Abstract
Both patient-centered and person-focused care are important, but they are different. In contrast to patient-centered care (at least as described in the current literature with assessments that are visit-based), person-focused care is based on accumulated knowledge of people, which provides the basis for better recognition of health problems and needs over time and facilitates appropriate care for these needs in the context of other needs. That is, it specifically focuses on the whole person. Proposed enhancements and innovations to primary care do not appear to address person-focused care. Tools to assess person-focused care are available and deserve more widespread use in primary care.
Introduction
The benefits to health from advances in medicine in the 20th century have led to a shift away from patients' problems to disease processes, without consideration of the changing contexts in which people live and work and with a demonstrated decline in focus on the person.1 This article explains why the concept of patient-centered care must be supplemented with the concept of person-focused care.
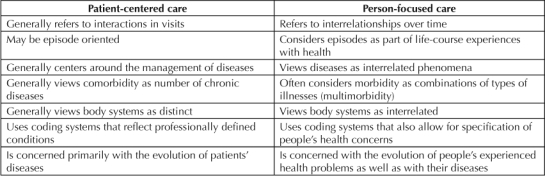
Patient-centered is a term in widespread use; in the US, for example, the recent movement toward reforming primary care is known as the patient-centered medical home. The preponderance of the literature assesses patient-centered care by focusing on visits involving care of (generally chronic) diseases, whereas person-focused care is provided to patients over time independent of care for particular diseases2 (Table 1).
Table 1.
Differences between patient-centered care and person-focused care
The Importance of Recognizing Patients' Health Problems as They See Them
Both patient-centered care and person-focused care require adequate recognition of health problems experienced by people. Care is better when it recognizes what patients' problems are rather than what the diagnosis is.3 The challenge is to do better at recognizing and documenting their problems. Assessing quality of problem recognition requires documenting the problems and how they change in response to what clinicians do.
Diagnoses are professional interpretations of observations and, increasingly, of laboratory values. A few primary care researchers in various countries have been trying at least since the late 1980s to understand the relationship between presenting problems and eventual diagnoses.4 There is still poor understanding of this relationship, and the more it is neglected, the less attention can be focused on problem reduction over time as a legitimate goal of treatment.
Patient-Centered Care
Most studies of patient-centeredness are carried out in settings involving visits.5 Sixteen of the 57 references in a recent review6 have the words communication or interaction in their titles. Prompted by a perceived poor understanding of the term, the authors asserted that patient-centeredness is “determined by the quality of interactions between patients and clinicians” and indicated that they equate patient-centeredness with communication skills, which “are a fundamental component of the approach to care that is characterized by continuous healing relationships, shared understanding, emotional support, trust, patient enablement and activation, and informed choices.”7 In their discussion of physician training, they make it clear that all physicians (not only primary care physicians [PCPs]) need such training.
Visit-based studies of communication and/or interaction between patients and professionals provide most of the evidence for the utility of patient-centeredness. The literature is replete with evidence that communication patterns, both verbal and nonverbal, make a difference, as measured by whether patients are more knowledgeable, more willing to adhere to recommendations, or more “satisfied” with their care. There is no doubt that patterns of communication make a difference, but the extent to which good communication in individual visits is a sufficient strategy to provide the person focus and “continuous healing” that good primary care requires is unknown. It may be that other skills, such as the accumulation of knowledge about people's resilience and vulnerability to threats to their health, are critical as patients move from one health problem to others.
Inherent in a person focus is the notion that attention to patients' problems in the context of their multimorbidity is at least as important as appropriate care for their individual diagnoses.
Person-Focused Care
Studies that focus on the prevention and management of patients' problems over time provide a different and complementary approach to a visit-oriented approach. The literature on primary care-oriented health systems postulates that one of the mechanisms for benefit results from a greater focus on patients as they transition from one health problem to another.8 Primary care is person-focused, not disease-focused, care over time. To be person-focused, it must be accessible, comprehensive (dealing with all problems except those too uncommon to maintain competence), continuous over time, and coordinating when patients have to receive care elsewhere. The essence of person focus implies a time focus rather than a visit focus. It extends beyond communication because much of it relies on knowledge of the patient (and of the patient population) that accrues over time and is not specific to disease-oriented episodes. Physicians and patients working together to reach mutual decisions often require a long-standing relationship.9 Patients are more likely to follow medication regimens if they share their physicians' belief about causes of health outcomes.10 This is unlikely to be the case when visits are with practitioners not well known to patients (and vice versa).
