Abstract
Background/Aims
Pyogenic liver abscess (PLA) is a serious, life threatening condition with a high mortality rate that represents a diagnostic and therapeutic challenge. The aim of this study was to collect demographic data and clinical, laboratory and microbiological characteristics of PLA patients treated between 2000 and 2010. We also aimed to collect information regarding our management experience of these cases.
Methods
As a retrospective review, 47 patients with PLA in a tertiary referral center were examined to determine their demographic characteristics, clinical features, and laboratory, imaging, and microbiologic findings as well as the treatment outcome.
Results
Cryptogenic PLA was the most frequently identified type of PLA, while benign biliary tract disease was the most frequently identifiable cause of PLA (18/47 patients; 38.3%). Leukocytosis and elevated alanine transaminase were common laboratory findings and were observed in 35 (74.5%) and 22 (46.8%) patients, respectively. Increased fibrinogen was also detected in 11 of 15 investigated cases (73.3%). Notably, infection-induced thrombocytopenia occurred in 8 patients (17%). Diabetes mellitus was associated with the occurrence of infection induced shock when compared to the non-diabetic group (p<0.05). Patients with two or more comorbid diseases had longer hospitalizations when compared to patients with one comorbid disease or those without comorbidities (p<0.001). The number of days needed to establish diagnosis was correlated with the length of hospitalization (p<0.001). The overall hospital mortality rate was 2.1% (1/47).
Conclusions
Characteristics of PLA patients from the past 10 years are presented. The number of days needed to establish a PLA diagnosis was correlated with the length of the hospital stay. The hospital stay of PLA patients can be further improved by early diagnosis and effective treatments during the early stages of PLA progression.
Keywords: Asian Continental Ancestry Group, Pyogenic liver abscess, Clinical audit, Early diagnosis, Treatment outcome
INTRODUCTION
Pyogenic liver abscess (PLA) is a serious, life threatening condition, with a mortality rate of 6% to 14%.1-4 PLA remains a major diagnostic and therapeutic challenge, despite advances in diagnostic technology and new strategies for treatment. Its clinical incidence varies from region to region, but has been reported between 0.006% to 2.2% of the hospital admissions.5,6 The mortality rate for liver abscess has changed in the last decades, because of improved imaging modalities, nutritional, and therapeutic support of critically ill patients.3,4,7,8
The etiology and management of PLA has changed substantially in the past few decades. Due to the advent of highly developed imaging techniques and accurate chemical tests, early diagnosis, precise localization of PLA and images-guided percutaneous aspiration and drainage of abscess can be achieved easily. However, a high index of suspicion with PLA is the cornerstone of prevention for misdiagnosis and improvement for prognosis. The present study is a retrospective analysis of 47 patients with PLA managed in a hospital of China mainland in the past decade. The demographic, clinical, laboratory and microbiological features, and management outcomes were studied.
MATERIALS AND METHODS
In-patients medical records with a principal diagnosis of liver abscess in the Second Affiliated Hospital of Nanjing Medical University, Nanjing, were identified using the clinical document database of the hospital. From June 2000 to June 2010, all ethnic Chinese patients with liver abscess were identified. All were adult patients older than 18 years. Amoebic liver abscess and fungal liver abscess were excluded from the analysis. Newer interventional procedures, radiofrequency ablation (RFA) or after transcatheter arterial chemoembolization (TACE) may lead to PLA of hepatic tumor, and the application time of RFA and TACE varied from hospital to hospital in China in the recent decade. Therefore, cases with RFA or TACE associated infection in liver cancer focus were excluded for decreasing bias.
