Responses to a 2010 survey by LIVESTRONG showed that, compared with the general population, persons affected by cancer had greater enthusiasm for electronic information exchange between patients and health care providers. Especially valued were security and privacy of communication.
Abstract
Purpose:
The Health Information Technology for Economic and Clinical Health (HITECH) Act has placed an emphasis on electronic health information exchange (EHIE). Research on needs of patient, especially those touched by cancer, has been sparse. Here, we present data on preferences for EHIE among those touched by cancer compared with a nationally representative sample of American adults.
Methods:
Two surveys were used: an online survey designed by LIVESTRONG (the Lance Armstrong Foundation) and a dual-frame, nationally representative sample of adults collected through the National Cancer Institute's Health Information National Trends Survey (HINTS).
Results:
The LIVESTRONG EHIE survey yielded a sample of 8,411 respondents, including 433 currently receiving cancer treatment, 298 living with cancer as a chronic disease, 2,343 post-treatment survivors, and 5,337 with no history of cancer. The HINTS sample consisted of 7,674 respondents representative of the general adult population. Comparisons revealed a strong positive view of the value of EHIE within the cancer-relevant groups, especially among those living with cancer as a chronic disease. Only about half of the general population showed a similar degree of enthusiasm for EHIE. When asked about specific functions for EHRs, respondents valued privacy and security above all, followed by improving care coordination and data sharing between providers.
Conclusion:
These data suggest that the EHIE needs among those touched by cancer may be greater than in the general population. This is particularly important because people affected by cancer are among those who access our health care system most frequently and who have the most at stake.
Introduction
Policy and practice related to electronic health information exchange (EHIE) are rapidly changing, most notably affected by implementation of the Health Information Technology for Economic and Clinical Health (HITECH) Act of 2009. The HITECH Act makes use of American Recovery and Reinvestment Act funds to stimulate the adoption and “meaningful use” of electronic heath records (EHRs).1,2 The meaningful use criteria are intended to increase health care provider use of—and patient access to—electronic health information by attaching reimbursement structures to adoption of EHRs.3,4
Ultimately, EHIE is intended to improve the quality and safety of patient care and to enable patients to be more active participants in their health care.5 However, a better understanding of patient attitudes and preferences regarding EHIE is needed to keep EHIE policy and practice patient centered.6 People affected by cancer offer an excellent model for studying perspectives on health care initiatives, such as EHIE, across a disease trajectory.7 In this brief article, we provide perspectives on EHIE among people affected by cancer, including those in treatment, post-treatment, and living with cancer as a chronic illness, and compare their perspectives with those of the American public.
Methods
Participants and Procedures
LIVESTRONG EHIE survey.
In April 2010, LIVESTRONG advertised an electronic survey on EHIE to registered constituents through e-mail, Facebook, and Twitter. In addition, in an effort to reach people outside of the constituent population, LIVESTRONG posted a blog with a link to the survey on the Avon/Love Army of Women Web site. These new media techniques reflect a growing trend among cancer researchers to exploit the participative aspects of technology to drive recruitment.8 As of August 2010, 8,564 persons had completed the survey, 8,411 of whom were included in the present study (respondents who did not report sociodemographic data were excluded; n = 153). Survey responses were completed anonymously. The survey protocol was reviewed and approved by the Western Institutional Review Board.
Health Information National Trends Survey 2008.
The Health Information National Trends Survey (HINTS) is a biennial survey performed by the National Cancer Institute that provides publicly available, nationally representative data on the adult American public's attitudes and knowledge regarding cancer prevention and control, with an emphasis on health information technology.9,10 The third iteration of the survey took place between January and May 2008 and used a dual-frame sample design that combined responses from a traditional random digit dial, computer-assisted telephone interview (n = 4,092) with responses from a mailed, self-administered paper and pencil survey (n = 3,582). The dual-frame design has been shown to improve survey coverage for individuals who maintain cellular telephones but do not have landlines.11 Further details on methodology and response rates can be found elsewhere.12,13
Measures
LIVESTRONG EHIE survey.
The LIVESTRONG survey included content in three areas: perspectives on the importance of EHIE and its potential impact on quality of care; respondents' willingness to share their electronic health data for the purposes of research; and preferences related to specific functional capabilities of EHRs. A full copy of the LIVESTRONG EHIE survey can be found online (http://livestrongblog.org).
HINTS 2008.
