Abstract
Extracellular matrix (ECM) is essential for all stages of angiogenesis. In the adult, angiogenesis begins with endothelial cell (EC) activation, degradation of vascular basement membrane, and vascular sprouting within interstitial matrix. During this sprouting phase, ECM binding to integrins provides critical signaling support for EC proliferation, survival, and migration. ECM also signals the EC cytoskeleton to initiate blood vessel morphogenesis. Dynamic remodeling of ECM, particularly by membrane-type matrix metalloproteases (MT-MMPs), coordinates formation of vascular tubes with lumens and provides guidance tunnels for pericytes that assist ECs in the assembly of vascular basement membrane. ECM also provides a binding scaffold for a variety of cytokines that exert essential signaling functions during angiogenesis. In the embryo, ECM is equally critical for angiogenesis and vessel stabilization, although there are likely important distinctions from the adult because of differences in composition and abundance of specific ECM components.
The extracellular matrix provides basic support for endothelial cell proliferation, survival, and migration. In conjunction with cytokines (e.g., VEGF), it also regulates blood vessel morphogenesis and maturation.
The extracellular matrix (ECM) provides a critical framework for angiogenesis through structural support and also by conferring molecular signals essential for all stages of blood vessel formation, including vascular sprouting, lumen formation, vessel maturation, and ultimately vessel stabilization. In addition, ECM provides an immobilizing scaffold for cytokines that are important for angiogenesis. Thus, by providing basic structural support, direct signaling functions, and scaffolding for cytokines, ECM exerts fundamental control over angiogenesis. Moreover, the established functional complexity of ECM together with known mechanisms available for dynamic ECM remodeling suggest that ECM is capable of exerting precise control over all aspects of angiogenesis and blood vessel maturation.
This article is divided into four parts: (1) Overview of angiogenesis and ECM in the adult; (2) key functions of ECM during angiogenesis; (3) distinctions between the composition of embryonic and adult ECMs, including implications for the involvement of specific integrins in angiogenesis; and (4) ECM remodeling during vascular tube formation and stabilization. The scientific literature on ECM and angiogenesis is vast, and it is therefore impossible to cover this topic completely in a single article. Thus, rather than striving for an exhaustive review of the literature, we have sought to provide an overview and also provide specific examples of ECM function in angiogenesis. In particular, we have focused on the importance of ECM in vascular morphogenesis.
OVERVIEW OF ANGIOGENESIS AND ECM IN THE ADULT
Normally, in the adult, quiescent blood vessels are covered on the ablumenal (basal) surface with a continuous basement membrane consisting primarily of laminins, collagen type IV, nidogens, and the heparan sulfate proteoglycan, perlecan (Hayashi et al. 1992; Hallmann et al. 2005; Bix and Iozzo 2008). However, during the earliest stages of angiogenesis, such as in response to the angiogenic cytokine VEGF induced by wounding and ischemia, vascular basement membrane is degraded (Sundberg et al. 2001; Rowe and Weiss 2008; Chang et al. 2009). Following disruption of basement membrane, and with the ensuing stage known as vascular sprouting (Nicosia and Madri 1987), vessels become leaky and hyperpermeable to blood plasma proteins (Sundberg et al. 2001). This vascular hyperpermeability causes leakage of the ECM proteins fibrinogen, vitronectin, and fibronectin from the blood (Senger 1996; Sundberg et al. 2001). Fibrinogen is subsequently converted to fibrin through enzymatic coagulation, and together with extravasated vitronectin and fibronectin instantly transform the interstitial collagen matrix to form a new, provisional ECM. Thus, the early stages of sprouting angiogenesis are generally believed to proceed in an environment rich in preexisting interstitial collagens in combination with fibrin, vitronectin, and fibronectin derived from the blood plasma. As vascular morphogenesis proceeds and vascular sprouts acquire lumens and mature, neovessels are again enshrouded in vascular basement membrane with associated pericytes and thereby achieve stability (Grant and Kleinman 1997; Benjamin et al. 1999). Recent studies show that pericyte recruitment to vascular tubes directly controls this basement membrane assembly step in vitro and in vivo (Stratman et al. 2009a, 2010). Thus, in response to stimulation with angiogenic cytokines, angiogenesis in the adult is generally believed to proceed through the following basic stages: (1) degradation of vascular basement membrane and activation of quiescent endothelial cells (ECs); (2) sprouting and proliferation of ECs within provisional ECM; (3) lumen formation within the vascular sprouts, thereby creating vascular tubes; and (4) coverage of vascular tubes with mature vascular basement membrane in association with supporting pericytes.
It seems logical to expect that vascular basement membrane components associated with normal blood vessel quiescence and stability might directly function in this capacity; and observations in vivo (Risau and Lemmon 1988) together with investigations in vitro, do indeed support a role for basement membrane in conferring vessel stabilization and vascular barrier integrity (Bonanno et al. 2000; Liu and Senger 2004; Stratman et al. 2009a) (see sections Key Functions of ECM during Angiogenesis, and ECM Remodeling during Vascular Tube Formation and Stabilization). Similarly, it seems logical that components of provisional ECM would serve to support the sprouting and lumen-forming stages of angiogenesis, and there is considerable evidence that provisional ECM does indeed serve this role. Although there are distinctly different components of provisional ECM, there is abundant evidence that each of the major components (i.e., interstitial collagens, fibrin, fibronectin, and vitronectin) support EC proliferation and migration (see section Key Functions of ECM during Angiogenesis). Moreover, there is strong evidence that interstitial collagen and fibrin each support key stages of vascular morphogenesis, including cord and lumen formation (see sections Key Functions of ECM during Angiogenesis, and ECM Remodeling during Vascular Tube Formation and Stabilization).
Thus, a basic model for framing the complex roles of ECM in adult angiogenesis is to envisage the process beginning with ECs residing on a vessel-stabilizing vascular basement membrane ECM, followed by cytokine-initiated exposure of ECs to a provisional ECM that favors sprouting and lumen formation within that provisional ECM, followed by transitioning of ECs again to interactions with vessel-stabilizing vascular basement membrane. Although undoubtedly oversimplified, the fundamentals of this model are well supported by currently available evidence. Moreover, the basic complexity of ECM (i.e., the large number of distinctly different matrix proteins), combined with additional complexity provided by proteolytic remodeling that generates cell-guidance pathways (see section ECM Remodeling during Vascular Tube Formation and Stabilization) as well as matrix fragments with angiostatic functions (reviewed in Sund et al. 2004; Bix and Iozzo 2005; see also Lu et al. 2011), is well matched to the biological complexity of angiogenesis.
KEY FUNCTIONS OF ECM DURING ANGIOGENESIS
Adhesion to ECM Regulates Endothelial Cell (EC) Proliferation, Survival, and Migration
At the most fundamental level, angiogenesis requires EC activation, proliferation, and survival. Angiogenic cytokines are most generally credited with driving EC proliferation and supporting EC survival; however, EC adhesion to ECM through cell-surface integrins is equally critical (Akiyama et al. 1989; Wary et al. 1996; Meredith and Schwartz 1997; Giancotti and Ruoslahti 1999). In particular, EC adhesion to ECM through integrins is required for efficient cytokine activation of the Erk1/Erk2 MAP kinase signaling pathway (Short et al. 1998; Aplin et al. 1999), and activation of this pathway is necessary for EC proliferation and angiogenesis (Seger and Krebs 1995; Vinals and Pouyssegur 1999; Roovers and Assoian 2000; Assoian and Schwartz 2001). Adhesion-dependent activation of the Erk1/Erk2 MAP kinase pathway also functions critically in supporting EC survival by suppressing apoptosis (Ilan et al. 1998; Aoudjit and Vuori 2001; Perruzzi et al. 2003). Furthermore, the expression and activities of cyclin-dependent kinases, which are required for cell cycle progression and therefore for EC proliferation, are also dependent on EC adhesion to ECM (Fang et al. 1996; Zhu et al. 1996; Assoian 1997). Thus, without adhesion to ECM, EC proliferation ceases and apoptosis is induced, underscoring the fundamental importance of ECM for angiogenesis.
Vascular ECs also require adhesion to ECM for migration; and EC migration is essential for sprouting of new blood vessels from the existing vasculature (Ausprunk and Folkman 1977). Angiogenic cytokines stimulate migration, but such motility is strictly dependent on EC adhesion to ECM. Moreover, evidence from in vitro experiments indicates that many of the interstitial and provisional ECM components that are encountered during sprouting angiogenesis, including fibrin and collagen I, are capable of supporting cytokine-stimulated migration (Dejana et al. 1985; Nicosia and Madri 1987; van Hinsbergh et al. 2001; Senger et al. 2002). Additionally, gradients of immobilized ECM components can by themselves drive haptotactic migration in vitro, independently of cytokines (Senger and Perruzzi 1996; Senger et al. 2002). Although the significance of haptotactic, ECM-driven migration in vivo lacks direct confirmation, it seems plausible that the high concentrations of provisional ECM encountered by ECs during the sprouting phase of angiogenesis may drive outward migration through this mechanism. Thus, sprouting ECs may migrate in response to both gradients of angiogenic cytokine (chemotaxis) and ECM (haptotaxis). Regardless, all EC motility, including random migration, is absolutely dependent on EC adhesion to ECM.
Although the general importance of ECM for EC migration, proliferation, and survival is unequivocal, the relative importance of various ECM components in supporting these processes is less clear, often because of functional overlap among different matrix proteins. For example, cytokine activation of the MAP kinase pathway in microvascular ECs and proliferation of microvascular ECs are similarly supported by attachment to either collagen I or vitronectin (Perruzzi et al. 2003). Moreover, a variety of ECM components support EC migration (Dejana et al. 1985; Nicosia and Madri 1987; Senger and Perruzzi 1996; van Hinsbergh et al. 2001; Senger et al. 2002), although perhaps not with equal potency (Senger and Perruzzi 1996). There is also evidence that ECM shows maximal activity in promoting EC survival when multiple ECM components are present, indicating that different components of ECM may function cooperatively (Perruzzi et al. 2003).