The following demographic data and clinical information were obtained from each patient's record: age, gender, presenting symptoms and signs, number of non-malignant comorbidities, underlying etiology, diabetes mellitus, presence of malignancy, positive microbiological culture (including blood and abscess aspirate), electrocardiogram (ECG) with ST segment elevation, imaging modality performed, characteristics of abscess (size, location, and number of abscesses), percutaneous aspiration performed or not, drainage catheter inserted or not, duration of drainage, requirement of surgical treatment, number of days needed to establish diagnosis, duration of hospital stay, and treatment outcome. The following laboratory parameters were retrieved for analysis: white cell count, platelet count, blood levels of C-reactive protein, hemoglobin, urea, creatinine, albumin, globulin, total bilirubin, alkaline phosphatase (ALP), fibrinogen and alanine transaminase (ALT), prothrombin time (PT), and activated partial thromboplastin time (APTT). The value on the day of admission was chosen for analysis. Toxic myocarditis was diagnosed according to clinical presentation, ST segment elevation9 and serum cardiac biomarkers (creatine kinase, troponin I and T).10
Statistical analysis was performed using SPSS version 11.0 (SPSS Inc., Chicago, IL, USA) software. All continuous data was expressed as mean±standard deviation (SD). Statistics used included chi-squared test, Fisher's exact test and Student's t-test, Mann-Whitney U test and Wilcoxon Signed Rank Test. Differences were considered statistically significant at p<0.05.
RESULTS
1. Clinical features
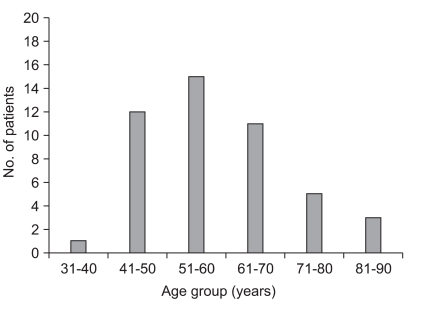
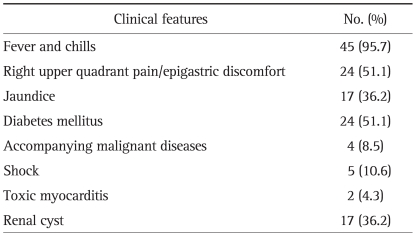
From June 2000 to June 2010 inclusive, 56 patients were diagnosed with PLA at the Second Affiliated Hospital, Nanjing Medical University. Forty-seven of 56 patients with complete documents being available were included. All patients were ethnic Chinese. Twenty-five patients were men and 22 women (male-to-female ratio, 1.14:1). The age range was 35 to 88 years (mean±SD, 59.6±12 years). The age group with the greatest number of patients was 51 to 60 years (Fig. 1), followed by the second age group 41 to 50 years, instead of 61 to 70 years. As shown in Table 1, the most common presenting features were fever and chills (95.7%), followed by right upper quadrant pain and/or epigastric discomfort in 24 patients (51.1%). Comorbi dity included hypertension, diabetes mellitus, senile stroke, ischemic heart disease, congestive heart failure, malignant diseases (two with colon cancer, another two with bile ducts cancer) and biliary diseases. Twenty-four patients (51.1%) had diabetes mellitus. Interestingly, seventeen (36.2%) had renal cysts. Diabetes mellitus was associated with occurrence of infection induced shock when compared to non-diabetic group (p=0.049). There was no significant finding in any of other parameters in Table 1 between patients with diabetes mellitus and patients without diabetes mellitus.
Fig. 1.
Age distribution of 47 patients with pyogenic liver abscess.
No., number.
Table 1.
Clinical Features of 47 Patients with Pyogenic Liver Abscess
No., number.
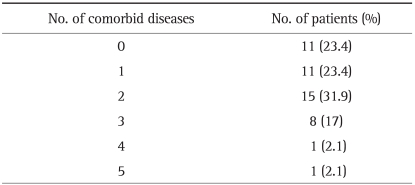
Twenty-five patients (53.2%) had two or more comorbid diseases (Table 2), such as cholelithiasis, cholecystitis, pneumonia, diabetes mellitus and cancer. Patients with two or more comorbid diseases had longer duration of hospitalization when compared to patients with one or without any comorbid disease (Wilcoxon Signed Rank Test, p<0.001).
Table 2.
