Abstract
Background: In January 2007, Texas expanded the Children's Health Insurance Program (CHIP) to include perinatal care for the unborn children of undocumented low-income women and certain documented women ineligible for Medicaid or CHIP because of income or residency status. CHIP Perinatal includes coverage for undocumented women and provides a glimpse into the birth outcomes of this difficult-to-reach population.
Objective: Community Health Choice (CHC) is the largest health maintenance organization provider of CHIP Perinatal in Texas, and we sought to determine preterm and low-birth-weight rates among women enrolled in CHC CHIP Perinatal and compare them with women of similar low-income status enrolled in Medicaid.
Methods: We conducted a retrospective cohort study of women enrolled in the CHC CHIP Perinatal and Medicaid plans and who delivered between January 1 and August 31, 2008. Logistic regression was used to determine odds of poor birth outcome, and analyses were adjusted for maternal age.
Results: The CHC cohort included 10,763 pregnant women enrolled in CHIP Perinatal and 4614 pregnant women enrolled in Medicaid. Those in the Medicaid group are significantly more likely to have preterm (adjusted odds ratio [aOR] = 2.1; 95% confidence interval [CI], 1.8–2.4) and low-birth-weight infants (aOR = 2.2; 95% CI, 1.9–2.6) than those in the CHIP Perinatal group. Within the Medicaid population, Hispanic women have the lowest preterm and low-birth-weight rates (6.6% and 5.8%, respectively), and non-Hispanic black women have the highest preterm and low-birth-weight rates (11.3% and 12.4%, respectively). However, Hispanic women enrolled in Medicaid are more likely to have preterm (aOR = 1.7; 95% CI, 1.4–2.1) and low-birth-weight infants (aOR = 1.6; 95% CI ,1.3–2.0) than their mostly Hispanic CHIP Perinatal counterparts.
Conclusion: Women enrolled in CHC CHIP Perinatal have significantly lower prematurity rates than women of similar economic status enrolled in Medicaid, despite receiving less comprehensive medical benefits. Favorable birth outcomes for the mostly Hispanic CHIP Perinatal population persist even when restricting the comparison Medicaid group to Hispanics. Further analysis controlling for factors such as social and behavioral characteristics is needed to better understand differences between the CHIP Perinatal and Medicaid populations.
Introduction
Preterm birth and low birth weight constitute leading causes of infant morbidity and mortality in the US. In 2007, preterm infants accounted for 11.0% and low-birth-weight infants accounted for 6.5% of live singleton births.1 In 2006, preterm-related complications accounted for 36.1% of infant deaths.2 In addition to high infant mortality, premature infants incur more health complications than full-term infants.3,4 According to a 2007 report from the Institute of Medicine, preterm infants resulted in an average medical expenditure of $33,200 in the first year of life, compared with $3325 for full-term infants.5 The high rate and cost of preterm and low-birth-weight infants are growing public health concerns, and addressing issues of prematurity is essential to improving birth outcomes.
Texas has high preterm and low-birth-weight rates. In 2007, preterm infants accounted for 12.1% and low-birth-weight infants accounted for 6.7% of live singleton births (Center for Health Statistics, personal communication, 29 Nov 2010).a Two public insurance programs provide coverage for the majority of low-income pregnant women in Texas: the State of Texas Access Reform (STAR) Medicaid plan and the Children's Health Insurance Program (CHIP) Perinatal plan.6 For simplicity, we refer to STAR Medicaid as Texas Medicaid. Texas Medicaid provides comprehensive medical coverage and unlimited prescriptions for pregnancy and non-pregnancy-related conditions. Eligibility requires an income ≤185% of the federal poverty guideline7 and a minimum of five years as a permanent resident. CHIP Perinatal is an extension of CHIP and provides coverage for the unborn children of undocumented women, documented women with less than five years' permanent residency status, and some higher-income women not eligible for Medicaid or CHIP. Eligibility requires an income ≤200% of the federal poverty guideline, and there is no stipulation on residency status. The CHIP Perinatal program only covers medical care related to the unborn child. Benefits include up to 20 prenatal visits, prescription coverage for pregnancy-related conditions, labor and delivery, and two postpartum visits.
