Abstract
Many commentators view the conversion of small, independent primary care practices into patient-centered medical homes as a vital step in creating a better-performing health care system. The country’s first national medical home demonstration, which ran from June 1, 2006, to May 31, 2008, and involved thirty-six practices, showed that this transformation can be lengthy and complex. Among other features, the transformation process requires an internal capability for organizational learning and development; changes in the way primary care clinicians think about themselves and their relationships with patients as well as other clinicians on the care team; and awareness on the part of primary care clinicians that they will need to make long-term commitments to change that may require three to five years of external assistance. Additionally, transforming primary care requires synchronizing practice redesign with development of the health care “neighborhood,” which is made up of a broad range of health and health care resources available to patients. It also requires payment reform that supports practice development and a policy environment that sets reasonable expectations and time frames for the adoption of appropriate innovations.
Many people hope that the widespread adoption of the patient-centered medical home model will improve the quality and constrain the costs of health care. Although still unproven in large-scale demonstrations, the medical home represents an important upgrade of the traditional primary care practice.
The model unites four compelling areas of health reform activity.1,2 First, there is growing evidence that the “four pillars of primary care” contribute to a health care system of higher quality at lower cost and with more equity.3–5 The four pillars are access to first-contact care, coordinated care, comprehensive care, and sustained personal relationships.
Second, most medical home models incorporate the Chronic Care Model,6,7 for which there is growing evidence of positive effects on chronic disease outcomes.
Third, the “patient-centered” part of the medical home depends on having activated, engaged patients who want better service and transparency in health care and seek to form partnerships with health care practices. Patients are asking for the care they want and need, when and how they want and need it, as well as for access to information to make appropriate choices.
Fourth, the medical home incorporates new health information technologies, electronic clinical information systems, and telecommunications capabilities.
When coupled with primary care payment reform, the medical home offers great promise for improved health outcomes at lower cost for the American people.8
The National Demonstration Project
In June 2006 the American Academy of Family Physicians launched the first large-scale demonstration of the patient-centered medical home. A well-publicized national recruitment effort and a detailed application process yielded 337 family practices. Of these, thirty-six mostly small, independent practices were selected to transform themselves into patient-centered medical homes. Practices in this group were randomized to two groups: “facilitated intervention” and “self-directed,” as explained further below. The authors made up an independent evaluation team and have published results of the demonstration project as a supplement to the Annals of Family Medicine, which is available free online.9
The initial project model was based on practice redesign principles articulated in a report on the future of family medicine.10 The model continued to evolve as the principles of the patient-centered medical home developed.11 The model, which is available online,12 included more than fifty individual components in eight categories or domains: access to care and information, practice services, care management, continuity of care, practice-based care teams, quality and safety, health information technology (IT), and practice management. The core of the model envisioned a continuous relationship between a person and his or her personal physician, who would coordinate care to advance wellness and treat illness.
To assist the intervention practices, the project employed three practice enhancement facilitators from diverse backgrounds in finance, practice management, and organizational psychology. They worked intensively with six practices apiece, making four to six site visits during the two-year project and maintaining contact by phone and e-mail with several key players in each practice nearly daily. They also connected their practices with project consultants and other external resources, who could assist in areas such as advanced-access (or same-day) scheduling, office design, and patient flow. In many cases, facilitators served at the interface of the practice and a health IT vendor to assist with product or system implementation challenges.
