Abstract
Background
Computerized, tailored interventions have the potential to be a cost-effective means to assist a wide variety of individuals with behavior change. To examine the effect of computerized tailored physical activity reports on primary care patients' physical activity at six months.
Design
Two-group randomized clinical trial with primary care physicians as the unit of randomization. Patients were placed in the intervention (n=187) or control group (n=207) based on their physician's assignment.
Setting/Participants
Primary care physicians (n=22) and their adult patients (n=394) from Philadelphia, PA. The study and analyses were conducted from 2004-2010.
Intervention
The intervention group completed physical activity surveys at baseline, one, three, and six months. Based on their responses, participants received four feedback reports at each time point. The reports aimed to motivate participants to increase physical activity, personalized to the participant's needs; they also included an activity prescription. The control group received identical procedures except they received general reports on preventive screening based on their responses to preventive screening questions.
Main outcome measure
Minutes of physical activity measured by the 7-Day Physical Activity Recall interview at six months.
Results
Participants were 69% female, 59% African American, and had diverse educational and income levels; the retention rate was 89.6%. After adjusting for baseline levels of activity and gender, the intervention group increased their total minutes of physical activity by a mean of 133 minutes, while the control group had a mean increase of 99 minutes (p=0.39).
Conclusions
Although we saw an increase in physical activity within both groups, computerized tailored physical activity reports did not significantly increase physical activity levels beyond control among ethnically and socioeconomically diverse adults in primary care.
Keywords: primary care issues, physical activity, behavioral medicine, randomized clinical trial
Introduction
Patients see their primary care providers an average of four times per year,1 and the majority of the population in the US, UK, and Australia believe that physical activity promotion should be a part of routine medical care.2-5 Thus, successful primary care interventions to promote physical activity behavior could have a significant public health impact. Physical activity counseling by physicians may prime patients, making them more open to considering health behavior change.6;7 Yet, despite the potentially positive benefits of counseling, physicians confront many well-documented barriers when counseling patients.8-10 As a result, efforts to assist physicians in behavioral health counseling have had mixed results.11 While some studies show that clinician counseling increases patients' physical activity12-17 other studies18-22 have not demonstrated significant results.
Given the challenges of clinician counseling to promote physical activity, other communication technologies (e.g., telephone, the Internet) which target primary care populations and tailor messages to them to promote physical activity may be promising. A review of telephone counseling to promote physical activity counseling23 found strong support for their efficacy in supporting behavior change. There is also growing support for other novel electronic technologies such as short-message service texting interventions which appear to have some short-term benefit on health behavior change.24 However, the majority of these interventions focused on chronic disease management, but not health behaviors such as physical activity.
This paper reports on the use of a specific communication technology-- computerized tailored reports--as a potentially effective and important strategy to promote physical activity among ethnically diverse primary care patients. Previous studies have shown that computerized tailored reports given to patients may help patients recall personalized advice to improve their health,25 remain abstinent from tobacco,26 enhance physical activity motivation and behavior,27;28 and improve self-management skills.29 While a growing body of studies supports the use of computerized interventions as a means to provide personalized, tailored information,30;31 less is known about the role of such technology as an interactive strategy to facilitate change, especially for ethnically diverse primary care populations.
The primary objective of this study was to determine whether providing computerized tailored reports to adult primary care patients increased participation in regular, moderate-to-vigorous intensity physical activity. We hypothesized that the computerized tailored reports would increase physical activity among adults compared to an attention/contact control group. Our secondary objectives were to examine whether the computerized tailored reports would increase motivation, use of strategies and techniques for change, self-efficacy, and discussions about physical activity with primary care clinicians.
Methods
Design
The Computerized Health Improvement Project (CHIP) was a randomized controlled trial conducted in 2004-2007 with two groups: exercise (intervention) and prevention (control).
Setting
Patients were recruited through a total of 22 primary care providers (21 attending physicians and one nurse practitioner) from a family medicine practice affiliated with Jefferson Medical College in Philadelphia, Pennsylvania. Thomas Jefferson University Institutional Review Board approved the study protocol.
Randomization
Randomization was at the level of the physician; each physician was assigned to one of the study conditions by a statistician using random number generation. Thus, patients were assigned to either the intervention or control group based on their physician's randomized assignment. Cluster randomization was used to minimize the risk of cross-contamination between the two groups and to maximize consistency in physician behavior by having patients with the same study assignment.
Recruitment, Enrollment
Each provider initially reviewed a list of their current patients and excluded individuals based on the exclusion criteria. Research staff mailed recruitment letters to patients requesting them to call if interested. Interested patients were screened for eligibility. Adults were excluded if they were physically active (>150 minutes/week), participating in another research study, pregnant, and/or had medical contraindications to exercise. Participants were required to read and write in English, reside in the Philadelphia area, and have a primary care provider participating in the study.
Eligible patients then had a baseline visit to provide written informed consent and to complete baseline survey measures (described below). Next, treadmill testing, using the modified Bruce protocol, was used to verify participant eligibility.32 Although guidelines for moderate intensity exercise do not require asymptomatic individuals to have a medical exam and clinical exercise testing,32 physicians may recommend treadmill testing for patients who plan to begin non-medically supervised vigorous activities. Participants with abnormal treadmill test results suggesting cardiovascular disease were excluded.
Intervention (Exercise) Group
Participants in the intervention group completed physical activity surveys mailed to them at baseline, 1, 3, and 6 months. The surveys asked about current physical activity habits, self-efficacy, decision-making about physical activity, health status, and chronic conditions.
