Implementation of computerized provider order entry for complex chemotherapy regimens supported Memorial Sloan-Kettering Cancer Center's strategic plan to successfully establish a distributive, networked health care delivery system.
Abstract
Implementation of a computerized provider order entry system for complex chemotherapy regimens at a large cancer center required intense effort from a multidisciplinary team of clinical and systems experts with experience in all facets of the chemotherapy process. The online tools had to resemble the paper forms used at the time and parallel the successful established process as well as add new functionality. Close collaboration between the institution and the vendor was necessary. This article summarizes the institutional efforts, challenges, and collaborative processes that facilitated universal chemotherapy computerized electronic order entry across multiple sites during a period of several years.
Introduction
Government-sponsored incentives established through the Health Information Technology for Economic and Clinical Health Act have prompted many institutions to implement electronic health records (EHRs) at their facilities.1,2 There is debate in the literature as to whether or not EHRs improve efficiency.3–5 However, it has been shown that medication error rates are reduced when computerized provider order entry (CPOE) and clinical decision support systems are used.6 Memorial Sloan-Kettering Cancer Center's (MSKCC) effort to transition to an electronic record began in the early 1990s. In 2003, after phased implementation of the EHR and the CPOE, attention focused on chemotherapy order entry and online verification.7,8 Implementation of CPOE for multidrug chemotherapy and biologic therapy regimens that use a variety of dosing formulas can be extremely complex. This endeavor would have a particularly significant impact on practice at MSKCC, given that the annual number of chemotherapy doses had grown to exceed 150,000 by 2003 and that many patients receive potentially toxic high-dose or investigational therapies. It was therefore critical that this CPOE functionality be precisely designed and implemented.
Goals
Implementation of the electronic chemotherapy order sets would provide a safe and more efficient ordering method for patients receiving complex treatment regimens. The online tools had to resemble the paper forms at the time and parallel the successful established process as well as add new functionalities, such as automated dose calculation and online verification, to improve patient safety. Orders would no longer be illegible, incomplete, or lost; all of which would result in decreased wait times for patients. Although design and development would be complicated, the end product would be a system that would be easier to use for all involved in the chemotherapy process—from prescribers entering orders to verification nurses, pharmacists verifying and preparing the drugs, and nurses administering the treatment. The system would also be accessible remotely for those prescribing or reviewing the regimens. Standards of care would be established and incorporated into developed chemotherapy order sets. With a wholly electronic system in place, data would be retrievable to use for resource management, strategic planning, and quality assessment.
Planning
A multidisciplinary group was formed to provide input from both management and end users into the design, workflows, and testing of the new system. Members consisted of a Systems Project Manager (S.G.), clinical systems analysts, experienced verification nurses, chemotherapy pharmacists, treating nurses, operational managers and medical oncologists, including the Director of Chemotherapy Practice (N.T.S), a GI oncologist with a high-volume practice (E.M.O'R.), and the Lymphoma Service Chief, who had computer programming experience (A.D.Z.). The team reported to an executive committee that included the Physician-in-Chief, Chair of the Department of Medicine, Senior Vice President/Hospital Administrator, Chief Nursing Officer, and Director of Pharmacy Services. The cost of the project fell under the institution's strategic planning efforts to establish a complete electronic system for all medication, diagnostic, and consultative orders. Investigational orders would be implemented along with standard regimens, but pediatric treatments were felt to present unique challenges and would be the last group to implement the system after gaining system usage experience in the adult patient services.
