES–health relationship is relatively scarce (Adler et al., 1994). A second explanation suggests that the link between SES and health represents a spurious association stemming from the relationships of both social status and health outcomes to underlying genetic vulnerabilities. These genetic factors may similarly influence cognitive processes, resulting in associations among SES, health, and cognitions which appear to be causally linked but are, in reality, unrelated. The most likely explanation for the inverse relationship of SES with cardiovascular risk lies in a complex interaction of genes, environment, and behavior. This is clearly an important area of future research.
If social cognitions serve merely as bridges to emotional factors, these affective experiences may be the ‘true’ mediators. Hostility, a disposition reflecting anger proneness and a distrustful view of others (Barefoot, Dodge, Peterson, Dahlstrom, & Williams, 1989), is predictive of CHD (Barefoot et al., 1983; Dembroski et al., 1989) and has been inversely related to SES (Barefoot, Peterson, Dahlström, & Williams, 1991; Scherwitz, Perkins, Chesney, & Hughes, 1991). Depression has also been linked with acute coronary events (Rosengren et al., 2004) and has been hypothesized to contribute to variation in SES–health disparities (Anderson & Armstead, 1995; Wilkinson, 1997). However, some evidence suggests an independent role for cognitions in the development of coronary disease. The protective effect of optimism against CHD demonstrated by Kubzansky et al. (2001) was not reduced upon adjustment for anger and hostility. Chen and Matthews (2001) examined both cognitive appraisals and anger as pathways from low SES to higher cardiovascular reactivity and showed an effect of threat appraisal above and beyond anger. It is possible that additional emotional factors that have not been examined, such as anxiety, may account for the observed associations between cognitive factors and disease. More likely, it is the interplay of cognitive and affective dimensions of psychological functioning (Forgas, 2001) which influences physical well-being (Salovey, Detweiler, Steward, & Bedell, 2001).
Interventions
The challenge of addressing socioeconomic disparities in health remains a prominent theme in public health research, and varied approaches for reducing disparities have been proposed. Recent work emphasizes promoting cleaner and safer living environments (Vlahov & Galea, 2002), improving access to quality care for disadvantaged groups (Weech-Maldonado, Dreachslin, & Dansky, 2002), and reducing societal income inequalities (Kaplan, 2000). Relevant to the present review, educational and health promotion approaches utilizing cognitive strategies may be a valuable intervention technique. Gollwitzer and colleagues (Gollwitzer & Brandstätter, 1997; Gollwitzer & Schaal, 1998) suggest that formulating goal-directed plans in a specific context more effectively facilitates the carrying out of intentions, such as going on a healthier diet (Verplanken & Faes, 1999). Investigations into attitude change demonstrate that directed-thinking tasks may increase the probability of engaging in a specific health behavior (McGuire & McGuire, 1996; Ratcliff et al., 1999), and self-efficacy manipulations (Chambliss & Murray, 1979) have been shown to assist in losing weight.
Risk-stratification based on socioeconomic position may enable health care professionals to target these interventions where they are needed most. School programs may promote resilience to stressful social events by incorporating components to reduce pessimism and increase optimism (Gillham & Reivich, 1999) or to minimize cognitive biases (Chen & Matthews, 2001) possibly reducing the physiological toll of cardiovascular responses.
Additionally, raising individuals’ educational status through cognitive interventions may demonstrate protective health effects. Work on stereotype threat has indicated that disidentification with academic pursuits among stereotyped groups contributes to reinforcement of the SES hierarchy through resulting low academic performance (Major, Spencer, Schmader, Wolf, & Crocker, 1997). Supporting this finding, children with higher perceptions of school-specific control perform better academically than children who attribute school performance to external causes (Bandura, Barbaranelli, Caprara, & Pastorelli, 1996; Butler & Orion, 1990; Harter, 1992). Perceived control may enhance academic performance via associations with positive mood, curiosity, pride, and persistence (Skinner, 1995).
In sum, myriad factors influence SES differences in coronary disease and associated health behaviors, including the price of healthy foods, access to physical fitness resources, and barriers to medical care. Additionally, social cognitive resources, by influencing how events are perceived, may exacerbate or ameliorate the behavioral and physiological responses to stress that lead to social gradients in health (Taylor & Seeman, 1999). Although the social cognitive factors reviewed here may not fully explain the SES–CHD relationship, evidence supports a potentially key role.
Short Biographies
Jennifer E. Phillips holds an MS in Psychology from the University of Pittsburgh, where she is in the process of completing her dissertation, entitled Socioeconomic Status, Amygdala Reactivity, and Selective Attention to Threat. Throughout her graduate career Ms. Phillips’ research has focused on examining the associations between socioeconomic factors and cardiovascular disease and its associated risk factors, with particular emphasis on the role of psychological factors in this relationship. She has co-authored papers in this area for Brain, Behavior, and Immunity, Obesity, and Psychosomatic Medicine. As her research interests have evolved over the course of graduate training, she has identified obesity as one primary area of focus. She recently collaborated on a chapter on disordered eating for the International Handbook of Behavior, Diet, and Nutrition.
Dr. William M. P. Klein is Associate Director of the Behavioral Research Program in the Division of Cancer Control and Population Sciences at the National Cancer Institute (NCI). He joined NCI from the Psychology Department at the University of Pittsburgh, where he was a member of the faculty in the Social Psychology and the Biological and Health Psychology graduate programs. Dr. Klein completed his PhD in Social Psychology at Princeton University in 1991. His research interests fall largely under the areas of self-judgment, risk perception, and risk communication. For example, he has been interested in how risk perception biases are related to the processing of health communications, to health decision-making, and to health behavior; how social processes (e.g., social comparison, self-affirmation, peer influence, self-evaluation, self-presentation) influence responses to personalized feedback and risk communication; the influence of affective factors such as worry on risk appraisal and health decisions; the impact of ambiguity on responses to feedback and risk messages; the role of optimism in health behavior and psychological functioning; and applications of theory to risk communication and health behavior intervention. Dr. Klein’s work has been supported by the NCI, National Science Foundation, and several private foundations.