ECM Function in Formation of Vascular Cords, the Precursors to Vascular Tubes with Lumens
In addition to proliferation and migration, ECs must collectively undergo morphogenesis to form new blood vessels. In the embryo, where this process has been studied extensively, the earliest stages of vascular morphogenesis involve transition of endothelial precursor cells to a spindle-shaped morphology (Drake and Little 1999) together with alignment into solid, multicellular, cord-like structures that form integrated polygonal networks (Vernon and Sage 1995; Drake et al. 1997). These cord-like structures also have been identified during angiogenesis in the adult (Aloisi and Schiaffino 1971). During maturation, the solid vascular cords form hollow lumens, and the ECs are sequestered from the interstitial matrix through establishment of a continuous basal lamina (Aloisi and Schiaffino 1971; Drake et al. 1997), a process that is stimulated by EC-pericyte interactions (Stratman et al. 2009a).
The ECM is critical for morphogenesis of new blood vessels at several levels. First, ECM serves as a three-dimensional malleable scaffold through which individual ECs and clusters of ECs can transduce tensional forces to other ECs at a considerable distance without direct cell–cell contact. Thus, by generating tension-based guidance pathways within ECM, ECs are able to link up and form multicellular cords (Davis and Camarillo 1995; Vernon and Sage 1995). In addition, ECM can exert important signaling functions directly to regulate EC shape and morphogenesis. For example, three-dimensional interstitial collagen I stimulates ECs in vitro to assume a spindle-shaped morphology and to align into cords similarly to those observed during angiogenesis in vivo (Delvos et al. 1982; Montesano et al. 1983; Jackson et al. 1994; Richard et al. 1998; Sweeney et al. 1998; Whelan and Senger 2003). Within collagen I gels, these cords mature to form tubes with hollow lumens through formation and coalescence of intracellular vacuoles (Davis and Camarillo 1996) and expansion of the lumenal compartment through ECM proteolysis (Chun et al. 2004; Saunders et al. 2006; Stratman et al. 2009b). Importantly, there is considerable evidence that interactions between interstitial collagens and ECs are highly relevant in vivo. As discussed above, sprouting ECs migrate and proliferate within a provisional matrix rich in interstitial collagens (Paku and Paweletz 1991; Sundberg et al. 2001). In addition, ECs isolated from tumors express >10-fold more transcripts encoding interstitial collagens type I and III than ECs isolated from corresponding control tissue (St Croix et al. 2000), thus suggesting that interstitial collagen expression by tumor ECs is conducive for angiogenesis. In further support of this hypothesis, expression of collagen I by isolated EC clones in vitro correlates with spontaneous multicellular organization of these ECs into cords (Fouser et al. 1991; Iruela-Arispe et al. 1991). Finally, proline analogs that interfere with collagen triple helix assembly and β-aminopropionitrile, that inhibits collagen cross-linking, each inhibit neovascularization in animal models (Ingber and Folkman 1988), providing further evidence that collagens play a crucial role in angiogenesis.
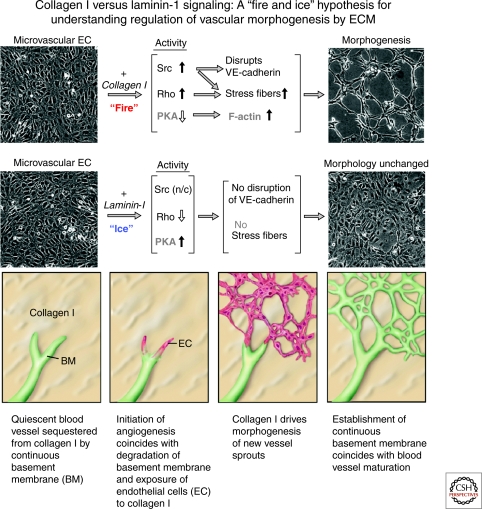
The mechanism through which collagen I provokes ECs to form vascular cords requires direct interactions between collagen I and cell-surface integrins. Upon ligation of integrins, collagen I induces actin stress fibers through multiple signaling pathways, including activation of Rho and Src (Liu and Senger 2004) and p38 MAP kinase (Sweeney et al. 2003), suppression of cyclic AMP (Whelan and Senger 2003), and suppression of Rac activity (Liu and Senger 2004). Suppression of cyclic AMP results in reduced activity of cyclic AMP-dependent protein kinase A (PKA), causing a marked induction of actin polymerization (Whelan and Senger 2003). Coordinate activation of Rho and Src and suppression of Rac activity by collagen I organize polymerized actin into stress fibers, thereby driving EC contractility, transition to spindle-shaped morphology, and ultimately alignment into cords (see Fig. 1) (Liu and Senger 2004). Consistent with the importance of each of these pathways for vascular morphogenesis in vitro, cyclic AMP analogs and inhibitors of Rho, Src, and p38 MAP kinase each block collagen I-induced stress fiber and cord formation (Sweeney et al. 2003; Whelan and Senger 2003; Liu and Senger 2004). Moreover, a dominant-negative RhoA mutant blocks cord formation both in vitro and in vivo (Hoang et al. 2004).
Figure 1.
Signals transduced by interstitial collagen type I and laminin-1 (laminin-111) in dermal microvascular ECs, and consequences for capillary morphogenesis in vitro. In this proposed model, interstitial collagens, but not laminins, activate Src and Rho and suppress Rac and PKA activities through β1 integrins. Such signaling results in induction of actin stress fibers, disruption of VE-cadherin, and formation of precapillary cords. In contrast, laminins activate Rac and PKA and suppress Rho activity and therefore do not provoke morphogenesis. Although laminin-1 (revised nomenclature = laminin-111) is not one of the laminin isoforms typically associated with vascular basement membranes (see text) and therefore further testing of this model requires additional investigations with vascular laminin isoforms, these marked distinctions in signaling by collagen type I (“fire”) and laminin-1 (“ice”) suggest a mechanism through which degradation of basement membrane and exposure of activated and proliferating ECs to interstitial collagens within the provisional matrix initiates morphogenesis of new capillary sprouts. (n/c) = no change. (This figure is adapted from Liu and Senger [2004] and Davis and Senger [2005] and is reprinted, with permission, from the Federation of American Societies for Experimental Bio (FASEB) ©2004 and Wolters Kluwer Health ©2005, respectively.)
Activation of Src and Rho and suppression of Rac activity by collagen I also disrupts VE-cadherin from intercellular junctions (Fig. 1) (Liu and Senger 2004), and loosening of cell–cell contacts is likely important for cord formation. In marked contrast to interstitial collagen I, basement membrane laminin-111 does not activate Src or Rho or suppress cyclic AMP or protein kinase A activity, nor does it induce actin stress fibers in microvascular ECs (Whelan and Senger 2003; Liu and Senger 2004). Consistent with these distinctions, laminin-111 also fails to induce cord formation or changes in EC shape. Rather, laminin-111 induces persistent activation of the GTPase Rac (Liu and Senger 2004), and such activation is highly consistent with improved endothelial barrier function and vessel maturation (Garcia et al. 2001; Wojciak-Stothard and Ridley 2002; Waschke et al. 2004). However, laminin-111 is not one of the laminin isoforms typically associated with vascular basement membranes (Hallmann et al. 2005), and therefore further investigations with vascular laminin isoforms such as laminin-411 and laminin-421 are required. These findings have suggested to us a model, whereby interstitial collagens of the provisional matrix and laminins of the vascular basement membrane differentially regulate various stages of angiogenesis. As summarized in Figure 1, degradation of the laminin-rich basal lamina is predicted to reduce Rac activity and thereby diminish integrity of cell–cell junctions during the sprouting phase. Sprouting ECs are exposed to underlying interstitial collagens and begin to invade, resulting in activation of signaling pathways that drive changes to a spindle-shaped morphology and cord formation. Subsequently, as the newly formed capillary sprouts mature into new vessels with mature lumens, the intact laminin-rich basement membrane is reestablished, thereby sequestering ECs from interstitial collagens and reestablishing normal activation levels for signaling pathways that regulate EC stress fiber formation and barrier integrity (Fig. 1).
ECM Function in Lumen Formation
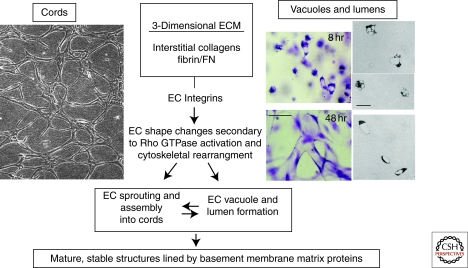
In addition to inducing formation of vascular cords, three-dimensional (3-D) collagen I induces and supports lumen formation by ECs (Fig. 2) (Davis and Camarillo 1996; Davis et al. 2007; Aplin et al. 2008; Koh et al. 2008; Iruela-Arispe and Davis 2009). Lumen formation also occurs in 3-D fibrin and plasma clots that are also representative of provisional matrix (Nicosia and Madri 1987; Bayless et al. 2000; van Hinsbergh et al. 2001; Sainson et al. 2005; Nakatsu and Hughes 2008) (see section Overview of Angiogenesis and ECM in the Adult). Lumen formation in both collagen I and fibrin is integrin- and Rho GTPase-dependent, involving the formation and coalescence of pinocytic intracellular vacuoles in conjunction with ECM proteolysis (Fig. 2) (Davis and Camarillo 1996; Bayless and Davis 2002; Davis and Bayless 2003; Kamei et al. 2006; Saunders et al. 2006; Stratman et al. 2009b). These intracellular vacuoles coalesce further to form intracellular lumens (Folkman and Haudenschild 1980; Meyer et al. 1997; Yang et al. 1999; Bayless and Davis 2002; Davis and Bayless 2003; Egginton and Gerritsen 2003; Lubarsky and Krasnow 2003) that exocytose by fusion with the plasma membrane allowing for multicellular assembly of tubes by adjacent ECs. Mechanisms that coordinate ECM proteolysis with the EC cytoskeleton to regulate lumen formation are described further in section ECM Remodeling during Vascular Tube Formation and Stabilization.