Four three-day learning sessions brought key intervention-practice “stakeholders” together to discuss model components and share implementation experiences. Stakeholders in all cases included a physician “champion” and one or more clinical or administrative staff. Appendix Exhibit 1 summarizes one practice’s experience working with its facilitator to implement model components.13 Practices made substantial progress, and both groups were able to put the majority of model components into place, although facilitated practices adopted more model components than self-directed practices did.14
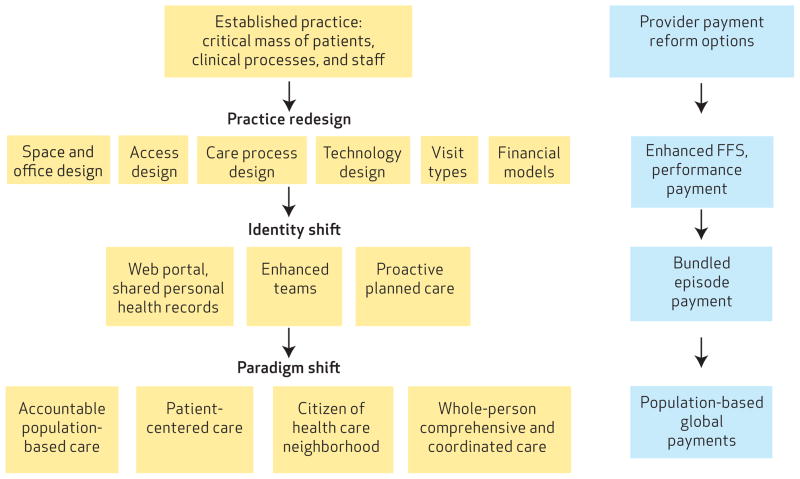
EXHIBIT 1.
Provider Payment Reform Options To Support Change And Transformation To A Medical Home Model
SOURCE Authors’ analysis. NOTE FFS is fee-for-service.
Practices were particularly successful in implementing those discrete components of the model that could be adopted with minimal impact on individual roles and work identities and that had little ripple effect on other practice processes. For example, all practices were able to implement same-day appointments, and nearly all were able to implement electronic prescribing and improved patient access to laboratory results. Implementation was more difficult for components that required fundamental changes in established routines and coordination across work groups, or that challenged traditional roles and models of practices. Integration with community services, wellness promotion, proactive population management, and team-based care presented the greatest challenges.14
The project design had several important limitations. First, the project did not include changes in physician reimbursement, although practices generally anticipated that payment reform would eventually favor the changes they were making. The implementation strategy emphasized health IT, chronic care management, and access to care. There was little emphasis on specific changes to enhance patient-centeredness and on coordination across the care resources that make up the health care “neighborhood”—ranging from specialists and hospitals to social, nutritional, and wellness services. Finally, although the facilitators received training in managing communication and relationships, this was not emphasized in all practices.
Lessons From The National Demonstration Project
TRANSFORMATION, NOT INCREMENTAL CHANGES
Transformation is more than a series of incremental changes. Practices that were included in the national demonstration project made heroic efforts and attempted to implement as many model components as possible over the two-year life of the project. The findings suggest that many of the chronic care and health IT components may be implemented by highly motivated practices. Nevertheless, even with extensive assistance from their facilitator, the availability of expert consultation, and the incentive of being in a national spotlight, two years was not long enough to implement the entire model and to transform work processes.
Putting discrete model components in place appears to be far easier than modifying existing roles and work patterns for using them effectively. As outlined in Appendix Exhibit 2,13 most practices were able to incorporate many model components, but actual transformation at the practice level often did not occur. For example, many practices implemented disease registries without reconfiguring work processes to use them effectively for population management, such as identifying all patients with asthma and proactively suggesting that they obtain influenza vaccination.
To become medical homes, practices need to see themselves as organizations that apply the four pillars of primary care to the needs and preferences of patients in their communities, rather than as organizations that process patients for the convenience of physicians. As collaborative care teams are established and services are better coordinated across the larger health care neighborhood, structures and processes within practices need to encompass a broader set of proactive, population-based, integrated activities for patients, groups of patients, and eventually entire defined populations. For most practices, this represents a major paradigm shift.
Although the implementation methods of the national demonstration project had notable strengths, the short time frame and the rush to get model components in place made it challenging for the facilitators to pay attention to the practices’ internal relationship systems—such as interpersonal communication, trust, and respectful interaction. Rushing to get model components in place without paying attention to relationship systems has a downstream cost that is likely to be counterproductive in the long haul.
To succeed as medical homes and be good citizens of the health care neighborhood, practices need to be nimble; capable of continuous learning; and adept at self-assessment, reflection, and improvisation.15 We suggest that implementation models begin with assessing to what degree practices have these features and thus have an inherent capability to change. For more typical practices that are less informed or motivated than those in the national demonstration project, it is likely that facilitators will be even more important in transforming practices than was the case for practices in the demonstration.
