Abstract
Background
Reducing blood pressure (BP) after stroke reduces risk for recurrent events. Our aim was to describe hypertension care among veterans with ischemic stroke including BP control by discharge and over the 6 months post stroke event.
Methods and Results
The Office of Quality and Performance Stroke Special Study included a systematic sample of veterans hospitalized for ischemic stroke in 2007. We examined BP control (<140/90 mmHg) at discharge excluding those who died, enrolled in hospice, or had unknown discharge disposition (N=3640, 3382 adjusted analysis). The second outcome was BP control (<140/90 mmHg) within 6-months post-stroke, excluding patients who died /readmitted within 30 days, lost to follow-up or did not have a BP recorded (N=2054, 1915 adjusted analysis). The population was white (62.7 %) and male (97.7%); 46.9% were <65 years of age; 29% and 37% had a history of cerebrovascular or cardiovascular disease, respectively. Among the 3640 stroke patients 1573(43%) had their last documented BP prior to discharge >140/90 mmHg. Black race (adjusted OR 0.77 [95% CI 0.65, 0.91]), diabetes (OR 0.73 [95% CI 0.62, 0.86]) and hypertension history (OR 0.51 [95% CI 0.42, 0.63]) were associated with lower odds for controlled BP at discharge. Of the 2054 stroke patients seen within 6 months from their index event, 673 (32.8%) remained uncontrolled. By 6 months post event, neither race nor diabetes was associated with BP control; whereas history of hypertension continued to have lower odds of BP control. For each 10 point increase in systolic BP > 140 mmHg at discharge, odds of BP control within 6 months post discharge decreased by 12% (95% CI (8%, 18%)).
Conclusions
BP values in excess of national guidelines are common after stroke. Forty three percent of patients were discharged with an elevated BP and 33% remained uncontrolled by 6 months.
Keywords: hypertension, quality of care, secondary prevention, stroke prevention
Reducing patients' blood pressure after a cerebrovascular event has been demonstrated to improve secondary prevention.1 There is a continuous positive relationship between blood pressure (BP) and risk of cardiovascular disease (CVD) events.2 Diet, exercise and treatment with antihypertensive medications have also been associated with reductions in recurrent stroke, myocardial infarction, and vascular events regardless of whether the patient had a history of hypertension.3 However, the extent to which this potential benefit has been realized in routine clinical practice is much less clear. Deficiencies in delivery of secondary prevention and in the quality of care have been noted after incident cardiovascular and cerebrovascular events.4–7
A proposed means to realize the potential benefits of secondary prevention emphasizes treatment initiation at hospital discharge. Organized approaches which initiate secondary prevention medications prior to hospital discharge may improve adherence to guidelines.8–10 Studies suggest that in hospital behavior strongly influences post discharge community practice.11 There is however, increasing evidence that BP among patients with stroke remains poorly controlled after stroke hospitalization leading to high rates of recurrent strokes.6, 12, 13 Although stroke care guidelines provide recommendations regarding the in-hospital initiation of management for some stroke risk factors such as lipids,14, 15 no specific recommendations are made regarding the initiation of antihypertensive agents at hospital discharge. The American Heart Association/American Stroke Association strongly recommends that treatment of hypertension should be instituted after the acute period in patients who have consistently elevated BP.15 Similarly, the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) guidelines suggests that for the stroke patient, hypertension treatment be initiated with an angiotensin converting enzyme inhibitor (ACEI) combined with a thiazide type diuretic, based on the results of the perindopril protection against recurrent stroke study (PROGRESS trial).16
We had a unique opportunity to assess post-stroke BP care among nearly all veterans admitted to a Veterans Health Administration (VHA) facility for an acute ischemic stroke event. This allowed us to address a major gap in the literature regarding the quality of hypertension care and characteristics of high risk veterans admitted with an ischemic stroke. We perceive this to be a critical first step in the potential design of interventions targeted to persons at greatest risk of uncontrolled BP. Our aim was to describe the quality of hypertension care among veterans after hospitalization for an acute ischemic stroke. The quality of hypertension management was assessed on the basis of three outcomes: BP control at discharge, antihypertensive medications prescribed at discharge, and BP control over the 6 months post ischemic stroke event. We hypothesized that certain risk factors including diabetes and multiple co-morbidities would lead to suboptimal BP control among stroke patients at discharge and in the 6 months post discharge. We also hypothesized that the prescription of combination ACEI with a thiazide diuretic at discharge would be associated with better BP control over the 6 months after the acute stroke hospitalization.
METHODS
Study Design, Setting and Data Sources
The Office of Quality and Performance (OQP) Stroke Special Study was a retrospective cohort of veterans admitted to a Veterans Affairs Medical Center (VAMC) in the United States and Puerto Rico during Fiscal Year (FY) 2007 (October 1, 2006 through September 30, 2007) with a primary discharge diagnosis of ischemic stroke, identified using a modified high specificity algorithm17 of the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes (N=5721 possible stroke events). A systematic sample of 5000 medical records was identified, using an approach that included all ischemic stroke patients at VAMCs with 55 or fewer ischemic stroke hospitalizations in FY 2007 and an 80% random sample of ischemic stroke patients at VAMCs with more than 55 ischemic stroke hospitalizations in FY 2007. Because of this sampling strategy, the number of stroke patients per VAMC who were included in this study ranged from 1 to 198 (Mean=38 and Standard deviation [SD] =28). Medical record abstraction on the 5000 charts was performed by the West Virginia Medical Institute External Peer Review Program using remote electronic medical records (EMR). Chart abstraction by this professional review organization involved a computer-guided chart abstraction and customized reporting system. Among the 307 data elements, 90% demonstrated good or very good interrater reliability [Kappa statistic ≥0.70 (κ)]. The lowest interobserver reliability which we utilized was for history of hypertension (κ=0.67). Kappa statistics for abstracted BP was between 0.70–1.0 (highest for discharge BP; lower agreement for BP obtained in outpatient setting within 6 months post discharge). Kappa statistics for elements of the discharge medication list varied between 0.81 and 0.95. Veterans were excluded from the cohort (N=1013) if they were hospitalized for transient ischemic attack or were admitted for post-stroke rehabilitation, experienced an ischemic stroke during a hospitalization for another condition, or were admitted for elective carotid endarterectomy during the index hospitalization. This left 3987 patients seen in 130 VAMCs in the OQP study sample. The date of admission for stroke hospitalization was considered the index event date.