HINTS items that measured perspectives on the importance of EHIE and respondents' willingness to share their electronic health information for the purposes of research were used in the present study. In addition, both surveys measured sociodemographic data including age, sex, race, and number of visits to a health care provider in the past 12 months. Full copies of the HINTS instruments and technical information on data characteristics can be found online (http://hints.cancer.gov).
Analytic Approach
So that perspectives on EHIE can be appreciated across the cancer spectrum, results of the LIVESTRONG EHIE survey are presented for four distinct groups: people with a personal history of cancer who are currently receiving treatment, people with a personal history of cancer who have finished primary treatment, people living with cancer as a chronic illness, and people with no personal history of cancer. Where the LIVESTRONG survey was harmonized with HINTS, comparisons are provided for nationally representative estimates.
Results
Table 1 shows the respondents' sociodemographic characteristics and perspectives on the importance of (1) their providers being able to share health information electronically, (2) their ability to retrieve their own health information electronically, and (3) their willingness to share their anonymous health information for the purposes of research. Respondents to the LIVESTRONG EHIE survey attached significant value to their health care providers being able to share electronic health information and to their ability to retrieve their own health information electronically. Approximately half of the American public viewed these activities as “very important,” whereas percentages among the LIVESTRONG survey respondents ranged from 82% to 68% and were particularly high among respondents receiving treatment for cancer or living with cancer as a chronic illness. Those in treatment and those who classified themselves as cancer survivors also reported the most visits to a health care provider in the past 12 months; as such, they may be acutely aware of the potential benefits of EHIE.
Table 1.
Sociodemographic Characteristics and Views on Electronic Health Information Exchange
| Characteristic | Survivors on Treatment (n = 433) | Living With Cancer As a Chronic Illness (n = 298) | Post-Treatment Survivors (n = 2,343) | No Personal History of Cancer (n = 5,337) | General Adult Population HINTS (n = 7,674) |
|---|---|---|---|---|---|
| Age, years | 66.7% between 40 and 64 | 68.5% between 40 and 64 | 71.7% between 40 and 64 | 65.8% between 40 and 64 | 52% between 35 and 64 |
| Sex, % female | 70.5 | 65.7 | 69.6 | 56.6 | 51.4 |
| Race, % white | 94.0 | 95.0 | 93.1 | 88.9 | 76.1 |
| Five or more visits to a health care provider in the past 12 months, % | 85.0 | 82.4 | 55.3 | 37.0 | 25.5 |
| “Very important” that my health care providers are able to share my medical information with each other electronically, % | 79.8 | 82.1 | 75.4 | 68.7 | 47.9 |
| “Very important” that I can get my own medical information electronically, % | 75.1 | 81.1 | 70.8 | 69.5 | 51.7 |
| “Strongly agree” that scientists doing research should be able to review my medical information if the information cannot be linked to me personally, % | 59.4 | 70.4 | 60.0 | 55.9 | 32.4 |
Abbreviation: HINTS, Health Information National Trends Survey.
Survey respondents were also willing to share their anonymous health information for the purposes of research. Nearly one third of the American public “strongly agreed” with this practice, and more than half of respondents to the LIVESTRONG survey did as well (ranging from 55.9% of those with no personal history of cancer to > 70% of individuals living with cancer as a chronic illness).
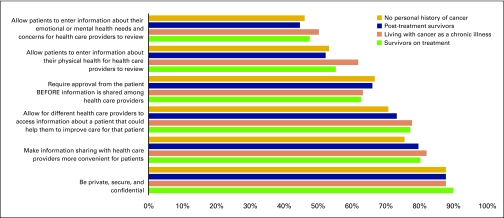
Using data from the LIVESTRONG EHIE survey, Figure 1 shows the perceived importance of different EHR functional capabilities. Nearly all respondents “strongly agreed” that privacy and security are important; > 70% wanted EHRs to make health information sharing with providers more convenient for patients and for multiple health care providers to be able to access the patient's EHR.
Figure 1.
Perceived importance of different functional capabilities of electronic health records.
Most LIVESTRONG EHIE survey respondents wanted the ability to enter their own reports of their physical health into the EHR, and nearly half want the same capability for reports of their emotional health. Most respondents also want patient approval to be required before providers share information via EHIE.
Finally, Table 2 shows that, across the entire study sample, respondents expressed high confidence that EHIE would improve the quality of their health care.
Table 2.