NEW COGNITIVE MODELS
New cognitive models are required for innovative care teams. We learned from the national demonstration project how difficult it is for practices to truly innovate with “care teams”—clinicians working together, depending on the patient’s needs, and not always including a physician-leader. Care teams require physicians working in tandem with other clinicians, such as nurses, nurse practitioners, and physician assistants. Transformation to team-based care requires that primary care physicians and other health professionals envision new roles for themselves and that practices incorporate new paradigms of how best to care for patients. Both of these challenges are more difficult than anyone had imagined.
The task of primary care has expanded many-fold since its resurgence in the 1960s. In addition to a wide range of preventive and wellness services, the escalating burden of chronic illness, obesity, and sedentary lifestyles requires behavioral approaches. Furthermore, the growing prevalence of mental health and substance abuse issues requires innovative, team-based primary care. The primary care activities required of medical homes have simply outrun the ability of any one discipline to single-handedly provide comprehensive care.
Most primary care physicians work on a cognitive model that emphasizes their autonomy in commanding a staff to support their work of advising and treating individual patients within private, face-to-face encounters. New ways of thinking about primary care will need to emphasize working within more collaborative teams and using multiple channels of care such as tele-medicine, e-visits, and group visits. The focus will need to expand from individual patients to encompass populations. A more partnering relationship with patients and much greater transparency will also be required. The latter may involve sharing all health care information, including communication among specialty consultants, with the patient.
Similarly, the current practice paradigm largely views team-based care as physicians’ delegating tasks to others to streamline the work of the practice and make the physician more efficient. Instead, medical homes need to embrace teams that work virtually and “asynchronously.” For example, teams should form around patients’ needs, using effective communication and collaboration that may be enhanced electronically and may not require face-to-face contact. Practices need to work this way internally and in interactions with the health care neighborhood, and they should coordinate care to meet patients’ varied and changing needs and preferences.
In the national demonstration project, we found that changing roles was perhaps most difficult for physicians, who believed deeply that primary care doctoring was based on a strong, trusting relationship between a patient and a physician. Sharing that relationship with other practice staff members was, for many, a significant challenge to their identity as physicians.
There is much to honor and preserve in the rich heritage and values of healing relationships between primary care physicians and their patients. Fulfilling the task of primary care in the medical home, however, now asks physicians to work in new ways, in care teams that can improvise to respond to varied and changing patient needs and preferences. To achieve a national transformation to medical homes, thousands of primary care physicians will need assistance from their professional organizations in understanding and adopting new ways of practicing.
ADAPTIVE RESERVE
We learned from the national demonstration project that a rapid pace of implementation can quickly overwhelm a practice’s ability to manage the complex changes required. Although most practices appeared to be functioning well at baseline, the unrelenting pressure for constant change led to “change fatigue,” which was manifested as faltering progress, unresolved tension and conflict, burn-out and turnover, and both passive and active resistance to further change.
The more successful practices had an internal capability for organizational learning and development. We labeled this capability the “adaptive reserve.”1,2,16 It includes the nature of leadership within the practice (shared and facilitative versus centralized and authoritarian); an aligned management model in which clinical care, practice operations, and financial functions share a consistent vision of the practice; and healthy relationships within the practice. The latter includes rich communication, a shared sense of trust, and a shared commitment to protecting regular time for reflection.
The components of adaptive reserve are highly interrelated. For example, facilitative leadership may result in rich communication, empowering staff to identify and suggest new ideas and to feel secure enough to raise concerns about the varied effects of changes.
Adaptive reserve is not a constant property of a practice; it needs ongoing attention and replenishment.1,2,16 A critical role of an external change agent—such as a facilitator—in any implementation model is to assist the practice in periodically assessing and strengthening its adaptive reserve.
COMPLICATED TECHNOLOGY
Information technology is not “plug and play.” The practices in the national demonstration project appeared to be early adopters of electronic health records. Seventy-one percent had such records in place at baseline, and most of the others implemented them during the two years of the project.