Comorbid Diseases in Patients with Pyogenic Liver Abscess
No., number.
2. Laboratory features
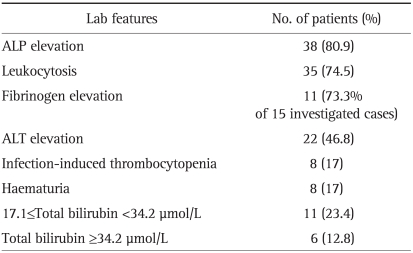
The most common laboratory abnormality among investigated and included items was increased ALP in 38 patients (80.9%) (Table 3). This was followed by leukocytosis in 35 patients (74.5%), increased fibrinogen (73.3%, 11 of 15 investigated cases) and elevated ALT in 22 patients (46.8%). Notably, infection-induced thrombocytopenia occurred in 8 patients (17%) and haematuria was confirmed by urine test in 8 patients (17%). Interestingly, 12 patients (25.5%) had a normal white blood cell count and 30 patients (63.8%) had normal total bilirubin.
Table 3.
Laboratory Features of 47 Patients with Pyogenic Liver Abscess
No., number.
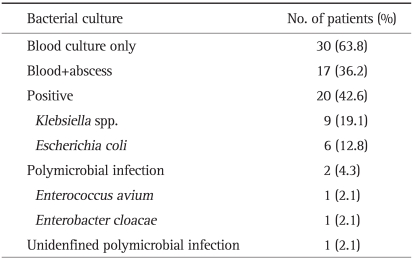
3. Microbiological findings
Blood or abscess culture was positive in 20 of 47 patients (42.6%) (Table 4). Culture from aspirate of liver abscess was positive in 74 of 89 patients who underwent percutaneous aspiration of liver abscess (positive rate, 83.1%). The most common organism identified was Klebsiella spp. (19.1%), followed by Escherichia coli (12.8%).
Table 4.
Microbiological Findings of 47 Patients with Pyogenic Liver Abscess
No., number.
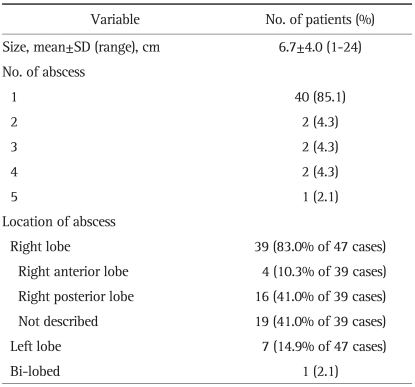
4. Radiological features
Ultrasound as most convenient and first-line investigation was performed for 47 patients (100.0%). Computed tomography (CT) scan or/and magnetic resonance imaging (MRI) were performed if they were further needed for differential diagnosis of liver cancer or cancer with infection and the investigation was done with the consent of patients. Twenty (42.6%) of 47 cases underwent CT scanning and 5 (10.6%) cases with MRI. The data of sizes of abscess were collected from the radiological reports. As shown in Table 5, the mean size of liver abscess was 6.7±4.0 cm (range, 1 to 24 cm). The majority of patients had solitary liver abscess (85.1%). Most of the liver abscesses were found in the right hepatic lobe (83%). Between the group of patients with multiple abscesses (≥2 abscess, n=7) and patients with solitary liver abscess (n=40), there was no significant finding for gender, diabetic, symptom, white blood cell count, platelets changing (p>0.05) (Table 5). Between the group of patients with large abscesses (diameter ≥6.7 cm) and patients with small abscess (<6.7 cm), there was no significant finding for gender, diabetic, symptom, white blood cells count, platelets changing (p>0.05). Patients with large abscesses had longer duration of hospitalization when compared to patients with the group of small size of abscess (37.3±17.3 days vs. 25.0±10.8 days, p=0.01).
Table 5.
Radiologic Characteristics of Pyogenic Liver Abscess
No., number.
