Five years after implementation of a full paperless electronic health record within a four-hospital care system, the system's oncology practice is experiencing significant improvements in safety, efficiency, and research productivity in both inpatient and outpatient settings.
Abstract
The electronic health record (EHR) was adopted into the NorthShore University HealthSystem, a four-hospital integrated health system located in suburban Chicago, in 2003. By 2005, all chemotherapy and medicine order entry was conducted through the EHR, completing the incorporation of a fully paperless EHR in our hospital-based oncology practice in both the inpatient and outpatient settings. The use of the EHR has dramatically changed our practice environment by improving efficiency, patient safety, research productivity, and operations, while allowing evaluation of adherence to established quality measures and incorporation of new quality improvement initiatives. The reach of the EHR has been substantial and has influenced every aspect of care at our institution over the short period since its implementation. In this article, we describe subjective and objective measures, outcomes, and achievements of our 5-year EHR experience.
Introduction
NorthShore University HealthSystem (NorthShore; Evanston, IL) is a four-hospital integrated health care system located in the northern suburbs of Chicago with 8,000 employees and 2,100 physicians on the medical staff, including 700 in the faculty group practice. The institution has more than 1 million office visits per year, and also has a large integrated research institute. NorthShore functions as the principal teaching affiliate of the University of Chicago Pritzker School of Medicine.
The Kellogg Cancer Center (KCC) was started in 1981 as a single outpatient center at Evanston Hospital (Evanston, IL). Additional KCCs were added at Glenbrook Hospital (Glenview, IL) in 1987, and at Highland Park Hospital (Highland Park, IL) in 2000. Medical oncology care is provided by 14 members of the NorthShore University HealthSystem Medical Group Hematology/Oncology Division, as well as several independent groups and practitioners. Three gynecologic oncologists and three neuro-oncologists also practice at the KCCs, and several surgeons and other practitioners see patients at KCCs as part of multidisciplinary clinics. This article will mainly focus on the experience of the 14-member medical hematology/oncology division practicing out of the three KCCs.
The electronic health record (EHR), Epic (Epic, Verona, WI), was first implemented in 2003 for inpatient charting and documentation at the Glenbrook, Evanston, and Highland Park Hospitals. In the ensuing months, the same Epic health record was implemented in the outpatient offices affiliated with the practice group (currently 700 members), which included the KCCs. Chemotherapy drug ordering remained paper-based until September 2005, at which time the Beacon Oncology Module was implemented and embedded in the Epic system, and this has since been our sole method for ordering chemotherapy in the outpatient setting. After Beacon implementation, paper was no longer used for charting or the ordering of medications, laboratory, or radiology tests. Additional important milestones for the whole organization included implementation of the Epic record in the offices of some independent practitioners beginning in 2005 (94 independent physicians to date); bar-coding medication administration in 2007; adding a hospital billing module in 2009 and initiation of Epic at the Skokie Hospital in 2009, after its integration into the health system 1 year earlier. Electronic prescribing (e-prescribing) of outpatient medications to a patient's preferred pharmacy was implemented in 2010.
The EHR has significantly affected all operations in outpatient medical oncology at our institution, for health care practitioners and patients alike. This article describes how the EHR affects documentation, communication, and ordering of chemotherapy and focuses on the use of the Epic EHR for operational purposes, quality improvement, and research.
Epic EHR Impact on Documentation and Communication
The same Epic documentation is used for inpatient and outpatient care, facilitating seamless access to notes by inpatient physicians, nursing, and other staff seeking information about outpatient care, and vice versa. A particular value of the EHR in our system has been the opportunity for optimal communication in the multidisciplinary care of patients with cancer. This includes the internal messaging and sharing of laboratory, radiology, and other data between NorthShore oncologists and other health care providers; external communication to primary care physicians, surgical and radiation oncologists, and referring physicians; and routing of information needed for consultation, new appointments, test scheduling, and facilities operations. Our system's NorthShore Connect messaging system allows patients to communicate nonurgent questions or needs directly with their physician and nurse. Patients can also access test results after a physician release (immediate) or an auto-timed release (3 days for most labs, 7 days for most radiology and other procedures), and can access other parts of their medical record. In total, 140,000 patients in the NorthShore system have taken advantage of this feature, and 50.2% of KCC patients seen in April 2011 were enrolled.