A clear strategy of the project’s implementation team was to put in place further technological enhancements such as registries, e-prescribing, and patient portals. This proved more difficult than originally envisioned because the health IT currently marketed to primary care practices resembles a jumble of jigsaw pieces rather than components of an integrated and interoperable system.
To be effective, medical homes need to coordinate care across hospitals, specialty offices, nursing homes, and social services agencies. This requires more of health IT than merely moving data from one site to another. Health ITmust support virtual and asynchronous communication and must provide rich communication and decision support among the care teams, consultants, and patients.
Given the poor interoperability of current health IT and its limited ability to support the complex integrating and prioritizing functions of primary care, we suggest that practices develop a technology plan that does not necessarily start with an electronic health record. Practices might begin with e-prescribing, electronic data sharing with local hospitals, decision support in the examining room, disease registries, and interactive patient web portals. Later, practices can link these pieces with fully interoperable electronic health records that support relationships and complex decisions.2
Implications For Health Reform
BUILDING HEALTH CARE NEIGHBORHOODS
To meet diverse and comprehensive patient needs, medical homes need to have robust and collaborative relationships with hospitals, nursing homes, specialists, other health care professionals, and community agencies. This integrated neighborhood must appear seamless to the patient.17 Rather than a system that asks medical homes to keep patients from falling through the cracks, a health care neighborhood should coordinate and integrate care and eliminate the cracks. The pillars of primary care, particularly comprehensiveness and coordination, cannot be achieved in a disconnected system.
Linking the resources that make up the health care neighborhood brings new challenges to health IT. In addition to making data available across the neighborhood, the technology must facilitate continuity and coordination and must provide the capability for real time and asynchronous communication among care teams both within practices and across the neighborhood, involving the patient as well.
Even if it were possible to “fix” primary care in isolation by creating a medical home, placing it back into a disorganized health care neighborhood would only invite further dysfunction and frustration. The concept of an accountable care organization has emerged as a particular way to create a neighborhood by explicitly bringing together payers and clinician groups to collectively share risk and bring accountable care to a given population.18,19
To be successful, the medical home must evolve in collaboration with the larger neighborhood, as is envisioned by accountable care organizations. Similarly, these organizations need the primary care foundation that a medical home can provide.20 This requires a concerted national effort and the political will to invest in long-term system development instead of promising a quick, single-stroke fix.
REDESIGN AND PAYMENT REFORM
Various physician payment reform strategies are being discussed. They provide options for a staged approach that supports the transformation of small primary care practices to medical homes.21–23 A developmental approach consists of interrelated changes in three domains, or levels, combined with payment options that will support each one (Exhibit 1).
In the first level are a set of medical home model components that, although difficult for practices to adopt, can be added incrementally to the current practice model, as shown in the national demonstration project (see Appendix Exhibit 1).13 It is unlikely that large numbers of less motivated practices can make these changes without up-front support. This can come in the form of enhanced fee-for-service or robust performance payments, or both.
Second-level changes require changes in people’s identities, roles, and cognitive models. This is where many national demonstration project practices faltered (as illustrated in Appendix Exhibit 2).13 At the second level, bundled payment for episodes of ambulatory care could incentivize the identity shifts required and enable development of more-functional care teams for planned, proactive, population-based care.
The third level of development requires a shift in the paradigm of primary care practice and promotes integration within functional health care neighborhoods. At this level, practices must transform themselves into highly nimble organizations that work seamlessly as part of the local health care neighborhood to contribute to the health of defined populations. Accomplishing the third level will require support and risk-sharing incentives in the form of global payments.
Conclusions
The national demonstration project provides timely and invaluable lessons about on-the-ground promises and challenges of practice redesign and the medical home. It shows that highly motivated practices can implement many of the model components in a relatively brief time frame of two years.
Nevertheless, it also suggests that transformation to a patient-centered medical home, focused on optimizing the four pillars of primary care, is a long-term proposition and much more than a series of incremental improvements made over two years. Despite the huge current federal investment in expanding health IT and achieving “meaningful use,” much of the technology is not ripe for use, and interoperability within practices and across health care neighborhoods has not been demonstrated.