Analytic Population
From this inception cohort of 3987 patients, we excluded veterans who died during the index hospitalization, enrolled in hospice or comfort care, or had an unknown discharge disposition. We also excluded patients for whom there was no BP recorded throughout hospital stay. This population was the analytic population for the first analysis where the outcome was BP control at the time of discharge. For analysis 2 we included patients who had follow-up at a VHA outpatient clinic within 6 months of their index hospitalization. We excluded patients who died or were readmitted within 30 days, those who were lost to follow-up, and those who were seen in a VHA outpatient clinic but who did not have BP measurement.
Outcomes
BP control at discharge
To identify BP control at the time of discharge, we used the last available inpatient BP measurement prior to discharge from the hospital. Suboptimal blood pressure was defined according to the Veterans Affairs/ Department of Defense guidelines for uncontrolled BP (systolic BP≥140 mmHg or diastolic BP ≥90 mmHg).18
New BP medications at discharge
We also examined all antihypertensive medications prescribed at admission and at discharge. Antihypertensives were classified into one of seven potential categories including: 1. thiazide type diuretics; 2. angiotensin converting enzyme inhibitor/ angiotensin receptor blockers (ACE/ARB) 3. beta blockers 4. calcium channel blockers (CCB) 5. alpha adrenergic agents 6. centrally acting antihypertensives and 7. other diuretics. We compared the discharge list of antihypertensive medication categories to the admission list of antihypertensive medication categories for each patient and determined if they received a new prescription for a drug class at the time of discharge.
BP control within 6 months
Regarding BP control within 6 months of the stroke event, if more than one BP was available during the 6 month post discharge period we used the last available BP reading during that time frame. As per VHA performance measures addressing hypertension, only outpatient BPs obtained at primary care and selected specialty care clinics were used (online data supplement). BP measurements taken in the emergency department, ambulatory surgery, urgent care visit, or during an inpatient admission were excluded. Consistent with our definition of BP control we used a threshold of <140/90 mmHg as controlled for all patients.
Covariates
We determined a priori covariates for inclusion in each model based on clinical significance. These included patient age (18–64, 65–74, ≥75years old), gender, race (white, black, other), stroke severity measured by the National Institutes of Health (NIH) stroke scale (which was recorded retrospectively when not available) (0–2, 3–9, 10+), and multiple measures of co-morbidity including the number of preadmission medications, history of cardiovascular disease or cerebrovascular disease, diabetes, hypertension, hyperlipidemia and the number of co-morbidities at admission. For the models that examined BP control within 6 months after index event, we also included covariates known to be important in long-term BP control including the systolic and diastolic BP at the time of discharge, the number of visits since hospital discharge, and the type of antihypertensive category prescribed at discharge.
Statistical Analysis
Descriptive analyses such as frequency, mean, standard error, and cross-tabulations were used to describe patient characteristics at the time of hospitalization for ischemic stroke. Since patient BP control was a binary outcome (controlled or uncontrolled) we used logistic regression models. To accommodate the correlation of outcomes for patients from the same facility, we included a random facility effect.
For the analysis examining BP control at discharge, the predictor variables of interest were the presence of multiple co-morbidities and diabetes. For the analysis examining BP control within 6 months of discharge, we postulated that receipt of combination thiazide diuretic and an ACE/ ARB at discharge would increase the odds of BP control. Patients who left the hospital with uncontrolled BP were considered an important subgroup for the evaluation of BP outcomes within 6 months of follow-up, therefore they were examined separately. We also conducted a sensitivity analysis to determine if addition of a new antihypertensive medication during the index hospitalization was associated with BP control at the 6 month BP measurement. Odds ratios (OR) and 95% confidence intervals (95% CI) are reported. Statistical analyses were conducted using the NLmixed procedure in SAS for Windows version 9.1 (SAS Institute, Cary, NC). This study received institutional review boards approval. A HIPAA waiver and waiver of consent were obtained to review medical records of patients and all information contained in the analytic dataset was considered a limited dataset.
RESULTS
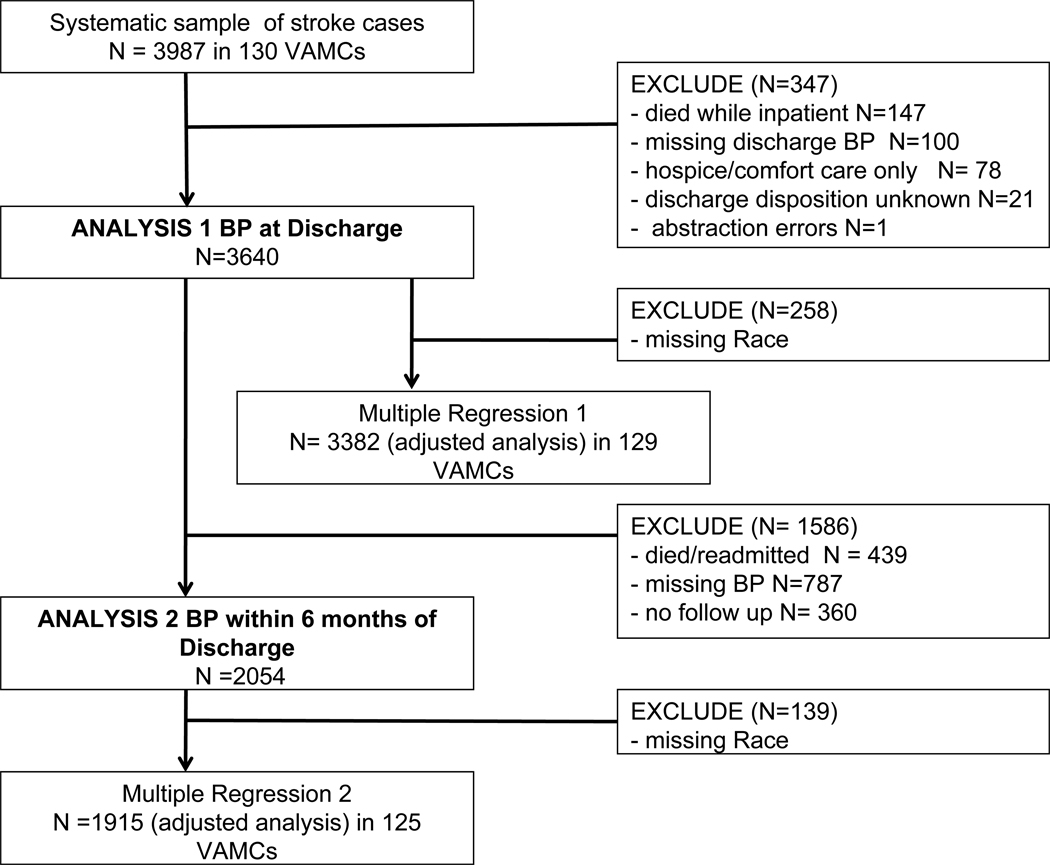
The flow of patients included in each analysis is shown in Figure 1. Of the 3987 patients in the inception cohort who were hospitalized for an acute ischemic stroke, we excluded 347 cases (8.7%) for the following reasons: in hospital mortality (N=147), missing BP information (N=100); hospice or comfort care (N=78) and unknown disposition or abstraction errors (N=22). Thus in first analysis (unadjusted analysis) there were 3640 patients and another 258 (7.1%) patients were excluded from the adjusted analysis due to missing race data (N=3382 in 129 facilities).
