Abstract
There is ample scientific evidence to support the importance of gender issues in health and illness. If we fail to take such sex and gender differences sufficiently into account, this will affect the quality of health care provided to men and women, and this is precisely what good medical education means to prevent. In this paper examples are given that show how knowledge, attitudes and skills relating to sex and gender can be implemented in both optional and compulsory courses. Next, factors that can facilitate or impede the implementation of gender specific medical education are described. Finally, the author discusses what needs to be done to educate future physicians that are equipped with appropriate expertise to deal with aspects of gender in medicine.
Introduction
Medical education generally confines itself to specific sex-based reproductive function disorders, such as pregnancy, infertility, birth control, menstrual disorders, and prostate disorders when it deals with differences between men and women. However, there is growing awareness that biological differences between the sexes comprise many more issues than this small set of reproductive functions [1]. There is an increasing body of evidence, for instance, to show that men and women differ in terms of the incidence, symptom presentation, symptoms, and prognosis of many other health issues, such as STDs, HIV/AIDS, cardiovascular diseases, Chronic Obstructive Pulmonary Disease (COPD), depression, anxiety disorders, and auto-immune disorders. Gender blindness in medicine means many physicians are unaware that a great deal of existing medical knowledge is founded on knowledge of the male body as the prototype of the human body [2].
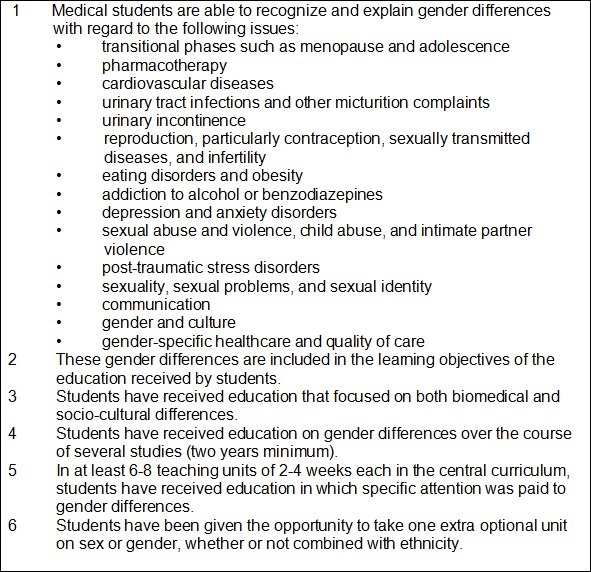
Health differences between the sexes, besides being related to biological differences, are also related to psychological, social and cultural factors [3]. Some examples of additional differences between male and female patients include risk factors, the development of gender identity, the life cycle, communication and the consequences of diseases and their treatment. If we fail to take such sex and gender differences sufficiently into account, this will affect the quality of health care provided to men and women, and this is precisely what good medical education means to prevent. Therefore, we have drafted a list of conditions, based on medical literature, interviews with experts and personal experiences, which successful integration of sex and gender in the medical curriculum needs to meet (see Figure 1 (Fig. 1)).
Figure 1. Characteristics of the successful integration of gender into the basic medical curriculum.
In this paper, I will first give some examples showing how knowledge, attitudes and skills relating to sex and gender can be implemented in medical education. Then I will outline which facilitating and impeding factors are involved in implementing gender-specific medical education. Finally, I will discuss what needs to be done to prepare future physicians for being able to handle aspects of gender in medicine expertly.
Sex and gender in the medical curriculum: some exemples
Both optional and compulsory curricula offer plenty of scope for implementation of sex and gender: the optional curriculum may help to profile specific gender themes, and the core curriculum may integrate gender-specific aspects into regular medical education.
Profiling sex and gender in the optional curriculum
We recently developed an optional course, aiming for students not only to acquire knowledge of gender differences in epidemiology, manifestation and treatment of diseases, but also to expand their awareness of how gender shapes individual behaviour, thought and prejudice. In addition, this course focuses on developing skills for bringing gender-specific medical aid into practice, drawing on a body of multi-disciplinary medical knowledge supplied by lecturers specializing in general practice, sexology, gynaecology, urology, anatomy, psychiatry and health law.