References
- Aalto A, Weinman J, French DP, Aro AR, Manderbacka K, Keskimäki I. Sociodemographic differences in myocardial infarction risk perceptions among people with coronary heart disease. Journal of Health Psychology. 2007;12:316–329. doi: 10.1177/1359105307074270. [DOI] [PubMed] [Google Scholar]
- Abramson L, Seligman Y, Teasdale M. Learned helplessness in humans: Critique and reformulation. Abnormal Psychology. 1978;87:49–74. [PubMed] [Google Scholar]
- Adler NE, Boyce T, Chesney MA, Cohen S, Folkman S, Kahn R, et al. Socioeconomic status and health: The challenge of the gradient. American Psychologist. 1994;49:15–24. doi: 10.1037//0003-066x.49.1.15. [DOI] [PubMed] [Google Scholar]
- Adler NE, Epel ES, Castellazzo G, Ickovics JR. Relationship of subjective and objective social status with psychological and physiological functioning: Preliminary data in healthy white women. Health Psychology. 2000;19:586–592. doi: 10.1037//0278-6133.19.6.586. [DOI] [PubMed] [Google Scholar]
- Ainsworth BE, Wilcox S, Thompson WW, Richter DL, Henderson KA. Personal, social, and physical environmental correlates of physical activity in African American women in South Carolina. American Journal of Preventive Medicine. 2003;25(Suppl):S23–S29. doi: 10.1016/s0749-3797(03)00161-2. [DOI] [PubMed] [Google Scholar]
- Ajzen I. The theory of planned behavior. Organizational Behavior and Human Decision Processes. 1991;50:179–211. [Google Scholar]
- Amato PR, Zuo J. Rural poverty, urban poverty, and psychological well-being. Sociology Quarterly. 1992;33:229–240. [Google Scholar]
- American Heart Association. 2009 http://www.americanheart.org.
- Anderson NB, Armstead CA. Toward understanding the association of socioeconomic status and health: A new challenge for the biopsychosocial approach. Psychosomatic Medicine. 1995;57:213–225. doi: 10.1097/00006842-199505000-00003. [DOI] [PubMed] [Google Scholar]
- Armitage CJ, Conner M. Efficacy of the theory of planned behavior: A meta-analytic review. British Journal of Social Psychology. 2001;40:471–499. doi: 10.1348/014466601164939. [DOI] [PubMed] [Google Scholar]
- Bandura A, Barbaranelli C, Caprara GV, Pastorelli C. Multifaceted impact of self-efficacy beliefs on academic functioning. Child Development. 1996;67:1206–1222. [PubMed] [Google Scholar]
- Bandura A, Reese L, Adams NE. Microanalysis of action and fear arousal as a function of differential levels of perceived self-efficacy. Journal of Personality and Social Psychology. 1982;43:5–21. doi: 10.1037//0022-3514.43.1.5. [DOI] [PubMed] [Google Scholar]
- Bandura A, Taylor CB, Williams SL, Mefford IA, Barchas JD. Catecholamine secretion as a function of perceived coping self-efficacy. Journal of Consulting and Clinical Psychology. 1985;53:406–414. doi: 10.1037//0022-006x.53.3.406. [DOI] [PubMed] [Google Scholar]
- Barefoot JC, Dahlstrom WG, Williams RB. Hostility, CHD incidence, and total mortality: A 25-year follow-up study of 255 physicians. Psychosomatic Medicine. 1983;45:59–63. doi: 10.1097/00006842-198303000-00008. [DOI] [PubMed] [Google Scholar]
- Barefoot JC, Dodge KA, Peterson BL, Dahlstrom WG, Williams RB., Jr The Cook-Medley Hostility Scale: Item content and ability to predict survival. Psychosomatic Medicine. 1989;51:46–57. doi: 10.1097/00006842-198901000-00005. [DOI] [PubMed] [Google Scholar]
- Barefoot JC, Peterson BL, Dahlström WG, Williams RB. Hostility patterns and health implications: Correlates of Cook-Medley hostility scores in a national survey. Health Psychology. 1991;10:18–24. doi: 10.1037//0278-6133.10.1.18. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Barrios FX, Niehaus JC. The influence of smoker status, smoking history, sex, and situational variables on smokers’ self-efficacy. Addictive Behaviors. 1985;10:425–429. doi: 10.1016/0306-4603(85)90040-1. [DOI] [PubMed] [Google Scholar]
- Baum A, Garofalo JP, Yali AM. Socioeconomic status and chronic stress. Does stress account for SES effects on health? Annals of the New York Academy of Sciences. 1999;896:131–144. doi: 10.1111/j.1749-6632.1999.tb08111.x. [DOI] [PubMed] [Google Scholar]
- Bennett P, Moore L, Smith A, Murphy S, Smith C. Health locus of control and value for health as predictors of dietary behavior. Psychology and Health. 1995;10:41–54. [Google Scholar]
- Best JA, Steffy RA. Smoking modification procedures tailored to subject characteristics. Behavior Therapy. 1971;2:177–191. [Google Scholar]
- Blair A, Booth D, Lewis V, Wainwright C. The relative success of official and informal weight reduction techniques: Retrospective correlational evidence. Psychology and Health. 1989;3:195–206. [Google Scholar]
- Blascovich J, Spencer SJ, Quinn D, Steele C. African Americans and high blood pressure: The role of stereotype threat. Psychological Science. 2001;12:225–229. doi: 10.1111/1467-9280.00340. [DOI] [PubMed] [Google Scholar]
- Bosma H, Schrijvers C, Mackenbach JP. Socioeconomic inequalities in mortality and importance of perceived control: Cohort study. British Medical Journal. 1999;319:1469–1470. doi: 10.1136/bmj.319.7223.1469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosma H, Van Jaarsveld CH, Tuinstra J, Sanderman R, Ranchor AV, Van Eijk JT, et al. Low control beliefs, classical coronary risk factors, and socio-economic differences in heart disease in older persons. Social Science and Medicine. 2005;60:737–745. doi: 10.1016/j.socscimed.2004.06.018. [DOI] [PubMed] [Google Scholar]
- Brawley LR, Rogers WM. Social psychological aspects of fitness promotion. In: Seraganian P, editor. Exercise Psychology: The Influence of Physical Exercise on Psychological Processes. New York, NY: Wiley; 1993. pp. 254–298. [Google Scholar]
- Brod MI, Hall SM. Joiners and non-joiners in smoking treatment: A comparison of psychosocial variables. Addictive Behaviors. 1984;9:217–221. doi: 10.1016/0306-4603(84)90061-3. [DOI] [PubMed] [Google Scholar]