Figure 2.
Fundamental contribution of the ECM-integrin-cytoskeletal signaling axis to the assembly of EC cords and lumens during vasculogenesis and angiogenesis. In this schematic, two models of EC morphogenesis are illustrated. In the left panel, confluent human microvascular EC monolayers were overlaid with a type I collagen gel and allowed to undergo cord formation, illustrating how collagenous ECM markedly converts an EC monolayer into an interconnecting network of cords. This process is dependent on the α1β1 and α2β1 integrins and the small GTPase, RhoA. In the right panels, human ECs are suspended as individual cells in 3-D collagen matrices and are fixed, stained, and photographed at 8 and 48 hr of culture, illustrating intracellular vacuoles and early lumen formation at 8 hr and interconnecting networks of EC-lined tubes at 48 hr. Bar equals 50 µm. The three panels on the far right side are cross-sections from plastic-embedded collagen gels revealing EC intracellular vacuoles (upper two right panels) or EC lumens (lower right panel). Bar equals 25 µm. The vacuole and lumen formation process shown is completely dependent on the α2β1 integrin and the Cdc42 and Rac1 small GTPases. (This figure is adapted from Davis and Senger [2005] and reprinted, with permission, from Wolters Kluwer Health ©2005.)
ECM as a Scaffold Presenting Cytokines: Implications for Vascular Morphogenesis, Stabilization, and Maturation
ECM also serves as a scaffold for growth factors that exert fundamental control over angiogenesis. Growth-factor-containing ECM allows ECs to respond simultaneously to signals through growth factor receptors and integrins (Hynes 2009; Somanath et al. 2009; Chen et al. 2010). Such cosignaling may provide a mechanism for growth factors to exert distinctly different outcomes, depending on the particular ECM environment (e.g., collagen-rich interstitial matrices versus basement membrane matrices) and at different stages of vascular morphogenesis and stabilization. Angiogenic cytokines typically have affinity for heparan sulfate and thereby become anchored to heparan sulfate proteoglycans (i.e., syndecans, perlecan, versican, glypicans) either on the EC surface or in the surrounding ECM (Gerhardt et al. 2003; Mitsi et al. 2008). Also, many angiogenic cytokines directly bind to angiogenesis-promoting ECM scaffolds such as collagen type I and fibrin/fibronectin matrices (Kanematsu et al. 2004). For example, VEGF binds to fibronectin (Wijelath et al. 2002; Mitsi et al. 2008), and hepatocyte growth factor (HGF) and keratinocyte growth factor (KGF) each bind directly to collagen type I whereas BMP-4 binds collagen type IV (Ruehl et al. 2002; Rahman et al. 2005; Wang et al. 2008). Interestingly, BMP-1, which is a proteinase that activates BMPs as well as procollagens, lysyl oxidase, probiglycan, etc., also recently has been shown to interact with fibronectin (Huang et al. 2009). Furthermore, three hematopoietic stem cell cytokines, stem cell factor (SCF), interleukin-3 (IL-3), and stromal-derived factor-1 α (SDF-1α) have been shown to control formation of vascular tubes and coassembly of vascular tubes with associated pericytes when incorporated into 3-D collagen matrices (Stratman et al. 2009a). Also, the ECM proteins thrombospondin-1 and thrombospondin-2, which can inhibit angiogenesis (Streit et al. 1999; Armstrong and Bornstein 2003), bind various angiogenic cytokines such as FGF-2, VEGF, and HGF (Margosio et al. 2003) and thereby may prevent their binding to proangiogenic ECM or otherwise interfere with cytokine activity. Angiopoietin-1 has been reported to promote cell adhesion through the integrin α5β1 and the angiopoietin receptor, Tie-2, has been found to associate with α5β1, a fibronectin receptor (Carlson et al. 2001; Cascone et al. 2005; Saharinen et al. 2008). One interesting possibility is that angiopoietin-1 becomes anchored to fibronectin matrices to affect vessel formation and/or stabilization through Tie-2 and α5β1 cosignaling. Of particular interest is the activity of fibrillins, that are major components of the elastin-rich microfibrils required for large-vessel elasticity and compliance, toward binding and regulating the activity of TGF-β isoforms as well as BMPs (Ramirez and Dietz 2007, 2009; Wagenseil and Mecham 2009). Disruption of fibrillin expression increases activation of TGF-β signaling leading to vascular abnormalities such as vascular malformations (Ramirez and Dietz 2007, 2009). Thus, growth factors that control angiogenesis are capable of binding directly to provisional ECM scaffolds implicated in supporting vascular morphogenesis (e.g., collagen or fibrin matrices), ECM that promotes vascular stabilization (e.g., basement membrane matrices), and ECM that regulates vessel elasticity (e.g., elastin, fibrillins). Consequently, cytokine-ECM interactions are likely important in regulating vascular morphogenesis as well as vessel maturation and function.
DISTINCTIONS BETWEEN THE COMPOSITIONS OF EMBRYONIC AND ADULT ECMs: IMPLICATIONS FOR ANGIOGENESIS AND THE INVOLVEMENT OF SPECIFIC INTEGRINS
Embryonic Vasculogenesis Versus Adult Angiogenesis
The preceding sections have focused on ECM as it relates to angiogenesis in the adult. A fundamental and intriguing question that clearly warrants additional investigation involves the composition of ECM associated with vascular morphogenesis in the embryo (vasculogenesis) (Hynes 2007; Davis and Senger 2008). One of the difficulties with investigating ECM function during vasculogenesis is that there are currently no 3-D models that mimic the composition of the embryonic ECM. Thus, the development of such models is an important future goal. Nonetheless, it is clear that there is much less fibrillar collagen during embryonic development in comparison with adult tissues; instead, embryonic ECM is known to be rich in glycosaminoglycans, such as hyaluronic acid, proteoglycans, fibronectin, and tenascins (Hynes 2007; Davis and Senger 2008).
In particular, developing embryos depend on the presence of fibronectin for vasculogenesis; fibronectin knockout mice show severe defects in vascular development together with other abnormalities (Francis et al. 2002; Astrof et al. 2007; Astrof and Hynes 2009). Perhaps the central importance of fibronectin in vasculogenesis involves its mechano-sensitive action in self-assembly during morphogenesis and tissue growth (Sakai et al. 2003; Vogel 2006; Hynes 2007; Smith et al. 2007). Fibronectin contains biologically active cryptic sites that affect this self-assembly process, particularly in its III-I domain (Morla and Ruoslahti 1992; Zhong et al. 1998; Davis et al. 2000; Gao et al. 2003; Smith et al. 2007; Vakonakis et al. 2007; see article by Schwarzbauer and DeSimone 2011). Interestingly, this domain is exposed when fibronectin is absorbed to cell surfaces or ECM (Zhong et al. 1998; Davis et al. 2000; Smith et al. 2007), and it appears to be particularly exposed when cells exert mechanical force on fibronectin through integrin-based interactions (Zhong et al. 1998; Smith et al. 2007). Of particular interest, EC-pericyte interactions markedly induce perivascular deposition of fibronectin during the formation of vascular tubes (Stratman et al. 2009a). Because pericytes actively migrate along the ablumenal surface of tubes during fibronectin deposition, in conjunction with vascular basement membrane matrix assembly (Stratman et al. 2009a), it is likely that tensional forces could be generated by ECs and/or pericytes to facilitate matrix assembly. Disruption of fibronectin assembly also interferes with perivascular collagen type IV assembly; thus, basement membrane assembly is dependent on the deposition of fibronectin that is itself a key component of vascular basement membranes (Stratman et al. 2009a). Thus, fibronectin may play a particularly important role in ECM assembly during processes such as vascular morphogenesis that depend on mechanical forces (Hynes 2007; Zhou et al. 2008; Astrof and Hynes 2009; Stratman et al. 2009a). Also, fibronectin is alternatively spliced (IIIA and IIIB), and these particular isoforms appear to play a particularly critical role in promoting vascular tube assembly and maturation during development (Astrof et al. 2007; Astrof and Hynes 2009).
During development and also in the adult, it is clear that vascular basement membrane matrix assembly represents a fundamental step in the maturation of vessels (Miner and Yurchenco 2004; Davis and Senger 2005; Rhodes and Simons 2007; Eble and Niland 2009; Stratman et al. 2009a; Wiradjaja et al. 2010). This is an example where the functional roles of such matrices in adults and embryos appear very similar. One approach to assess the function of these proteins has been to knock out basement membrane matrix genes in mice (Table 1). It is interesting that the cardiovascular system appears particularly vulnerable to basement membrane gene knockouts because of the mechanical forces and stresses exerted on the heart and vasculature during development and postnatal life. Knockouts of fibronectin, laminin isoforms, collagen IV, and perlecan result in very significant cardiovascular dysfunction that results in embryonic lethality in most cases (Table 1). Additional defects in the vasculature are likely because of the importance of these basement membrane components for vascular morphogenesis, remodeling, and stabilization.
Table 1.