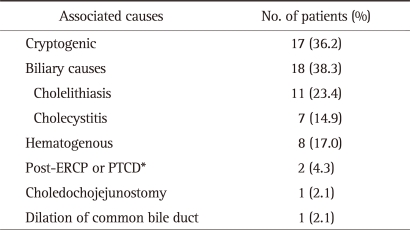
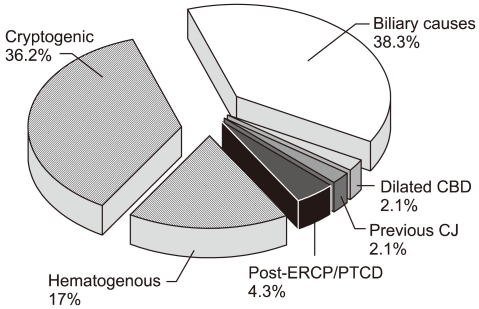
5. The potential causes of the PLA
As shown in Table 6 and Fig. 2, the cause of PLA in 17 patients (36.2%) was not clear. Benign biliary tract diseases, including cholelithiasis and cholecystitis were identified in 18 patients (38.3%). The cause of PLA in 8 patients (17.0%) was assigned to be hematogenous origin. Endoscopic retrograde cholangiopancreatography (ERCP) or percutaneous transhepatic cholangio drainage (PTCD) leaded to PLA in two patients with hepato-pancreatico-biliary (HPB) (Fig. 2) malignancy and biliary obstruction. One patient developed liver abscess after choledochojejunostomy.
Table 6.
Causes of Pyogenic Liver Abscess
No., number.
*Post-endoscopic retrograde cholangiopancreatography (ERCP) or percutaneous transhepatic cholangio drainage (PTCD) in patients with hepato-pancreatico-biliary cancer.
Fig. 2.
Causes of pyogenic liver abscess.
CBD, common bile duct; ERCP, endoscopic retrograde cholangiopancreatography; PTCD, percutaneous transhepatic cholangio drainage; CJ, choledochojejunostomy.
6. Management and outcome
Intravenous broad spectrum antibiotics were given to all patients. The reason for not performing image-guided aspiration and drainage was small size of the abscess <2-3 cm, no liquefaction in the abscess, or clinical improvement with antibiotics. Ultrasound or CT-guided needle aspiration of liver abscess was performed in 18 (38.3%) patients, 8 (17.0%) of these patients underwent continuous drainage after needle aspiration. The range of drainage duration was 3 to 14 days. Surgery or drainage after surgery was required in three patients (6.4%). There was no major complication of interventional drainages or percutaneous aspiration. ERCP was not used as the interventional method to treat liver abscess. One patient (2.1%) died before percutaneous aspiration or surgery.
Accurate diagnosis of PLA was achieved at a median duration of 3 days after admission (range, 1 to 11 days). Mean hospital days was 28.3 days (28.3±16.5 days; range, 2 to 68 days). Wilcoxon Signed Rank Test showed the number of days needed to establish diagnosis was correlated with the number of hospital days (p<0.001). One patient died within the same hospital admission (mortality, 2.1%), and 5 patients (10.6%) required to be referred to local primary hospital for further treatment.