Perceptions of How Electronic Health Information Exchange Will Affect Care
| Perception | Survivors on Treatment | Living With Cancer As a Chronic Illness | Post-Treatment Survivors | Health Care Provider/Professional | No Personal History of Cancer |
|---|---|---|---|---|---|
| Care will improve, % | 86.3 | 84.4 | 85.9 | 84.5 | 84.5 |
| Care will stay the same, % | 11.2 | 12.9 | 11.2 | 11.4 | 11.8 |
| Care will worsen, % | 2.6 | 2.7 | 2.9 | 4.0 | 3.8 |
Discussion
These findings shed light on the similarities and differences in attitudes toward EHIE between a population affected by cancer (surveyed online) and the broader public (survey both on- and offline). Respondents to the LIVESTRONG EHIE survey showed a strong preference for wanting to obtain their own medical information electronically and for endorsing EHIE between their providers. These findings concur with the hypothesized value that EHIE might offer in the context of cancer care, which is often complex and involves multiple providers.14–18 Fewer in the general public recognized the intrinsic value of EHIE. Willingness to share personal data for research was highest among those with a personal history of cancer (ranging from 59.4% to 70.4%) and lower among LIVESTRONG survey respondents without a personal history of cancer (55.9%) and the general population (32.4%). These results are promising as the medical community evaluates ways in which increases in EHIE can be used to create large population-level databases for the purposes of research.
When it came to discussing the perceived importance of functional capabilities of EHRs, respondents to the LIVESTRONG EHIE survey supported data sharing among health care providers, provided that data sharing occurs in a private, secure, and confidential way. This desire to improve care coordination of care may reflect a more realistic view of technology as facilitator, and not a barrier, in meeting personal health goals and gaining an appreciation of the complexity of cancer care.19,20 Finally, approximately half of respondents wanted to enter their own physical and mental health outcomes into the EHR. Studies of using information technology to capture patient-reported outcomes using tools such as previsit e-journals have been evaluated positively by patients and providers.21
It should be noted that the LIVESTRONG sample is limited to people with Internet access and does not represent a random sampling of people affected by cancer. In addition, the differences observed between respondents to the LIVESTRONG EHIE survey and the general public (represented by HINTS) may reflect differences with respect to health history and/or Internet use (even among LIVESTRONG respondents without a personal history of cancer). However, given the 2-year difference in survey dates (LIVESTRONG in 2010; HINTS in 2008) the differences may also reflect changes over time in how people generally think about EHIE amid a dynamic and ever-evolving health information environment.
The data from this study give support to the commentary expressed in Journal of the American Medical Association calling for the development of enhanced capabilities for patient engagement through personal access to electronic health information.22 As policy makers, practitioners, and health information system designers move to instantiate requirements from the HITECH Act while taking patient perspectives into account, these findings suggest that the needs for and preferences related to EHIE among people touched by cancer may be greater than those expressed by the public at large.
Acknowledgment
Supported by the National Cancer Institute and LIVESTRONG. E.B.B. had full access to all the data in the study and takes responsibility for the data and the accuracy of the data analysis.
Portions of these data have been published in a LIVESTRONG report (http://www.livestrong.org/pdfs/3-0/EHIReport) and presented at the ASCO Annual Meeting, June 3-7, 2011, Chicago, IL.
Authors' Disclosures of Potential Conflicts of Interest
The authors indicated no potential conflicts of interest.