Vascular developmental defects secondary to mouse knockouts of ECM basement membrane matrix genes
| Basement membrane component | Mouse knockout phenotype | Specific vascular phenotypic defects/comments | References |
|---|---|---|---|
| Laminin α4 chain (laminins 411, 421) | Mild, early postnatal lethality, newborns lethargic, pale, and icteric because of anemia and hemorrhage, survivors improve and have normal life span. Corneal angiogenesis assays with FGF-2 reveal early, more intense sprouting and grossly distorted vasculature with apparent hemorrhages and dilated vessels. | Diffuse hemorrhagic phenotype from smaller vessels, particularly associated with parturition. Discontinuous basement membrane in capillaries with reduction in collagen type IV and nidogen staining but normal levels of perlecan. Adult null mice correct these defects and have normal levels of collagen type IV, nidogen, perlecan, and express laminin-511 in capillary basement membranes. | Thyboll et al. 2001 |
| Laminin α5 chain (laminins 511, 521) | Embryonic lethality between E13.5 and 16.5 with limb, neural tube, and placental defects. Placental labyrinth is malformed which primarily consists of interacting trophoblasts and endothelial cells with intervening basement membranes. | At E13.5-16.5, vessels were present in placental labryrinth, but the branching complexity was markedly reduced and vessel diameters were significantly increased. In normal embryos, trophoblasts and ECs are separated only by a basement membrane while in the mutant, only the ECs remained adherent to the basement membrane creating a cell-free space. | Miner et al. 1998 |
| Fibronectin | Embryonic lethality after E8.5 with deficits in mesodermal development, particularly, notochord, somites, heart, as well as embryonic and extraembryonic vasculature. Combined knockout of alternatively spliced exons EIIIA and EIIIB show embryonic lethality (usually by E10.5) because of cardiovascular defects including failure of vascular remodeling and hemorrhage. | Cardiac and vascular defects vary with the genetic background (more severe defects in 129S4 vs. C57BL/6J background) as well as vessel location. In some cases, defects in EC-mesenchymal interactions (e.g., heart and aorta) may underlie the vascular morphogenic defects observed. | George et al. 1993; George et al. 1997; Astrof et al. 2007 |
| Collagen type IV, α1/2 chain | Embryonic lethality between E10.5-E11.5; basement membrane laminin and nidogen-1 were detected underlying epithelia and endothelia, although showed weaker and more patchy staining. Areas of basement membrane discontinuity and fragmentation were apparent. Excessive amounts of maternal blood was present in the yolk sac cavity indicative of hemorrhage as was the presence of pericardial bleeding. | Impairment of the placental labyrinth was apparent as its thickness was reduced. At the time of embryonic death, dilated blood vessels were observed. Overall, vascular development appeared relatively normal with reduced capillary density sprouting into the neural layer. However, hemorrhage was observed in the heart and arteries with excessive yolk sac hemorrhage indicative of abnormalities in EC basement membrane contacts or stability. | Poschl et al. 2004 |
| Perlecan | Embryonic lethality between E10-E12 as well as perinatally. The lethality occurs because of hemopericardium and cardiac arrest. There is no evidence for placental or vascular defects. | There are few apparent vascular developmental defects except for some microaneurysms that form in several tissues including lung, skin, and brain. | Costell et al. 1999 |
| Nidogens 1 and 2 | Viable mice, some seizure-like symptoms with loss of muscle control in hindlimbs, no discernable vascular phenotype. Overall, normal basement membrane assembly and Immunostaining of major basement membrane components. | Minimal to no vascular abnormalities, some structural abnormalities in basement membrane matrix of brain capillaries. Nidogen 2 appears to be expressed in higher amounts in EC basement membranes compared to other basement membranes. Probable compensation for both nidogens 1 and 2 following knockout. | Murshed et al. 2000; Dong et al. 2002; Miosge et al. 2002 |
| Collagen type XVIII | Viable mice with eye abnormalities. Overall, vascular basement membranes and vascular development (with the exception of the eye) appear normal. | Delayed regression of hyaloid vessels in the vitreous; abnormal outgrowth of retinal vessels which may be secondary to the lack of regression and/or alterations in VEGF expression through changes in retinal hypoxia. | Fukai et al. 2002 |
In adult tissues, collagen matrices appear to present a physical barrier to sprouting angiogenesis and subsequent formation of lumens and tubes, processes that require MMP-dependent cleavage of collagen (Haas et al. 1998; Zhou et al. 2000; Chun et al. 2004; Saunders et al. 2006; Stratman et al. 2009b). In addition, collagen I is highly cross-linked in adult animals through enzymes such as lysyl oxidase that further stabilize this key component of interstitial matrix (Wagenseil and Mecham 2009). An interesting and unanswered question is whether embryonic ECM presents a physical barrier similar to interstitial collagens in the adult and whether different cell surface enzymes are required for modifying embryonic ECM during vasculogenesis.
Integrins in Embryonic Vasculogenesis and Adult Angiogenesis
Integrin binding to ECM plays a critical role in controlling both embryonic vasculogenesis and adult angiogenesis (Davis and Senger 2005; Hynes 2007). Numerous studies have implicated a variety of integrins; and the relative importance of specific integrins likely depends, at least in part, on the composition of the ECM. During embryonic development, fibronectin receptors appear particularly significant with α5β1 required for formation of vascular tubes (Francis et al. 2002; Hynes 2007; Astrof and Hynes 2009) and α4β1 and α9β1 required for development of lymphatic vessels (Avraamides et al. 2008). These observations likely relate directly to the abundance of fibronectin in embryonic ECM (Astrof and Hynes 2009), as discussed above. In the adult, there is evidence that αv integrins (Friedlander et al. 1995; Stupack and Cheresh 2004; Avraamides et al. 2008; Feng et al. 2008), that bind components of provisional ECM derived through leakage of plasma proteins (e.g., fibrin, vitronectin, plasma fibronectin) and α1β1 and α2β1 integrins (Senger et al. 1997, 2002), that bind interstitial collagens, are also important for angiogenesis. These observations are consistent with the abundance of provisional ECM in adult tissues during wound repair and other settings in which angiogenesis occurs (see section Overview of Angiogenesis and ECM in the Adult). The role of collagen receptors during embryonic vasculogenesis is less clear. Mouse knockouts have not shown them to be essential (Zweers et al. 2007; Zhang et al. 2008); however, a recent study indicates a role for α2β1 in zebrafish vascular development (San Antonio et al. 2009). Thus, it seems likely that multiple integrins can regulate neovascularization depending on the composition of ECM. In addition, integrins also play an important role in maturation and stabilization of vascular tubes by binding vascular basement membrane components. In particular, integrins α5β1, α3β1, α6β1, and α1β1 bind basement membrane matrix during vascular tube/pericyte interactions in 3-D collagen matrices (Stratman et al. 2009a).
ECM REMODELING DURING VASCULAR TUBE FORMATION AND STABILIZATION
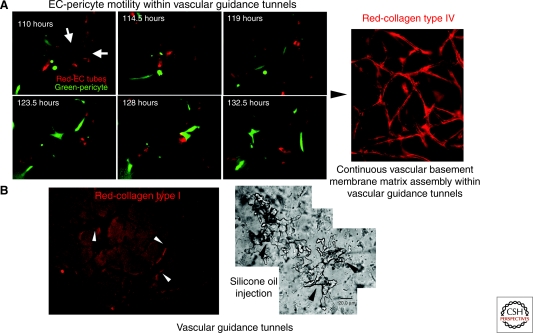
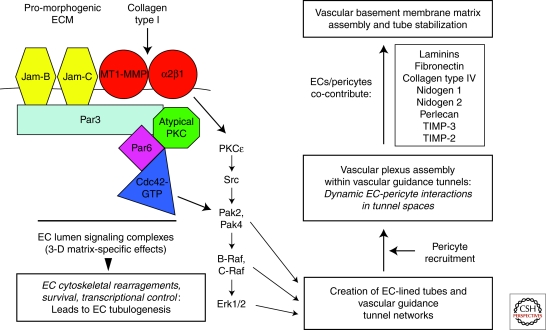
MT1-MMP and Formation of Vascular Guidance Tunnels within ECM
Studies in vitro indicate that ECM proteolysis by cell surface MT1-MMP plays a critical function in facilitating and expanding EC tubes (Chun et al. 2004; Saunders et al. 2006; Stratman et al. 2009b). Proteolysis also clears ECM to create vascular guidance tunnels (Fig. 3) that facilitate mural cell recruitment, followed by basement membrane assembly, and vessel maturation and stabilization (Chun et al. 2004; Davis et al. 2007; Stratman et al. 2009a,b). As summarized in Figure 4, complex signaling cascades involving the functional coupling of Cdc42 with MT1-MMP and integrins together with PKC epsilon, Src, Pak-2, Pak-4, B-Raf, C-Raf, Erk 1/2 and the polarity components Par3, Par6b, and atypical PKC isoforms are essential for formation of vascular tubes in 3-D collagen I (Koh et al. 2008, 2009; Sacharidou et al. 2010). Importantly, MT1-MMP is required for the formation of vascular guidance tunnels (Fig. 3), but once vascular guidance tunnels have formed, ECs are able to migrate within these physical spaces independently of MMP activity (Stratman et al. 2009b). Interestingly, previous work indicates that the tumor vasculature appears to regrow (after induction of tumor vessel regression with anti-VEGFR2 treatments) along previously formed basement membrane sleeves following cessation of the therapy (Mancuso et al. 2006).
Figure 3.
Vascular guidance tunnels: ECM conduits generated during vessel tubulogenesis that regulate EC-pericyte interactions, ECM remodeling, vascular basement membrane matrix assembly, and vessel stabilization. The process of EC tubular morphogenesis in 3-D collagen matrices leads to the creation of networks of EC-lined tubes, and also networks of vascular guidance tunnels in which ECs reside. The tunnels are formed during lumen and tube formation through EC cell surface proteolysis by MT1-MMP. EC-lined tubes within vascular guidance tunnels recruit pericytes to the tube ablumenal surface; subsequently, pericytes migrate along this surface within the tunnels. (A) Time-lapse imaging of EC tubes (RFP-labeled) and pericytes (GFP-labeled) reveals motility of pericytes along the tube ablumenal surface over time. Arrows indicate EC tube ablumenal surface. Bar equals 25 µm. Active motility of pericytes along tubes leads to EC-pericyte interactions and contributions of basement membrane components, such as collagen type IV, which is deposited continuously along the ablumenal surface (right panel; Bar equals 50 µm). (B) Vascular guidance tunnels are formed during EC tubulogenesis through MT1-MMP-mediated proteolysis and can be shown using anticollagen type I antibodies (left panel; Bar equals 50 µm; the tunnels are the negative stained areas; arrowheads indicate tunnel borders) or by microinjection of tunnels with silicone oil (right panel; Bar equals 20 µm; arrowheads indicate tunnel borders).