Figure.
Flow of patients included in each analysis
For the second analysis we excluded 1586 of the 3640 cases (43.6%) for the following reasons: 30 day mortality or readmission (N=439), missing BP information (N=787), no follow-up visit within 6 months in the VHA system (N=360). Thus in second analysis of BP control at 6 months (unadjusted analysis) there were 2054 patients and another 139 patients (6.8%) were excluded from the adjusted analysis due to missing race data (N=1915 patients in 125 facilities).
Characteristics
Patient characteristics are demonstrated in table 1. Twenty one percent had no history of hypertension at the time of their stroke. The study population was predominately white (62.7%) and male (97.7%); 46.9% were less than 65 years of age and 30.7% were 75 years or older; 29% had a past history of cerebrovascular disease and 37% had a history of cardiovascular disease. Fifty percent of patients had an NIH stroke scale of 0–2 indicating a relatively mild stroke; however at admission patients had a high burden of co-morbid illness. Patients had an average of 3.5 co-morbidities and had a mean Charlson co-morbidity score of 4.7 (standard deviation [SD] ±2.0). Scores of 0 indicates no diabetes, heart disease, cancer, chronic pulmonary disease, connective tissue disease, cerebrovascular disease, peripheral vascular disease, renal disease, or liver disease while higher scores indicate a greater burden of co-morbidity. The mean number of admission medications was 7 (SD ±5). Two-thirds of the sample (67.5%) was discharged home and the remainder was discharged to nursing homes or other facilities.
Table 1.
Characteristics of patients admitted for ischemic stroke stratified by history of hypertension (percent shown unless otherwise indicated)
| Full cohort N=3640 |
HTN History N=2877 (79%) |
No HTN History N= 763 (21%) |
|
|---|---|---|---|
| Gender (%) | |||
| Males | 97.7 | 98.0 | 96.7 |
| Age (%) | |||
| <65 | 46.9 | 45.4 | 52.4 |
| 65– 74 | 22.4 | 23.8 | 17.2 |
| 75+ | 30.7 | 30.8 | 30.4 |
| Race (%) | |||
| White | 62.7 | 61.3 | 68.0 |
| Black | 23.5 | 24.8 | 18.4 |
| Other | 6.8 | 6.8 | 6.4 |
| Missing race | 7.1 | 7.1 | 7.2 |
| NIH stroke scale (%) | |||
| 0–2 | 50.9 | 50.4 | 52.8 |
| 3–9 | 40.0 | 40.5 | 38.3 |
| 10 + | 9.0 | 9.1 | 8.9 |
| Weight available (%) | 81.0 | 80.0 | 84.7 |
| Weight (median IQR) | 185 (159 – 214) | 187 (162 – 217) | 174 (149 – 201) |
| Current Smoker (%) | 35.9 | 34.3 | 42.1 |
| Charlson Score (mean ±SD) | 4.7 ± 2.0 | 4.8 ± 1.9 | 4.4 ± 2.1 |
| Number of Co morbidities at admission (mean ±SD) | 3.5 ± 2.1 | 3.9 ± 2.0 | 2.0 ±1.8 |
| Co morbidities (%) | |||
| Cerebrovascular disease* | 28.8 | 31.3 | 19.1 |
| Cardiovascular disease† | 36.8 | 39.1 | 27.8 |
| Atrial Fibrillation | 15.2 | 16.2 | 11.5 |
| Diabetes | 40.1 | 44.8 | 22.4 |
| Hyperlipidemia | 48.7 | 53.8 | 29.6 |
| Renal disease | 1.1 | 1.2 | 0.5 |
| Liver disease | 2.0 | 1.9 | 2.0 |
| HIV | 0.8 | 0.7 | 1.2 |
| Cancer‡ | 7.3 | 7.0 | 8.7 |
| Pulmonary disease | 15.7 | 15.2 | 17.4 |
| Use of antipsychotic medication‖ | 5.3 | 5.2 | 5.8 |
| Depression | 16.8 | 17.0 | 16.4 |
| Dementia | 7.3 | 7.6 | 6.2 |
| Peptic Ulcer disease | 1.6 | 1.5 | 2.1 |
| Rheumatologic Disorders§ | 0.5 | 0.6 | 0.4 |
| N medications at admission (mean ±SD) | 7.1 ± 4.9 | 7.6 ± 4.8 | 5.4 ± 4.9 |
| Discharged to home (%) | 67.5 | 67.5 | 67.8 |
Cerebrovascular disease includes carotid endarterectomy, carotid stent, ischemic stroke or TIA
Cardiovascular disease includes history of coronary artery disease, acute myocardial infarction, coronary artery bypass, percutaneous transluminal coronary angioplasty with or without stent placement or any history of peripheral vascular disease
Cancer includes any diagnosis of leukemia, lymphoma, or any solid tumor in past 5 years, metastatic tumor, or multiple myeloma
Antipsychotics include chlorpromazine; fluphenazine; thioridizine: trifluoroperazine; thiothixene; aripiprazole; clozapine: haloperidol; loxapine: molindone; olanzapine: quetiapine: risperidone; ziprasidone
Rheumatologic disorders include Lupus and any vasculitis
Characteristics of patients excluded from the 6 month BP analysis for missing BP or visits compared to those included are shown in online data supplement. Patients who were excluded from the analysis tended to be older and sicker, as evidenced by a higher NIH stroke scale at admission and a lower proportion being discharged to home. More excluded patients were discharged to nursing home facilities.
BP control and antihypertensive medications at discharge
Among the 3640 patients hospitalized for stroke, 1573 (43%) had the last documented BP prior to discharge greater than or equal to 140/90mmHg. In the adjusted analysis (N=3382), black race (adjusted OR 0.77 [95% CI 0.65, 0.91]), diabetes (OR 0.73 [95% CI 0.62, 0.86]) and history of hypertension (OR 0.51 [95% CI 0.42, 0.63]) were associated with decreased odds for controlled BP at hospital discharge. Increased number of admission medications was associated with increased odds of controlled BP (OR 1.32 [95% CI 1.08, 1.60 for 4–7 medications] and OR 1.34 [95% CI 1.10, 1.63], for 8 or more medications) compared to those on 0–3 medications at admission. (Table 2)
Table 2.