Epic EHR–Based Ordering of Chemotherapy
Ordering of chemotherapy is performed via the Beacon module. Our group assisted in the design of this module and acted as a beta testing site. Chemotherapy orders may be written and signed at the time of service, or written and signed ahead of time with prespecified treatment parameters before release. Chemotherapy is tracked electronically within electronic flow sheets; discrete data points can be used for operational, quality, and research purposes as described later in this article.
We have demonstrated that Beacon-based ordering of chemotherapy is more complete than paper ordering and provides a greater level of safety and satisfaction for staff. The outcomes of our study comparing paper charts to the EHR show that using EHR/computerized physician order entry (CPOE) systems improves completeness of the medical record and chemotherapy order documentation (93% v 67% completeness of the components of the chemotherapy order; P < .001) and user satisfaction with the medical record system. The study also highlighted an increase in documented pharmacy interventions in EHR/CPOE charts versus paper charts.1
Epic EHR Effect on Operations and on Meeting Meaningful Use Criteria
Our group has used data from Epic and Beacon extensively for operational uses. This includes optimizing patient scheduling and staffing needs through the use of operational templates. On-demand access to monthly statistical, cost, and revenue reports (itemized by drug, physician, disease site, and treatment plan) provides the ability to evaluate growth, productivity, future staffing needs, inventory management, and budget variances and projections. Dose tracking has facilitated medication use evaluations that have affected patient safety (bevacizumab-induced hypertension), cost containment (rapid rate rituximab, Kras testing for cetuximab) and regulatory adherence (erythropoetic stimulating agents Risk Evaluation and Mitigation Strategies project), billing, and revenue capture.
Epic has been formatted so that documentation completed in the EHR meets Center for Medicare & Medicaid Services Medicare and other carriers' billing requirements with date stamps and electronic signatures. Discrete fields have been built to satisfy billing requirements such as diagnosis, chemotherapy doses, infusion start and stop times, as well as medical necessity for both diagnostic testing and therapeutic agents, and are easily searchable by internal coders as well as external auditors.
We use our EHR to help meet and document many of the required meaningful use criteria as defined by the federal government.2 At each visit, the EHR problem list, patient smoking status, and patient allergy list are reviewed and marked as reviewed. Institutionally and within oncology, we routinely participate in electronic medication reconciliation and have tracked the results for more than a year. Currently, we have > 90% compliance with medication reconciliation in the outpatient oncology setting. We have been providing patients with After Visit Summaries (AVSs; including free-texted patient instructions, updated medication list, upcoming appointments, pending tests, and same-day test results) for more than a year. We currently have a 65% compliance rate, as measured by the most rigorous method- patient recall of receiving an AVS in response to a telephone interview in the days after their visit (and 90% when the measurement is simply electronic tracking of printing the AVS). We implemented e-prescribing institutionally in December 2010 and currently use e-prescribing for all prescriptions in the clinic, with the exception of narcotics and oral chemotherapy agents.
Billing for physician evaluation and management services is performed electronically at the point of service by the physician. This has led to a very short time in account receivable of 30 days.
Epic EHR Impact on Quality and Research
The EHR has been used to support both quality improvement initiatives and research for our cancer center. Within the EHR, data elements, including laboratory values, demographic data, medical history, infusional drug administration, and oral chemotherapy prescriptions, are stored in discrete structured fields and entered into a data warehouse.3 The data warehouse is a clearinghouse for data from the clinical, laboratory, and billing systems for the institution in an Oracle-based platform. Our institution has a robust bioinformatics infrastructure with the ability to generate reports from the data warehouse by using Cognos software as a reporting tool that allows us to address both the process and outcomes of cancer care.