- Brondolo E, Rieppi R, Kelly KP, Gerin W. Perceived racism and blood pressure: A review of the literature and conceptual and methodological critique. Annals of Behavioral Medicine. 2003;25:55–65. doi: 10.1207/S15324796ABM2501_08. [DOI] [PubMed] [Google Scholar]
- Brunner EJ, Marmot MJ, Nanchahal K, Shipley MJ, Stansfield SA, Juneja M, et al. Social Inequality in coronary risk: Central obesity and the metabolic syndrome. Evidence from the Whitehall II study. Diabetologia. 1997;40:1341–1349. doi: 10.1007/s001250050830. [DOI] [PubMed] [Google Scholar]
- Bullock HE. Attributions for poverty: A comparison of middle-class and welfare recipient attitudes. Journal of Applied Social Psychology. 1999;29:2059–2082. [Google Scholar]
- Butler R, Orion R. When pupils do not understand the determinants of their success and failure in school: Relations between internal, teacher and unknown perceptions of control and school achievement. British Journal of Educational Psychology. 1990;60:63–75. doi: 10.1111/j.2044-8279.1990.tb00922.x. [DOI] [PubMed] [Google Scholar]
- Carey MP, Snel DL, Carey KB, Richards CS. Self-initiated smoking cessation: A review of the empirical literature from a stress and coping perspective. Cognitive Therapy and Research. 1989;13:323–341. [Google Scholar]
- Carlisle-Frank P. Examining personal control beliefs as a mediating variable in the health-damaging behavior of substance use: An alternative approach. The Journal of Psychology. 1991;125:381–397. doi: 10.1080/00223980.1991.10543300. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. 2009 http://www.cdc.gov/
- Chambliss CA, Murray EJ. Efficacy attribution, locus of control, and weight loss. Cognitive Therapy and Research. 1979;3:349–353. [Google Scholar]
- Chandola T, Kuper H, Singh-Manoux A, Bartley M, Marmot M. The effect of control at home on CHD events in the Whitehall II study: Gender differences in psychosocial domestic pathways to social inequalities in CHD. Social Science & Medicine. 2004;58:1501–1509. doi: 10.1016/S0277-9536(03)00352-6. [DOI] [PubMed] [Google Scholar]
- Chen E, Langer DA, Raphaelson YE, Matthews KA. Socioeconomic status and health in adolescents: The role of stress interpretations. Child Development. 2004;75:1039–1052. doi: 10.1111/j.1467-8624.2004.00724.x. [DOI] [PubMed] [Google Scholar]
- Chen E, Matthews KA. Cognitive Appraisal Biases: An approach to understanding the relation between socioeconomic status and cardiovascular reactivity in children. Annals of Behavioral Medicine. 2001;23:101–111. doi: 10.1207/S15324796ABM2302_4. [DOI] [PubMed] [Google Scholar]
- Christakis NA, Fowler JH. The spread of obesity in a Large social network over 32 years. New England Journal of Medicine. 2007;357:370–379. doi: 10.1056/NEJMsa066082. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kaplan G, Salonen JT. The role of psychological characteristics in the relation between socioeconomic status and perceived health. Journal of Applied Social Psychology. 1999;29:445–467. [Google Scholar]
- Coletti G, Supnick JA, Payne TJ. The Smoking Self-Efficacy Questionnaire (SSEQ): Preliminary scale development and validation. Behavioral Assessment. 1985;7:765–782. [Google Scholar]
- Conrad KM, Flay BR, Hill D. Why children start smoking cigarettes: Predictors of onset. British Journal of Addiction. 1992;87:1711–1724. doi: 10.1111/j.1360-0443.1992.tb02684.x. [DOI] [PubMed] [Google Scholar]
- Cooper R, Cutler J, Desvigne-Nickens P, Fortmann SP, Friedman L, Havlik R, et al. Trends and disparities in coronary heart disease, stroke, and other cardiovascular diseases in the United States. Findings of the National Conference on Cardiovascular Disease Prevention. Circulation. 2000;102:3137–3147. doi: 10.1161/01.cir.102.25.3137. [DOI] [PubMed] [Google Scholar]
- Corbett CF. Research-based practice implications for patients with diabetes. Part II: Diabetes self-efficacy. Home Healthcare Nurse. 1999;17:587–596. doi: 10.1097/00004045-199909000-00010. [DOI] [PubMed] [Google Scholar]
- Corti R, Binggeli C, Sudano I, Spieker LE, Wenzel RR, Lüscher TF, et al. The Beauty and the Beast: Aspects of the Autonomic Nervous System. News in Physiological Sciences. 2000;15:125–129. doi: 10.1152/physiologyonline.2000.15.3.125. [DOI] [PubMed] [Google Scholar]
- Courneya KS, Friedenreich CM, Arthur K, Bobick TM. Understanding exercise motivation in colorectal cancer patients: A prospective study using the theory of planned behavior. Rehabilitation Psychology. 1999;44:68–84. [Google Scholar]
- Croizet JC, Claire T. Extending the concept of stereotype threat to social class: The intellectual underperformance of students from low socioeconomic backgrounds. Personality and Social Psychology Bulletin. 1998;24:588–594. [Google Scholar]
- Cromwell R, Butterfield E, Brayfield F, Curry J. Acute Myocardial Infarction: Reaction and Recovery. St Louis, MO: Mosby; 1977. [Google Scholar]
- Dembroski TM, MacDougall JM, Costa PT, Grandits GA. Components of hostility as predictors of sudden death and myocardial infarction in the Multiple Risk Factor Intervention Trial. Psychosomatic Medicine. 1989;51:514–521. doi: 10.1097/00006842-198909000-00003. [DOI] [PubMed] [Google Scholar]
- Desmond SM, Price JH, Eoff TA. Nurses’ perception regarding health care and the poor. Psychological Reports. 1989;65:1043–1052. [PubMed] [Google Scholar]
- DiClemente CC. Self-Efficacy and smoking cessation maintenance: A preliminary report. Cognitive Therapy and Research. 1981;5:175–187. [Google Scholar]
- DiClemente CC, Fairhurst S, Piotrowski N. The role of self-efficacy in the addictive behaviors. In: Maddux J, editor. Self-efficacy, Adaptation, and Adjustment: Theory, Research, and Application. New York, NY: Plenum Press; 1995. pp. 109–141. [Google Scholar]