Figure 4.
Molecular signaling events controlling vascular tube morphogenesis, matrix remodeling, and stabilization in 3-D extracellular matrices. Multicomponent signaling complexes control EC lumen and tube formation in 3-D matrices. A key aspect of this mechanism is the integration of Cdc42-mediated signaling with cell surface proteolysis through MT1-MMP. A downstream kinase signaling cascade is activated leading to EC cytoskeletal changes, survival, and transcriptional control that regulates EC tubular morphogenesis. EC tube formation leads to the generation of networks of vascular guidance tunnel spaces within the ECM that are occupied by ECs, thereby allowing for EC motility and remodeling events (illustrated in Fig. 3). Pericytes are recruited to these EC-lined tunnels and EC-pericyte motility within these tunnels and along the tube ablumenal surface leads to ECM remodeling and vascular basement membrane matrix assembly. Both ECs and pericytes have been shown to contribute basement membrane matrix components (illustrated in Fig. 5), as well as TIMP-2 and TIMP-3, which together control the formation and stability of the vascular basement membrane.
Pericyte Recruitment Stimulates ECM Remodeling and Vascular Basement Membrane Matrix Assembly within Vascular Guidance Tunnels
Identification of vascular tunnels suggested the possibility that they serve a more complex function than simply providing an ablumenal surface for ECs during formation of vascular tubes. Indeed, in a coculture model involving pericytes and ECs, pericytes were observed selectively along the ablumenal surface of tubes and importantly within vascular guidance tunnels (Fig. 3) (Stratman et al. 2009a,b). Thus, ECs and pericytes coassociate within the tunnels. In addition, time-lapse microscopy showed dynamic motility of pericytes along the EC ablumenal surface within the tunnels (Fig. 3) (Stratman et al. 2009a) and showed that both ECs and pericytes were simultaneously motile. Interestingly, pericyte recruitment to EC-lined tubes along the ablumenal surface led to continuous deposition of basement membrane matrix (Figs. 3 and 5). In the absence of pericytes, EC-lined tubes are not able to deposit a basement membrane, a finding that was confirmed with electron microscopy (Stratman et al. 2009a); thus, pericyte recruitment to tubes in vitro and in vivo regulates this process (Stratman et al. 2009a, 2010).
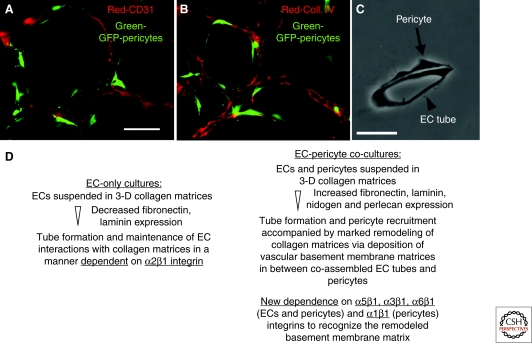
Figure 5.
Pericyte recruitment to EC-lined tubes leads to vascular basement membrane matrix assembly in 3-D matrices. Green-fluorescent protein (GFP)-tagged bovine retinal pericytes were mixed with ECs in 3-D collagen matrices over a period of 5 days, during which EC tubes formed and recruited pericytes. Cultures were fixed at 5 days and immunostained for CD31 (panel A) or for collagen type IV (panel B); bar equals 50 µm. Thin plastic sections were obtained and photographed under transmitted light (panel C); bar equals 25 µm. (Panel D) RT-PCR and protein analyses of EC-only and EC-pericyte cocultures revealed specific changes in ECM and integrin expression, indicating distinctly different regulation in EC-pericyte cocultures in comparison with ECs alone (Stratman et al. 2009a).
Why is pericyte recruitment necessary to stimulate vascular basement membrane matrix assembly around vascular tubes? Key findings from studies designed to answer this question are summarized in Figure 5. In particular, synthesis of fibronectin as well as specific laminins, nidogens, and perlecan, together with integrins that bind basement membrane ECM, were more abundant in EC/pericyte cocultures in comparison with EC-only cultures (Stratman et al. 2009a). Thus, both ECs and pericytes adapt to their changing environment during vascular basement membrane assembly by increasing expression of integrins that recognize this new matrix.
CONCLUDING REMARKS
By providing mechanical stability and cell adhesion, ECM has been shown to be essential for all stages of angiogenesis. In addition to providing basic support for EC proliferation, survival, and migration, ECM also regulates key stages of blood vessel morphogenesis and maturation. Although angiogenic cytokines such as VEGF are often represented as the key mediators of neovascularization, there is a growing body of evidence that ECM and dynamic changes in the composition of ECM are equally important, particularly in regulating vascular morphogenesis and the stabilization of new blood vessels. Thus, at a minimum, angiogenesis should be viewed as a collaboration between cytokines and ECM, wherein ECM actively controls, rather than merely supports, the formation, architecture, and maturation of new blood vessels.
ACKNOWLEDGMENTS
The authors would like to thank Drs. Amber Stratman, Anastasia Sacharidou, Wonshill Koh, Michael Davis, and Yanqiu Liu for their contributions to many of the experiments described. G.E.D. was supported by NIH grants HL79460, HL 59373, and HL 87308; D.R.S. was supported by NIH grants CA 129339 and NS64498.
Footnotes
Editors: Richard Hynes and Kenneth Yamada
Additional Perspectives on Extracellular Matrix Biology available at www.cshperspectives.org
REFERENCES
- Akiyama SK, Yamada SS, Chen WT, Yamada KM 1989. Analysis of fibronectin receptor function with monoclonal antibodies: Roles in cell adhesion, migration, matrix assembly, and cytoskeletal organization. J Cell Biol 109: 863–875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aloisi M, Schiaffino S 1971. Growth of elementary blood vessels in diffusion chambers: Electron microscopy of capillary morphogenesis. Virchows Arch Abt B Zellpath 8: 328–341 [DOI] [PubMed] [Google Scholar]
- Aoudjit F, Vuori K 2001. Matrix attachment regulates Fas-induced apoptosis in endothelial cells: A role for c-flip and implications for anoikis. J Cell Biol 152: 633–643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aplin AE, Short SM, Juliano RL 1999. Anchorage-dependent regulation of the mitogen-activated protein kinase cascade by growth factors is supported by a variety of integrin α chains. J Biol Chem 274: 31223–31228 [DOI] [PubMed] [Google Scholar]
- Aplin AC, Fogel E, Zorzi P, Nicosia RF 2008. The aortic ring model of angiogenesis. Meth Enzymol 443: 119–136 [DOI] [PubMed] [Google Scholar]
- Armstrong LC, Bornstein P 2003. Thrombospondins 1 and 2 function as inhibitors of angiogenesis. Matrix Biol 22: 63–71 [DOI] [PubMed] [Google Scholar]
- Assoian RK 1997. Anchorage-dependent cell cycle progression. J Cell Biol 136: 1–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Assoian RK, Schwartz MA 2001. Coordinate signaling by integrins and receptor tyrosine kinases in the regulation of G1 phase cell-cycle progression. Curr Opin Genet Dev 11: 48–53 [DOI] [PubMed] [Google Scholar]
- Astrof S, Hynes RO 2009. Fibronectins in vascular morphogenesis. Angiogenesis 12: 165–175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Astrof S, Crowley D, Hynes RO 2007. Multiple cardiovascular defects caused by the absence of alternatively spliced segments of fibronectin. Dev Biol 311: 11–24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ausprunk DH, Folkman J 1977. Migration and proliferation of endothelial cells in preformed and newly formed blood vessels during tumor angiogenesis. Microvasc Res 14: 53–65 [DOI] [PubMed] [Google Scholar]
- Avraamides CJ, Garmy-Susini B, Varner JA 2008. Integrins in angiogenesis and lymphangiogenesis. Nat Rev Cancer 8: 604–617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bayless KJ, Davis GE 2002. The Cdc42 and Rac1 GTPases are required for capillary lumen formation in three-dimensional extracellular matrices. J Cell Sci 115: 1123–1136 [DOI] [PubMed] [Google Scholar]
- Bayless KJ, Salazar R, Davis GE 2000. RGD-dependent vacuolation and lumen formation observed during endothelial cell morphogenesis in three-dimensional fibrin matrices involves the α(v)β(3) and α(5)β(1) integrins. Am J Pathol 156: 1673–1683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benjamin LE, Golijanin D, Itin A, Pode D, Keshet E 1999. Selective ablation of immature blood vessels in established human tumors follows vascular endothelial growth factor withdrawal. J Clin Invest 103: 159–165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bix G, Iozzo RV 2005. Matrix revolutions: “Tails” of basement-membrane components with angiostatic functions. Trends Cell Biol 15: 52–60 [DOI] [PubMed] [Google Scholar]
- Bix G, Iozzo RV 2008. Novel interactions of perlecan: Unraveling perlecan’s role in angiogenesis. Microsc Res Tech 71: 339–348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonanno E, Iurlaro M, Madri JA, Nicosia RF 2000. Type IV collagen modulates angiogenesis and neovessel survival in the rat aorta model. In Vitro Cell Dev Biol Anim 36: 336–340 [DOI] [PubMed] [Google Scholar]
- Carlson TR, Feng Y, Maisonpierre PC, Mrksich M, Morla AO 2001. Direct cell adhesion to the angiopoietins mediated by integrins. J Biol Chem 276: 26516–26525 [DOI] [PubMed] [Google Scholar]