Development of meaningful care teams also implies major changes in the ways individuals and groups within practices view their roles and the ways they work together. Accomplishing these dramatic changes requires ongoing and relentless dedication to improvement that challenges the adaptive reserve of even the most robust practice.
Addressing each of these lessons by themselves requires significant time and effort. Because they are interdependent, an implementation process needs to address all four lessons together, bringing an even greater challenge.
Furthering the development of patient-centered medical homes in small, independent primary care practices will require a nurturing policy environment that sets reasonable expectations and time frames for iterative innovations. Instead of focusing on individual practices and a “just do it” approach, medical homes need to be conceptualized and developed as part of integrated health care neighborhoods requiring long-term commitments and perhaps three to five years of external assistance. Getting there will require synchronizing practice redesign with reimbursement reform. It will require innovation in health systems design and the courage to take collective action to improve the health of the American people.
Acknowledgments
The American Academy of Family Physicians provided funding support for this evaluation, including a Research Center grant. The evaluation was also partially supported by the Commonwealth Fund, a national, private foundation based in New York City that supports independent research on health care issues and makes grants to improve health care practice and policy. The views presented here are those of the authors and not necessarily those of the Commonwealth Fund, its directors, officers, or staff. Kurt Stange was supported in part by the Harry and Elsa Jiler American Cancer Society Clinical Research Professorship. The authors express their appreciation for the cooperation and dedication of the physicians and staff of the family practices that participated in the national demonstration project. The authors make up an independent evaluation team under contract with the American Academy of Family Physicians. The terms of the contract gave the authors complete discretion for evaluating and disseminating findings of the national demonstration project without review or permission by the Academy. The national demonstration project was designed and implemented by TransforMED LLC, formerly a division, and now a wholly owned subsidiary, of the American Academy of Family Physicians.
Contributor Information
Paul A. Nutting, Professor of family medicine and the director of research at the Center for Research Strategies, University of Colorado Health Sciences Center, in Denver
Benjamin F. Crabtree, Director of research, Department of Family Medicine, at the University of Medicine and Dentistry of New Jersey, in Somerset
William L. Miller, Chair of the Department of Family Medicine at the Lehigh Valley Health Network, in Allentown, Pennsylvania
Kurt C. Stange, Professor of family medicine at Case Western Reserve University, in Cleveland, Ohio
Elizabeth Stewart, Senior scientist and director of evaluation at the American Academy of Family Physicians National Research Network, in Leawood, Kansas.
Carlos Jaén, Chair of the Department of Family and Community Medicine, University of Texas Health Sciences Center, in San Antonio.
NOTES
- 1.Miller WL, Crabtree BF, Nutting PA, Stange KC, Jaen CR. Primary care practice development: a relationship-centered approach. Ann Fam Med. 2010;8(Suppl):s68–79. doi: 10.1370/afm.1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nutting PA, Miller WL, Crabtree BF, Jaen CR, Stewart EE, Stange KC. Initial lessons from the first national demonstration project on practice transformation to a patient-centered medical home. Ann Fam Med. 2009;7:254–60. doi: 10.1370/afm.1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rosenthal TC. The medical home: growing evidence to support a new approach to primary care. Am Board Fam Med. 2008;21(5):427–40. doi: 10.3122/jabfm.2008.05.070287. [DOI] [PubMed] [Google Scholar]
- 4.Starfield B. Primary care: concept, evaluation, and policy. New York (NY): Oxford University Press; 1992. [Google Scholar]