- Diez-Roux AV, Nieto FJ, Tyroler HA, Crum LD, Szklo M. Social inequalities and atherosclerosis. The atherosclerosis risk in communities study. American Journal of Epidemiology. 1995;141:960–972. doi: 10.1093/oxfordjournals.aje.a117363. [DOI] [PubMed] [Google Scholar]
- Dzewaltowski DA, Noble JM, Shaw JM. Physical activity participation: Social cognitive theory versus the theories of reasoned action and planned behavior. Journal of Sport & Exercise Psychology. 1990;12:388–405. doi: 10.1123/jsep.12.4.388. [DOI] [PubMed] [Google Scholar]
- Emmons KM, Barbeau EM, Gutheil C, Stryker JE, Stoddard AM. Social influences, social context, and health behaviors among working-class, multiethnic adults. Health Education and Behavior. 2007;34:315–334. doi: 10.1177/1090198106288011. [DOI] [PubMed] [Google Scholar]
- Evenson KR, Wilcox S, Pettinger M, Brunner R, King AC, McTiernan A. Vigorous leisure activity through women’s adult life – The Women’s Health Initiative observational cohort study. American Journal of Epidemiology. 2002;156:945–953. doi: 10.1093/aje/kwf132. [DOI] [PubMed] [Google Scholar]
- Feldman JM, Hilterman RJ. Stereotype attribution revisited: The role of stimulus characteristics, racial attitude, and cognitive differentiation. Personality and Social Psychology Bulletin. 1974;1:62–65. [Google Scholar]
- Finkelstein DM, Kubzansky LD, Capitman JA, Goodman E. Socioeconomic differences in adolescent stress: The role of psychological resources. Journal of Adolescent Health. 2007;40:127–134. doi: 10.1016/j.jadohealth.2006.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flowers BJ. Perceived control, illness status, stress, and adjustment to cardiac illness. The Journal of Psychology. 1994;128:567–576. doi: 10.1080/00223980.1994.9914914. [DOI] [PubMed] [Google Scholar]
- Ford ES, Merritt RK, Heath GW, Powell KE, Washburn RA, Kriska A, et al. Physical activity behaviors in lower and higher socioeconomic status populations. American Journal of Epidemiology. 1991;133:1246–1256. doi: 10.1093/oxfordjournals.aje.a115836. [DOI] [PubMed] [Google Scholar]
- Forgas JP. Handbook of Affect and Social Cognition. New York, NY: Lawrence Erlbaum Associates; 2001. [Google Scholar]
- Gallo LC, Matthews KA. Understanding the association between socioeconomic status and physical health: Do negative emotions play a role? Psychological Bulletin. 2003;129:10–51. doi: 10.1037/0033-2909.129.1.10. [DOI] [PubMed] [Google Scholar]
- Gans KM, Assmann SF, Sallar A, Lasater TM. Knowledge of cardiovascular disease prevention: An analysis from two New England communities. Preventive Medicine. 1999;29:229–237. doi: 10.1006/pmed.1999.0532. [DOI] [PubMed] [Google Scholar]
- Gecas V. The social psychology of self-efficacy. Annual Review of Sociology. 1989;15:291–316. [Google Scholar]
- Gerin W, Litt MD, Deich J, Pickering TG. Self-efficacy as a component of active coping: Effects on cardiovascular reactivity. Journal of Psychosomatic Research. 1996;40:485–493. doi: 10.1016/0022-3999(95)00642-7. [DOI] [PubMed] [Google Scholar]
- Gianaros PJ, Horenstein JA, Cohen S, Matthews KA, Brown SM, Flory JD, et al. Perigenual anterior cingulated morphology covaries with perceived social standing. Social Cognitive and Affective Neuroscience. 2007;2:161–173. doi: 10.1093/scan/nsm013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbons FX, Gerrard M. Predicting young adults’ health risk behavior. Journal of Personality and Social Psychology. 1995;69:505–517. doi: 10.1037//0022-3514.69.3.505. [DOI] [PubMed] [Google Scholar]
- Gillham JE, Reivich KJ. Prevention of depressive symptoms in schoolchildren: A research update. Psychological Science. 1999;10:461–462. [Google Scholar]
- Giltay EJ, Geleijnse JM, Zitman FG, Hoekstra T, Schouten EG. Dispositional optimism and all-cause and cardiovascular mortality in a prospective cohort of elderly Dutch men and women. Archives of General Psychiatry. 2004;61:1126–1135. doi: 10.1001/archpsyc.61.11.1126. [DOI] [PubMed] [Google Scholar]
- Giltay EJ, Kamphuis MH, Kalmijn S, Zitman FG, Kromhout D. Dispositional optimism and the risk of cardiovascular death: The Zutphen Elderly Study. Archives of Internal Medicine. 2006;166:431–436. doi: 10.1001/archinte.166.4.431. [DOI] [PubMed] [Google Scholar]
- Gollwitzer PM, Brandstätter V. Implementation intentions and effective goal pursuit. Journal of Personality and Social Psychology. 1997;73:186–199. doi: 10.1037//0022-3514.81.5.946. [DOI] [PubMed] [Google Scholar]
- Gollwitzer PM, Schaal B. Metacognition in action: The importance of implementation intentions. Personality and Social Psychology Review. 1998;2:124–136. doi: 10.1207/s15327957pspr0202_5. [DOI] [PubMed] [Google Scholar]
- Goodman E, Adler NE, Daniels SR, Morrison JA, Slap GB, Dolan LM. Impact of objective and subjective social status on obesity in a biracial cohort of adolescents. Obesity Research. 2003;11:1018–1026. doi: 10.1038/oby.2003.140. [DOI] [PubMed] [Google Scholar]
- Goodman E, Adler NE, Kawachi I, Frazier AL, Huang B, Colditz GA. Adolescents’ perceptions of social status: Development and evaluation of a new indicator. Pediatrics. 2001;108:1–8. doi: 10.1542/peds.108.2.e31. [DOI] [PubMed] [Google Scholar]
- Grewen K, Girdler SS, West SG, Bragdon E, Costello N, Light C. Stable pessimistic attributions interact with socioeconomic status to influence blood pressure and vulnerability to hypertension. Journal of Women’s Health and Gender-Based Medicine. 2000;9:905–915. doi: 10.1089/152460900750020946. [DOI] [PubMed] [Google Scholar]
- Gump BB, Matthews KA, Räikkönen K. Modeling relationships among socioeconomic status, hostility, cardiovascular reactivity, and left ventricular mass in African American and White children. Health Psychology. 1999;18:140–150. doi: 10.1037//0278-6133.18.2.140. [DOI] [PubMed] [Google Scholar]