Quality
The KCC oncology pharmacists have taken a leadership role in the use of the Epic EHR for quality improvement (QI), particularly within medical oncology. Since we adopted the Epic EHR in 2003, our oncology pharmacy residents have used the Epic EHR for their annual projects, many of which have focused on QI initiatives (Table 1).1,4–6 These quality projects were either made possible or made more feasible through the Epic EHR.
Table 1.
Oncology Pharmacy Residency Projects That Used the Electronic Health Record
| Year | Resident | Project |
|---|---|---|
| 2006-2007 | Cara Harshberger | Implementation of Electronic Medical Record Evaluation1 |
| 2007-2008 | Abigail Jannazzo | Improving Adherence and Safety of Oral Chemotherapy6 |
| 2008-2009 | Cheryl Jee | Incidence and Management of Bevacizumab-Associated Hypertension in the Outpatient Clinic4 |
| 2009-2010 | Pamela Menas | The Incidence and Management of Arthralgias in Breast Cancer Patients Treated with Aromatase Inhibitors in an Outpatient Oncology Clinic5 |
| 2010-2011 | Shannon Gavin | Oxaliplatin-Induced Hypersensitivity Reactions |
High-Risk Medications
The EHR has been used to monitor high-risk medications, including both infusional and oral therapeutics. Pharmacy and nursing access to real-time notes and patient data allows for optimal communication and monitoring of infusional chemotherapy and for oral chemotherapy drugs when the prescriptions are written electronically.
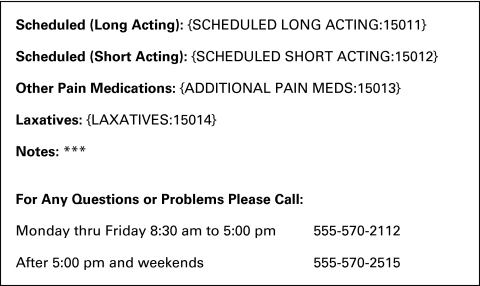
The EHR has been used to standardize and monitor toxicity and symptom management in treatments requiring high-risk medications. For example, pain management discharge instructions have been developed, which are customized and provided to patients after their visit (Figure 1). In addition to improving communication with patients, these instructions are recorded within the EHR, ensuring that the entire care team across both inpatient and outpatient settings is aware of the pain management plan.
Figure 1.
Kellogg Cancer Center pain management discharge instructions, pain management schedule. This instruction sheet can be embedded in discharge instructions given with each encounter. Each category (long acting, short acting, other, and laxatives) is followed by a pull-down menu with drug and dose choices and room for free-text notes.
A major focus of our QI efforts has been improving the safe administration of high-risk medications. Documentation within the EHR has facilitated this process. Treatment plan notes that document the intended dosing and schedule of each chemotherapy agent, as well as the goals of therapy, are required when the treatment plan is generated and are updated when doses are modified. The treatment plan notes are readily visible to all practitioners involved in the treatment of each patient. They provide a valuable communication and validation of physician treatment intention and the actual order and are used to assist in the verification process. Improved access and frequent use of the treatment plan note have reduced the number of unnecessary clarification phone calls and pages between nurses or pharmacists and the ordering physician, which can otherwise delay the start of drug administration.
Potential chemotherapy medication errors are monitored, evaluated trended, and reported to oncology staff on a monthly basis. Over a 6-month period, the treatment plan note enabled pharmacy to identify and prevent five potential dose-modification omissions and errors caused by treatment plan omission or copy/paste issues.
Use of an initial treatment plan note at our Kellogg Cancer Center increased from 11% to 79% of all orders placed within the cancer center over the first 1-year period of required implementation (early 2009- early 2010). Furthermore, on the basis of input from pharmacy staff and physicians and nurses, we created a screen within the EHR called the “Big Picture,” a concise report that provides a readily available and complete longitudinal profile of critical laboratory results, vitals signs, chemotherapy, and supportive care medications.
Treatment plan notes were considered critical by pharmacy, nursing, and physician leadership but created and additional documentation burden beyond the progress note and chemotherapy order. A incentive-based approach was used to overcome initial physician concerns, with a portion of discretionary salary specifically designated during the 12-month development period, to be fully paid only to those physicians who achieved an 80% chemotherapy note completion rate. It became subjectively very clear during this time that the short time investment required by the physician was recouped by fewer pages and interruptions.