- 5.Starfield B, Shi LY, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457–502. doi: 10.1111/j.1468-0009.2005.00409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Milbank Q. 1996;74(4):511–44. [PubMed] [Google Scholar]
- 7.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: the Chronic Care Model, part 2. JAMA. 2002;288:1909–14. doi: 10.1001/jama.288.15.1909. [DOI] [PubMed] [Google Scholar]
- 8.Reid RJ, Coleman K, Johnson EA, Fishman PA, Hsu C-C, Soman MP, et al. The Group Health medical home at year two: cost savings, higher patient satisfaction, and less burnout for providers. Health Aff (Millwood) 2010;29(5):835–43. doi: 10.1377/hlthaff.2010.0158. [DOI] [PubMed] [Google Scholar]
- 9.Bayliss EA, Phillips WR, editors. Leawood (KS): AAFP; 2010. Annals of Family Medicine supplement: evaluation of the American Academy of Family Physicians’ patient-centered medical home national demonstration project [Internet] [cited 2011 Feb 2]. Available from: http://www.annfammed.org/content/vol8/Suppl_1/ [Google Scholar]
- 10.Martin JC, Avant RF, Bowman MA, Bucholtz JR, Dickinson JR, Evans KL, et al. The Future of Family Medicine: a collaborative project of the family medicine community. Ann Fam Med. 2004;2(Suppl 1):S3–32. doi: 10.1370/afm.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stewart EE, Nutting PA, Crabtree BF, Stange KC, Miller WL, Jaen CR. Implementing the patient-centered medical home: observation and description of the national demonstration project. Ann Fam Med. 2010;8(Suppl 1):s21–32. doi: 10.1370/afm.1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.TransforMED. The TransforMED patient-centered model [Internet] Leawood (KS): TransforMED; 2008. [cited 2010 Dec 16]. Available from: http://www.transformed.com/pdf/TransforMEDMedicalHomeModel-letter.pdf. [Google Scholar]
- 13.To access the Appendix, click on the Appendix link in the box to the right of the article online.
- 14.Nutting PA, Crabtree BF, Stewart EE, Miller WL, Palmer R, Stange KC, et al. Effect of facilitation on practice outcomes in the national demonstration project of the patient-centered medical home. Ann Fam Med. 2010;8(Suppl 1):s33–44. doi: 10.1370/afm.1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Crabtree BF, Miller WL, McDaniel RR, Jr, Stange KC, Nutting PA, Jaen CR. A survivor’s guide for primary care physicians. J Fam Pract. 2009;58(8):E1–7. [PMC free article] [PubMed] [Google Scholar]
- 16.Nutting PA, Crabtree BF, Miller WL, Stewart EE, Stange KC, Jaen CR. Journey to the patient-centered medical home: a qualitative analysis of the experiences of practices in the national demonstration project. Ann Fam Med. 2010;8(Suppl 1):s45–56. doi: 10.1370/afm.1075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fisher ES. Building a medical neighborhood for the medical home. N Engl J Med. 2008;359(12):1202–5. doi: 10.1056/NEJMp0806233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McClellan M, McKethan AN, Lewis JL, Roski J, Fisher ES. A national strategy to put accountable care into practice. Health Aff (Millwood) 2010;29(5):982–90. doi: 10.1377/hlthaff.2010.0194. [DOI] [PubMed] [Google Scholar]
- 19.Shortell SM, Casalino LP, Fisher ES. How the Center for Medicare and Medicaid Innovation should test accountable care organizations. Health Aff (Millwood) 2010;29(7):1293–98. doi: 10.1377/hlthaff.2010.0453. [DOI] [PubMed] [Google Scholar]
- 20.Rittenhouse DR, Shortell SM, Fisher ES. Primary care and accountable care—two essential elements of delivery system reform. N Engl J Med. 2009;361(24):2301–3. doi: 10.1056/NEJMp0909327. [DOI] [PubMed] [Google Scholar]
- 21.Mechanic RE, Altman SH. Payment reform options: episode payment is a good place to start. Health Aff (Millwood) 2009;28(2):w262–71. doi: 10.1377/hlthaff.28.2.w262. [DOI] [PubMed] [Google Scholar]
- 22.Guterman S, Davis K, Schoen C, Stremikis K. Reforming provider payment: essential building block for health reform. New York (NY): Commonwealth Fund; 2009. [Google Scholar]
- 23.Berenson RA, Rich EC. US approaches to physician payment: the construction of primary care. J Gen Intern Med. 2010;25(6):613–8. doi: 10.1007/s11606-010-1295-z. [DOI] [PMC free article] [PubMed] [Google Scholar]