- Cascone I, Napione L, Maniero F, Serini G, Bussolino F 2005. Stable interaction between α5β1 integrin and Tie2 tyrosine kinase receptor regulates endothelial cell response to Ang-1. J Cell Biol 170: 993–1004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang SH, Kanasaki K, Gocheva V, Blum G, Harper J, Moses MA, Shih SC, Nagy JA, Joyce J, Bogyo M, et al. 2009. VEGF-A induces angiogenesis by perturbing the cathepsin-cysteine protease inhibitor balance in venules, causing basement membrane degradation and mother vessel formation. Cancer Res 69: 4537–4544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen TT, Luque A, Lee S, Anderson SM, Segura T, Iruela-Arispe ML 2010. Anchorage of VEGF to the extracellular matrix conveys differential signaling responses to endothelial cells. J Cell Biol 188: 595–609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chun TH, Sabeh F, Ota I, Murphy H, McDonagh KT, Holmbeck K, Birkedal-Hansen H, Allen ED, Weiss SJ 2004. MT1-MMP-dependent neovessel formation within the confines of the three-dimensional extracellular matrix. J Cell Biol 167: 757–767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costell M, Gustafsson E, Aszodi A, Morgelin M, Bloch W, Hunziker E, Addicks K, Timpl R, Fassler R 1999. Perlecan maintains the integrity of cartilage and some basement membranes. J Cell Biol 147: 1109–1122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis GE, Bayless KJ 2003. An integrin and Rho GTPase-dependent pinocytic vacuole mechanism controls capillary lumen formation in collagen and fibrin matrices. Microcirculation 10: 27–44 [DOI] [PubMed] [Google Scholar]
- Davis GE, Camarillo CW 1995. Regulation of endothelial cell morphogenesis by integrins, mechanical forces, and matrix guidance pathways. Exp Cell Res 216: 113–123 [DOI] [PubMed] [Google Scholar]
- Davis GE, Camarillo CW 1996. An α2β1 integrin-dependent pinocytic mechanism involving intracellular vacuole formation and coalescence regulates capillary lumen and tube formation in three-dimensional collagen matrix. Exp Cell Res 224: 39–51 [DOI] [PubMed] [Google Scholar]
- Davis GE, Senger DR 2005. Endothelial extracellular matrix: biosynthesis, remodeling, and functions during vascular morphogenesis and neovessel stabilization. Circ Res 97: 1093–1107 [DOI] [PubMed] [Google Scholar]
- Davis GE, Senger DR 2008. Extracellular matrix mediates a molecular balance between vascular morphogenesis and regression. Curr Opin Hematol 15: 197–203 [DOI] [PubMed] [Google Scholar]
- Davis GE, Bayless KJ, Davis MJ, Meininger GA 2000. Regulation of tissue injury responses by the exposure of matricryptic sites within extracellular matrix molecules. Am J Pathol 156: 1489–1498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis GE, Koh W, Stratman AN 2007. Mechanisms controlling human endothelial lumen formation and tube assembly in three-dimensional extracellular matrices. Birth Defects Res C Embryo Today 81: 270–285 [DOI] [PubMed] [Google Scholar]
- Dejana E, Languino LR, Polentarutti N, Balconi G, Ryckewaert JJ, Larrieu MJ, Donati MB, Mantovani A, Marguerie G 1985. Interaction between fibrinogen and cultured endothelial cells. Induction of migration and specific binding. J Clin Invest 75: 11–18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delvos U, Gajdusek C, Sage H, Harker LA, Schwartz SM 1982. Interactions of vascular wall cells with collagen gels. Lab Invest 46: 61–72 [PubMed] [Google Scholar]
- Dong L, Chen Y, Lewis M, Hsieh JC, Reing J, Chaillet JR, Howell CY, Melhem M, Inoue S, Kuszak JR, et al. 2002. Neurologic defects and selective disruption of basement membranes in mice lacking entactin-1/nidogen-1. Lab Invest 82: 1617–1630 [DOI] [PubMed] [Google Scholar]
- Drake CJ, Little CD 1999. VEGF and vascular fusion: Implications for normal and pathological vessels. J Histochem Cytochem 47: 1351–1355 [DOI] [PubMed] [Google Scholar]
- Drake CJ, Brandt SJ, Trusk TC, Little CD 1997. TAL1SCL is expressed in endothelial progenitor cells/angioblasts and defines a dorsal-to-ventral gradient of vasculogenesis. Dev Biol 192: 17–30 [DOI] [PubMed] [Google Scholar]
- Eble JA, Niland S 2009. The extracellular matrix of blood vessels. Curr Pharm Des 15: 1385–1400 [DOI] [PubMed] [Google Scholar]
- Egginton S, Gerritsen M 2003. Lumen formation: In vivo versus in vitro observations. Microcirculation 10: 45–61 [DOI] [PubMed] [Google Scholar]
- Fang F, Orend G, Watanabe N, Hunter T, Ruoslahti E 1996. Dependence of cyclin E-CDK2 kinase activity on cell anchorage. Science 271: 499–502 [DOI] [PubMed] [Google Scholar]
- Feng W, McCabe NP, Mahabeleshwar GH, Somanath PR, Phillips DR, Byzova TV 2008. The angiogenic response is dictated by β3 integrin on bone marrow-derived cells. J Cell Biol 183: 1145–1157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folkman J, Haudenschild C 1980. Angiogenesis in vitro. Nature 288: 551–556 [DOI] [PubMed] [Google Scholar]
- Fouser L, Iruela-Arispe L, Bornstein P, Sage EH 1991. Transcriptional activity of the α1(I)-collagen promoter is correlated with the formation of capillary-like structures by endothelial cells in vitro. J Biol Chem 266: 18345–18351 [PubMed] [Google Scholar]
- Francis SE, Goh KL, Hodivala-Dilke K, Bader BL, Stark M, Davidson D, Hynes RO 2002. Central roles of α5β1 integrin and fibronectin in vascular development in mouse embryos and embryoid bodies. Arterioscler Thromb Vasc Biol 22: 927–933 [DOI] [PubMed] [Google Scholar]
- Friedlander M, Brooks PC, Shaffer RW, Kincaid CM, Varner JA, Cheresh DA 1995. Definition of two angiogenic pathways by distinct α v integrins. Science 270: 1500–1502 [DOI] [PubMed] [Google Scholar]
- Fukai N, Eklund L, Marneros AG, Oh SP, Keene DR, Tamarkin L, Niemela M, Ilves M, Li E, Pihlajaniemi T, et al. 2002. Lack of collagen XVIII/endostatin results in eye abnormalities. EMBO J 21: 1535–1544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao M, Craig D, Lequin O, Campbell ID, Vogel V, Schulten K 2003. Structure and functional significance of mechanically unfolded fibronectin type III1 intermediates. Proc Natl Acad Sci 100: 14784–14789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia JG, Liu F, Verin AD, Birukova A, Dechert MA, Gerthoffer WT, Bamberg JR, English D 2001. Sphingosine 1-phosphate promotes endothelial cell barrier integrity by Edg-dependent cytoskeletal rearrangement. J Clin Invest 108: 689–701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- George EL, Georges-Labouesse EN, Patel-King RS, Rayburn H, Hynes RO 1993. Defects in mesoderm, neural tube and vascular development in mouse embryos lacking fibronectin. Development 119: 1079–1091 [DOI] [PubMed] [Google Scholar]
- George EL, Baldwin HS, Hynes RO 1997. Fibronectins are essential for heart and blood vessel morphogenesis but are dispensable for initial specification of precursor cells. Blood 90: 3073–3081 [PubMed] [Google Scholar]
- Gerhardt H, Golding M, Fruttiger M, Ruhrberg C, Lundkvist A, Abramsson A, Jeltsch M, Mitchell C, Alitalo K, Shima D, et al. 2003. VEGF guides angiogenic sprouting utilizing endothelial tip cell filopodia. J Cell Biol 161: 1163–1177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giancotti FG, Ruoslahti E 1999. Integrin signaling. Science 285: 1028–1032 [DOI] [PubMed] [Google Scholar]
- Grant DS, Kleinman HK 1997. Regulation of capillary formation by laminin and other components of the extracellular matrix. EXS 79: 317–333 [DOI] [PubMed] [Google Scholar]
- Haas TL, Davis SJ, Madri JA 1998. Three-dimensional type I collagen lattices induce coordinate expression of matrix metalloproteinases MT1-MMP and MMP-2 in microvascular endothelial cells. J Biol Chem 273: 3604–3610 [DOI] [PubMed] [Google Scholar]
- Hallmann R, Horn N, Selg M, Wendler O, Pausch F, Sorokin LM 2005. Expression and function of laminins in the embryonic and mature vasculature. Physiol Rev 85: 979–1000 [DOI] [PubMed] [Google Scholar]
- Hayashi K, Madri JA, Yurchenco PD 1992. Endothelial cells interact with the core protein of basement membrane perlecan through β1 and β3 integrins: An adhesion modulated by glycosaminoglycan. J Cell Biol 119: 945–959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoang MV, Whelan MC, Senger DR 2004. Rho activity critically and selectively regulates endothelial cell organization during angiogenesis. Proc Natl Acad Sci 101: 1874–1879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang G, Zhang Y, Kim B, Ge G, Annis DS, Mosher DF, Greenspan DS 2009. Fibronectin binds and enhances the activity of bone morphogenetic protein 1. J Biol Chem 284: 25879–25888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hynes RO 2007. Cell-matrix adhesion in vascular development. J Thromb Haemost 5: 32–40 [DOI] [PubMed] [Google Scholar]
- Hynes RO 2009. The extracellular matrix: Not just pretty fibrils. Science 326: 1216–1219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ilan N, Mahooti S, Madri JA 1998. Distinct signal transduction pathways are utilized during the tube formation and survival phases of in vitro angiogenesis. J Cell Sci 111: 3621–3631 [DOI] [PubMed] [Google Scholar]