Workflow Development
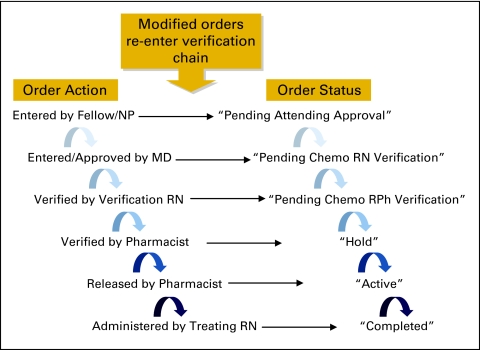
Over the years, MSKCC had developed safe workflows for chemotherapy ordering, verification, preparation, and administration. The team sought to recreate this successful process in an entirely electronic format with two major goals in mind: inefficiencies inherent to a paper process could be eliminated by eradicating the need to hand carry orders between buildings, by consolidating numerous outpatient and inpatient workflows into one standard process, and by providing remote access to prescribers and verification staff; patient safety would be improved through functions such as automatic dose calculations and decision support such as electronically limiting available route options for certain drug orders (eg, vincristine).9,10 Security rights to enter chemotherapy orders would be electronically limited to licensed independent practitioners—including physicians, nurse practitioners, and fellows—with expertise in the management of malignancies. Orders placed by a fellow or nurse practitioner would require approval by an attending physician. Once placed, chemotherapy orders would enter a queue with the verification statuses clearly visible on the forms and changing in real-time as the order is processed along the verification chain (Fig 1). Each order set would accommodate all or part of one cycle of therapy and could include several days or weeks of therapy as mapped out by the regimen (Fig 2). All of the orders in a given regimen would be approved together as a set. If there were any questions regarding the order, the conversation with the physician would be documented in a “Proceed with Chemotherapy” order placed in the system directly or as a verbal order by a licensed independent practitioner to a nurse or a pharmacist. Orders requiring modification would automatically restart the verification process once adjusted. Nurses would be allowed to cancel orders if a patient did not show up for an appointment or if instructed to do so by a fellow or attending, but nurses would not be able to change dates or originate orders.
Figure 1.
Chemotherapy (chemo) order verification chain. MD, medical doctor; NP, nurse practitioner; RN, registered nurse; RPh, registered pharmacist.
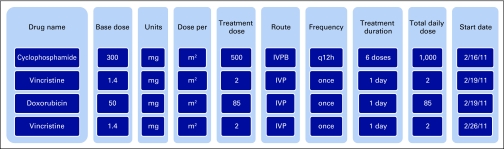
Figure 2.
Example order set. IVP, intravenous push; IVPB, intravenous piggyback; q12h, every 12 hours.
System Requirements
The team developed a list of essential functionalities to be incorporated into the ordering and verification processes. Eclipsys (now Allscripts, Chicago, IL), the CPOE software vendor, had a medical oncologist on staff with both clinical and software development experience and was able to collaborate closely with MSKCC to create a customized order entry form that was easy to use and that mirrored the paper order in both appearance and function. The product also needed to be flexible enough to allow for on-site configurability by the institution's systems team. Table 1 lists characteristics of the order entry form.
Table 1.
Characteristics of the Order Entry Form
| Characteristic | Description |
|---|---|
| Multiorder grid | Multidrug chemotherapy regimens can be prescribed on one form in which each row represents a separate electronic order. |
| Order dependency | Orders in the grid are linked to each other. |
| Height/weight | Data feeds in from a separate centralized functionality and cannot be changed directly on the order. |
| Built-in calculators | Dosing formulas include those per m2, per kg, flat dose, and area under the curve. |
| Data modifiers include ideal body weight and adjusted/ideal body weight. | |
| Dosing can be capped for individual drugs in specified regimens. | |
| Dose rounding is automated per predefined rules. | |
| Total daily dose | Total daily dose is calculated and displayed on form. |
| Dose modifications | Doses can be adjusted by fixed percentages. |
| Reasons for modification are indicated on the form. | |
| Relevant results policy | Applicable laboratory results specific to the service are displayed on the form. |
| Regimen modification | Chemotherapy agents within the order set can be added or removed on the fly. |
| Prescribing limitations | Administration routes and units can be restricted for each drug. |
| Associated orders | Standard antiemetics and hydration can be ordered by clicking one check box. |
| Relative dates | Subsequent doses can be placed relative to the date of first dose (eg, T + 7). |
| Verification chain | Orders feed sequentially to attending, verification registered nurse, pharmacy (Fig 2). |
| Order statuses | Statuses appear on grid with automatic real-time updates. |
| Advanced orders can be kept in “hold” status until required to be released. |
Clinical Decision Support Features
To improve the safety of the chemotherapy process, several automated safety checks and orders were configured into the system (Table 2). Applicable recent lab results were displayed on the order form along with predefined treatment parameters. The majority of order sets were built with defaulted base doses, which automatically calculated the treatment dose when the form was opened. Rules were created for automated dose rounding, with approval obtained from various external research groups. Calculated treatment doses of individual chemotherapy agents could be capped at the regimen level. Physicians could copy and reorder an entire chemotherapy order set for a subsequent cycle of therapy, thereby reducing dose transcription errors. Providers could toggle directly from the order form to the pharmacy system, which displays previously dispensed therapy. Investigational order sets included a link to the online copy of the research protocol. Height and weight were patient-specific values entered into the EHR and could not be modified directly on the orders. In addition, the system alerted the ordering physician to absolute and percentage changes in height and weight when the physician reordered an active regimen. The clinician could then choose whether to use the old or new values to calculate doses for the current treatment. Dose modifications could be applied to each individual drug in the set, and the reason for modification could be selected from a drop-down list on the order form.