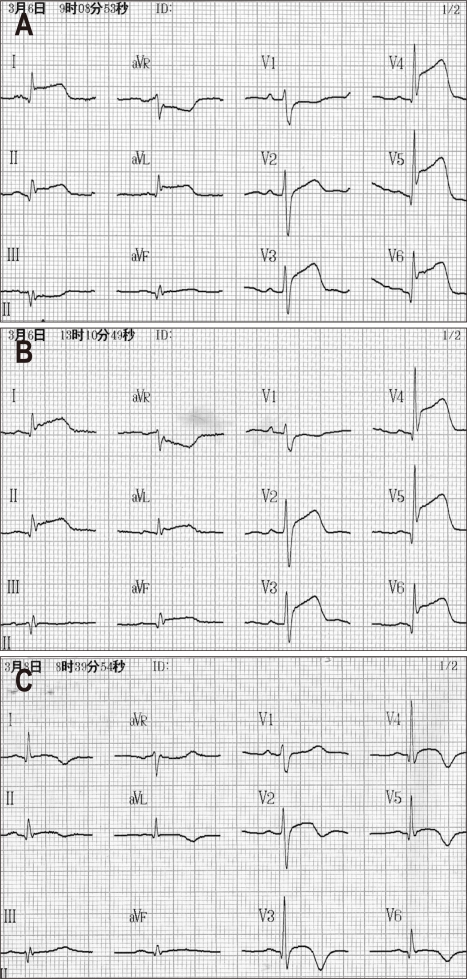
According the documents, the most serious condition with dramatically changing was the patient with final diagnosis as PLA associated with toxic myocarditis, shock, infection induced thrombocytopenia and type 2 diabetes mellitus. The patient, a 44-year-old man, was admitted to hospital without positive finding by liver ultrasound 12 hours before admission. Twenty hours after admission, the platelets decreased to 10×109/L, and ECG showed elevation in all ST-segments of six leads (Fig. 3) and also increase in cardiac-specific troponin T and troponin I more than 20 times the normal level. The patient had no chest pain and ST segments elevation further remained for 24 hours. Platelet transfusion was given after thrombotic thrombocytopenia purpura and heparin-induced thromb ocytopenia were precluded. Ultrasound showed 6.0×5.0 cm size of liver abscess at the second day after admission. ECG and cardiac markers were followed up 1 to 2 times per two days in the first week (data not shown). After 15 days of treatment using intravenous third-generation cephalosporins with metronidazole, the patient was discharged with the prescription of one week-oral ciprofloxacin.
Fig. 3.
Electrocardiogram (ECG) tracking at 8 hours (A), 12 hours (B), and 56 hours (C) after admission in a typical case with infection-induced toxic myocarditis. No obvious ST elevation is observed in the emergent ECG prior to admission (data not shown).
DISCUSSION
The clinical presentation in many cases of PLA are non-specific in nature and are difficult to diagnose early.7 This disease is particularly important in emergency room since the time for patient evaluation is often limited and mortality is high. PLA was traditionally considered as a subacute entity with a median of symptom duration before admission of over 2 weeks.11 A high index of suspicion should be maintained in patients with diabetes mellitus, previous biliary tract intervention or gastrointestinal malignancy.12 The trend of PLA varies from region to region3,4,13-15 and was even called as an endemic disease.15 However, there are very few English literatures reflecting the changing trend of PLA in China mainland.
The previous studies focusing on the period from 1990-20004 and 1998-20043 in Hong Kong reported that there had been a trend for progressive increase in the age of presentation of PLA. The mean age of these patient in the later report3 was 62.6 years and the age group with the greatest number of patients was 61 to 70 years. However, our retrospective review from 2000-2010 in Nanjing (in China mainland) showed the mean age was 59.6 years, and the age group with the greatest number of patients was 51 to 60 years (Fig. 1), followed by the age group 41 to 50 years, instead of group 61 to 70 years. Local economic status and the health care support system in China mainland before 2005 may be one of important aspects affecting trends changing, including the timely and effective treatment on biliary diseases, the hematogenous spread from distant foci, diabetes mellitus and so on.
Newer interventional procedures such as RFA or TACE leading to PLA of hepatic tumor16-18 and the application time of RFA and TACE varied from hospital to hospital in China. Therefore, for decreasing bias, we excluded the cases with RFA or TACE associated infection in liver cancer focus.
The presenting features can be non-specific and the diagnosis requires a high index of suspicion. It is interesting to note that right upper quadrant pain/epigastric discomfort was present in 51.1% of patients. Twelve patients (25.9%) had normal white blood cell count. Diabetes mellitus is also commonly found,13 reflecting the importance of host immunity in the pathogenesis of this condition. The present results indicated that diabetes mellitus may be associated with occurrence of infection induced shock. Cryptogenic PLA was the most frequently noticed and was followed by benign biliary tract diseases, as the most frequently identifiable cause in 18 patients (38.3%). The abscess was most common in right lobe (83%). Previous studies3,4,19 also reported similar findings. 17.0% of PLA were hematogenous spread from distant foci in gastrointestinal tract, urinary tract and even foreign body.20 Patients with two or more comorbid diseases may be prior to patients with one or without any comorbid disease have longer duration of hospitalization.