Adjusted odds of controlled BP (<140/90 mmHg) at time of hospital discharge among 3640 patients hospitalized for acute ischemic stroke
| BP uncontrolled N= 1573 (%) |
BP controlled N=2067(%) |
Unadjusted OR (95% CI) |
Adjusted* OR (95%CI) |
|
|---|---|---|---|---|
| Gender | ||||
| Male | 97.6 | 97.9 | Ref | Ref |
| Female | 2.4 | 2.1 | 0.88 (0.56, 1.37) | 0.86 (0.53, 1.39) |
| Age | ||||
| <65 | 46.2 | 47.3 | Ref | Ref |
| 65–74 | 23.4 | 21.6 | 0.90 (0.76, 1.07) | 0.86 (0.72, 1.03) |
| 75+ | 30.2 | 31.1 | 1.00 (0.86, 1.17) | 0.88 (0.74, 1.04) |
| Race | ||||
| White | 64.0 | 70.0 | Ref | Ref |
| Black | 28.6 | 22.8 | 0.73 (0.62, 0.86) | 0.77 (0.65, 0.91) |
| Other | 7.4 | 7.2 | 0.90 (0.69, 1.18) | 0.95 (0.72, 1.25) |
| NIH stroke scale | ||||
| 0–2 | 53.0 | 49.3 | Ref | Ref |
| 3–9 | 38.6 | 41.1 | 1.15 (1.00, 1.32) | 1.16 (0.99, 1.35) |
| 10+ | 8.4 | 9.6 | 1.24 (0.97, 1.58) | 1.29 (1.00, 1.66) |
| N medications at admission | ||||
| 0–3 | 27.0 | 23.9 | Ref | Ref |
| 4–7 | 30.6 | 31.9 | 1.17 (0.98, 1.40) | 1.32 (1.08, 1.60) |
| 8+ | 42.4 | 44.2 | 1.18 (1.00, 1.39) | 1.34 (1.10, 1.63) |
| N Co-morbidities at admission (mean± SD) | 3.6 ± 2.0 | 3.4 ± 2.1 | 0.98 (0.94, 1.01) | 1.01 (0.95, 1.08) |
| Co-morbidities | ||||
| Cerebrovascular disease | 29.4 | 28.2 | 0.94 (0.81, 1.09) | 0.90 (0.76, 1.08) |
| Cardiovascular disease | 35.2 | 37.9 | 1.12 (0.98, 1.28) | 1.15 (0.94, 1.41) |
| Diabetes | 44.0 | 37.2 | 0.75 (0.66, 0.86) | 0.73 (0.62, 0.86) |
| Hypertension | 85.0 | 74.5 | 0.52 (0.43, 0.61) | 0.51 (0.42, 0.63) |
| Hyperlipidemia | 49.4 | 48.1 | 0.95 (0.83, 1.08) | 1.02 (0.86, 1.20) |
The adjusted logistic regression model had 3382 patients; 258 patients were excluded because of missing information on race. The model included gender, age, race, NIH stroke scale, number of preadmission medications, history of cardiovascular disease, cerebrovascular disease, diabetes, hypertension, hyperlipidemia, and the mean centered number of co- morbidities at admission with facility as a random effect (N=129)
The proportions of patients with discharge prescriptions for antihypertensive agents are reported in table 3. Fifteen percent of patients (N=548/3640) received a discharge prescription for combination ACEI or ARB and a thiazide diuretic. Fifty four percent of patients were discharged with a prescription for an ACEI/ARB (N=1969 prescriptions). Of these, more than 25% were new prescriptions for an ACEI/ARB. The second most commonly prescribed antihypertensive at discharge was beta blockers (1737 prescriptions [47.7%]) and 22% were new prescriptions. CCB’s constituted 928 discharge prescriptions (25.5%) and of these 20% were new. Thiazide diuretics were 22% of the discharge prescriptions (N=794) and of these 30% were new prescriptions.
Table 3.
The proportion of antihypertensive medications prescribed at discharge and proportion which are new prescriptions for antihypertensive medications (total sum greater than 100% as some patients received more than 1 prescription)
| Discharge prescriptions N=3640 patients (%) |
History of Hypertension N=2877 (%) |
No history of Hypertension N=763 (%) |
New prescription* for antihypertensive at Discharge |
|
|---|---|---|---|---|
| Combination ACE/ ARB† + Thiazide | 548 (15.0) | 505 (17.6) | 43 (5.6) | 197/548=36.0% |
| Thiazide diuretics | 794 (21.8) | 710 (24.7) | 84 (11.0) | 240 / 794 = 30.2% |
| ACEI/ARB† | 1969 (54.1) | 1722(59.8) | 247 (32.4) | 498 / 1969 = 25.3% |
| Beta Blockers | 1737(47.7) | 1513 (52.6) | 224 (29.4) | 378 / 1737 = 21.8% |
| Calcium Channel Blockers | 928 (25.5) | 846 (29.4) | 82 (10.8) | 187 / 928 = 20.2% |
| Alpha adrenergic | 487(13.4) | 410 (14.2) | 77 (10.1) | 74 / 487 = 15.2% |
| Centrally acting agents | 231(6.4) | 214 (7.4) | 17 (2.2) | 86 / 231 = 37.2% |
| Other diuretics | 579 (15.9) | 507 (17.6) | 72 (9.4) | 88 / 579 = 15.2% |
Angiotensin Converting Enzyme Inhibitor/ Angiotensin Receptor Blocker
New prescription was determined by comparing the discharge list of medications to the admission list of medications. 2760 patients had at least 1 anti-hypertensive drug at admission and 2985 patients had at least 1 anti hypertensive drug at discharge.
BP control within 6 months of stroke hospitalization
There were 2054 patients who had a follow-up BP measurement within 6 months of discharge from the stroke and were eligible for the second analysis. For approximately 30% of this cohort that follow-up BP measurement was within 3 months of discharge from the index event. Another 37% had a follow-up BP measurement 4–5 months post stroke event and the remaining 32% had their BP measurement obtained at 6 months post stroke event. Of the 2054 stroke patients seen within 6 months from their index event (analysis 2 cohort), 673 (32.8%) were uncontrolled at their follow-up BP measurement. Results of the multivariable logistic regression model assessing BP control by 6 months are reported in Table 4. By 6 months post event the association for decreased odds for controlled BP seen at hospital discharge disappeared among black patients and those with diabetes but remained among those with history of hypertension. Increasing systolic BP at the time of hospital discharge, but not diastolic, was associated with decreased odds of BP control within the 6 month follow-up (OR 0.99 [95%CI 0.98, 0.99] for a 1 unit increase in systolic); or for each 10 point increase in systolic BP > 140 mmHg at discharge the odds of BP control within 6 months post discharge decreased by 12% (95% CI 8%, 18%). The prescription for combination ACEI/ Thiazide diuretic at discharge was not associated with improved odds of BP control at 6 months (OR 1.20 [95% CI 0.88, 1.62]).