Author Contributions
Conception and design: Ellen B. Beckjord, Ruth Rechis, Stephanie Nutt
Provision of study materials or patients: Ruth Rechis
Collection and assembly of data: Ruth Rechis, Stephanie Nutt
Data analysis and interpretation: Ellen B. Beckjord, Ruth Rechis, Stephanie Nutt, Lawrence N. Shulman, Bradford W. Hesse
Manuscript writing: Ellen B. Beckjord, Ruth Rechis, Stephanie Nutt, Lawrence N. Shulman, Bradford W. Hesse
Final approval of manuscript: Ellen B. Beckjord, Ruth Rechis, Stephanie Nutt, Lawrence N. Shulman, Bradford W. Hesse
References
- 1.Blumenthal D. Launching HITECH. New Engl J Med, 2010;362:382. doi: 10.1056/NEJMp0912825. [DOI] [PubMed] [Google Scholar]
- 2.Blumenthal D, Tavenner M. The “meaningful use” regulation for electronic health records. N Engl J Med. 2010;363:501–504. doi: 10.1056/NEJMp1006114. [DOI] [PubMed] [Google Scholar]
- 3.Markel Foundation. New York, NY: Markle Foundation, Center for American Progress, Engelberg Center for Health Care Reform at Brookings; 2009. Demonstrating Meaningful Use of Health IT for 2011 and Beyond. [Google Scholar]
- 4.Office of the Secretary Health and Human Services. HITECH Act (45 CFR Part 160), Federal Register. 2009 [Google Scholar]
- 5.Blumenthal D, Glaser JP. Information technology comes to medicine. N Engl J Med. 2008;356:2527–2534. doi: 10.1056/NEJMhpr066212. [DOI] [PubMed] [Google Scholar]
- 6.Simborg DW. Consumer empowerment versus consumer populism in healthcare IT. J Am Med Inform Assoc. 2010;17:370–372. doi: 10.1136/jamia.2010.003392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rowland JH, Bellizzi KM. Cancer survivors and survivorship research: A reflection on today's successes and tomorrow's challenges. Hematol Oncol Clin North Am. 2008;22:181–200. doi: 10.1016/j.hoc.2008.01.008. [DOI] [PubMed] [Google Scholar]
- 8.Fox S. Washington, DC: Pew Research Center; 2010. Cancer 2.0: A Summary of Recent Research. [Google Scholar]
- 9.Nelson DE, Kreps GL, Hesse BW, et al. The Health Information National Trends Survey (HINTS): Development, design, and dissemination. J Health Comm. 2004;9:443–460. doi: 10.1080/10810730490504233. [DOI] [PubMed] [Google Scholar]
- 10.Finney Rutten L, Hesse BW, Moser RP, et al., editors. Cresskill, NJ: Hampton Press; 2010. Building the Evidence Base in Cancer Communication. [Google Scholar]
- 11.Link MW. Implications of cell phone usage in survey research for informing communication research and practice. In: Finney Rutten L, Hesse BW, Moser RP, et al., editors. Building the Evidence Base in Cancer Communication. Cresskill, NJ: Hampton Press; 2010. pp. 61–72. [Google Scholar]
- 12.Hesse BW, Moser RP, Rutten LJ. Surveys of physicians and electronic health information. N Engl J Med. 2010;362:859–860. doi: 10.1056/NEJMc0909595. [DOI] [PubMed] [Google Scholar]
- 13.Chou YW, Hunt YM, Beckjord EB, et al. Social media use in the United States: Implications for health communication. J Med Internet Res. 2009;11:e48. doi: 10.2196/jmir.1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hesse BW, Hanna C, Massett HA, et al. Outside the box: Will information technology be a viable intervention to improve the quality of cancer care? J Natl Cancer Inst Monogr. 2010:81–89. doi: 10.1093/jncimonographs/lgq004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bloomrosen M, Detmer DE. Informatics, evidence-based care, and research: Implications for national policy: A report of an American Medical Informatics Association health policy conference. J Am Med Inform Assoc. 2010;17:115–123. doi: 10.1136/jamia.2009.001370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jacobs LA, Palmer SC, Schwartz LA, et al. Adult cancer survivorship: Evolution, research, and planning care. CA Cancer J Clin. 2009;59:391–410. doi: 10.3322/caac.20040. [DOI] [PubMed] [Google Scholar]
- 17.Landier W. Survivorship care: Essential components and models of delivery. Oncology (Williston Park) 2009;23:46–53. [PubMed] [Google Scholar]
- 18.Oeffinger KC, McCabe MS. Models for delivering survivorship care. J Clin Oncol. 2006;24:5117–5124. doi: 10.1200/JCO.2006.07.0474. [DOI] [PubMed] [Google Scholar]
- 19.Taplin S, Massett H, Lillie S, et al. Taking HINTS: Understanding users' needs in order to achieve the potential of information technology in cancer care delivery. In: Finney Rutten L, Hesse BW, Moser RP, et al., editors. Building the Evidence Base in Cancer Communication. Cresskill, NJ: Hampton Press; 2010. pp. 271–295. [Google Scholar]
- 20.Hesse BW, Shneiderman B. eHealth research from the user's perspective. Am J Prevent Med. 2007;32(suppl):S97–S103. doi: 10.1016/j.amepre.2007.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wald JS, Businger A, Gandhi TK, et al. Implementing practice-linked pre-visit electronic journals in primary care: Patient and physician use and satisfaction. J Am Med Inform Assoc. 2010;17:502–506. doi: 10.1136/jamia.2009.001362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Krist AH, Woolf SH. A vision for patient-centered information systems. J Am Med Inform Assoc. 2011;305:300–301. doi: 10.1001/jama.2010.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]