Important themes in this course are the role of gender in diseases, the relation between identity development and gender and the influence of the students’ own socialization on the doctor-patient relationship. Students write an autobiographical essay on their socialization into manhood/womanhood. They practise the main attributes of gender-specific medical aid on purpose-trained simulation patients. They acquire knowledge and skills relating to gender and sex differences in sexual function and dysfunction [4]. They also learn to identify indicators of sexual abuse and specific disorders, such as post-traumatic stress disorder. Finally, students are encouraged to examine their own attitudes towards topics such as homosexuality, sexual coercion and setting up boundaries in the execution of professional practice. To conclude the course, all students hold a presentation on one of these topics.
Throughout the course, there is a mix of theory and observation in the GP’s and gynaecologist’s practice, reflection and hands-on skills practising and personal and professional levels. This optional course was evaluated as one of the top-scoring courses at the Nijmegen University Medical Centre [5].
Integrating sex and gender into the core curriculum
All compulsory parts of medical core curricula deal with angina pectoris and alcohol abuse. Both these disorders are now supported by a body of evidence-based sex and gender differences, which may serve as examples to illustrate the importance of gender in everyday practice. I will first mention some of these differences and then indicate how they can be incorporated into the medical curriculum.
Angina pectoris
Coronary heart diseases occur some ten to fifteen years later in women than they do in men because endogenous oestrogen levels in the reproductive phase delay the onset of atherosclerosis. In diagnosing angina pectoris in women, therefore, physicians must be aware of gender differences in symptom presentation as women present typical angina pectoris complaints less frequently. First of all, angina pectoris in women either does not involve chest pain at all, or the chest pain may be obscured by other complaints [6], [7], such as dyspnoea upon exertion, fatigue, dizziness and nausea. Secondly, if angina pectoris in women does manifest itself by way of chest pain, this pain tends to be less typical and more often an unpleasant feeling somewhere in the chest, which does not disappear within ten minutes in rest nor upon administration of nitroglycerine [8].
Because the symptomatology of angina pectoris in women may be fuzzy, we have produced a risk profile to improve diagnostics of coronary diseases in women, and I will list the main gender differences in risk factors. The first is diabetes mellitus: diabetes elevates risk of coronary heart disease by a factor two in men and by a factor four in women [9], [10]. Taking into account the high prevalence of diabetes mellitus in older women, this makes diabetes the number one risk factor for cardiovascular diseases in women [11], [12]. Smoking constitutes a major risk of coronary ischaemia in both sexes, but it is an even more serious threat to women. Women over 35 who smoke and take oral contraception, moreover, run a ten times higher risk of myocardial infarction than women of the same age who neither smoke nor take oral contraception. Diagnosing angina pectoris in women, therefore, requires knowledge of differences in symptom presentation. We deal with all such aspects of knowledge in lectures, study assignments, tutorials, and test questions.
Another factor involved is that women themselves tend to underestimate their risk of coronary diseases and, consequently, consult their GPs later than men [13]. Physicians in their turn also tend to be slower in relating chest pain in women to coronary diseases, even more so if women present symptoms in emotional rather than matter-of-fact ways [14]. Women are also given exercise ECG and coronary angiography tests less frequently and receive therapy in line with prevailing guidelines less often [15]. Apparently, physicians work on the basis that angina pectoris in women is of an innocent nature. We discuss such stereotypical assumptions in seminars as telling examples for reflection on gender stereotyping in medicine.
Alcohol abuse
Alcohol abuse is three to five times as prevalent in men as in women. Women have a greater biological susceptibility to alcohol as they have lower body weight, smaller livers, relatively more body fat than water and lower alcoholhydrogenase (enzyme) levels, all of which slow down the decomposition of alcohol in the body and elevate risk of liver and brain damage.
It is not easy to detect alcohol abuse. Indicators in women may include menstrual complaints, abdominal pain, sexual issues, and irregular use of contraception. Female alcohol addicts also tend to evoke repugnance: drunken females, and, even more so, drunken mothers, are considered more reprehensible than drunken men.
The functions of alcohol intake are also different in women and men. Women drink to be able to sustain an unsatisfactory relationship, to dispel loneliness, to boost self-confidence, to feel more feminine and to soften the painful impact of maltreatment or sexual abuse. Men drink to control others, to be aggressively dominant, to save their face, to regulate their emotions and to improve their achievements. One might say that, in both sexes, alcohol serves to reinforce a gender-stereotyped self-image of femininity or masculinity [16].
Alcohol abuse may be concomitant with or caused by mental disorders. In men, alcohol can mask underlying depression; in women, it often goes hand in hand with an anxiety disorder. Another important difference is that male alcohol addicts generally have non-drinking spouses who take care of them, whereas half the female addicts have partners that are also addicts, which seriously disrupts their lives and their family life. Alcohol-abusing men are often violent and tend to engage in abuse against their partners [17].