Table 4.
Odds of controlled BP (<140/90 mmHg) within 6 months post stroke hospitalization (n=2054 unadjusted)
| BP uncontrolled N=673 (%) |
BP controlled N=1381(%) |
Unadjusted OR (95% CI) |
Adjusted OR* (95%CI) |
|
|---|---|---|---|---|
| Gender | ||||
| Male | 97.4 | 97.4 | Ref | Ref |
| Female | 2.6 | 2.6 | 0.97 (0.54, 1.74) | 0.87 (0.47, 1.62) |
| Age | ||||
| <65 | 53.8 | 49.1 | Ref | Ref |
| 65–74 | 21.6 | 22.0 | 1.12 (0.88, 1.42) | 1.25 (0.96, 1.63) |
| 75+ | 24.6 | 28.9 | 1.28 (1.03, 1.61) | 1.23 (0.95, 1.59) |
| Race* | ||||
| White | 59.8 | 69.1 | Ref | Ref |
| Black | 30.0 | 24.2 | 0.69 (0.55, 0.86) | 0.84 (0.66, 1.06) |
| Other | 10.0 | 6.8 | 0.59 (0.41, 0.84) | 0.63 (0.44, 0.91) |
| N Co-morbidities at admission (mean± SD) | 3.4 ± 2.0 | 3.5 ± 2.0 | 1.03 (0.98, 1.08) | 1.06 (0.96, 1.17) |
| Co-morbidities | ||||
| Cerebrovascular disease | 24.6 | 28.0 | 1.20 (0.97, 1.49) | 1.16 (0.89, 1.50) |
| CVD | 32.6 | 36.5 | 1.19 (0.98,1.45) | 1.02 (0.76, 1.36) |
| Diabetes | 46.2 | 40.2 | 0.78 (0.65, 0.94) | 0.81 (0.64, 1.03) |
| Hypertension | 87.0 | 77.3 | 0.51 (0.39, 0.66) | 0.52 (0.38, 0.71) |
| Hyperlipidemia | 50.8 | 54.2 | 1.15 (0.95, 1.38) | 1.08 (0.86, 1.37) |
| Systolic BP at Discharge mmHg (mean± SD) | 141 ± 22 | 133 ± 19 | 0.98 (0.98, 0.99) | 0.99 (0.98, 0.99) |
| Diastolic BP at Discharge mmHg (mean± SD) | 79 ±14 | 75 ± 12 | 0.97 (0.97, 0.98) | 0.99 (0.98,1.00) |
| N Visits Post Discharge (mean± SD) | 5.8 ± 4.9 | 6.2 ±4.8 | 1.02 (1.00, 1.04) | 1.02 (0.99, 1.04) |
| Antihypertensives at DC | ||||
| Thiazide + ACE/ ARB | 18.2 | 15.9 | 0.85 (0.66, 1.08) | 1.20 (0.88, 1.62) |
| Thiazide | 6.4 | 6.7 | 1.06 (0.72, 1.54) | 1.24 (0.80, 1.91) |
| ACE/ARB | 40.2 | 39.8 | 0.98 (0.81, 1.19) | 1.09 (0.86, 1.39) |
| Beta Blockers | 52.0 | 47.6 | 0.84 (0.70, 1.01) | 0.90 (0.72, 1.11) |
| CCB | 31.6 | 25.3 | 0.73 (0.60, 0.90) | 0.90 (0.72, 1.13) |
| All other classes | 33.6 | 31.0 | 0.89 (0.73, 1.08) | 0.89 (0.71, 1.11) |
One hundred thirty-nine patients were missing race information-- BP uncontrolled N= 45 (6.7%) and BP controlled N=94 (6.8%). The resulting adjusted logistic model had 1915 patients and included the variables gender, age, race, history of cardiovascular disease, cerebrovascular disease, Diabetes, hypertension, hyperlipidemia, number of co-morbidities at admission, systolic and diastolic BP at discharge, number of visits since hospital discharge, class of antihypertensive drugs prescribed at discharge. Facility was a random effect (N=125)
Subgroup and Sensitivity Analysis
Among the subgroup of patients who were discharged from the hospital with a last documented BP of ≥ 140/90 mmHg (N=1573), 885 (56.3%) of them had a follow-up BP measurement available within 6 months post stroke event. Among this subgroup of 885 patients, 360 patients (40.7%) remained uncontrolled at their follow-up BP measurement within 6 months of hospital discharge. Patient with diabetes or history of hypertension had lower odds of BP control compared to those patients without these diseases. Higher systolic or diastolic BP at hospital discharge was also associated with lower odds of BP control (online data supplement).
We conducted a sensitivity analysis to examine the effect of receiving any new antihypertensive medication at discharge on BP control at the 6 month follow-up time-point. The results of this sensitivity analysis were consistent with the results of the main analysis in that higher discharge systolic BP and presence of hypertension were associated with lower odds of BP control. Among patients with uncontrolled 6 month BP 248/673 (36.8%) patients had a new drug added compared to 372/1381 (26.9%) of those with controlled BP (adjusted OR 0.69 [95% CI 0.55, 0.86]). We also examined the rate of post-discharge BP control among those persons with a follow-up BP who were discharged home (N=1637) compared to those with follow-up BPs but discharged to nursing homes and other facilities (N=417). Of the 1637 discharged to home 1087(66.4%) had controlled BP at the 6 month follow-up visit. Of the 417 patients discharged to nursing homes and other facilities, 294 (70.5%) were controlled at the 6 month follow-up visit.
DISCUSSION
The main findings of our study demonstrate that 43% of patients with acute ischemic stroke had their last documented in hospital BP value ≥140/90 mmHg and 33% remained uncontrolled by 6 months post hospitalization. BP values in excess of national guidelines are common,19, 20 particularly after stroke.7, 21–23 After adjustment for age, sex and other confounders that might influence a patient's BP, the probability of being controlled remained significantly lower for patients with history of diabetes and/or hypertension. These data suggest that increased efforts to improve hypertension management at discharge and follow-up may be beneficial to certain subgroups of patients. Blood pressure is the most consistent and powerful predictor of stroke, such that hypertension is causally involved in nearly 70% of all stroke cases.24 Veterans with uncontrolled hypertension are vulnerable to developing cardiovascular events and are at a particularly high risk for developing a recurrent or secondary cerebrovascular event.