Table 2.
Safety and Decision Support Features Incorporated Into Chemotherapy CPOE
| Feature |
|---|
| Predefined regimens and base doses |
| Acceptance of generic drug names only |
| Use of Tallman lettering for drug names |
| Weight change alert |
| Automatically calculated doses |
| Ability to incorporate capping of doses for specific drug |
| Maximum dose checking in pharmacy module |
| Automatically calculated dose modifications |
| Restriction of routes of administration and units choices for each drug |
| Recent lab results on order form |
| Allergy and drug-drug interaction alerts |
| Duplicate order alert |
| Access to pharmacy system to view prior dispensed doses |
| Direct link to investigational protocols from order form |
| Alert if chemotherapy drug discontinued after last cycle was ordered |
| Ability to copy entire order set forward to next cycle without “rewriting” |
| Implementation of standard supportive medication and hydration order sets |
Abbreviation: CPOE, computerized provider order entry.
Rather than having to place individual antiemetic and hydration orders, a check box order for the institution's “Standard antiemetics and hydration” prompted the pharmacist to enter regimen-specific supportive medications. The existing basic system alerts, such as medication interactions and allergy checking, were extended to include chemotherapy agents. Although we were careful not to cause “alert-fatigue,” selected additional warnings, such as duplicate order alerts, were built into the system. Although pre- and postrollout data was not tracked, all of these measures significantly decreased the frequency of phone calls from the verification and pharmacy staff to the physicians, thus minimizing distractions that could have been a contributing factor to making errors. Therefore, these clinical decision alerts were expected to not only improve patient safety but also improve efficiency and decrease wait times for the patients.
Order Set Development
As a large cancer center with more than 150 oncologists, MSKCC's services are each composed of malignancy-specific physician experts. Medical oncologists from each service—including service chiefs or their designees who had previously helped develop preprinted paper orders—were asked to be the point physicians to create the online order sets, be a resource for others, and champion the system to their team. In addition to the features mentioned above and outlined in Figure 2, the forms included the regimen name, diagnosis, on/off research study indication, protocol number, and parameters for treatment. Other fields included the start date, regimen notes, and drug details as well as the ability to modify the base dosage by percentages and to indicate the reason for dose modification.
Initial versions of the order sets were generated from hundreds of predefaulted paper regimen forms that had been developed over the years, and additional sets were added after review by the disease services. The opportunity was taken to establish and incorporate standard management approaches within and across disease teams when possible. To organize the forms so that they could be found easily in the system, a naming convention was established that would start with the service title and then include the regimen name and any descriptors. A group that included the service physician, the verification nurse, the research nurse, the pharmacist, the treatment nurse, the chemotherapy practice director, and the assistance of the systems analysts was granted remote access to the test environment, and the group reviewed all order sets in detail, both as individual members and then together as a group before loading the order set. Several permutations of the common regimens generally in use were built to minimize potential errors that might arise during real-time modifications of the order sets. Medications were listed on the form in the order of administration, according to the MSKCC's nursing policies and as listed on the institution's online chemotherapy guidelines reference page. To supplement the ability to remove drugs from or add drugs to existing regimens, a decision was made to create a blank order set with blank lines for chemotherapy agents to achieve the flexibility necessary to tailor treatment to each patient's needs.
Implementation
By 2006, the system was built, validated with scenario-based testing, and ready for use in the clinical environment. A pilot to test the order entry functionality was conducted by one physician in the lymphoma service clinic. The online verification functionality was added and validated in a second pilot in a busy GI oncologist's practice. During the pilots, the implementation team met regularly to review feedback from the participants and then incorporated suggested changes to the workflow and system design.