Adverse events associated with high-risk medications are tracked within the EHR. We have used the EHR to monitor bevacizumab-related toxicity and to standardize our ordering process and point of order review verification. Consistent with other reports, we found that 31% of our patients experienced bevacizumab-induced hypertension.4 Because of these adverse effects, the required bevacizumab treatment monitoring criteria of a urine protein creatinine ratio (UPC) and blood pressure are now linked to the medication order. This has enabled the pharmacy to identify patients who may be candidates for increased monitoring and treatment of hypertension via our standardized bevacizumab-induced hypertension treatment algorithm. We have also standardized a 6-week time interval for establishing the UPC ratio, eliminating approximately 700 annual urine collections at a cost savings of approximately $44,000. Lastly, in light of reports supporting decreased infusion times for bevacizumab, we have safely reduced the infusion times via a standardized order. Over 6 months, this translated to approximately 300 hours of infusion chair time saved, which greatly benefits patients and conserves health care resources.
Our pharmacists also developed order functionality that has facilitated the dose calculation of carboplatin and other agents that require close monitoring of renal function through serum creatinine and creatinine clearance values (ie, pemetrexed, cisplatin, and zoledronic acid). These values are now readily available and placed in highly visible areas within the EHR to facilitate the ordering process. The standardized functionality for carboplatin dosing enabled the pharmacy to document individual calculations from two separate oncology-credentialed pharmacists. Documentation of the variables used and initials of the two pharmacists increased from a baseline of 60% in the previous system to 99% with the EHR.
An oral chemotherapy project, whose data was generated from Epic, resulted in the development of a dedicated outpatient point of care oncology (POC) pharmacy.6 This project also identified and implemented areas of system improvements, resulting in an increase in oncologist prescribing compliance within the EHR for oral chemotherapy from 21% at baseline to 73% (near 100% now after the study period). As a result, nearly all oral chemotherapy and related data are readily accessible in flow sheets, and discreet data points and can be used for operational, quality, and research purposes. These electronic orders automatically populate the patient medication list and medication flow sheet, thus improving medication reconciliation and helping our clinicians and pharmacists to evaluate drug-drug interactions of oral medications and, as below, facilitating operational and research undertakings.
A POC oncology outpatient pharmacy was established in early 2010 and now is the acquisition source for most of our patients' oral chemotherapy, allowing our pharmacists access to the EHR and on-site patient-pharmacists interaction. More than 50% of oral chemotherapy drugs from the largest KCC, at Evanston Hospital, are now filled at our POC pharmacy. Through our EHR, our POC oncology pharmacists can track when patients start oral chemotherapies and systematically call them 1 week later to assess for adherence and toxicity. On a 5-point survey scale, patient satisfaction with pharmacy services increased from 3.8 at baseline (their prior out-of-hospital or in-hospital, non-POC pharmacy) pharmacy service to 4.9 with the POC pharmacy, 6 months after its implementation.
In addition to the projects noted above, we have also reviewed the safety of reduced-dose pegfilgrastim (4 mg) for patients with breast cancer receiving docetaxel and cyclophosphamide. The retrospective review demonstrated decreased bone pain (odds ratio = 4.99; P = .002) and did not affect febrile neutropenia risk (0% v 0%) compared with 6 mg.
A rapid-rate rituximab performance improvement project resulted in decreased infusion time for second dose rituximab to 90 minutes versus standard titrated infusion with no significant change in reaction rate (3% versus 3.4% internal data).
The EHR facilitated a PI project comparing elastomeric infusion pumps with mechanical (DME pumps), resulting in $47,000 cost savings and improved patient, nursing, and pharmacy preference outcomes.7
A pharmacy-driven anemia management project became possible with documentation capabilities (hemoglobin linked to drug prescription) in the EHR, enabling pharmacists at different location to assess a patient's response to erythropoietin stimulating agent treatment and adherence to institutional and Medicare guidelines.