- Ingber D, Folkman J 1988. Inhibition of angiogenesis through modulation of collagen metabolism. Lab Invest 59: 44–51 [PubMed] [Google Scholar]
- Iruela-Arispe ML, Davis GE 2009. Cellular and molecular mechanisms of vascular lumen formation. Dev Cell 16: 222–231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iruela-Arispe ML, Diglio CA, Sage EH 1991. Modulation of extracellular matrix proteins by endothelial cells undergoing angiogenesis in vitro. Arterioscler Thromb 11: 805–815 [DOI] [PubMed] [Google Scholar]
- Jackson CJ, Knop A, Giles I, Jenkins K, Schrieber L 1994. VLA-2 mediates the interaction of collagen with endothelium during in vitro vascular tube formation. Cell Biol Int 18: 859–867 [DOI] [PubMed] [Google Scholar]
- Kamei M, Saunders WB, Bayless KJ, Dye L, Davis GE, Weinstein BM 2006. Endothelial tubes assemble from intracellular vacuoles in vivo. Nature 442: 453–456 [DOI] [PubMed] [Google Scholar]
- Kanematsu A, Yamamoto S, Ozeki M, Noguchi T, Kanatani I, Ogawa O, Tabata Y 2004. Collagenous matrices as release carriers of exogenous growth factors. Biomaterials 25: 4513–4520 [DOI] [PubMed] [Google Scholar]
- Koh W, Stratman AN, Sacharidou A, Davis GE 2008. In vitro three dimensional collagen matrix models of endothelial lumen formation during vasculogenesis and angiogenesis. Meth Enzymol 443: 83–101 [DOI] [PubMed] [Google Scholar]
- Koh W, Sachidanandam K, Stratman AN, Sacharidou A, Mayo AM, Murphy EA, Cheresh DA, Davis GE 2009. Formation of endothelial lumens requires a coordinated PKC{epsilon}-, Src-, Pak- and Raf-kinase-dependent signaling cascade downstream of Cdc42 activation. J Cell Sci 122: 1812–1822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y, Senger DR 2004. Matrix-specific activation of Src and Rho initiates capillary morphogenesis of endothelial cells. FASEB J 18: 457–468 [DOI] [PubMed] [Google Scholar]
- Lu P, Takai K, Weaver V, Werb Z 2011. Extracellular matrix degradation and remodeling in development and disease. Cold Spring Harb Perspect Biol 10.1101/cshperspect.a005058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lubarsky B, Krasnow MA 2003. Tube morphogenesis: Making and shaping biological tubes. Cell 112: 19–28 [DOI] [PubMed] [Google Scholar]
- Mancuso MR, Davis R, Norberg SM, O’Brien S, Sennino B, Nakahara T, Yao VJ, Inai T, Brooks P, Freimark B, et al. 2006. Rapid vascular regrowth in tumors after reversal of VEGF inhibition. J Clin Invest 116: 2610–2621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Margosio B, Marchetti D, Vergani V, Giavazzi R, Rusnati M, Presta M, Taraboletti G 2003. Thrombospondin 1 as a scavenger for matrix-associated fibroblast growth factor 2. Blood 102: 4399–4406 [DOI] [PubMed] [Google Scholar]
- Meredith JE, Schwartz MA 1997. Integrins, adhesion and apoptosis. Trends Cell Biol 7: 146–150 [DOI] [PubMed] [Google Scholar]
- Meyer GT, Matthias LJ, Noack L, Vadas MA, Gamble JR 1997. Lumen formation during angiogenesis in vitro involves phagocytic activity, formation and secretion of vacuoles, cell death, and capillary tube remodelling by different populations of endothelial cells. Anat Rec 249: 327–340 [DOI] [PubMed] [Google Scholar]
- Miner JH, Yurchenco PD 2004. Laminin functions in tissue morphogenesis. Annu Rev Cell Dev Biol 20: 255–284 [DOI] [PubMed] [Google Scholar]
- Miner JH, Cunningham J, Sanes JR 1998. Roles for laminin in embryogenesis: Exencephaly, syndactyly, and placentopathy in mice lacking the laminin α5 chain. J Cell Biol 143: 1713–1723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miosge N, Sasaki T, Timpl R 2002. Evidence of nidogen-2 compensation for nidogen-1 deficiency in transgenic mice. Matrix Biol 21: 611–621 [DOI] [PubMed] [Google Scholar]
- Mitsi M, Forsten-Williams K, Gopalakrishnan M, Nugent MA 2008. A catalytic role of heparin within the extracellular matrix. J Biol Chem 283: 34796–34807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montesano R, Orci L, Vassalli P 1983. In vitro rapid organization of endothelial cells into capillary-like networks is promoted by collagen matrices. J Cell Biol 97: 1648–1652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morla A, Ruoslaht E 1992. A fibronectin self-assembly site involved in fibronectin matrix assembly: Reconstruction in a synthetic peptide. J Cell Biol 118: 421–429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murshed M, Smyth N, Miosge N, Karolat J, Krieg T, Paulsson M, Nischt R 2000. The absence of nidogen 1 does not affect murine basement membrane formation. Mol Cell Biol 20: 7007–7012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakatsu MN, Hughes CC 2008. An optimized three-dimensional in vitro model for the analysis of angiogenesis. Methods Enzymol 443: 65–82 [DOI] [PubMed] [Google Scholar]
- Nicosia RF, Madri JA 1987. The microvascular extracellular matrix. Developmental changes during angiogenesis in the aortic ring-plasma clot model. Am J Pathol 128: 78–90 [PMC free article] [PubMed] [Google Scholar]
- Paku S, Paweletz N 1991. First steps of tumor-related angiogenesis. Lab Invest 65: 334–346 [PubMed] [Google Scholar]
- Perruzzi CA, de Fougerolles AR, Koteliansky VE, Whelan MC, Westlin WF, Senger DR 2003. Functional overlap and cooperativity among αv and β1 integrin subfamilies during skin angiogenesis. J Invest Dermatol 120: 1100–1109 [DOI] [PubMed] [Google Scholar]
- Poschl E, Schlotzer-Schrehardt U, Brachvogel B, Saito K, Ninomiya Y, Mayer U 2004. Collagen IV is essential for basement membrane stability but dispensable for initiation of its assembly during early development. Development 131: 1619–1628 [DOI] [PubMed] [Google Scholar]
- Rahman S, Patel Y, Murray J, Patel KV, Sumathipala R, Sobel M, Wijelath ES 2005. Novel hepatocyte growth factor (HGF) binding domains on fibronectin and vitronectin coordinate a distinct and amplified Met-integrin induced signalling pathway in endothelial cells. BMC Cell Biol 6: 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramirez F, Dietz HC 2007. Fibrillin-rich microfibrils: Structural determinants of morphogenetic and homeostatic events. J Cell Physiol 213: 326–330 [DOI] [PubMed] [Google Scholar]
- Ramirez F, Dietz HC 2009. Extracellular microfibrils in vertebrate development and disease processes. J Biol Chem 284: 14677–14681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes JM, Simons M 2007. The extracellular matrix and blood vessel formation: Not just a scaffold. J Cell Mol Med 11: 176–205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richard L, Velasco P, Detmar M 1998. A simple immunomagnetic protocol for the selective isolation and long-term culture of human dermal microvascular endothelial cells. Exp Cell Res 240: 1–6 [DOI] [PubMed] [Google Scholar]
- Risau W, Lemmon V 1988. Changes in the vascular extracellular matrix during embryonic vasculogenesis and angiogenesis. Dev Biol 125: 441–450 [DOI] [PubMed] [Google Scholar]
- Roovers K, Assoian RK 2000. Integrating the MAP kinase signal into the G1 phase cell cycle machinery. Bioessays 22: 818–826 [DOI] [PubMed] [Google Scholar]
- Rowe RG, Weiss SJ 2008. Breaching the basement membrane: Who, when and how? Trends Cell Biol 18: 560–574 [DOI] [PubMed] [Google Scholar]
- Ruehl M, Somasundaram R, Schoenfelder I, Farndale RW, Knight CG, Schmid M, Ackermann R, Riecken EO, Zeitz M, Schuppan D 2002. The epithelial mitogen keratinocyte growth factor binds to collagens via the consensus sequence glycine-proline-hydroxyproline. J Biol Chem 277: 26872–26878 [DOI] [PubMed] [Google Scholar]
- Sacharidou A, Koh W, Stratman AN, Mayo AM, Fisher KE, Davis GE 2010. Endothelial lumen signaling complexes control 3D matrix-specific tubulogenesis through interdependent Cdc42- and MT1-MMP-mediated events. Blood 115: 5259–5269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saharinen P, Eklund L, Miettinen J, Wirkkala R, Anisimov A, Winderlich M, Nottebaum A, Vestweber D, Deutsch U, Koh GY, et al. 2008. Angiopoietins assemble distinct Tie2 signalling complexes in endothelial cell–cell and cell–matrix contacts. Nat Cell Biol 10: 527–537 [DOI] [PubMed] [Google Scholar]
- Sainson RC, Aoto J, Nakatsu MN, Holderfield M, Conn E, Koller E, Hughes CC 2005. Cell-autonomous notch signaling regulates endothelial cell branching and proliferation during vascular tubulogenesis. FASEB J 19: 1027–1029 [DOI] [PubMed] [Google Scholar]
- Sakai T, Larsen M, Yamada KM 2003. Fibronectin requirement in branching morphogenesis. Nature 423: 876–881 [DOI] [PubMed] [Google Scholar]
- San Antonio JD, Zoeller JJ, Habursky K, Turner K, Pimtong W, Burrows M, Choi S, Basra S, Bennett JS, DeGrado WF, et al. 2009. A key role for the integrin α2β1 in experimental and developmental angiogenesis. Am J Pathol 175: 1338–1347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders WB, Bohnsack BL, Faske JB, Anthis NJ, Bayless KJ, Hirschi KK, Davis GE 2006. Coregulation of vascular tube stabilization by endothelial cell TIMP-2 and pericyte TIMP-3. J Cell Biol 175: 179–191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwarzbauer JE, DeSimone DW 2011. Fibronectins, their fibrillogenesis, and in vivo functions. Cold Spring Harb Perspect Biol 3: a005041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seger R, Krebs EG 1995. The MAPK signaling cascade. FASEB J 9: 726–735 [PubMed] [Google Scholar]