- Haley A, Forman D, Poppas A, Hoth K, Gunstad J, Jefferson A, et al. Carotid artery intima-media thickness and cognition in cardiovascular disease. International Journal of Cardiology. 2007;121:148–154. doi: 10.1016/j.ijcard.2006.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanson MJ. Cross-cultural study of beliefs about smoking among teenaged females. Western Journal of Nursing Research. 1999;21:635–647. doi: 10.1177/01939459922044090. [DOI] [PubMed] [Google Scholar]
- Harrison LA, Stevens CM, Monty AN, Coakley CA. The consequences of stereotype threat on the academic performance of White and non-White lower income college students. Social Psychology of Education. 2006;9:341–357. [Google Scholar]
- Harter S. The relationship between perceived competence, affect, and motivational orientation within the classroom: Processes and patterns of change. In: Boggiano AK, Pittman TS, editors. Achievement and Motivation: A Social-developmental Perspective. New York, NY: Cambridge University Press; 1992. pp. 77–114. [Google Scholar]
- Hausenblas HA, Carron A, Mack DE. Applications of the theories of reasoned action and planned behavior to exercise behavior: A meta-analysis. Journal of Sport & Exercise Psychology. 1997;19:36–51. [Google Scholar]
- Hemingway H, Marmot M. Psychosocial factors in the aetiology and prognosis of coronary heart disease: Systematic review of prospective cohort studies. British Medical Journal. 1998;318:1460–1468. doi: 10.1136/bmj.318.7196.1460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James W, Woodruff A, Werner W. Effect of internal and external control upon changes in smoking behavior. Journal of Consulting Psychology. 1965;29:184–186. doi: 10.1037/h0021909. [DOI] [PubMed] [Google Scholar]
- Kaplan GA. Economic Policy is Health Policy: Conclusions from the Study of Income Inequality, Socioeconomic Status, and Health. Paper presented at Income Inequality, Socioeconomic Status, and Health Conference; Washington, D.C. sponsored by the National Policy Association and the Association for Health Services Research; 2000. [Google Scholar]
- Karasek R. Job demands, job decision latitude and mental strain: Implications for job redesign. Administrative Science Quarterly. 1979;24:285–306. [Google Scholar]
- Keil JE, Sutherland SE, Knapp RG, Tyroler HA. Does equal socioeconomic status in black and white men mean equal risk of mortality? American Journal of Public Health. 1992;82:1133–1136. doi: 10.2105/ajph.82.8.1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King AC, Castro C, Wilcox S, Eyler AA, Sallis JF, Brownson RC. Personal and environmental factors associated with physical inactivity among different racial-ethnic groups of U.S. middle-aged and older-aged women. Health Psychology. 2000;19:354. doi: 10.1037//0278-6133.19.4.354. [DOI] [PubMed] [Google Scholar]
- Klein WMP. Comparative risk estimates relative to the average peer predict behavioral intentions and concern about absolute risk. Risk, Decision, and Policy. 2002;7:193–202. [Google Scholar]
- Klein WM, Weinstein ND. Social comparison and unrealistic optimism about personal risk. In: Buunk BP, Gibbons FX, editors. Health Coping and Wellbeing: Perspectives from Social Comparison Theory. Mahwah, NJ: Erlbaum; 1997. pp. 25–62. [Google Scholar]
- Ko GT, Chan JC, Yeung VT, Chow CC, Tsang LW, Cockram CS. A low socio-economic status is an additional risk factor for glucose intolerance in high risk Hong Kong Chinese. European Journal of Epidemiology. 2001;17:289–295. doi: 10.1023/a:1017935707807. [DOI] [PubMed] [Google Scholar]
- Kohn ML, Schooler C. Job conditions and personality: A longitudinal assessment of their reciprocal effects. The American Journal of Sociology. 1982;87:1257–1286. [Google Scholar]
- Kubzansky LD, Sparrow D, Vokonas P, Kawachi I. Is the glass half empty or half full? A prospective study of optimism and coronary heart disease in the normative aging study. Psychosomatic Medicine. 2001;63:910–916. doi: 10.1097/00006842-200111000-00009. [DOI] [PubMed] [Google Scholar]
- Lachman ME, Weaver SL. The Sense of control as a moderator of social class differences in health and well being. Journal of Personality and Social Psychology. 1998;74:763–773. doi: 10.1037//0022-3514.74.3.763. [DOI] [PubMed] [Google Scholar]
- Lawlor DA, Ebrahim S, Davey Smith G. Socioeconomic position in childhood and adulthood and insulin resistance: Cross sectional survey using data from British women’s heart and health study. British Medical Journal. 2002;325:805–810. doi: 10.1136/bmj.325.7368.805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leahy RL. The development of the conception of economic inequality: I. Descriptions and comparisons of rich and poor people. Child Development. 1981;52:523–532. [Google Scholar]
- Lynch JW, Davey Smith G, Kaplan GA, House JS. Income inequality and mortality: Importance to health of individual income, psychosocial environment, or material conditions. BMJ. 2000;320:1200–1204. doi: 10.1136/bmj.320.7243.1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch JW, Everson SA, Kaplan GA, Salonen R, Salonen JT. Does low socioeconomic status potentiate the effects of heightened cardiovascular responses to stress on the progression of carotid atherosclerosis? American Journal of Public Health. 1998;88:389–394. doi: 10.2105/ajph.88.3.389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch E, Liu K, Spring B, Hankinson A, Wei GS, Greenland P. Association of ethnicity and socioeconomic status with judgments of body size: The Coronary Artery Risk Development in Young Adults (CARDIA) Study. American Journal of Epidemiology. 2007;165:1055–1062. doi: 10.1093/aje/kwk114. [DOI] [PubMed] [Google Scholar]