In 2008, women comprised 39% of the adult undocumented immigrant population in the US, and infants born to an undocumented parent comprised 8% (340,000) of US births.8 Texas has the second largest population of undocumented immigrants, estimated at 1.45 million (of 11.9 million in the US).9 CHIP Perinatal serves as the safety-net public insurance for the unborn children of undocumented women. Launched in January 2007, Texas CHIP Perinatal has enrolled 182,549 unborn children (Center for Strategic Decision Support, personal communication, 2010 Nov 30).b However, the program's impact on birth outcomes is not known. Although it provides perinatal care for the unborn child, it does not cover non-pregnancy-related conditions for the pregnant woman. We conducted a retrospective cohort study to determine the preterm and low-birth-weight rates of women enrolled in CHIP Perinatal and compare them with women of similar low-income status enrolled in Texas Medicaid.
Methods
Data Source
Community Health Choice (CHC) is the largest health maintenance organization (HMO) provider of CHIP Perinatal in Texas and sole provider in the 20 counties of the Texas Gulf Coast region. It also administers the Texas Medicaid program in 6 of the 20 Texas Gulf Coast counties. The CHC database contains members' date of birth, ZIP code of residence, information on other primary insurance, and data on the newborn's gestational age and birth weight. Claims data identify pregnant women and live infants with a diagnosis code from the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) for pre-term birth. CHC also encourages facilities to submit delivery notifications with data on gestational age. These identified additional preterm births. Self-reported maternal race and/or ethnicity data was abstracted for Texas Medicaid members only. CHIP Perinatal does not collect race and/or ethnicity data for pregnant women or the infants they deliver.
Participants
The study population included pregnant women enrolled in the CHC CHIP Perinatal or Medicaid programs, who resided in Brazoria, Fort Bend, Galveston, Harris, Montgomery, or Waller County, and delivered between January 1 and August 31, 2008. Pregnant women possessing other primary insurance were excluded. The final study population included singleton neonates with birth weights ≥500g delivered to women meeting the inclusion criteria. Multiple-gestation births were excluded because those babies are more likely to be born preterm and at low birth weights.
Definitions of Variables
Pregnancy outcomes of interest included preterm birth and low birth weight. Preterm birth was defined as birth before 37 completed weeks of gestation. Low birth weight was defined as a weight <2500g at birth.
Statistical Analysis
Statistical analysis was carried out with Stata software (version 9.2; StataCorp, College Station, TX, USA). Logistic regression was used to determine odds of poor birth outcome for babies delivered by women in the CHC CHIP Perinatal and Medicaid plans. Analyses were adjusted for maternal age. Odds ratios (OR) with 95% confidence intervals (CIs) were calculated. ORs were considered statistically signifi-cant if the 95% CIs excluded one.
Results
Women enrolled in CHC CHIP Perinatal delivered 10,966 babies between January 1 and August 31, 2008. Analysis excluded 96 sets of twins, 2 sets of triplets, 4 singletons with birth weights <500g, and 1 fetus that died. The final CHIP Perinatal study population included 10,763 singletons.
Women enrolled in CHC Texas Medicaid delivered 5015 babies between January 1 and August 31, 2008. Analysis excluded 68 sets of twins, 1 baby whose twin sibling died, 1 baby whose twin sibling's member number could not be located, 6 singletons with birth weights <500 g, 3 fetuses that died, and 254 babies delivered to women with other primary insurance. The final CHC Texas Medicaid study population included 4614 singletons.