A laboratory test standardization and cetuximab-induced hypomagnesemia guideline project required pretreatment laboratory results built into each treatment plan and real-time status of the lab accessible to all. A resultant protocol was developed for cetuximab patients for magnesium lab frequency and treatment algorithm.
Lastly, we have utilized the EHR to support the QI initiatives within the Cancer Committee, a hospital professional staff committee charged with cancer oversight and planning and maintaining accreditation. Beginning in the fall of 2010, we enrolled in the ASCO Quality Oncology Practice Initiative, and we are in the process of standardizing our documentation in an effort to facilitate the data abstraction from patient charts required for this program. For example, in our initial survey, we found that fewer than 50% of our notes included adequate documentation of pain assessment by the second visit. This was addressed by education of both physician and nursing staff, as well as a planned update to the clinician note template. The flexibility to customize the template facilitates behavioral change.
Research
The EHR has also been used to support the clinical trial process. Each research team works with Kellogg Pharmacy to generate specific treatment plan templates in Beacon for every protocol before patients are enrolled. The template includes required laboratory tests and specific requirements for administration of investigational and supportive care drugs. In addition, a “Best Practice Alert” is placed in the chart of every patient enrolled onto a clinical trial. This alert serves as a flag to all members of the care team (across both inpatient and outpatient settings) and includes a link to research notes, treatment calendar, protocol, and consent form.
The EHR has also facilitated both retrospective chart reviews and the development of prospective databases within the data warehouse. This has been particularly helpful when studying patients treated with oral therapeutics, which can be difficult in the paper chart setting.8,9 Because oral chemotherapy agents have been ordered through the Epic EHR for many years, reports can be generated that include patients treated with a particular agent over a specified time period with pertinent demographic data and laboratory results, including tumor histology. Several of the research groups within the cancer center have also traditionally used prospective databases that are on other platforms, such as Microsoft Access.10 Data that are within discrete fields can be imported directly from Epic into these other database platforms. In addition, we are in the process of building identically structured fields from existing prospective databases into the Epic data warehouse. Research-specific data (eg, tissue microarray or genomic profiling) will still need to be entered separately via a Web portal.
Need for Ongoing EHR Training
As with any technology, successful use of the Epic EHR utility is highly dependent on the proficiency of the users. To this end, a sound training program for new users is essential, followed by appropriate updates and retraining based on perceived and real deficiencies.11,12 All new faculty members are required to complete an online training module before the first day of practice, followed by a generic half-day classroom session with an Epic trainer and one or two individual sessions in the clinic. In addition to the valuable initial formal training, fellow physicians and other health care providers prove to be invaluable resources, often more valuable than the formal training, which is of necessity broad and generic. Many practical tricks of the trade are learned in this way, often in the clinic. Regular updates are e-mailed with attached relevant screen shots, and Epic trainers are anxious to ensure good understanding of the new material.
Implementation of already available or specifically created functionality requires a concerted effort on the part of individual physicians and leadership. Voluntary implementation from our motivated group is the rule. Tying needed implementations to salary (through discretionary bonus, as was done with implementation of the chemotherapy notes and AVS implementation) or through nonmonetary recognition (eg, praise in e-mails and at meetings) has helped to speed the implementation of tough undertakings.
Conclusion
The full implementation of Epic and Beacon in the inpatient and outpatient setting at NorthShore University Health System KCCs has significantly changed our practice culture. Chemotherapy ordering is more complete and safer. Legibility errors are gone, communication is instantly available from any location, and both outpatient records of hospitalized patients and inpatient records of outpatients are available electronically. We have been able to use Epic and Beacon to meet the meaningful use criteria, as well as for operational and quality and research purposes. Going forward, with the implementation of the institutional data warehouse and informatics group, the data available through the record will allow for extensive and productive research.
Ackowledgment
Presented in part at the Hematology/Oncology Pharmacy Association Annual Conference, Denver, CO, June 14-16, 2007, and at the 41st American Society of Health-System Pharmacists Midyear Clinical Meeting, Anaheim, CA, December 3-7, 2006.