The second finding of our study is that only 15% of patients received the antihypertensive combination of ACEI/ARB and thiazide diuretics. There is a large body of evidence that has demonstrated the beneficial effects of BP control in secondary stroke prevention, even among those without a history of hypertension. A meta-analysis of clinical trials noted a risk reduction of 28% (95% CI 15%–39%) for any recurrent stroke with antihypertensive treatment among those who have previously had a stroke.25 High blood pressure is a powerful risk factor for recurrent stroke among stroke survivors. The PROGRESS trial of post-stroke patients, demonstrated that therapy with a diuretic and ACEI lowered blood pressure by 12/5 mmHg and reduced recurrence of stroke by 43 percent among those randomized to perindopril and indapamide therapy (absolute risk reduction 0.9% per year).3 We postulated that the prescription of both combination ACEI/ARB and thiazide diuretic at discharge would more often lead to BP control by 6 months, however our data did not confirm this hypothesis. Moreover, none of the medication classes we investigated or receipt of a new BP medication at discharge were associated with improved BP control at 6 months. We also found that the receipt of a new BP medication was associated with decreased odds of BP control at 6 months. This finding may be due to confounders in that sicker patients may be more likely to receive new medication prescriptions and more likely to have the outcome of interest (poor BP control). A more recent meta-analysis suggested that the reduction in stroke risk is related to the magnitude of BP reduction,1 although a J shaped phenomena has been suggested within the literature.26, 27 Any of the commonly used antihypertensive agents have the potential to reduce the risk of stroke, through reductions in BP.28 The key is not which agent to use but to use an agent and to treat to goal. Our findings did confirm that the higher the discharge BP, the lower the odds of BP control within 6 months post discharge.
There are limitations to our study due to its retrospective design. First, the population that we studied was predominantly male veterans who were admitted with ischemic stroke and may not be representative of hypertension management in post-stroke patients in the private sector. However, hypertension management in the private sector has often been described as suboptimal, with VHA being held as a gold standard for quality care29–36 Another limitation is the use of a single BP measurement in the determination of BP control both at discharge and at 6 months. In 2004, Tierney and colleagues37 set out to determine the predictive ability of a single outpatient BP measurement on the 5-year risk of myocardial infarction, stroke, ischemic heart disease, heart failure, renal insufficiency, and death from any cause. These investigators found that for each 10 mmHg increase in systolic BP at a single outpatient visit there was a 10% (95% CI 2%–18%) increase in the 5-year risk of having a first myocardial infarction, 7% (95% CI, 3%–11%) increased risk of first or recurrent stroke, 9% (95% CI, 3%–15%) increased risk of ischemic heart disease, and 13% (95% CI, 6%–21%) increased risk of developing renal insufficiency. Our results demonstrate that by using a single outpatient measurement of BP almost 33% of patients have uncontrolled BP by 6 months post event. We were also relatively limited in the sample size for this 6 month follow-up analysis. We required that patients have at least one post event BP available in an outpatient clinic, and remain alive after their event. It is possible that patients who were well controlled, or conversely had severe disease, did not have an outpatient visit (or were managed by a provider in the private sector) and therefore did not have a recorded BP. The comparison of those included to those missing BP or outpatient visits demonstrated that those with missing BP values were significantly older, sicker with more severe strokes, and fewer were discharged home (online data supplement). The rate of post-discharge BP control was very similar for persons with a follow-up BP who were discharged home compared to those with follow-up BPs but discharged to nursing homes and other facilities. Because the post-discharge sample consisted largely of persons with milder strokes and those discharged home, our results may be more generalizable to this patient population. It is also possible that patients received their antihypertensive care outside the VHA. Additionally, based on our data, we are unable to determine which BP medications people had been on prior to stroke hospitalization and found not to work. Nor could we examine how effectively BP had been controlled in the outpatient setting prior to their stroke. Finally the medications that we analyzed are currently limited to the medications prescribed at discharge. Currently we do not have access to the pharmacy benefits data for the time subsequent to discharge to investigate if these antihypertensive medications were filled, refilled, or actually taken, after discharge. Medication adherence to the prescribed antihypertensive regimen post stroke event may remain a barrier to achieving BP control among stroke patients due to the newly acquired cognitive, communicative, and physical limitations that may prevent patients from refilling their medications post stroke.
In conclusion, we describe the quality of hypertension care among patients who have been hospitalized for an acute ischemic stroke. We propose that secondary prevention should include efforts to initiate risk factor control and antihypertensive medication initiation prior to hospital discharge. In hospital initiation of secondary prevention strategies have become the standard of care for patients with cardiovascular disease.38, 39 Future interventions could also target those at highest risk for poorly controlled BP, including those with a prior diagnosis of hypertension and multiple co-morbidities including diabetes. The quality of care for patients with cerebrovascular could be beneficially affected through the systematic in hospital initiation of secondary prevention strategies, thus enhancing guideline adherence and improving the care among those at highest risk for a vascular event.
What is Known.
Deficiencies in delivery of secondary preventative care have been noted after stroke; and reducing patients' blood pressure after stroke has been demonstrated to improve risk for recurrent stroke.
Treatment of hypertension should be instituted after the acute stroke period in patients who have consistently elevated blood pressure.
What this Article Adds
43% of patients with acute ischemic stroke had their last documented in hospital blood pressure value ≥140/90 mmHg and 33% remained uncontrolled by 6 months post hospitalization; the probability of being controlled remained significantly lower for patients with history of diabetes and/or hypertension.
Only 15% of patients received the recommended antihypertensive combination of ACEI/ARB and thiazide diuretics at the time of discharge.
We propose that the quality of care for patients with cerebrovascular could be beneficially affected through the systematic in hospital initiation of secondary prevention strategies, thus enhancing guideline adherence and improving the care among those at highest risk for a vascular event.
Supplementary Material
Acknowledgments
Funding Sources: The project reported here was supported by the Department of Veterans Affairs, Veterans Health Administration, Health Services Research and Development Service Quality Enhancement Research Initiative (RRP 09-184). Dr. Roumie is the Staff physician and Assistant Professor of Internal Medicine and Pediatrics at Tennessee Valley healthcare System and Vanderbilt University. The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
Veterans Health Administration (VHA) Office of Quality and Performance (OQP)
VA Health Services Research and Development (HSR&D) Stroke Quality Enhancement Research Initiative Program (RRP 09-184).