- Senger DR 1996. Molecular framework for angiogenesis: A complex web of interactions between extravasated plasma proteins and endothelial cell proteins induced by angiogenic cytokines. Am J Pathol 149: 1–7 [PMC free article] [PubMed] [Google Scholar]
- Senger DR, Perruzzi CA 1996. Cell migration promoted by a potent GRGDS-containing thrombin-cleavage fragment of osteopontin. Biochim Biophys Acta 1314: 13–24 [DOI] [PubMed] [Google Scholar]
- Senger DR, Claffey KP, Benes JE, Perruzzi CA, Sergiou AP, Detmar M 1997. Angiogenesis promoted by vascular endothelial growth factor: Regulation through α1β1 and α2β1 integrins. Proc Natl Acad Sci 94: 13612–13617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senger DR, Perruzzi CA, Streit M, Koteliansky VE, de Fougerolles AR, Detmar M 2002. The α1β1 and α2β1 integrins provide critical support for vascular endothelial growth factor signaling, endothelial cell migration, and tumor angiogenesis. Am J Pathol 160: 195–204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Short SM, Talbott GA, Juliano RL 1998. Integrin-mediated signaling events in human endothelial cells. Mol Biol Cell 9: 1969–1980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith ML, Gourdon D, Little WC, Kubow KE, Eguiluz RA, Luna-Morris S, Vogel V 2007. Force-induced unfolding of fibronectin in the extracellular matrix of living cells. PLoS Biol 5: e268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Somanath PR, Ciocea A, Byzova TV 2009. Integrin and growth factor receptor alliance in angiogenesis. Cell Biochem Biophys 53: 53–64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- St Croix B, Rago C, Velculescu V, Traverso G, Romans KE, Montgomery E, Lal A, Riggins GJ, Lengauer C, Vogelstein B, et al. 2000. Genes expressed in human tumor endothelium. Science 289: 1197–1202 [DOI] [PubMed] [Google Scholar]
- Stratman AN, Malotte KM, Mahan RD, Davis MJ, Davis GE 2009a. Pericyte recruitment during vasculogenic tube assembly stimulates endothelial basement membrane matrix formation. Blood 114: 5091–5101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stratman AN, Saunders WB, Sacharidou A, Koh W, Fisher KE, Zawieja DC, Davis MJ, Davis GE 2009b. Endothelial cell lumen and vascular guidance tunnel formation requires MT1-MMP-dependent proteolysis in 3-dimensional collagen matrices. Blood 114: 237–247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stratman AN, Schwindt AE, Malotte KM, Davis GE 2010. Endothelial-derived PDGF-BB and HB-EGF coordinately regulate pericyte recruitment during vasculogenic tube assembly and stabilization. Blood 116: 4720–4730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Streit M, Riccardi L, Velasco P, Brown LF, Hawighorst T, Bornstein P, Detmar M 1999. Thrombospondin-2: A potent endogenous inhibitor of tumor growth and angiogenesis. Proc Natl Acad Sci 96: 14888–14893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stupack DG, Cheresh DA 2004. Integrins and angiogenesis. Curr Top Dev Biol 64: 207–238 [DOI] [PubMed] [Google Scholar]
- Sund M, Xie L, Kalluri R 2004. The contribution of vascular basement membranes and extracellular matrix to the mechanics of tumor angiogenesis. Apmis 112: 450–462 [DOI] [PubMed] [Google Scholar]
- Sundberg C, Nagy JA, Brown LF, Feng D, Eckelhoefer IA, Manseau EJ, Dvorak AM, Dvorak HF 2001. Glomeruloid microvascular proliferation follows adenoviral vascular permeability factor/vascular endothelial growth factor-164 gene delivery. Am J Pathol 158: 1145–1160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sweeney SM, Guy CA, Fields GB, San Antonio JD 1998. Defining the domains of type I collagen involved in heparin- binding and endothelial tube formation. Proc Natl Acad Sci 95: 7275–7280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sweeney SM, DiLullo G, Slater SJ, Martinez J, Iozzo RV, Lauer-Fields JL, Fields GB, San Antonio JD 2003. Angiogenesis in collagen I requires α2β1 ligation of a GFP*GER sequence and possibly p38 MAPK activation and focal adhesion disassembly. J Biol Chem 278: 30516–30524 [DOI] [PubMed] [Google Scholar]
- Thyboll J, Kortesmaa J, Cao R, Soininen R, Wang L, Iivanainen A, Sorokin L, Risling M, Cao Y, Tryggvason K 2002. Deletion of the laminin α4 chain leads to impaired microvessel maturation. Mol Cell Biol 22: 1194–1202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vakonakis I, Staunton D, Rooney LM, Campbell ID 2007. Interdomain association in fibronectin: Insight into cryptic sites and fibrillogenesis. EMBO J 26: 2575–2583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Hinsbergh VW, Collen A, Koolwijk P 2001. Role of fibrin matrix in angiogenesis. Ann NY Acad Sci 936: 426–437 [DOI] [PubMed] [Google Scholar]
- Vernon RB, Sage EH 1995. Between molecules and morphology: Extracellular matrix and creation of vascular form. Am J Pathol 147: 873–883 [PMC free article] [PubMed] [Google Scholar]
- Vinals F, Pouyssegur J 1999. Confluence of vascular endothelial cells induces cell cycle exit by inhibiting p42/p44 mitogen-activated protein kinase activity. Mol Cell Biol 19: 2763–2772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogel V 2006. Mechanotransduction involving multimodular proteins: Converting force into biochemical signals. Annu Rev Biophys Biomol Struct 35: 459–488 [DOI] [PubMed] [Google Scholar]
- Wagenseil JE, Mecham RP 2009. Vascular extracellular matrix and arterial mechanics. Physiol Rev 89: 957–989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X, Harris RE, Bayston LJ, Ashe HL 2008. Type IV collagens regulate BMP signalling in Drosophila. Nature 455: 72–77 [DOI] [PubMed] [Google Scholar]
- Wary KK, Mainiero F, Isakoff SJ, Marcantonio EE, Giancotti FG 1996. The adaptor protein Shc couples a class of integrins to the control of cell cycle progression. Cell 87: 733–743 [DOI] [PubMed] [Google Scholar]
- Waschke J, Baumgartner W, Adamson RH, Zeng M, Aktories K, Barth H, Wilde C, Curry FE, Drenckhahn D 2004. Requirement of Rac activity for maintenance of capillary endothelial barrier properties. Am J Physiol Heart Circ Physiol 286: H394–H401 [DOI] [PubMed] [Google Scholar]
- Whelan MC, Senger DR 2003. Collagen I initiates endothelial cell morphogenesis by inducing actin polymerization through suppression of cyclic AMP and protein kinase A. J Biol Chem 278: 327–334 [DOI] [PubMed] [Google Scholar]
- Wijelath ES, Murray J, Rahman S, Patel Y, Ishida A, Strand K, Aziz S, Cardona C, Hammond WP, Savidge GF, et al. 2002. Novel vascular endothelial growth factor binding domains of fibronectin enhance vascular endothelial growth factor biological activity. Circ Res 91: 25–31 [DOI] [PubMed] [Google Scholar]
- Wiradjaja F, DiTommaso T, Smyth I 2010. Basement membranes in development and disease. Birth Defects Res C Embryo Today 90: 8–31 [DOI] [PubMed] [Google Scholar]
- Wojciak-Stothard B, Ridley AJ 2002. Rho GTPases and the regulation of endothelial permeability. Vascul Pharmacol 39: 187–199 [DOI] [PubMed] [Google Scholar]
- Yang S, Graham J, Kahn JW, Schwartz EA, Gerritsen ME 1999. Functional roles for PECAM-1 (CD31) and VE-cadherin (CD144) in tube assembly and lumen formation in three-dimensional collagen gels. Am J Pathol 155: 887–895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Z, Ramirez NE, Yankeelov TE, Li Z, Ford LE, Qi Y, Pozzi A, Zutter MM 2008. α2β1 integrin expression in the tumor microenvironment enhances tumor angiogenesis in a tumor cell-specific manner. Blood 111: 1980–1988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhong C, Chrzanowska-Wodnicka M, Brown J, Shaub A, Belkin AM, Burridge K 1998. Rho-mediated contractility exposes a cryptic site in fibronectin and induces fibronectin matrix assembly. J Cell Biol 141: 539–551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou Z, Apte SS, Soininen R, Cao R, Baaklini GY, Rauser RW, Wang J, Cao Y, Tryggvason K 2000. Impaired endochondral ossification and angiogenesis in mice deficient in membrane-type matrix metalloproteinase I. Proc Natl Acad Sci 97: 4052–4057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou X, Rowe RG, Hiraoka N, George JP, Wirtz D, Mosher DF, Virtanen I, Chernousov MA, Weiss SJ 2008. Fibronectin fibrillogenesis regulates three-dimensional neovessel formation. Genes Dev 22: 1231–1243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu X, Ohtsubo M, Bohmer RM, Roberts JM, Assoian RK 1996. Adhesion-dependent cell cycle progression linked to the expression of cyclin D1, activation of cyclin E-cdk2, and phosphorylation of the retinoblastoma protein. J Cell Biol 133: 391–403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zweers MC, Davidson JM, Pozzi A, Hallinger R, Janz K, Quondamatteo F, Leutgeb B, Krieg T, Eckes B 2007. Integrin α2β1 is required for regulation of murine wound angiogenesis but is dispensable for reepithelialization. J Invest Dermatol 127: 467–478 [DOI] [PubMed] [Google Scholar]