The laboratory features are also non-specific for diagnosis of PLA. Notably, the ratio of leukocytosis in 47 patients (35, 74.5%) was followed by increased fibrinogen (73.3%, 11 of 15 investigated cases), indicating fibrinogen may be a promising circulation marker for infection, at least as a useful early marker for PLA. Further studies based on large samples are needed.
Similarly, the most frequent organism isolated from blood and abscess aspirate was Enterobacteriaceae (Klebsiella spp., followed by Escherichia coli).4,21 This is probably explained by the high incidence of a biliary cause of liver abscess.1-4,11,19,22,23 The low positive rate of bacterial culture (44/80, 55%) was probably related to the use of empirical antibiotics treatment prior to the drainage procedure.
Intravenous antibiotics were given to all these patients and this was the only treatment for 22 patients (19.8%). The most commonly used antibiotics were second and third-generation cephalosporins with or without metronidazole. This regimen covered most of the identified organisms and was similar to regimens used in other centers.3,4 Based on the classic work, open surgical drainage or closed aspiration, ultrasound or CT-guided needle aspiration of liver abscess was performed in 18 (38.3%) patients, 8 (17.0%) of these patients underwent continuous drainage. The range of drainage duration was 3 to 14 days. Surgery or drainage after surgery was required in three patients (6.4%). The application rate of interventional treatment is much lower than that in the previous report4 that percutaneous aspiration of liver abscess was performed in 80.2% of patients and catheters were inserted in 68.5% of patients in a Hong Kong hospital.
Ultrasound was reported as 85.8% sensitivity of liver abscess at emergency department.12 In the present study, one patient's condition (briefly introduced in Results) deteriorated dramatically even he had no positive ultrasound finding when he had shock, infection induced thrombocytopenia and serious toxic myocarditis. Patients with such non-specific clinical features could pose a diagnostic challenge to clinicians. Effective intravenous antibiotics and systemic treatments (without interventional procedures) at early stage showed the importance to short the hospital days.
ERCP has been found to be a useful investigation and treatment modality for patients with PLA.3,4,23,24 These reports highlighted that ERCP is useful in the treatment of patients with PLA. However, in this series, there was no patient who underwent ERCP for treating PLA. Interestingly, in the two patients with biliary malignancy and common bile duct obstruction PLA occurred after they underwent ERCP or PTCD, respectively. This indicates that biliary interventional therapy may be the cause leading to or increasing the possibility of PLA.
A previous study reflected that age, rupture at presentation, emergency laparotomy, malignancy, hyperbilirubinemia, and elevated prothrombin time were risk factors associated with in-hospital mortality during period from 1984-1995 in Hong Kong.25 In another Hong Kong's study3 from 1998-2004, authors showed that malignancy, requirement for surgical intervention, and delayed diagnosis were independent risk factors associated with in-hospital mortality. Malignancy has long been described as a poor prognostic factor for patients with PLA.3,4,19,23,25,26 Poor nutritional status and an immunocomprised state are the likely factors contributing to the poor outcome.4 In the present study from 2000-2010, one patient died during his hospital admission (mortality, 2.1%). There had n ot been a rising trend in mortality with an increasing age at present, comparing the previous reports from Taiwan and Hong Kong.1,3,4,12,15,21 The present analysis showed that the number of days needed to establish diagnosis was correlated with the number of hospital days, indicating early diagnosis at the early stage of PLA progression would improve the prognosis and treatment outcome.