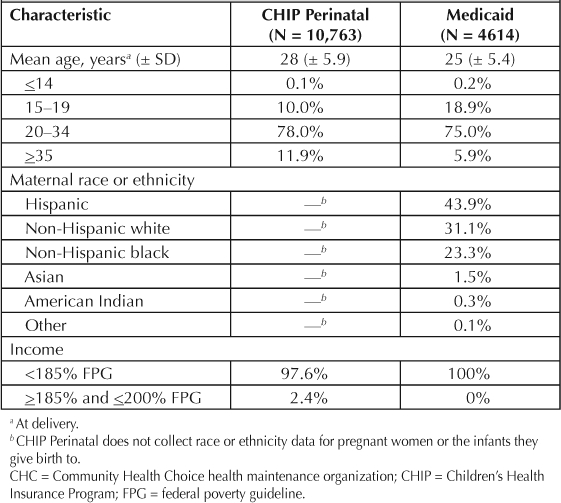
Maternal demographics are summarized in Table 1. Women enrolled in CHC CHIP Perinatal were older than women enrolled in Texas Medicaid. Both groups had similar incomes. Only 2.4% of women with CHIP Perinatal did not meet eligibility criteria for Texas Medicaid because of income status alone (income >185% but ≤200% of the federal poverty guideline). Although the CHIP Perinatal database does not contain race or ethnicity data, surname analysis suggests that the overwhelming majority of women enrolled in CHIP Perinatal are Hispanic.
Table 1.
Demographic characteristics of women enrolled in CHC CHIP Perinatal and Medicaid
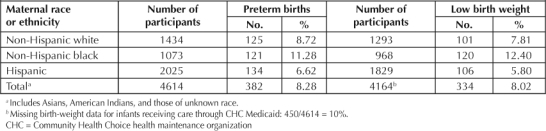
Infants born to CHIP Perinatal-enrolled women had significantly lower preterm and low-birth-weight rates than infants born to women receiving Texas Medicaid. Singleton infants born to women with CHC Texas Medicaid were more likely to be preterm (adjusted odds ratio [aOR] = 2.1; CI, 1.8-2.4) and have low birth weight (aOR = 2.2; CI, 1.9–2.6) than infants born to women with CHIP Perinatal (Table 2). Among infants born to women receiving care through Texas Medicaid, Hispanic infants had the lowest preterm and low-birth-weight rates (6.6% and 5.8%, respectively), and non-Hispanic black infants had the highest preterm and low-birth-weight rates (11.3% and 12.4%, respectively) (Table 3). Although infants born to Hispanic women enrolled in Medicaid had lower preterm and low-birth-weight rates compared with other infants born to non-Hispanic women enrolled in Medicaid, these rates were higher than their mostly Hispanic CHIP Perinatal counterparts. Infants born to Hispanic women enrolled in Medicaid were more likely to be preterm (aOR, 1.7; CI, 1.4–2.1) and have low birth weight (aOR, 1.6; CI, 1.3–2.0) than CHIP Perinatal infants.
Table 2.
Birth outcomes among women enrolled in CHC CHIP Perinatal and Medicaida
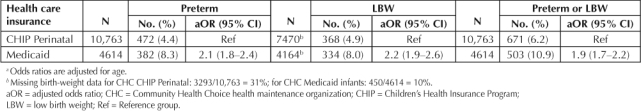
Table 3.
Birth outcomes by race or ethnicity of women enrolled in CHC Medicaid
Discussion
In our study, women enrolled in CHIP Perinatal unexpectedly had significantly better birth outcomes than women enrolled in Texas Medicaid, despite more limited medical coverage. The CHIP Perinatal program provides a glimpse into the birth outcomes of undocumented women. Only 2.4% of the women with CHC CHIP Perinatal did not meet eligibility requirements for Medicaid because of income status. The remaining 97.6% presumably did not meet eligibility requirements for Medicaid because of inadequate residency status. It is unclear why this population of mostly undocumented Hispanic women had significantly better birth outcomes compared with their low-income Medicaid counterparts. Ethnicity may play a role. National and regional data consistently show that Hispanics have birth outcomes comparable to those of non-Hispanic whites and significantly better than those of non-Hispanic blacks.2,10 Interestingly, favorable birth outcomes for this mostly Hispanic CHIP Perinatal population persisted even when we restricted the comparison Texas Medicaid population to Hispanic women. Various studies show better birth outcomes and overall health among certain immigrant populations compared with their US-native ethnic-racial counterparts.11,12 Decreased adverse health behaviors, increased social support, and selective migration represent possible explanations for the healthy migrant phenomenon.13,14 Our study results showing differences in birth outcomes by maternal residency status are consistent with outcomes of prior studies showing better health outcomes among certain immigrant populations. However, it is uncertain how factors such as maternal behavior (eg, cigarette smoking, alcohol use, and drug use), level of social support, time of entry into prenatal care, service use, appointment adherence, and self-efficacy compare between women with CHIP Perinatal and Medicaid.