Veterans Affairs Career Development Award 04-342-2 (Roumie).
National Institute on Aging (K08 AG032886) and the American Federation of Aging Research through the Paul B. Beeson Career Development Award Program (Ross)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest Disclosures: Dr Bravata has received grants from Veterans Affairs and NHLBI which are relevant to the topic of this manuscript.
References
- 1.Rashid P, Leonardi-Bee J, Bath P. Blood pressure reduction and secondary prevention of stroke and other vascular events: a systematic review. Stroke. 2003;34:2741–2748. doi: 10.1161/01.STR.0000092488.40085.15. [DOI] [PubMed] [Google Scholar]
- 2.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 3.Chapman N, Huxley R, Anderson C, Bousser MG, Chalmers J, Colman S, Davis S, Donnan G, MacMahon S, Neal B, Warlow C, Woodward M. Effects of a perindopril-based blood pressure-lowering regimen on the risk of recurrent stroke according to stroke subtype and medical history: the PROGRESS Trial. Stroke. 2004;35:116–121. doi: 10.1161/01.STR.0000106480.76217.6F. [DOI] [PubMed] [Google Scholar]
- 4.Rudd AG, Lowe D, Hoffman A, Irwin P, Pearson M. Secondary prevention for stroke in the United Kingdom: results from the National Sentinel Audit of Stroke. Age Ageing. 2004;33:280–286. doi: 10.1093/ageing/afh107. [DOI] [PubMed] [Google Scholar]
- 5.Xu G, Liu X, Wu W, Zhang R, Yin Q. Recurrence after Ischemic Stroke in Chinese Patients: Impact of Uncontrolled Modifiable Risk Factors. Cerebrovasc Dis. 2006;23:117–120. doi: 10.1159/000097047. [DOI] [PubMed] [Google Scholar]
- 6.Kaplan RC, Tirschwell DL, Longstreth WT, Jr, Manolio TA, Heckbert SR, Lefkowitz D, El-Saed A, Psaty BM. Vascular events, mortality, and preventive therapy following ischemic stroke in the elderly. Neurology. 2005;65:835–842. doi: 10.1212/01.wnl.0000176058.09848.bb. [DOI] [PubMed] [Google Scholar]
- 7.Paul SL, Thrift AG. Control of hypertension 5 years after stroke in the North East Melbourne Stroke Incidence Study. Hypertension. 2006;48:260–265. doi: 10.1161/01.HYP.0000230610.81947.04. [DOI] [PubMed] [Google Scholar]
- 8.Ovbiagele B, Saver JL, Fredieu A, Suzuki S, Selco S, Rajajee V, McNair N, Razinia T, Kidwell CS. In-hospital initiation of secondary stroke prevention therapies yields high rates of adherence at follow-up. Stroke. 2004;35:2879–2883. doi: 10.1161/01.STR.0000147967.49567.d6. [DOI] [PubMed] [Google Scholar]
- 9.Ovbiagele B, Hills NK, Saver JL, Johnston SC. Antihypertensive medications prescribed at discharge after an acute ischemic cerebrovascular event. Stroke. 2005;36:1944–1947. doi: 10.1161/01.STR.0000177522.80092.b7. [DOI] [PubMed] [Google Scholar]
- 10.Bradley EH, Herrin J, Elbel B, McNamara RL, Magid DJ, Nallamothu BK, Wang Y, Normand SL, Spertus JA, Krumholz HM. Hospital quality for acute myocardial infarction: correlation among process measures and relationship with short-term mortality. JAMA. 2006;296:72–78. doi: 10.1001/jama.296.1.72. [DOI] [PubMed] [Google Scholar]
- 11.Rahiman A, Saver JL, Porter V, Buxton W, McNair N, Razinia T, Ovbiagele B. In-hospital initiation of secondary prevention is associated with improved vascular outcomes at 3 months. J Stroke Cerebrovasc Dis. 2008;17:5–8. doi: 10.1016/j.jstrokecerebrovasdis.2007.09.004. [DOI] [PubMed] [Google Scholar]
- 12.Hillis AE. Systemic blood pressure and stroke outcome and recurrence. Curr Hypertens Rep. 2005;7:72–78. doi: 10.1007/s11906-005-0058-4. [DOI] [PubMed] [Google Scholar]
- 13.Gil-Nunez AC, Vivancos-Mora J. Blood pressure as a risk factor for stroke and the impact of antihypertensive treatment. Cerebrovasc Dis. 2005;20:40–52. doi: 10.1159/000089356. [DOI] [PubMed] [Google Scholar]
- 14.Fonarow GC, Reeves MJ, Smith EE, Saver JL, Zhao X, Olson DW, Hernandez AF, Peterson ED, Schwamm LH. Characteristics, performance measures, and in-hospital outcomes of the first one million stroke and transient ischemic attack admissions in get with the guidelines-stroke. Circ Cardiovasc Qual Outcomes. 2010;3:291–302. doi: 10.1161/CIRCOUTCOMES.109.921858. [DOI] [PubMed] [Google Scholar]
- 15.Adams RJ, Albers G, Alberts MJ, Benavente O, Furie K, Goldstein LB, Gorelick P, Halperin J, Harbaugh R, Johnston SC, Katzan I, Kelly-Hayes M, Kenton EJ, Marks M, Sacco RL, Schwamm LH. Update to the AHA/ASA recommendations for the prevention of stroke in patients with stroke and transient ischemic attack. Stroke. 2008;39:1647–1652. doi: 10.1161/STROKEAHA.107.189063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, Jones DW, Materson BJ, Oparil S, Wright JT, Jr, Roccella EJ. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 17.Reker DM, Hamilton BB, Duncan PW, Yeh SC, Rosen A. Stroke: who's counting what? J Rehabil Res Dev. 2001;38:281–289. [PubMed] [Google Scholar]
- 18.Preformance OoQa. [Accessed September 7, 2010];Management of Hypertension in Primary Care (HTN) Available at: http://www.healthquality.va.gov/Hypertension_Clinical_Practice_Guideline.asp.