The consequences, finally, are also different: in women, we mainly find intra-psychological problems such as guilt and shame; in men, we find more clashes with the outside world, such as work-related conflicts (dismissal), brawls, and incidents involving penal law (traffic offences).
In summary, men and women show different help-seeking behaviours and ways of coping with complaints and diseases, and alcohol abuse is a fine example for dealing with such sex and gender differences in coping strategies. The indicators, functions, and consequences of alcohol abuse are different in men and women, and awareness of these differences is essential for future physicians and can be integrated into the medical curriculum in a variety of ways
Impeding and facilitating factors in implementing gender into medical education
One of the main research findings relating to medical education is that a predominantly biological curriculum orientation impedes the implementation of gender [18], [19], [20], [21]. A biological perspective leaves contextual factors out of consideration, whereas, in a gendered perspective, health and illness are regarded as products of the interaction between biological processes and living conditions of men and women.
Teachers commonly do not have sufficient knowledge of health-related gender issues [22]. This underscores the importance of teacher training and the development of new gender-sensitive educational programmes. We also need teachers that are content experts and that can serves as enthusing advocates [19]. If education managers and teachers consider gender issues in medicine as biased feminist issues that have no scientific merit, the implementation of gender will be up against major opposition. Gender blindness (non-awareness of the fact that a great deal of knowledge is based on research performed in men) and andronormativity (the male serving as the norm and the female as the deviation from this norm) are the major impediments to securing greater exposure for gender issues.
Motivated course coordinators, on the other hand, who have developed awareness of gender differences in their own physicians’ practice, are the main facilitators of gender issues in their medical teaching. This requires extra efforts aiming to pass on information to medical students as long as gender remains an underexposed topic in medical textbooks [23]. An invaluable aid in successful implementation of gender issues is that their importance be recognized at the policy level and that authority figures in the medical faculty visibly promote the theme [24]. It is also clear that female teachers are more gender-aware than male teachers, which urges the necessity of fostering alliances between female teachers and male managers [20]. It goes without saying that male teachers also need to be made more gender-aware.
Accessible teaching materials, finally, are a vital practical support for time-stressed teachers. Such materials, offering tailor-made translations of gender differences into concrete patient care and inspiring teaching methods, are greatly valued and widely used.
The future
It will take some time for sex- and gender-aware thought and action to be structurally embedded in medical education as learning outcomes. Therefore, gender must be included as a criterion in educational quality policies to prevent gender-specific education from remaining altogether noncommittal.
There are two gender-related themes that have so far remained underexposed. First of all, physicians need to reflect more on their own position as physicians and on their own development as men and women in a given culture. This will help to nurture their competence to empathize with other people’s stories and help them. Secondly, the scientific education of medical students should focus much more on the importance of gender and diversity for assessing and performing research projects. They should also acquire gender-specific knowledge in order to be able to ask appropriate scientific questions.
It will also be clear, finally, that the development of gender-specific medicine and a diversity-aware attitude is not complete once students have obtained their Master’s degrees in medicine but needs to be carried on into advanced medical education offering specialist programmes. To this end, some educational programmes have also been launched and evaluated favourably [25], [26], [27].
Conclusion
There is ample scientific evidence to support the importance of gender issues in health and illness. Sex- and gender-based knowledge, attitudes and skills must be part and parcel of the curriculum and quality-monitoring processes in medical education, either in the optional or in the core curriculum. An abundance of good practices is currently available, and to implement these, it is important to integrate biological aspects with psychosocial contexts in teaching programmes. This implementation process will be encouraged if staff and teachers are aware that teaching on gender issues is based on scientific knowledge. At the policy level, finally, the importance of gender needs to be actively advocated, which requires funding for teaching support and teacher professionalization.
The author
Prof. Dr. T. Lagro-Janssen, PhD, is professor Womens’studies Medicine, Department Primary and Community Care, Radboud University Medical Center, Nijmegen, the Netherlands.