One of the key elements of successful implementation was the establishment of a clear mandate that only electronic orders would be accepted after the rollout, so no clinicians could opt out of its use. Once the pilot was completed, news of its success spread across that service, and other GI oncologists were not averse to trying it out. The system was then introduced sequentially, on a service-by-service basis, given that MSKCC medical oncology teams consisted of five to 20 physicians, and each team required development of more than 100 service-specific order sets. Development of a service's electronic regimens began while the previous team rolled out. Compliance with training was assured, because individual physicians were granted access rights to the chemotherapy order forms only after they underwent one-on-one training by a systems analyst. Then, during the first week of each rollout, a group of systems analysts provided in-clinic support to the prescribers and verification staff. One feature that clinched physician buy-in and helped to smooth the rollout process was the ability they had to copy and reorder regimens for the next cycle.
After completion of the disease-specific rollouts, MSKCC's regional network sites, whose physicians were not limited to treating only one cancer grouping, started to use the whole array of electronic order sets. The process was then mirrored for the various disease-specific pediatric oncology services after a separate pediatric chemotherapy order form was created.
System Outcomes
The regular meetings continue, although less frequently, with anticipated completion of the institutional roll-out by the second quarter of 2011. To date, more than 1,250 conventional and investigational order sets for adults and 466 for pediatric patients have been created. In 2010, 73,225 order sets were placed by more than 416 practitioners, (attendings, fellows, and nurse practitioners) at eight sites for more than 150,000 chemotherapy visits and more than 225,000 doses of chemotherapy.
New order sets are created when requested by the specific services as new drugs and regimens are developed, in preparation for clinical trials in parallel to protocols being submitted to the institutional review board for review, or in response to drug shortages when substitutions become necessary. These order sets are reviewed by the multidisciplinary review group via e-mail and can be loaded within a short time frame if necessary. All order set usage is reviewed every 6 months, and sets are inactivated if deemed no longer useful by the service. Fewer than 1% of orders per year are placed using blank order sets. The institution's chemotherapy guidelines web content is regularly reviewed alongside the order sets to ensure that the listed regimens match those in use.
Data are readily available directly from system reports and reviews of the process are ongoing. Actual and “near-miss” chemotherapy events are reported through the institution's quality assessment online Reporting for Safety and Quality (RISQ) system and analyzed for events such as “wrong dose” or “wrong frequency.” Event rates are calculated by dividing the number of events by the institution's volume of dispensed chemotherapy doses. These data are then analyzed by a chemotherapy practice committee subgroup to look for patterns highlighting processes that need improvement. As a result of these reviews, alerts now warn prescribers of patient weight changes of more than 10% and unfulfilled pretreatment requirements, such as pregnancy testing. Numbers of illegible or lost orders were not tracked in the past, but they were the source of many delays and much discord between physicians and verification staff. These issues have disappeared since implementation of the online system, and a drop from 197 to 77 incomplete orders that were reported was noted between 2008 and 2009.
Challenges continue to exist, given that no system can be completely flexible; prescribers need to be constantly vigilant and not be lulled into a secure feeling that the system will catch all errors.11 At present, cumulative dose information only exists in the pharmacy system and is viewable by all clinicians. In addition, the pharmacy system generates an automatic alert for the pharmacist regarding cumulative anthracycline dosages, but this will be available in the ordering system when we convert to the vendor's pharmacy system this year. Using automated area under the curve–based formulas for carboplatin dosing and reordering can sometimes be difficult because doses may change in response to fluctuations in renal function. In addition, recently published US Federal Drug Administration guidelines for formula-based capping of doses need to be incorporated into the system, which requires development of additional functionality by the systems analysts.
Lessons Learned
Implementation of a CPOE for complex chemotherapy regimens supported MSKCC's strategic plan to successfully establish a distributive networked health care delivery system. The project took several years of intense design and effort from a multidisciplinary team of clinical and systems experts who spent hundreds of hours on this endeavor. Close collaboration between the institution and the vendor was necessary to develop a customized and configurable order form with functionality to match and improve upon the established process. However, mapping of existing workflows was necessary before new process standards could be established. A clear mandate and ease of use were crucial factors in obtaining buy-in and compliance from the clinical staff as was the involvement of end users in evaluation of the system's functionality. Selection of a physician-champion from each service was essential, and rolling out one service at a time—together with individual training for each physician—allowed for a smoother conversion to the online system. We learned as well that the completion of a system's implementation is never done. Once established, an electronic system needs constant monitoring and must have the flexibility to respond to quality improvement efforts, new treatment modalities, and changing clinical standards.