- Major B, Spencer S, Schmader T, Wolf C, Crocker J. Coping with negative stereotypes about intellectual performances: The role of psychological disengagement. Personality and Social Psychology Bulletin. 1997;24:34–50. [Google Scholar]
- Manfredi C, Cho YI, Crittenden KS, Dolecek TA. A path model of smoking cessation in women smokers of low socio-economic status. Health Education Research. 2007;22:747–756. doi: 10.1093/her/cyl155. [DOI] [PubMed] [Google Scholar]
- Manfredi C, Lacey L, Warnecke R, Buis M. Smoking-related behavior, beliefs, and social environment of young black women in subsidized public housing in Chicago. American Journal of Public Health. 1992;82:267–272. doi: 10.2105/ajph.82.2.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manuck SB, Kasprowicz AL, Monroe SM, Larkin KT, Kaplan JR. Psychophysiologic reactivity as a dimension of individual differences. In: Schneiderman N, Weiss SM, Kaufmann PG, editors. Handbook of Research Methods in Cardiovascular Behavioral Medicine. New York: Plenum; 1989. pp. 365–382. [Google Scholar]
- Marmot MG, Bosma H, Hemingway H, Brunner E, Stansfield S. Contribution of job control and other risk factors to social variations in coronary heart disease incidence. Lancet. 1997;350:235–239. doi: 10.1016/s0140-6736(97)04244-x. [DOI] [PubMed] [Google Scholar]
- Marmot M, Wilkinson RG. Social Determinants of Health. Oxford: Oxford University Press; 1999. [Google Scholar]
- McAuley E, Courneya KS. Adherence to exercise and physical activity as health-promoting behaviors: Attitudinal and self-efficacy influences. Applied and Preventative Psychology. 1993;2:65–77. [Google Scholar]
- McGuire WJ, McGuire CV. Enhancing self-esteem by directed-thinking tasks: Cognitive and affective positivity asymmetries. Journal of Personality and Social Psychology. 1996;70:1117–1125. doi: 10.1037//0022-3514.70.6.1117. [DOI] [PubMed] [Google Scholar]
- McLaren L, Kuh D. Women’s body dissatisfaction, social class, and social mobility. Social Science & Medicine. 2004;58:1575–1584. doi: 10.1016/S0277-9536(03)00209-0. [DOI] [PubMed] [Google Scholar]
- McLoyd VC. Socioeconomic disadvantage and child development. American Psychologist. 1998;53:185–204. doi: 10.1037//0003-066x.53.2.185. [DOI] [PubMed] [Google Scholar]
- Mendes WB, Blascovich J, Major B, Seery M. Challenge and threat responses during downward and upward social comparisons. European Journal of Social Psychology. 2001;31:477–497. [Google Scholar]
- Mirowsky J, Ross C. Paranoia and the structure of powerlessness. American Sociological Review. 1983;48:228–239. [PubMed] [Google Scholar]
- Morrison DM, Gillmore MR, Simpson EE, Wells EA. Children’s decisions about substance use: An application and extension of the theory of reasoned action. Journal of Applied Social Psychology. 1996;26:1658–1679. [Google Scholar]
- Moskowitz G. Social Cognition: Understanding Self and Others. New York: The Guilford Press; 2005. [Google Scholar]
- Mudde AN, de Vries H, Dolders MG. Evaluation of a Dutch community-based smoking cessation intervention. Preventive Medicine. 1995;24:61–70. doi: 10.1006/pmed.1995.1009. [DOI] [PubMed] [Google Scholar]
- National Heart, Lung, and Blood Institute (NHLBI) Report of the Conference on Socioeconomic Status and Cardiovascular Health and Disease. 1995 http://www.nhlbi.nih.gov/resources/docs/sesintro.htm.
- Neisser U, Boodoo G, Bouchard TJ, Boykin WA, Brody N, Ceci SJ, et al. Intelligence: Knowns and unknowns. American Psychologist. 1996;51:77–101. [Google Scholar]
- Norman P, Bennett P, Smith C, Murphy S. Health locus of control and health behaviour. Journal of Health Psychology. 1998;3:171–182. doi: 10.1177/135910539800300202. [DOI] [PubMed] [Google Scholar]
- Norman P, Conner M, Bell R. The theory of planned behavior and smoking cessation. Health Psychology. 1999;18:89–94. doi: 10.1037//0278-6133.18.1.89. [DOI] [PubMed] [Google Scholar]
- O’Callaghan FV, Callan VJ, Baglioni A. Cigarette use by adolescents: Attitude-behavior relationships. Substance Use and Misuse. 1999;34:455–468. doi: 10.3109/10826089909035656. [DOI] [PubMed] [Google Scholar]
- Ogden J, Wardle J. Control of eating and attributional style. British Journal of Clinical Psychology. 1990;29:445–446. doi: 10.1111/j.2044-8260.1990.tb00912.x. [DOI] [PubMed] [Google Scholar]
- Okun MA, Ruehlman L, Karoly P, Lutz R, Fairholme C, Schaub R. Social support and social norms: Do both contribute to predicting leisure-time exercise? American Journal of Health Behavior. 2003;27:493–507. doi: 10.5993/ajhb.27.5.2. [DOI] [PubMed] [Google Scholar]
- Paisley CM, Sparks P. Expectations of reducing fat intake: The role of perceived need within the Theory of Planned Behavior. Psychology and Health. 1998;13:341–353. [Google Scholar]
- Park Y, Zhu S, Palaniappan L, Heshka S, Carnethon MR, Heymsfield SB. The Metabolic syndrome: Prevalence and associated risk factor findings in the U.S. population from the third national Health and Nutrition Examination Survey, 1988–1994) Archives of Internal Medicine. 2003;163:427–435. doi: 10.1001/archinte.163.4.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearlin LI, Menaghan EG, Lieberman MA, Mullan JT. The stress process. Journal of Health and Social Behavior. 1981;22:337–356. [PubMed] [Google Scholar]
- Poag-DuCharme KA, Brawley LR. Self-efficacy theory: Use in the prediction of exercise behavior in the community setting. Journal of Applied Sport Psychology. 1993;5:178–194. [Google Scholar]
- Radcliffe NM, Klein WMP. Dispositional, unrealistic, and comparative optimism: Differential relations with knowledge and processing of risk information and beliefs about personal risk. Personality and Social Psychology Bulletin. 2002;28:836–846. [Google Scholar]
- Ratcliff CD, Czuchry M, Scarberry NC, Thomas JC, Dansereau DF, Lord CG. Effects of directed thinking on intentions to engage in beneficial activities: Actions versus reasons. Journal of Applied Social Psychology. 1999;29:994–1009. [Google Scholar]