Decreased adverse health behaviors, increased social support, and selective migration represent possible explanations for the healthy migrant phenomenon.13,14
The Department of Health and Human Services Healthy People 2020 report15 and the Institute of Medicine Unequal Treatment16 report highlight the importance of eliminating disparities in health and health care. These reports recommend improved collection of data on race, ethnicity, and primary language by public and private health plans for comparative measurements and disparities reduction. Before the establishment of the National Health Plan Collaborative in 2004, most health plans including Medicare and Medicaid had virtually no race or ethnicity data.17 The systematic collection of data on race and ethnicity proves vital for comparative measurements of health outcomes by race and ethnicity. Understanding the determinants of favorable health outcomes in certain populations is as important as understanding the determinants of poor health outcomes. At the organizational level, the Texas Health and Human Services CHIP Perinatal program should consider exploring means for collecting data on race and ethnicity. This may shed light as to why the CHIP Perinatal population has better birth outcomes.
Limitations
Our study had certain limitations. First, the ideal study evaluating CHIP Perinatal's impact on birth outcomes would entail a comparison of birth outcomes among undocumented low-income women before and after CHIP Perinatal. However, a database of undocumented low-income pregnant women before the advent of CHIP Perinatal does not exist. Second, our study is limited by the use of administrative claims data for epidemiologic analysis. CHC obtains preterm birth ICD-9-CM codes for administrative purposes and pays individual clinicians set professional fees irrespective of whether a birth is coded as preterm. Thus, the pre-term birth rates in our study may represent conservative estimates. Nevertheless, it is not expected that the coding behavior of clinicians would differ between the two health plans. Third, 31% of infants born to CHIP Perinatal-enrolled women and 10% of infants born to women receiving Texas Medicaid had missing birth weight data, and it is not clear if there were any differences in the infants who did have documented birth weights and those who did not. Fourth, the lack of complementary social, behavioral, and clinical data limited our ability to control for such variables. In addition, the lack of race and ethnicity data for CHIP Perinatal members precludes adjustments for those characteristics.
Conclusion
Certain characteristics inherent in the CHIP Perinatal population are associated with lower preterm and low-birth-weight rates compared to the Hispanic Medicaid and overall Medicaid populations. These lower rates exist in spite of limited medical benefits and similar economic status. In contrast, non-Hispanic black women with Medicaid have the highest preterm and low-birth-weight rates. Further studies controlling for factors such as social and behavioral characteristics are needed to better understand the differences between the CHIP Perinatal and Texas Medicaid populations that may account for differences in birth outcomes.
Disclosure Statement
The author(s) have no conflicts of interest to disclose.
Acknowledgments
Katharine O'Moore-Klopf, ELS, of KOK Edit provided editorial assistance.