Family physicians' views concerning genetic conditions support the notion that care over time is critical to understanding patients' needs and problems.11 In contrast to judging possible genetic predispositions to rare genetic problems, genetic influences on common illnesses cannot be determined in individual encounters with patients.11
A major failure of primary care, particularly in countries such as the US (where specialty care, including major teaching hospitals, is so dominant), is the great underestimation of the importance of long-term relationships with patients independent of care for specific disease episodes. A specialty dominance dictates that interest is mainly in individual diseases, chosen because they are costly or because they are thought to cause considerable premature mortality. Contrary to conventional wisdom, the main determinant of high costs of care is not the presence of chronic illnesses. Rather, it is the combination of various types of illnesses—that is, multimorbidity—over a period of time (Efrat Shadmi, PhD; Ran Balicer, MD, MPH, PhD; Karen Kinder, MBA, PhD; Chad Abrams, MA; Barbara Starfield, MD, MPH; Jonathan Weiner, DrPH, personal communication 2010).a,12
The importance of a person focus (a nondisease focus) in primary care is highlighted by primary care clinicians' views of their roles. They appreciate the importance of costs and severity of condition (which is difficult to judge in clinical settings, except in the case of acute conditions), but they identify three additional issues: patients' viewpoint of the problem's relative importance, the duration of time over which priorities are set (short or long term), and the level of evidence of benefit in primary care practice.13 Inherent in a person focus is the notion that attention to patients' problems in the context of their multimorbidity (multiple coexisting diseases) is at least as important as appropriate care for their individual diagnoses. Good primary care is not the sum of care for individual diseases.
Will Innovations and Enhancements to Primary Care Improve Problem Recognition and Person Focus?
Although most PCPs (and some specialists) think of their work as person-focused, reimbursement policies and the thrust of medical education toward professionally specified diagnoses do not reward or facilitate attention to patient-defined problems. Whether current enhancements to and innovations in primary care will change the current reality is an open question. Several of these approaches are currently in vogue: guidelines, payment for performance, chronic care management, and, in the US, the patient-centered medical home.
Guidelines
Adhering to guidelines, although often very helpful to physicians, predisposes them to emphasize the management of specific diseases because clinical guidelines focus on diseases. Many common diseases are syndromes—that is, common manifestations of diverse processes set in motion by interacting influences on health.14 The challenges in medical care today are vastly different and much more complex than they were in the mid-20th century because of the marked increase in early diagnoses of diseases and a resulting increase in the simultaneous presence of different diseases. Despite this reality, guideline supporters continue to develop algorithms for management in primary care that are based on an outmoded concept of health problems in populations: single, discrete diseases.
Furthermore, most guidelines that are “evidence-based” have been justified on the basis of evidence on “outcomes” that are almost always proxy outcomes measured by laboratory tests. Clinical trials do not identify the nature and extent of the health problems experienced by people participating in them or the extent to which problems experienced by the participants are resolved by the intervention being tested. As a result, “outcomes” do not involve determinations of whether the intervention caused unintended adverse effects, despite the evidence that adverse events are common.15 Knowledge of these adverse effects is left to voluntary reporting by astute clinicians who look for them. Person focus is not realized when likely adverse events are not systematically recorded and studied.
Guidelines, although generally applied only in primary care (not specialty practice) are not developed with consideration of the nature of primary care settings. In primary care, presenting problems are often not diagnoses but rather symptoms and signs (Jean Karl Soler, MD, MSc, MMCFD; Inge Okkes, MD; Henk Lamberts, MD; personal communication 2010).b Furthermore, the basis for guidelines is evidence from clinical trials, which exclude people with multiple morbidities.16 Problems related to the presence of multimorbidity are difficult to define, describe, and understand. PCPs are in the best position to know what types of problems should receive priority for guideline development, but they are rarely either consulted or in control over the selection of problems for guideline development, the interpretation of the results of trials, or the applicability of their results to their practice.17
Many patients are prone to ignore interventions based on guidelines. For example, discontinuation of prescribed lipid-lowering therapy approaches 50% after one year and 85% after two years.18 Adoption of guidelines, particularly those touted as preventive, fails to be consistent with the overwhelming purpose of medicine, which is the relief of suffering.19
Payment for Performance
Largely spurred by studies that suggest that only about 50% of widely accepted criteria for care of particular diseases are met in actual practice in the US, some health plans in the US and, particularly, the National Health System in the United Kingdom (under the Quality and Outcomes Framework) have introduced payment systems that reward physicians or health plans for adhering to guidelines in the care of their patients. Although payment for performance is, in theory, a laudable approach to encourage adherence to justified processes of care, several aspects of its application are problematic in terms of attention to people's problems.10,20–22
The limited range of quality indicators (mostly to a few common chronic diseases) is not conducive to recognizing the vast range of health problems that confront people. The fact that these are more likely in deprived populations makes most payment-for-performance schemes antithetical to fostering equity in delivering health services.3,23 Concomitantly, the effect is to place clinicians caring for these populations at risk of lower earnings.