Acknowledgment
We thank all the staff members at Memorial Sloan-Kettering Cancer Center without whose commitment, years of work, and dedication to patient care this project would not have been successful. There are too many to mention individually, but they include pharmacists, nurses, nurse practitioners, physicians, operational managers, and systems analysts.
Authors' Disclosures of Potential Conflicts of Interest
The authors indicated no potential conflicts of interest.
Author Contributions
Conception and design: Nancy T. Sklarin, Svetlana Granovsky, Andrew Zelenetz
Collection and assembly of data: Nancy T. Sklarin
Manuscript writing: Nancy T. Sklarin, Svetlana Granovsky, Eileen M. O'Reilly, Andrew Zelenetz
Final approval of manuscript: Nancy T. Sklarin, Svetlana Granovsky, Eileen M. O'Reilly, Andrew Zelenetz
References
- 1.One Hundred Eleventh Congress of the United States of America, The American Recovery and Reinvestment Act of 2009, Title XIII, Heath Information Technology. 2009:138. [Google Scholar]
- 2.Blumenthal D, Tavenner M. The “meaningful use” regulation for electronic health records. N Engl J Med. 2010;363:501–504. doi: 10.1056/NEJMp1006114. [DOI] [PubMed] [Google Scholar]
- 3.Cheriff AD, Kapur AG, Qiu M, et al. Physician productivity and the ambulatory EHR in a large academic multi-specialty physician group. Int J Med Inform. 2010;79:492–500. doi: 10.1016/j.ijmedinf.2010.04.006. [DOI] [PubMed] [Google Scholar]
- 4.Boonstra A, Broekhuis M. Barriers to the acceptance of electronic medical records by physicians from systemic review to taxonomy and interventions. BMC Health Services Res. 2010;10:231. doi: 10.1186/1472-6963-10-231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Amusan AA, Tongen S, Speedie SM, et al. A time-motion study to evaluate the impact of EMR and CPOE implementation on physician efficiency. J Healthc Inf Manag. 2008;22:31–37. [PubMed] [Google Scholar]
- 6.Collins CM, Elsaid KA. Using an enhanced oral chemotherapy computerized provider order entry system to reduce prescribing errors and improve safety. Int J Qual Health Care. 2011;23:36–43. doi: 10.1093/intqhc/mzq066. [DOI] [PubMed] [Google Scholar]
- 7.Sklarin NT, Granovsky S, Hagerty-Paglia J. Implementation of an electronic health record at an academic cancer center: Lessons learned and strategies for success. Am Soc Clin Oncol Ed Book. 2011:411–415. [Google Scholar]
- 8.Owens K. EMR Implementation: Big bang or a phased approach. J Med Pract Manage. 2008;23:279–281. [PubMed] [Google Scholar]
- 9.Brokel JM, Harrison MI. Redesigning care processes using an electronic health record: A system's experience. Jt Comm J Qual Patient Saf. 2009;35:82–92. doi: 10.1016/s1553-7250(09)35011-4. [DOI] [PubMed] [Google Scholar]
- 10.Baker DK, Hoffman JM, Hale GA, et al. Analysis of patient safety: Converting complex pediatric chemotherapy ordering processes from paper to electronic systems. In: Henriksen K, Battles JB, Keyes MA, et al., editors. Advances in Patient Safety: New Directions and Alternative Approaches—Vol 2: Culture and Redesign. Rockville, MD: Agency for Healthcare Research and Quality; 2008. pp. 1–13. [PubMed] [Google Scholar]
- 11.Campbell EM, Sittig DF, Ash JS, et al. Types of unintended consequences related to computerized provider order entry. J Am Med Inform Assoc. 2006;13:547–556. doi: 10.1197/jamia.M2042. [DOI] [PMC free article] [PubMed] [Google Scholar]