References
- 1.Wizemann TM, Pardue ML. Exploring the Biological contribution to Human Health. Does sex matter? Washington: National Academic Press; 2001. [PubMed] [Google Scholar]
- 2.Lagro-Janssen T. Sex, Gender and Health: Developments in Research. Eur J Womens Stud. 2007;14(1):9–20. doi: 10.1177/1350506807072314. Available from: http://dx.doi.org/10.1177/1350506807072314. [DOI] [Google Scholar]
- 3.Lagro-JanssenT, Lo Fo Wong S, van den Muijsenbergh M. The importance of gender in health problems. Eur J Gen Prac. 2008;14(Suppl 1):33–37. doi: 10.1080/13814780802436127. [DOI] [PubMed] [Google Scholar]
- 4.Lagro-Janssen T. De integratie van de factor sekse binnen het basiscurriculum Geneeskunde. TSG. 2002;4:269–271. [Google Scholar]
- 5.Radboud University Nijmegen. Annual Evaluation Optional Courses Medicine (internal report) Nijmegen: Radboud University; 2005-2006 and 2006-2007. [Google Scholar]
- 6.Elsaesser A, Hamm CW. Acute coronary syndrome: the risk of being female. Circulation. 2004;109(5):565–567. doi: 10.1161/01.CIR.0000116022.77781.26. Available from: http://dx.doi.org/10.1161/01.CIR.0000116022.77781.26. [DOI] [PubMed] [Google Scholar]
- 7.McSweeney JC, Cody M, O’Sullivan P, Elberson K, Moser DK, Garvin BJ. Women’s early warning symptoms of acute myocardial infarction. Circulation. 2003;108(21):2619–2623. doi: 10.1161/01.CIR.0000097116.29625.7C. Available from: http://dx.doi.org/10.1161/01.CIR.0000097116.29625.7C. [DOI] [PubMed] [Google Scholar]
- 8.Douglas PS, Ginsburg GS. The evaluation of chest pain in women. N Eng J Med. 2004;334:1311–1315. doi: 10.1056/NEJM199605163342007. Available from: http://dx.doi.org/10.1056/NEJM199605163342007. [DOI] [PubMed] [Google Scholar]
- 9.Wiersma JJ, TripMD, Piek JJ. Behandeling van patiënten met diabetes mellitus type 2 en tevens coronair hartziekten. Ned Tijdschr Geneeskd. 2006;150:361–365. [PubMed] [Google Scholar]
- 10.Barrett-Connor E, Giardina EG, Gitt AK, Gudat U, Steinberg HO, Tschoepe D. Women and heart disease – The role of diabetes and Hyperglycemia. Arch Intern Med. 2004;164(9):934–942. doi: 10.1001/archinte.164.9.934. Available from: http://dx.doi.org/10.1001/archinte.164.9.934. [DOI] [PubMed] [Google Scholar]
- 11.Lee WL, Cheung AM, Cape D, Zinman B. Impact of diabetes on coronary artery disease in women and men – A meta-analysis of prospective studies. Diabetes Care;23(7):962–968. doi: 10.2337/diacare.23.7.962. Available from: http://dx.doi.org/10.2337/diacare.23.7.962. [DOI] [PubMed] [Google Scholar]
- 12.Mosca L, Appel LJ, Benjamin EJ, Berra K, Chandra-Strobos N, Fabundi RP, Grady D, Haan CK, Hayes SN, Judelson DR, Keenan NL, McBride P, Oparil S, Ouyang P, Oz MC, Mendelsohn ME, Pasternak RC, Pinn VW, Robertson RM, Schenck-Gustafsson K, Sila CA, Smith SC, Jr, Sopko G, Taylor AL, Walsh BW, Wenger NK, Williams CL American Heart Association. Evidence-based guidelines for cardiovascular disease prevention in women. Circulation. 2004;109(5):672–693. doi: 10.1161/01.CIR.0000114834.85476.81. Available from: http://dx.doi.org/10.1161/01.CIR.0000114834.85476.81. [DOI] [PubMed] [Google Scholar]
- 13.Mosca L, Ferris A, Fabunmi R, Robertson RM American Heart Association. Tracking women’s awareness of heart disease: an American Heart Association National Study. Circulation. 2004;109(5):573–579. doi: 10.1161/01.CIR.0000115222.69428.C9. Available from: http://dx.doi.org/10.1161/01.CIR.0000115222.69428.C9. [DOI] [PubMed] [Google Scholar]
- 14.Birdwell BG, Herbers JE, Kroenke K. Evaluating chest pain: the patient’s presentation style alters. The psysician’s diagnostic approach. Arch Intern Med. 1999;153(17):1991–1995. doi: 10.1001/archinte.153.17.1991. Available from: http://dx.doi.org/10.1001/archinte.153.17.1991. [DOI] [PubMed] [Google Scholar]