Some limitations of this study should be noted. The data collected may be affected by factors such as poor standard of record keeping and lack of proper documentation of important events, and can be subject to inter and/or intra-observer bias during case review.3 The results represent the experience based on a small sample from a single center, and may not be generalizable to other areas with different epidemiologic or clinical settings.
In conclusion, PLA are non-specific in nature and continue to experience significant morbidity and mortality. The number of days needed to establish diagnosis was correlated with the number of hospital days. The hospital day of patients with PLA can be further improved by early diagnosis and effective treatments at the early stage of PLA progression.
ACKNOWLEDGEMENTS
The work was partially supported by grants from the National Natural Science Foundation of China (No. 30900667) and the Science and Technology Foundation of Medical University (08NMUZ021).
Conflicts of interest statement: None declared.
References
- 1.Yu SC, Ho SS, Lau WY, et al. Treatment of pyogenic liver abscess: prospective randomized comparison of catheter drainage and needle aspiration. Hepatology. 2004;39:932–938. doi: 10.1002/hep.20133. [DOI] [PubMed] [Google Scholar]
- 2.Alvarez Pérez JA, González JJ, Baldonedo RF, et al. Clinical course, treatment, and multivariate analysis of risk factors for pyogenic liver abscess. Am J Surg. 2001;181:177–186. doi: 10.1016/s0002-9610(00)00564-x. [DOI] [PubMed] [Google Scholar]
- 3.Lok KH, Li KF, Li KK, Szeto ML. Pyogenic liver abscess: clinical profile, microbiological characteristics, and management in a Hong Kong hospital. J Microbiol Immunol Infect. 2008;41:483–490. [PubMed] [Google Scholar]
- 4.Wong WM, Wong BC, Hui CK, et al. Pyogenic liver abscess: retrospective analysis of 80 cases over a 10-year period. J Gastroenterol Hepatol. 2002;17:1001–1007. doi: 10.1046/j.1440-1746.2002.02787.x. [DOI] [PubMed] [Google Scholar]
- 5.Miedema BW, Dineen P. The diagnosis and treatment of pyogenic liver abscesses. Ann Surg. 1984;200:328–335. doi: 10.1097/00000658-198409000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huang CJ, Pitt HA, Lipsett PA, et al. Pyogenic hepatic abscess. Changing trends over 42 years. Ann Surg. 1996;223:600–607. doi: 10.1097/00000658-199605000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Johannsen EC, Sifri CD, Madoff LC. Pyogenic liver abscesses. Infect Dis Clin North Am. 2000;14:547–563. vii. doi: 10.1016/s0891-5520(05)70120-3. [DOI] [PubMed] [Google Scholar]
- 8.Halvorsen RA, Jr, Foster WL, Jr, Wilkinson RH, Jr, Silverman PM, Thompson WM. Hepatic abscess: sensitivity of imaging tests and clinical findings. Gastrointest Radiol. 1988;13:135–141. doi: 10.1007/BF01889042. [DOI] [PubMed] [Google Scholar]
- 9.Wang K, Asinger RW, Marriott HJ. ST-segment elevation in conditions other than acute myocardial infarction. N Engl J Med. 2003;349:2128–2135. doi: 10.1056/NEJMra022580. [DOI] [PubMed] [Google Scholar]
- 10.Magnani JW, Dec GW. Myocarditis: current trends in diagnosis and treatment. Circulation. 2006;113:876–890. doi: 10.1161/CIRCULATIONAHA.105.584532. [DOI] [PubMed] [Google Scholar]
- 11.Bamberger DM. Outcome of medical treatment of bacterial abscesses without therapeutic drainage: review of cases reported in the literature. Clin Infect Dis. 1996;23:592–603. doi: 10.1093/clind/23.1.592. [DOI] [PubMed] [Google Scholar]