Performance measurement is increasingly being extended to interventions that have only a small clinical benefit at the same time that many important aspects of care are being neglected.24 Most quality indicators, which increasingly focus on earlier detection of disease, are not based on priorities regarding effectiveness and, especially, equity, and they have the effect of encouraging physicians to focus on compliance (both in terms of their own actions and in terms of patients' behaviors) rather than on problem resolution.24 Moreover, the assumption that it is justified to pay for performance in the care of people with selected diagnoses is highly questionable as an ethical strategy in the situation where the quality of diagnosis and clinical reasoning are suspect.25 Diagnostic errors are prevalent.26 In primary care especially, many if not most presented problems are not well defined, and the diagnosis remains uncertain. Physicians are not rewarded for recognizing and adequately responding to patients' problems.
The ethical aspects of pay for performance have been addressed by a major US primary care medical society, which proposed an ethics manifesto. It states:
Quality measures should identify excellent comprehensive care. They must recognize successful management of multiple complex chronic conditions, meeting the counseling and communication needs of patients, and providing continuity of care and other attributes of comprehensive care. All measures must sustain and enhance appropriate patient care and the physician-patient relationship.27
Although stopping short of acknowledging the critical importance of recognizing and dealing with people's health problems over time, both in and outside of formal consultations, the wording of this statement makes it clear that high-quality care includes person-focused goals.28
Chronic Care Management
The chronic care model is theoretically consistent with the primary care focus on care over time. It deviates from primary care in its application. Chronic has been interpreted as if it referred to chronic disease. This makes it inherently incompatible with primary care, which is person-focused. All of the implementations of chronic care management are disease-oriented, and they have all of the problems of disease-oriented care.
The literature is replete with evaluations purporting to show benefit, but the vast majority have focused only on one condition (mostly diabetes), and none have evaluated the effectiveness of the intervention on improvement in person-focused morbidity or mortality. Of 944 reviewed articles, only 82 were in primary care settings. Most were from the US.29 Greaves and Campbell concluded that the only demonstrably effective component of these new strategies could be attributed to better follow-up monitoring of patients.30 A review in New Zealand concluded that if anything, a focus on specific chronic illnesses is unlikely to lead to improved health, particularly in populations that have high morbidity burdens overall.31
The US Institute of Medicine report Crossing the Quality Chasm32 urges selecting priority conditions for attention to the quality of care. The list includes cancer, diabetes, emphysema, high cholesterol, HIV and AIDS, hypertension, ischemic heart disease, stroke, and “perhaps” also arthritis, asthma, gallbladder disease, stomach ulcers, back problems, Alzheimer disease, depression, and anxiety disorders. However, it does not include major and common problems such as inadequate nutrition, occupational diseases, osteoporosis, low birth weight and prematurity, repeated acute illnesses, or virtually any childhood disorder (except asthma), and a myriad of other conditions (such as chronic renal failure) that persist over time. Moreover, there is nothing inherently more chronic about “chronic diseases” than is the case for many acute but recurrent conditions such as sinusitis, urinary tract infection, and anemia of unknown origin. The public-health community is notably absent in defining the problems of populations.33
The Patient-Centered Medical Home
The patient-centered medical home, at least as reflected in the requirements for qualification, is heavily focused on care in the context of disease management or communication within specific encounters. There are notable exceptions. Reid and colleagues34,35 and Gilfillan and colleagues36 evaluated interventions consisting of elements such as secure e-mail interactions between patients and health care professionals, disease registries, care planning, self-management strategies, increased outreach to patients, team discussions, performance evaluation, practice teams, population profiling, home health, and designated specialists in settings where there was excellent primary care and included all patients (not just those with selected chronic diseases). Costs were reduced primarily by reducing hospitalizations and Emergency Department visits. In the studies by Reid et al, specialist visits unexpectedly increased, more so in the first year than in the second, suggesting that more patients' problems were recognized at the onset of the program, which then adapted to the increase in diagnosed multimorbidity over time.