Authors' Disclosures of Potential Conflicts of Interest
The authors indicated no potential conflicts of interest.
Author Contributions
Conception and design: Bruce E. Brockstein, George W. Carro, Janardan Khandekar, Robert de Wilton Marsh
Administrative support: Christine Van De Wege
Collection and assembly of data: Bruce E. Brockstein, Thomas Hensing, George W. Carro, Christine Van De Wege
Data analysis and interpretation: Bruce E. Brockstein, Thomas Hensing, George W. Carro, Christine Van De Wege
Manuscript writing: Bruce E. Brockstein, George W. Carro, Janardan Khandekar, Lynne Kaminer, Christine Van De Wege
Final approval of manuscript: Bruce E. Brockstein, Thomas Hensing, George W. Carro, Jennifer Obel, Janardan Khandekar, Lynne Kaminer, Christine Van De Wege, Robert de Wilton Marsh
References
- 1.Harshberger CA, Brockstein B, Carro G, et al. Evaluation of outcomes before and after electronic medical record (EMR) and computerized physician order entry (CPOE) system implementation in an outpatient oncology setting. ASCO Meeting Abstracts. 2007;25:17058. [Google Scholar]
- 2.Blumenthal D, Tavenner M. The “meaningful use” regulation for electronic health records. N Engl J Med. 2010;363:501–504. doi: 10.1056/NEJMp1006114. [DOI] [PubMed] [Google Scholar]
- 3.Robicsek A, Beaumont JL, Wright MO, et al. Electronic prediction rules for methicillin-resistant Staphylococcus aureus colonization. Infect Control Hosp Epidemiol. 2011;32:9–19. doi: 10.1086/657631. [DOI] [PubMed] [Google Scholar]
- 4.Jee C, Brockstein B, Hui W, et al. Incidence and management of bevacizumab associated hypertension in an outpatient oncology clinic. J Clin Oncol. 2009;(suppl):27. abstr e20677. [Google Scholar]
- 5.Menas P, Merkel D, Carro G, et al. Incidence and management of arthralgias in breast cancer patients treated with aromatase inhibitors in an outpatient oncology clinic. J Clin Oncol. 2010;(suppl):28. doi: 10.1177/1078155211434853. abstr e11062. [DOI] [PubMed] [Google Scholar]
- 6.Harper A, Carro G, Brockstein B, et al. Oral chemotherapy adherence and safety in an outpatient oncology setting. International Society of Oncology Pharmacy Practitioners/Hematology/Oncology Pharmacy Association Annual conference; June 18-21, 2008; abstr TR41. [Google Scholar]
- 7.Carro G, Lawton J, Harper A, et al. Evaluation of elastomeric and electronic medication pumps at an outpatient cancer center. Hematology/Oncology Pharmacy Association Annual conference; 2010; Abstr. [Google Scholar]
- 8.Shah NB, Fidler MJ, Walters KK, et al. Association of epithelial mesenchymal transition (EMT) markers and outcome measures in advanced non-small cell lung cancer (NSCLC) patients treated with erlotinib. J Clin Oncol. 2010;28(suppl):550s. abstr 7550. [Google Scholar]
- 9.Hensing TA, Fidler MJ, Wong F, et al. The association between PTEN expression and survival in patients (pts) with advanced non-small cell lung cancer (NSCLC) treated with erlotinib. J Clin Oncol. 2010;28(suppl):550s. abstr 7552. [Google Scholar]
- 10.Surati M, Robinson M, Nandi S, et al. Generation of comprehensive thoracic oncology database–tool for translational research. J Vis Exp. 2011;22:pii. doi: 10.3791/2414. 2414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lowes R. EMR success: Training is the key. Med Econ. 2004;81:TCP11–TCP4. [PubMed] [Google Scholar]
- 12.Boonstra A, Broekhuis M. Barriers to the acceptance of electronic medical records by physicians from systematic review to taxonomy and interventions. BMC Health Ser Res. 2010;10:231. doi: 10.1186/1472-6963-10-231. [DOI] [PMC free article] [PubMed] [Google Scholar]