- 19.Choma NN, Huang RL, Dittus RS, Burnham KE, Roumie CL. Quality improvement initiatives improve hypertension care among veterans. Circ Cardiovasc Qual Outcomes. 2009;2:392–398. doi: 10.1161/CIRCOUTCOMES.109.862714. [DOI] [PubMed] [Google Scholar]
- 20.Roumie CL, Elasy TA, Greevy R, Griffin MR, Liu X, Stone WJ, Wallston KA, Dittus RS, Alvarez V, Cobb J, Speroff T. Improving blood pressure control through provider education, provider alerts, and patient education: a cluster randomized trial. Ann Intern Med. 2006;145:165–175. doi: 10.7326/0003-4819-145-3-200608010-00004. [DOI] [PubMed] [Google Scholar]
- 21.Amar J, Cambou JP, Touze E, Bongard V, Jullien G, Vahanian A, Coppe G, Mas JL. Comparison of hypertension management after stroke and myocardial infarction: results from ECLAT1--a French nationwide study. Stroke. 2004;35:1579–1583. doi: 10.1161/01.STR.0000131547.71502.81. [DOI] [PubMed] [Google Scholar]
- 22.Amar J, Cambou JP, Quentzel S, Amelineau E, Danchin N. Controlled diastolic blood pressure, previous stroke and associated risk factors are obstacles to improving systolic blood pressure. J Hum Hypertens. 2007;21:893–896. doi: 10.1038/sj.jhh.1002243. [DOI] [PubMed] [Google Scholar]
- 23.Nicodeme R, Albessard A, Amar J, Chamontin B, Lang T. Poor blood pressure control in general practice: in search of explanations. Archives of cardiovascular diseases. 2009;102:477–483. doi: 10.1016/j.acvd.2009.02.013. [DOI] [PubMed] [Google Scholar]
- 24.Bronner LL, Kanter DS, Manson JE. Primary prevention of stroke. N Engl J Med. 1995;333:1392–1400. doi: 10.1056/NEJM199511233332106. [DOI] [PubMed] [Google Scholar]
- 25.Gueyffier F, Boissel JP, Boutitie F, Pocock S, Coope J, Cutler J, Ekbom T, Fagard R, Friedman L, Kerlikowske K, Perry M, Prineas R, Schron E. Effect of antihypertensive treatment in patients having already suffered from stroke. Gathering the evidence. The INDANA (INdividual Data ANalysis of Antihypertensive intervention trials) Project Collaborators. Stroke. 1997;28:2557–2562. doi: 10.1161/01.str.28.12.2557. [DOI] [PubMed] [Google Scholar]
- 26.Boutitie F, Gueyffier F, Pocock S, Fagard R, Boissel JP. J-shaped relationship between blood pressure and mortality in hypertensive patients: new insights from a meta-analysis of individual-patient data. Ann Intern Med. 2002;136:438–448. doi: 10.7326/0003-4819-136-6-200203190-00007. [DOI] [PubMed] [Google Scholar]
- 27.Gueyffier F. Editorial comment--Secondary prevention of stroke: beyond meta-analyses. Stroke. 2003;34:2748–2749. doi: 10.1161/01.STR.0000097306.83180.10. [DOI] [PubMed] [Google Scholar]
- 28.Turnbull F. Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet. 2003;362:1527–1535. doi: 10.1016/s0140-6736(03)14739-3. [DOI] [PubMed] [Google Scholar]
- 29.Singh H, Kalavar J. Quality of care for hypertension and diabetes in federal- versus commercial-managed care organizations. Am J Med Qual. 2004;19:19–24. doi: 10.1177/106286060401900104. [DOI] [PubMed] [Google Scholar]
- 30.Cushman WC, Ford CE, Cutler JA, Margolis KL, Davis BR, Grimm RH, Black HR, Hamilton BP, Holland J, Nwachuku C, Papademetriou V, Probstfield J, Wright JT, Jr, Alderman MH, Weiss RJ, Piller L, Bettencourt J, Walsh SM. Success and predictors of blood pressure control in diverse North American settings: the antihypertensive and lipid-lowering treatment to prevent heart attack trial (ALLHAT) J Clin Hypertens (Greenwich) 2002;4:393–405. doi: 10.1111/j.1524-6175.2002.02045.x. [DOI] [PubMed] [Google Scholar]
- 31.Carter BL, Malone DC, Ellis SL, Dombrowski RC. Antihypertensive Drug Utilization in Hypertensive Veterans With Complex Medication Profiles. J Clin Hypertens (Greenwich) 2000;2:172–180. [PubMed] [Google Scholar]
- 32.Borzecki AM, Wong AT, Hickey EC, Ash AS, Berlowitz DR. Hypertension control: how well are we doing? Arch Intern Med. 2003;163:2705–2711. doi: 10.1001/archinte.163.22.2705. [DOI] [PubMed] [Google Scholar]
- 33.Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988–2000. JAMA. 2003;290:199–206. doi: 10.1001/jama.290.2.199. [DOI] [PubMed] [Google Scholar]
- 34.Hyman DJ, Pavlik VN, Vallbona C. Physician Role in Lack of Awareness and Control of Hypertension. J Clin Hypertens (Greenwich) 2000;2:324–330. [PubMed] [Google Scholar]
- 35.Hyman DJ, Pavlik VN. Self-reported hypertension treatment practices among primary care physicians: blood pressure thresholds, drug choices, and the role of guidelines and evidence-based medicine. Arch Intern Med. 2000;160:2281–2286. doi: 10.1001/archinte.160.15.2281. [DOI] [PubMed] [Google Scholar]
- 36.Hyman DJ, Pavlik VN. Poor hypertension control: let's stop blaming the patients. Cleve Clin J Med. 2002;69:793–799. doi: 10.3949/ccjm.69.10.793. [DOI] [PubMed] [Google Scholar]
- 37.Tierney WM, Brunt M, Kesterson J, Zhou XH, L'Italien G, Lapuerta P. Quantifying risk of adverse clinical events with one set of vital signs among primary care patients with hypertension. Annals of Family Medicine. 2004;2:209–217. doi: 10.1370/afm.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Giugliano RP, Braunwald E. 2004 ACC/AHA guideline for the management of patients with STEMI: the implications for clinicians. Nat Clin Pract Cardiovasc Med. 2005;2:114–115. doi: 10.1038/ncpcardio0135. [DOI] [PubMed] [Google Scholar]
- 39.Braunwald E, Antman EM, Beasley JW, Califf RM, Cheitlin MD, Hochman JS, Jones RH, Kereiakes D, Kupersmith J, Levin TN, Pepine CJ, Schaeffer JW, Smith EE, 3rd, Steward DE, Theroux P, Gibbons RJ, Alpert JS, Faxon DP, Fuster V, Gregoratos G, Hiratzka LF, Jacobs AK, Smith SC., Jr ACC/AHA 2002 guideline update for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction--summary article: a report of the American College of Cardiology/American Heart Association task force on practice guidelines (Committee on the Management of Patients With Unstable Angina) J Am Coll Cardiol. 2002;40:1366–1374. doi: 10.1016/s0735-1097(02)02336-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.