The Measurement of Patient-Focused Care
Each of the four enhancements or innovations has features that are inimical to person-focused care. More attention to the concept of person focus over time and efforts to measure it may provide a new dimension to efforts to improve care.
The World Association of Family Physician Organizations developed the International Classification of Primary Care to document what physicians believe to be the problems presented by their patients.4 It has been applied primarily to track the progression of presenting problems to eventual diagnoses in episodes of care and is used in the Netherlands, Malta, Belgium, and Australia to characterize presenting problems. Its potential as a measure of resolution of patients' problems, or to document unexpected adverse events from interventions, is still to be fully realized.
Mushlin and Appel used a conceptually simple method to ascertain the resolution of patients' problems by sending them a postcard after visits.37 Their work does not appear to have received the attention it deserves as a method of determining patient-reported outcomes of care.
Researchers in Quebec explored the conceptual basis of instruments to assess the adequacy of primary care, including orientation to people instead of to specific diseases.38,39 On the basis of previous work,40 they looked for existing instruments that measured “interpersonal continuity” (communications in interactions) and relational continuity (accumulated knowledge of the person) as two distinct aspects of care. As already noted, communication and effective interactions are characteristic of all care; they are not unique to primary care. In contrast, relationship continuity is the essence of primary care; accumulated knowledge is critical to the person-focused interventions over time that are unique to primary care.
Mercer and Howie proposed adoption of a tool (the Consultation Quality Index, version 2) for incorporation into quality improvement, assessment, and payment for performance.41 Although this measure was intended to assess the quality of the consultation, it could be adapted to assess the quality of ongoing care.
Zulman and colleagues constructed a patient-clinician concordance score based on surveys in which patients were asked to rank their most important concerns, and clinicians were asked to rank the most important concerns likely to affect the patient's outcomes.42 Although this study was conducted in conjunction with patient visits, it could be adapted for use as a measure of ongoing relationships.
The Patient Activation Measure is based on the notion that the patient's role in problem definition is important and that people should be empowered to intervene proactively in their care. Studies using this tool43 have shown that more empowered people are less passive in interactions with clinicians, are more likely to be aware of potential adverse effects of treatment, have greater success in navigating health-services systems, have fewer unmet health needs and less delay in initiating care, and are less likely to lack a regular source of care, even after controlling for low socioeconomic status and poor perceived health status. They are also likely to have more responsive physicians—a major goal in achieving person-focused care.
The importance of person focus is also recognized in the Primary Care Assessment Tool (www.jhsph.edu/pcpc/pca_tools.html) a suite of comparable instruments for use in population health surveys, patient surveys of their experiences with primary care, clinician surveys of reports of primary care functions, and surveys of managers of health facilities. Examples of person-oriented questions asked in the population and patient surveys include the following:
If you have a question, can you call and talk to the doctor or nurse who knows you best?
Does your PCP know you very well as a person, rather than as someone with a medical problem?
Does your PCP know what problems are most important to you?
Interactions between patients and clinicians are changing.44 “Patient portals,” “virtual visits,” “asynchronous consulting,” and “remote monitoring” are becoming increasingly common. They will be useful only to the extent that people are confident in their clinicians' accumulated knowledge of their problems. Yee argued that the functioning of new primary care organizations must “include innovative forms of interactions that do not depend on traditional office visits.”45 Klinkman and van Weel urged thinking “far beyond the encounter as the unit of health care delivery” by means of standards and robust technology to move information.46 A World Health Organization report proposed a vast expansion of telemedicine to bridge the distance between people and health care.47 Internet-based technologies provide a new way of responding to patients, as experience in Kaiser Permanente is showing.48 Visit-based communications and the opportunity for conventional communication strategies will decline. Person-focused care over time, not just patient-centered interactions, requires a new strategy to ensure responsiveness to patient's problems as they experience them, not only as professionals define them.
… relationship continuity is the essence of primary care; accumulated knowledge is critical to the person-focused interventions over time that are unique to primary care.
Disclosure Statement
The author(s) have no conflicts of interest to disclose.
Acknowledgments
Katharine O'Moore-Klopf, ELS, of KOK Edit provided editorial assistance.