- Resnick B, Orwig D, Magaziner J, Wynne C. The effect of social support on exercise behavior in older adults. Clinical Nursing Research. 2002;11:52–70. doi: 10.1177/105477380201100105. [DOI] [PubMed] [Google Scholar]
- Ribisl KM, Winkleby MA, Fortmann SP, Flora JA. The interplay of socioeconomic status and ethnicity on Hispanic and White men’s cardiovascular disease risk and health communication patterns. Health Education and Research. 1998;13:407–417. doi: 10.1093/her/13.3.407. [DOI] [PubMed] [Google Scholar]
- Rose G, Marmot MG. Social Class and Coronary Heart Disease. British Heart Journal. 1981;45:13–19. doi: 10.1136/hrt.45.1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosengren A, Hawken S, Ounpuu S, Sliwa K, Zubaid M, Almahmeed WA, et al. Association of psychosocial risk factors with risk of acute myocardial infarction in 11 119 cases and 13 648 controls from 52 countries (the INTERHEART study): Case-control study. Lancet. 2004;364:953–962. doi: 10.1016/S0140-6736(04)17019-0. [DOI] [PubMed] [Google Scholar]
- Rovniak LS, Anderson ES, Winett RA, Stephens RS. Social cognitive determinants of physical activity in young adults: A prospective structural equation analysis. Annals of Behavioral Medicine. 2002;24:149–156. doi: 10.1207/S15324796ABM2402_12. [DOI] [PubMed] [Google Scholar]
- Salovey P, Detweiler JB, Steward W, Bedell B. Affect and health-relevant cognition. In: Forgas JP, editor. Handbook of Affect and Social Cognition. NJ: Erlbaum, Mahwah; 2001. pp. 344–368. [Google Scholar]
- Sarkar U, Fisher L, Schillinger D. Is self-efficacy associated with diabetes self-management across race/ethnicity and health literacy? Diabetes Care. 2006;29:823–829. doi: 10.2337/diacare.29.04.06.dc05-1615. [DOI] [PubMed] [Google Scholar]
- Scherwitz L, Perkins L, Chesney M, Hughes G. Hostility and health behaviours in young adults: The CARDIA study. Psychosomatic Medicine. 1991;136:136–145. doi: 10.1097/00006842-199101000-00004. [DOI] [PubMed] [Google Scholar]
- Schnall PL, Landsbergis PA. Job strain and cardiovascular disease. Annual Review of Public Health. 1994;15:381–411. doi: 10.1146/annurev.pu.15.050194.002121. [DOI] [PubMed] [Google Scholar]
- Seccareccia F, Menotti A, Prati PL. Coronary heart disease prevention: Relationship between socio-economic status and knowledge, motivation and behaviour in a free-living male, adult population. European Journal of Epidemiology. 1991;7:166–170. doi: 10.1007/BF00237361. [DOI] [PubMed] [Google Scholar]
- Seeman M. Alienation and Anomie. In: Robinson JP, Shaver PR, Wrightsman LS, editors. Measures of Personality and Social Psychological Attitudes. Vol. 1. San Diego, CA: Academic Press, Inc; 1991. pp. 291–372. [Google Scholar]
- Seigel D, Kuller L, Lazarus NB, Black D, Feigal D, Hughes G, et al. Predictors of cardiovascular events and mortality in the systolic hypertension in the elderly program pilot project. American Journal of Epidemiology. 1987;126:385–399. doi: 10.1093/oxfordjournals.aje.a114670. [DOI] [PubMed] [Google Scholar]
- Silagy C, Muir J, Coulter A, Thorogood M, Roe L. Cardiovascular risk and attitudes to lifestyle: What do patients think? BMJ. 1993;306:1657–1660. doi: 10.1136/bmj.306.6893.1657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh-Manoux A, Marmot MG, Adler NE. Does subjective social status predict health and change in health status better than objective status? Psychosomatic Medicine. 2005;67:855–861. doi: 10.1097/01.psy.0000188434.52941.a0. [DOI] [PubMed] [Google Scholar]
- Skinner EA. Perceived Control, Motivation, and Coping. Thousand Oaks, CA: Sage Publications; 1995. [Google Scholar]
- Sobal A, Stunkard AJ. Socioeconomic status and obesity: A review of the literature. Psychological Bulletin. 1989;105:260–275. doi: 10.1037/0033-2909.105.2.260. [DOI] [PubMed] [Google Scholar]
- Sonstroem R, Walker M. Relationship of attitudes and locus of control to exercise and physical fitness. Perceptual and Motor Skills. 1973;36:1031–1034. doi: 10.2466/pms.1973.36.3c.1031. [DOI] [PubMed] [Google Scholar]
- Sorel JE, Ragland DR, Syme SL, Davis WB. Educational status and blood pressure: The Second National Health and Nutrition Examination Survey, 1976–1980, and the Hispanic Health and Nutrition Examination Survey, 1982–1984. American Journal of Epidemiology. 1992;135:1339–1348. doi: 10.1093/oxfordjournals.aje.a116245. [DOI] [PubMed] [Google Scholar]
- Steele CM, Aronson J. Stereotype threat and the intellectual test performance of African-Americans. Journal of Personality and Social Psychology. 1995;69:797–811. doi: 10.1037//0022-3514.69.5.797. [DOI] [PubMed] [Google Scholar]
- Steele CM, Spencer S, Aronson J. Contending with group image: The psychology of stereotype and social identity threat. In: Zanna M, editor. Advances in Experimental Social Psychology. Vol. 37. San Diego, CA: Academic Press; 2002. pp. 379–440. [Google Scholar]
- Steptoe A, Wardle J. Motivational factors as mediators of socioeconomic variations in dietary intake patterns. Psychology and Health. 1999;14:391–402. [Google Scholar]
- Strecher VJ, Kreuter MW, Kobrin SC. Do cigarette smokers have unrealistic perceptions of their heart attack, cancer, and stroke risks? Journal of Behavioral Medicine. 1995;18:45–54. doi: 10.1007/BF01857704. [DOI] [PubMed] [Google Scholar]
- Sutton S. Predicting and explaining intentions and behavior: How well are we doing? Journal of Applied Social Psychology. 1998;28:1317–1338. [Google Scholar]
- Taylor S, Repetti RL, Seeman TE. What is an unhealthy environment and how does it get under the skin? Annual Review of Psychology. 1997;48:411. doi: 10.1146/annurev.psych.48.1.411. [DOI] [PubMed] [Google Scholar]