- 12.Lin AC, Yeh DY, Hsu YH, et al. Diagnosis of pyogenic liver abscess by abdominal ultrasonography in the emergency department. Emerg Med J. 2009;26:273–275. doi: 10.1136/emj.2007.049254. [DOI] [PubMed] [Google Scholar]
- 13.Kurtz LE, Greenberg RE. Pyogenic liver abscess associated with a gastrointestinal stromal tumor of the stomach. Am J Gastroenterol. 2010;105:232–233. doi: 10.1038/ajg.2009.497. [DOI] [PubMed] [Google Scholar]
- 14.Shah I, Bhatnagar S. Liver abscess in a newborn leading to portal vein thrombosis. Indian J Pediatr. 2009;76:1268–1269. doi: 10.1007/s12098-009-0244-5. [DOI] [PubMed] [Google Scholar]
- 15.Tsai FC, Huang YT, Chang LY, Wang JT. Pyogenic liver abscess as endemic disease, Taiwan. Emerg Infect Dis. 2008;14:1592–1600. doi: 10.3201/eid1410.071254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cheung YC, Ko SF, Ng SH, Chan SC, Cheng YF. Survival outcome of lobar or segmental transcatheter arterial embolization with ethanol-lipiodol mixture in treating hepatocellular carcinoma. World J Gastroenterol. 2005;11:2792–2795. doi: 10.3748/wjg.v11.i18.2792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hanazaki K, Kajikawa S, Horigome N, et al. Gas-forming liver abscess after transcatheter arterial embolization for hepatocellular carcinoma: report of a case. Surg Today. 1993;23:747–749. doi: 10.1007/BF00311717. [DOI] [PubMed] [Google Scholar]
- 18.Hashimoto T, Mitani T, Nakamura H, et al. Fatal septic complication of transcatheter chemoembolization for hepatocellular carcinoma. Cardiovasc Intervent Radiol. 1993;16:325–327. doi: 10.1007/BF02629168. [DOI] [PubMed] [Google Scholar]
- 19.Foo NP, Chen KT, Lin HJ, Guo HR. Characteristics of pyogenic liver abscess patients with and without diabetes mellitus. Am J Gastroenterol. 2010;105:328–335. doi: 10.1038/ajg.2009.586. [DOI] [PubMed] [Google Scholar]
- 20.Santos SA, Alberto SC, Cruz E, et al. Hepatic abscess induced by foreign body: case report and literature review. World J Gastroenterol. 2007;13:1466–1470. doi: 10.3748/wjg.v13.i9.1466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee SS, Chen YS, Tsai HC, et al. Predictors of septic metastatic infection and mortality among patients with Klebsiella pneumoniae liver abscess. Clin Infect Dis. 2008;47:642–650. doi: 10.1086/590932. [DOI] [PubMed] [Google Scholar]
- 22.Arakura N, Ozaki Y, Yamazaki S, et al. Abscess of the round ligament of the liver associated with acute obstructive cholangitis and septic thrombosis. Intern Med. 2009;48:1885–1888. doi: 10.2169/internalmedicine.48.2396. [DOI] [PubMed] [Google Scholar]
- 23.Lam YH, Wong SK, Lee DW, et al. ERCP and pyogenic liver abscess. Gastrointest Endosc. 1999;50:340–344. doi: 10.1053/ge.1999.v50.98065. [DOI] [PubMed] [Google Scholar]
- 24.Dull JS, Topa L, Balgha V, Pap A. Non-surgical treatment of biliary liver abscesses: efficacy of endoscopic drainage and local antibiotic lavage with nasobiliary catheter. Gastrointest Endosc. 2000;51:55–59. doi: 10.1016/s0016-5107(00)70388-9. [DOI] [PubMed] [Google Scholar]
- 25.Chu KM, Fan ST, Lai EC, Lo CM, Wong J. Pyogenic liver abscess. An audit of experience over the past decade. Arch Surg. 1996;131:148–152. doi: 10.1001/archsurg.1996.01430140038009. [DOI] [PubMed] [Google Scholar]
- 26.Chong VH, Lim KS. Pyogenic liver abscess as the first manifestation of hepatobiliary malignancy. Hepatobiliary Pancreat Dis Int. 2009;8:547–550. [PubMed] [Google Scholar]