Footnotes
a Shadmi, Assistant Professor, University of Haifa, Israel; Balicer, Director, Clalit Research Institute, Israel; Kinder, Associate Faculty, Johns Hopkins Bloomberg School of Public Health; Abrams, Software Engineer, Johns Hopkins Bloomberg School of Public Health; Starfield, University Distinguished Professor, Johns Hopkins Bloomberg School of Public Health; Weiner, Professor, Johns Hopkins Bloomberg School of Public Health
b Soler, Executive Director, Research Mediterranean Institute of Primary Care, Malta; Okkes, Professor, University of Amsterdam; Lamberts, Professor, University of Amsterdam
References
- Haslam DA. Who cares? The James Mackenzie Lecture 2006. Br J Gen Pract. 2007 Dec;57(545):987–93. doi: 10.3399/096016407782604884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nasmith L, Ballem P, Baxter R, et al. Transforming care for Canadians with chronic health conditions: put people first, expect the best, manage for results [monograph on the Internet] Ottawa, Ontario, Canada: Canadian Academy of Health Sciences; 2010. [cited 2011 Jan 24]. Available from: www.cahsacss.ca/e/pdfs/cdm%20final%20English.pdf. [Google Scholar]
- Starfield B. Primary care and equity in health: the importance to effectiveness and equity of responsiveness to peoples' needs. Humanity and Society. 2009;33:56–73. [Google Scholar]
- Soler JK, Okkes I, Wood M, Lamberts H. The coming of age of ICPC: celebrating the 21st birthday of the International Classification of Primary Care. Fam Pract. 2008 Aug;25(4):312–7. doi: 10.1093/fampra/cmn028. [DOI] [PubMed] [Google Scholar]
- Mead N, Bower P, Hann M. The impact of general practitioners' patient-centredness on patients' post-consultation satisfaction and enablement. Soc Sci Med. 2002 Jul;55(2):283–99. doi: 10.1016/s0277-9536(01)00171-x. [DOI] [PubMed] [Google Scholar]
- Epstein RM, Fiscella K, Lesser CS, Stange KC. Why the nation needs a policy push on patient-centered health care. Health Aff (Millwood) 2010 Aug;29(8):1489–95. doi: 10.1377/hlthaff.2009.0888. [DOI] [PubMed] [Google Scholar]
- Levinson W, Lesser CS, Epstein RM. Developing physician communication skills for patient-centered care. Health Aff (Millwood) 2010 Jul;29(7):1310–8. doi: 10.1377/hlthaff.2009.0450. [DOI] [PubMed] [Google Scholar]
- Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457–502. doi: 10.1111/j.1468-0009.2005.00409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kon AA. The shared decision-making continuum. JAMA. 2010 Aug 25;304(8):903–4. doi: 10.1001/jama.2010.1208. [DOI] [PubMed] [Google Scholar]
- Christensen AJ, Howren MB, Hillis SL, et al. Patient and physician beliefs about control over health: association of symmetrical beliefs with medication regimen adherence. J Gen Intern Med. 2010 May;25(5):397–402. doi: 10.1007/s11606-010-1249-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathers J, Greenfield S, Metcalfe A, Cole T, Flanagan S, Wilson S. Family history in primary care: understanding GPs' resistance to clinical genetics—qualitative study. Br J Gen Pract. 2010 May;60(574):e221–30. doi: 10.3399/bjgp10X501868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broemeling AM, Watson D, Black C. Chronic conditions and comorbidity among residents of British Columbia [monograph on the Internet] Vancouver, British Columbia, Canada: University of British Columbia: Centre for Health Services and Policy Research; 2005 Feb. [cited 2011 Mar 22]. Available from: www.chspr.ubc.ca/files/publications/2005/chspr05-08.pdf. [Google Scholar]
- Arvidsson E, André M, Borgquist L, Carlsson P. Priority setting in primary health care— dilemmas and opportunities: a focus group study. BMC Fam Pract. 2010 Sep 23;11:71. doi: 10.1186/1471-2296-11-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starfield B. Appendix A: Chronic illness and primary care; 2009. In: Nasmith L, Ballem P, Baxter R, et al., editors. Transforming care for Canadians with chronic health conditions: put people first, expect the best, manage for results—appendices [monograph on the Internet] Ottawa, Ontario, Canada: Canadian Academy of Health Sciences; 2010. [cited 2011 Jan 24]. Available from: www.cahsacss.ca/e/pdfs/cdm%20final%20Appendices.pdf. [Google Scholar]