- Taylor SE, Seeman TE. Psychosocial resources and the SES-health relationship. Annals of the New York Academy of Sciences. 1999;896:210–225. doi: 10.1111/j.1749-6632.1999.tb08117.x. [DOI] [PubMed] [Google Scholar]
- Thornton B, Gibbons FX, Gerrard M. Risk perceptions and prototype perception: Independent processes predicting risk behavior. Personality and Social Psychology Bulletin. 2002;28:986–999. [Google Scholar]
- Trafimow D, Trafimow JH. Predicting back pain sufferers’ intentions to exercise. The Journal of Psychology: Interdisciplinary and Applied. 1998;132:581–592. doi: 10.1080/00223989809599291. [DOI] [PubMed] [Google Scholar]
- Treiber FA, Kamarck T, Schneiderman N, Sheffield D, Kapuku G, Taylor T. Cardiovascular reactivity and development of preclinical and clinical disease states. Psychosomatic Medicine. 2003;65:46–62. doi: 10.1097/00006842-200301000-00007. [DOI] [PubMed] [Google Scholar]
- Trivedi AN, Ayanian JA. Perceived discrimination and use of preventive health services. Journal of General Internal Medicine. 2006;21:553–558. doi: 10.1111/j.1525-1497.2006.00413.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trost SG, Pate RR, Ward DS, Saunders R, Riner W. Correlates of objectively measured physical activity in preadolescent youth. American Journal of Preventive Medicine. 1999;17:120–126. doi: 10.1016/s0749-3797(99)00056-2. [DOI] [PubMed] [Google Scholar]
- Twenge JM, Campbell WK. Self-esteem and socioeconomic status: A meta-analytic review. Personality & Social Psychology Review. 2002;6:59–71. [Google Scholar]
- Vargas CM, Ingram DD, Gillum RF. Incidence of hypertension and educational attainment: The NHANES I epidemiologic follow-up study. First National Health and Nutrition Examination Survey. American Journal of Epidemiology. 2000;152:272–278. doi: 10.1093/aje/152.3.272. [DOI] [PubMed] [Google Scholar]
- Verplanken B, Faes S. Good intentions, bad habits, and effects of forming implementation intentions on healthy eating. European Journal of Social Psychology. 1999;29:591–604. [Google Scholar]
- Vlahov D, Galea S. Urbanization, urbanicity and health. Journal of Urban Health: Bulletin of the New York Academy of Medicine. 2002;79:S1–S12. doi: 10.1093/jurban/79.suppl_1.S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wannamethee GS, Whincup PH, Shaper G, Walker M. Influence of father’s social class on cardiovascular disease in middle-aged men. Lancet. 1996;348:1259–1263. doi: 10.1016/S0140-6736(96)02465-8. [DOI] [PubMed] [Google Scholar]
- Wardle J, Griffith J. Socioeconomic status and weight control practices in British adults. Journal of Epidemiology and Community Health. 2001;55:185–190. doi: 10.1136/jech.55.3.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wardle J, Steptoe A. Socioeconomic differences in attitudes and beliefs about health lifestyles. Journal of Epidemiology and Community Health. 2003;57:440–443. doi: 10.1136/jech.57.6.440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wardle J, Waller J, Rapoport L. Body dissatisfaction and binge eating in obese women: The role of restraint and depression. Obesity Research. 2001;9:778–787. doi: 10.1038/oby.2001.107. [DOI] [PubMed] [Google Scholar]
- Warshaw PR, Davis FD. Disentangling behavioral intention and behavioral expectation. Journal of Experimental Social Psychology. 1985;21:213–228. [Google Scholar]
- Weech-Maldonado R, Dreachslin JL, Dansky KH. Racial/ethnic diversity management and cultural competency: The case of Pennsylvania hospitals. Journal of Health Care Management. 2002;47:111–124. [PubMed] [Google Scholar]
- Weeks M, Lupfer MB. Complicating Race: The relationship between prejudice, race, and social class categorizations. Personality and Social Psychology Bulletin. 2004;30:972–984. doi: 10.1177/0146167204264751. [DOI] [PubMed] [Google Scholar]
- Weinberg R, Hughes H, Critelli J, England R, Jackson A. Effects of preexisting and manipulated self-efficacy on weight loss in a self-control program. Journal of Research in Personality. 1984;18:352–358. [Google Scholar]
- Weinstein ND. Accuracy of smokers’ risk perceptions. Annals of Behavioral Medicine. 1998;20:135–140. doi: 10.1007/BF02884459. [DOI] [PubMed] [Google Scholar]
- Weinstein ND, Rothman AJ, Sutton SR. Stage theories of health behavior: Conceptual and methodological issues. Health Psychology. 1998;17:445–453. doi: 10.1037//0278-6133.17.3.290. [DOI] [PubMed] [Google Scholar]
- Wheaton B. The Sociogenesis of Psychological Disorder: An Attributional Theory. Journal of Health and Social Behavior. 1980;21:100–124. [PubMed] [Google Scholar]
- Wilkinson RG. Health inequalities: Relative or absolute material standards? BMJ. 1997;314:591–595. doi: 10.1136/bmj.314.7080.591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson RG. Health, hierarchy, and social anxiety. Annals of the New York Academy of Sciences. 1999;896:48–63. doi: 10.1111/j.1749-6632.1999.tb08104.x. [DOI] [PubMed] [Google Scholar]
- Winkleby MA, Flora JA, Kraemer HC. A community-based heart disease intervention: Predictors of change. American Journal of Public Health. 1994;84:767–772. doi: 10.2105/ajph.84.5.767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright RE, Dismukes A. Cardiovascular effects of experimentally induced efficacy (ability) appraisals at low and high levels of avoidant task demand. Psychophysiology. 1995;43:172–176. doi: 10.1111/j.1469-8986.1995.tb03309.x. [DOI] [PubMed] [Google Scholar]
- Wright CE, Steptoe A. Subjective socioeconomic position, gender and cortisol responses to waking in an elderly population. Psychoneuroendocrinology. 2005;30:582–590. doi: 10.1016/j.psyneuen.2005.01.007. [DOI] [PubMed] [Google Scholar]
- Zang EA, Wynder EL. Smoking Trends in the United States between 1969 and 1995 Based on Patients Hospitalized with Non-Smoking Related Diseases. Preventive Medicine. 1998;27:854–861. doi: 10.1006/pmed.1998.0369. [DOI] [PubMed] [Google Scholar]