Footnotes
a Center for Health Statistics, Texas Department of State Health Services
b Center for Strategic Decision Support, Texas Health and Human Services Commission
References
- Martin JA, Hamilton BE, Sutton PD, et al. Births: final data for 2007. National vital statistics reports; vol 58 no. 24 [monograph on the Internet] Hyattsville, MD: National Center for Health Statistics; 2010 Aug 9. [cited 2011 Mar 25]. Available from: www.cdc.gov/nchs/data/nvsr/nvsr58/nvsr58_24.pdf. [PubMed] [Google Scholar]
- Mathews TJ, MacDorman MF. Infant mortality statistics from the 2006 period linked birth/infant death data set. National vital statistics reports; vol 58 no. 17 [monograph on the Internet] Hyattsville, MD: National Center for Health Statistics; 2010 Apr 30. [cited 2011 Mar 25]. Available from: www.cdc.gov/nchs/data/nvsr/nvsr58/nvsr58_17.pdf. [PubMed] [Google Scholar]
- Moster D, Lie RT, Markestad T. Long-term medical and social consequences of preterm birth. N Engl J Med. 2008 Jul 17;359(3):262–73. doi: 10.1056/NEJMoa0706475. [DOI] [PubMed] [Google Scholar]
- McIntire DD, Leveno KJ. Neonatal mortality and morbidity rates in late preterm births compared with births at term. Obstet Gynecol. 2008 Jan 11;111(1):35–41. doi: 10.1097/01.AOG.0000297311.33046.73. [DOI] [PubMed] [Google Scholar]
- Behrman RE, Butler AS, editors. Preterm birth: causes, consequences, and prevention. Washington, DC: National Academies Press; 2007. [PubMed] [Google Scholar]
- Texas Health and Human Services Commission [homepage on the Internet] Austin, TX: Texas Health and Human Services Commission; Texas Medicaid and CHIP in Perspective. 2011 Jan 27. [cited 2011 Mar 28] . Available from: www.hhsc.state.tx.us/medicaid/reports/PB8/PinkBook-TOC.html. [Google Scholar]
- The 2011 HHS Poverty Guidelines [monograph on the Internet] Washington, DC: US Department of Health and Human Services; revised 2011 Jan 21 [cited 2011 Mar 25]. Available from: http://aspe.hhs.gov/poverty/11poverty.shtml. [Google Scholar]
- Passel JS, Taylor P. Unauthorized immigrants and their US-born children [monograph on the Internet] Washington, DC: Pew Hispanic Center; 2010 Aug 11. [cited 2011 Mar 25] . Available from: http://pewhispanic.org/files/reports/125.pdf. [Google Scholar]
- Passel JS, Cohn DV. A portrait of unauthorized immigrants in the United States [monograph on the Internet] Washington, DC: Pew Hispanic Center; 2009 Apr 14. [cited 2011 Mar 25]. Available from: http://pewhispanic.org/files/reports/107.pdf. [Google Scholar]
- Leveno KJ, McIntire DD, Bloom SL, Sibley MR, Anderson RJ. Decreased preterm births in an inner-city public hospital. Obstet Gynecol. 2009 Mar;113(3):578–84. doi: 10.1097/AOG.0b013e318195e257. [DOI] [PubMed] [Google Scholar]
- Singh GK, Hiatt RA. Trends and disparities in socioeconomic and behavioural characteristics, life expectancy, and cause-specific mortality of native-born and foreign-born populations in the United States, 1979– 2003. Int J Epidemiol. 2006 Aug;35(4):903–19. doi: 10.1093/ije/dyl089. [DOI] [PubMed] [Google Scholar]
- Acevedo-Garcia D, Soobader MJ, Berkman LF. The differential effect of foreign-born status on low birth weight by race/ethnicity and education. Pediatrics. 2005 Jan;115(1):e20–30. doi: 10.1542/peds.2004-1306. [DOI] [PubMed] [Google Scholar]
- Elo IT, Culhane JF. Variations in health and health behaviors by nativity among pregnant Black women in Philadelphia. Am J Public Health. 2010 Nov;100(11):2185–92. doi: 10.2105/AJPH.2009.174755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hummer RA, Powers DA, Pullum SG, Gossman GL, Frisbie WP. Paradox found (again): infant mortality among the Mexican-origin population in the United States. Demography. 2007 Aug;44(3):441–57. doi: 10.1353/dem.2007.0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Healthy people 2020 [monograph on the Internet] Washington, DC: US Department of Health and Human Services; 2010. [cited 2011 Mar 25]. Available from: www.healthypeople.gov/2020/about/DisparitiesAbout.aspx. [Google Scholar]
- Smedley BD, Stith AY, Nelson AR, editors. Unequal treatment: confronting racial and ethnic disparities in health care. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- Lurie N, Fremont A, Somers SA, et al. The National Health Plan Collaborative to reduce disparities and improve quality. Jt Comm J Qual Patient Saf. 2008 May;34(5):256–65. doi: 10.1016/s1553-7250(08)34032-x. [DOI] [PubMed] [Google Scholar]