- Gérvas J, Starfield B, Heath I. Is clinical prevention better than cure? Lancet. 2008 Dec 6;372(9654):1997–9. doi: 10.1016/S0140-6736(08)61843-7. [DOI] [PubMed] [Google Scholar]
- Boyd CM, Darer J, Boult C, Fried LP, Boult L, Wu AW. Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: implications for pay for performance. JAMA. 2005 Aug 10;294(6):716–24. doi: 10.1001/jama.294.6.716. [DOI] [PubMed] [Google Scholar]
- Loxterkamp D, Kazal LA., Jr. Changing horses midstream: the promise and prudence of practice redesign. Ann Fam Med. 2008 Mar–Apr;6(2):167–70. doi: 10.1370/afm.822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaRosa JH, LaRosa JC. Enhancing drug compliance in lipid-lowering treatment. Arch Fam Med. 2000 Nov–Dec;9(10):1169–75. doi: 10.1001/archfami.9.10.1169. [DOI] [PubMed] [Google Scholar]
- Gérvas J, Pérez Fernández M. Uso apropiado de los metodos diagnosticos en la decision clinica. [In Portuguese] Actualizacion en Medicina de Familia. 2006;2:357–65. [Google Scholar]
- Garber AM. Evidence-based guidelines as a foundation for performance incentives. Health Aff (Millwood) 2005 Jan–Feb;24(1):174–9. doi: 10.1377/hlthaff.24.1.174. [DOI] [PubMed] [Google Scholar]
- Kravitz RL, Duan N, Braslow J. Evidence-based medicine, heterogeneity of treatment effects, and the trouble with averages. Milbank Q. 2004;82(4):661–87. doi: 10.1111/j.0887-378X.2004.00327.x. Erratum in: Milbank Q 2006;84(4):759–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heath I, Hippisley-Cox J, Smeeth L. Measuring performance and missing the point? BMJ. 2007 Nov 24;335(7629):1075–6. doi: 10.1136/bmj.39377.387373.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starfield B. Quality and outcomes framework: patient-centred? Lancet. 2008 Aug 30;372(9640):692–4. doi: 10.1016/S0140-6736(08)61124-1. [DOI] [PubMed] [Google Scholar]
- Werner RM, Asch DA. Clinical concerns about clinical performance measurement. Ann Fam Med. 2007 Mar–Apr;5(2):159–63. doi: 10.1370/afm.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wachter RM. Why diagnostic errors don't get any respect— and what can be done about them. Health Aff (Millwood) 2010 Sep;29(9):1605–10. doi: 10.1377/hlthaff.2009.0513. [DOI] [PubMed] [Google Scholar]
- Holmboe ES, Lipner R, Greiner A. Assessing quality of care: knowledge matters. JAMA. 2008 Jan 23;299(3):338–40. doi: 10.1001/jama.299.3.338. [DOI] [PubMed] [Google Scholar]
- Snyder L, Neubauer RL, American College of Physicians Ethics, Professionalism & Human Rights Committee Pay-for-performance principles that promote patient-centered care: an ethics manifesto. Ann Intern Med. 2007 Dec 4;147(11):792–4. doi: 10.7326/0003-4819-147-11-200712040-00011. [DOI] [PubMed] [Google Scholar]
- Kindig DA. A pay-for-population health performance system. JAMA. 2006 Dec 6;296(21):2611–3. doi: 10.1001/jama.296.21.2611. [DOI] [PubMed] [Google Scholar]
- Coleman K, Austin BT, Brach C, Wagner EH. Evidence on the Chronic Care Model in the new millennium. Health Aff (Millwood) 2009 Jan–Feb;28(1):75–85. doi: 10.1377/hlthaff.28.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greaves CJ, Campbell JL. Supporting self-care in general practice. Br J Gen Pract. 2007 Oct;57(543):814–21. [PMC free article] [PubMed] [Google Scholar]
- CBG Health Research Limited. Review of the implementation of CARE PLUS [monograph on the Internet] Wellington, New Zealand: Ministry of Health, New Zealand; 2006. [cited 2009 Feb 8]. Available from: www.moh.govt.nz/moh.nsf/pagesmh/5567/$File/review-implementation-care-plus.pdf. [Google Scholar]