- 15.Daly C, Clemens F, Lopez Sendon JL, Tavazzi L, Boersma E, Danchin N, Delahaye F, Gitt A, Julian D, Mulcahy D, Ruzyllo W, Thygesen K, Verheugt F, Fox KM Euro Heart Survey Investigators. Gender differences in the management and clinical outcome of stable angina. Circulation. 2006;113(4):490–498. doi: 10.1161/CIRCULATIONAHA.105.561647. Available from: http://dx.doi.org/10.1161/CIRCULATIONAHA.105.561647. [DOI] [PubMed] [Google Scholar]
- 16.Lammers SS. Alcoholverslaving. In: Lagro-Janssen T, Noordenbos G, editors. Noordenbos in Sekseverschillen in ziekte en gezondheid. Nijmegen: SUN; 1997. p. Alcoholverslaving. [Google Scholar]
- 17.Hegarty K, Gunn J. Chondros P, Small R. Association between depression and abuse by partners of women attending general practice: descriptive cross sectional survey. BMJ. 2004;328(7440):621–624. doi: 10.1136/bmj.328.7440.621. Available from: http://dx.doi.org/10.1136/bmj.328.7440.621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hamberg K, Larsson ML. Still far to go - An investigation of gender perspective in written cases used at a Swedish medical school. Med Teach. 2009;31(4):e131–e138. doi: 10.1080/01421590802516806. Available from: http://dx.doi.org/10.1080/01421590802516806. [DOI] [PubMed] [Google Scholar]
- 19.Verdonk P, Mans LJ, Lagro-Janssen AL. Integrating gender into a basic medical curriculum. Med Educ. 2005;39(11):1118–1125. doi: 10.1111/j.1365-2929.2005.02318.x. Available from: http://dx.doi.org/10.1111/j.1365-2929.2005.02318.x. [DOI] [PubMed] [Google Scholar]
- 20.Verdonk P, Benschop YW, De Haes JC, Lagro-Janssen AL. Making a gender difference: case studies of gender mainstreaming in medical education. Med Teach. 2008;30(7):e194–e201. doi: 10.1080/01421590802213206. Available from: http://dx.doi.org/10.1080/01421590802213206. [DOI] [PubMed] [Google Scholar]
- 21.Phillips SP. Evaluating women’s health and gender. Am J Obstet Gynecol. 2002;187(3Suppl):S22–S24. doi: 10.1067/mob.2002.127366. Available from: http://dx.doi.org/10.1067/mob.2002.127366. [DOI] [PubMed] [Google Scholar]
- 22.Lagro-Janssen T, Noordenbos G. Sekseverschillen in ziekte en gezondheid. Nijmegen: Sun; 1997. [Google Scholar]
- 23.Dijkstra AF, Verdonk P, Lagro-Janssen AL. Gender bias in medical textbooks: examples from coronary heart disease, depression, alcohol abuse and pharmacology. Med Educ. 2008;42(10):1021–1028. doi: 10.1111/j.1365-2923.2008.03150.x. Available from: http://dx.doi.org/10.1111/j.1365-2923.2008.03150.x. [DOI] [PubMed] [Google Scholar]
- 24.Celik H, Abma TA, Widdershoven GA, van Wijmen FC, Klinge I. Implementation of diversity in healthcare practices: barriers and opportunities. Patient Educ Couns. 2008;71(1):65–71. doi: 10.1016/j.pec.2007.11.021. Available from: http://dx.doi.org/10.1016/j.pec.2007.11.021. [DOI] [PubMed] [Google Scholar]
- 25.Celik HH, Kling I, Weijden TT, Widdershoven G, Lagro-Janssen T. Gender sensitivity among general practioners: Results of a training programme. BMC Med Educ. 2008;26:8–36. doi: 10.1186/1472-6920-8-36.. Available from: http://dx.doi.org/10.1186/1472-6920-8-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dielissen PW, Bottema BJ, Verdonk P, Lagro-Janssen AL. Incorporating and evaluating an integrated gender-specific medicine curriculum: a survey study in Dutch GP training. BMC Med Educ. 2009;9:58. doi: 10.1186/1472-6920-9-58. Available from: http://dx.doi.org/10.1186/1472-6920-9-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dielissen PW, Bottema BJ, Verdonk P, Lagro-Janssen TL. A training to teach gender specific medicine curriculum: a survey study in Dutch GP training. BMC Med Educ. 2009;9:58. doi: 10.1186/1472-6920-9-58. Available from: http://dx.doi.org/10.1186/1472-6920-9-58. [DOI] [PMC free article] [PubMed] [Google Scholar]