- Institute of Medicine Committee on Quality of Health Care in America. Crossing the quality chasm: a new health system for the 21st century. Washington, DC: National Academies Press; 2001. [Google Scholar]
- Raphael D. Shaping public policy and population health in the United States: why is the public health community missing in action? Int J Health Serv. 2008;38(1):63–94. doi: 10.2190/HS.38.1.d. [DOI] [PubMed] [Google Scholar]
- Reid RJ, Fishman PA, Yu O, et al. Patient-centered medical home demonstration: a prospective, quasi-experimental, before and after evaluation. Am J Manag Care. 2009 Sep 1;15(9):e71–87. [PubMed] [Google Scholar]
- Reid RJ, Coleman K, Johnson EA, et al. The group health medical home at year two: cost savings, higher patient satisfaction, and less burnout for providers. Health Aff (Millwood) 2010 May;29(5):835–43. doi: 10.1377/hlthaff.2010.0158. [DOI] [PubMed] [Google Scholar]
- Gilfillan RJ, Tomcavage J, Rosenthal MB, et al. Value and the medical home: effects of transformed primary care. Am J Manag Care. 2010 Aug;16(8):607–14. [PubMed] [Google Scholar]
- Mushlin AI, Appel FA. Testing an outcome-based quality assurance strategy in primary care. Med Care. 1980 May;18(5 Suppl):1–100. [PubMed] [Google Scholar]
- Santor F, Haggerty J, Beaulieu C, et al. Measuring interpersonal communication from the consumer perspective: comparison of primary healthcare evaluation instruments. Healthc Policy. 2011;6(4) [In press.] [PMC free article] [PubMed] [Google Scholar]
- Burge F, Haggerty J, Pineault R, et al. Measuring relationship continuity from the consumer perspective: comparison of primary healthcare evaluation instruments. Healthc Policy. 2011;6(4) [In press.] [PMC free article] [PubMed] [Google Scholar]
- Haggerty JL, Reid RJ, Freeman GK, Starfield BH, Adair CE, McKendry R. Continuity of care: a multidisciplinary review. BMJ. 2003 Nov 22;327(7425):1219–21. doi: 10.1136/bmj.327.7425.1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mercer SW, Howie JG. CQI-2—a new measure of holistic interpersonal care in primary care consultations. Br J Gen Pract. 2006 Apr;56(525):262–8. [PMC free article] [PubMed] [Google Scholar]
- Zulman DM, Kerr EA, Hofer TP, Heisler M, Zikmund-Fisher BJ. Patient-provider concordance in the prioritization of health conditions among hypertensive diabetes patients. J Gen Intern Med. 2010 May;25(5):408–14. doi: 10.1007/s11606-009-1232-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hibbard JH, Cunningham PJ. How engaged are consumers in their health and health care, and why does it matter. Research brief no. 8 [monograph on the Internet] Washington, DC: Center for Studying Health System Change; 2008. [cited 2008 Oct 19]. Available from: www.hschange.org/CONTENT/1019/ [PubMed] [Google Scholar]
- Dixon RF. Enhancing primary care through online communication. Health Aff (Millwood) 2010 Jul;29(7):1364–9. doi: 10.1377/hlthaff.2010.0110. [DOI] [PubMed] [Google Scholar]
- Yee HF., Jr. The patient-centered medical home neighbor: a subspecialty physician' s view. Ann Intern Med. 2011 Jan 4;154(1):63–4. doi: 10.7326/0003-4819-154-1-201101040-00011. [DOI] [PubMed] [Google Scholar]
- Klinkman M, van Weel C. Prospects for person-centred diagnosis in general medicine. J Eval Clin Pract. 2011 Apr;17(2):365–70. doi: 10.1111/j.1365-2753.2010.01582.x. [DOI] [PubMed] [Google Scholar]
- Telemedicine: opportunities and developments in member states. Report on the second global survey on ehealth: Global Observatory for eHealth series, vol. 2 [monograph on the Internet] Geneva, Switzerland: World Health Organization; 2010. [cited 2011 Jan 25]. Available from: www.who.int/goe/publications/goe_telemedicine_2010.pdf. [Google Scholar]
- Zhou YY, Kanter MH, Wang JJ, Garrido T. Improved quality at Kaiser Permanente through e-mail between physicians and patients. Health Aff (Millwood) 2010 Jul;29(7):1370–5. doi: 10.1377/hlthaff.2010.0048. [DOI] [PubMed] [Google Scholar]