After completing and returning each physical activity survey, research staff entered the participant's survey responses into a computer program. Then, a report was created and mailed to the participant, designed to motivate them to increase physical activity personalized to the participant's needs. The reports were based on both psychosocial measure (stage of change, processes of change, self-efficacy, and pros and cons) and the individual's reported amount of physical activity. We adapted the tailored messages from previous studies by Marcus and colleagues.33-36 Each message contained graphics, as images can be helpful for improving health messages for some audiences.37 All reports consisted of validated variables extracted from the physical activity survey: stage of change,36 decisional balance, cognitive and behavioral processes of change, and self-efficacy.36 The tailored reports provided congratulatory messages for participants who obtained the recommended amounts of physical activity, and tips on how to increase physical activity for those not meeting the recommended guidelines. Each tailored report also contained questions for patients to ask providers about activity levels and potential health benefits from additional physical activity. Participants received an activity prescription with instructions to bring the prescription to their next visit with their physician. The prescription contained areas in which physicians could prescribe a type of activity, intensity (moderate/hard), frequency, and duration.
Participants received a total of four tailored ipsative feedback reports, based on their responses to the preceding physical activity survey in the manner described above. Specifically, participants received feedback about how their currently reported physical activity compared to their previously reported amount, and how their activity compared to the recommended guidelines.
Control (prevention) group
Participants in the control group followed the same schedule and protocol. However, these individuals answered questions, using validated measures from the Behavioral Risk Factor Surveillance System (BRFSS), regarding preventive tests that they may have had (e.g., Pap testing, influenza vaccination). The feedback reports received by control participants contained information on recommended preventive tests and questions for patients to ask their provider about the suitability of screening tests for them.38
Incentives
Participants were paid up to $140 for their participation: $50 for completing the baseline visit, $10 for completing each of the three physical activity surveys, and $60 for completing the six-month visit. Participating primary care providers did not receive monetary compensation.
Measures
The main outcome measure was the 7-Day Physical Activity Recall (7-Day PAR), an interviewer-administered self-report physical activity measure of minutes spent in moderate and vigorous intensity leisure and non-leisure activities over a participant's preceding seven days.39;40 Validity and reliability of the 7-day PAR have been demonstrated.41-43 Trained staff administered the 7-Day PAR to all participants at baseline and six months.
Secondary measures included constructs from the transtheoretical model44 (motivation and behavior change) and intervention “dose” delivered and received by all participants. The theoretical constructs we examined were behavioral and cognitive processes (strategies and techniques for change), decisional balance, and self-efficacy. Behavioral and cognitive processes were assessed by asking participants to rate their responses to 24 statements on a five-point Likert scale (1-never, 2-seldom, 3-occasionally, 4-often, 5-repeatedly) such as “I tell myself I am able to be physically active if I want to”, “I make commitments to be physically active”, and “When I'm feeling tense, I find exercise a great way to relieve my worries.” We assessed self-efficacy by asking participants to rate their responses on a 5-point Likert scale (1-not at all confident, 2-slightly confident, 3-moderately confident, 4-very confident, 5-extremely confident) to statements such as, “How confident are you that you could exercise when you are tired?… In a bad mood?…When you feel you don't have time?” Decisional balance was measured by asking participants to rate their responses to six items on a 5-point Likert scale (1-not at all important, 2-slightly important, 3-moderately important, 4-very important, 5-extremely important) to statements such as, “Regular exercise would help me relieve tension,” “Regular exercise would take too much of my time”, and “I would feel more confident if I exercised regularly.” Finally, we measured intervention “dose” by the number of reports (of four total) participants received, read, showed, and discussed with their primary care provider. We measured participant health information using questions adapted from the BRFSS.45
Sample size
Statistical power was calculated a priori, taking into account the cluster randomization scheme, based on the absolute difference of minutes to be detected between groups. A target sample size of 330 patients (15 patients per each of 11 primary care providers per group) had 90% power to detect the postulated end-of-follow-up difference of 60 minutes of at least moderate activity per week, assuming a 5% type I error rate, between-physician variability that would not be large enough to result in an intraclass correlation coefficient exceeding 0.10, and a retention rate of 80%.
Statistical analysis
All analyses are based on a significance level of 0.05. Two sample t-tests for continuous variables and chi-square tests for categorical variables were used to evaluate the success of the randomization in balancing baseline covariates between intervention and control groups. Continuous outcomes (e.g., physical activity minutes per week) were converted to change scores by subtracting baseline scores from six month scores. We checked the distributions of the change scores using graphical techniques and saw no sizeable deviations from normality that would require transformation of the outcomes. All continuous primary and secondary outcomes were analyzed using analysis of covariance models, which adjusted the treatment effects for baseline levels and sex, which showed a between group difference at baseline. Physician was included as a random effect in modeling continuous outcomes to account for the cluster randomization scheme. When total activity minutes were analyzed as a dichotomous outcome, generalized estimating equations with a logit link were used to account for the cluster randomization scheme. As a secondary analysis, we used multiple imputation (m=10) based on Markov chain Monte Carlo methods46 so that all participants could be included in the analysis, to check the sensitivity of findings from the primary analysis which excluded participants missing the six month assessment. Subsequent analyses included adding interactions between intervention and sex or race and stratifying by features of the dependent variable (physical activity), i.e. moderate versus vigorous and nonleisure/occupational versus leisure.
Results
Participants
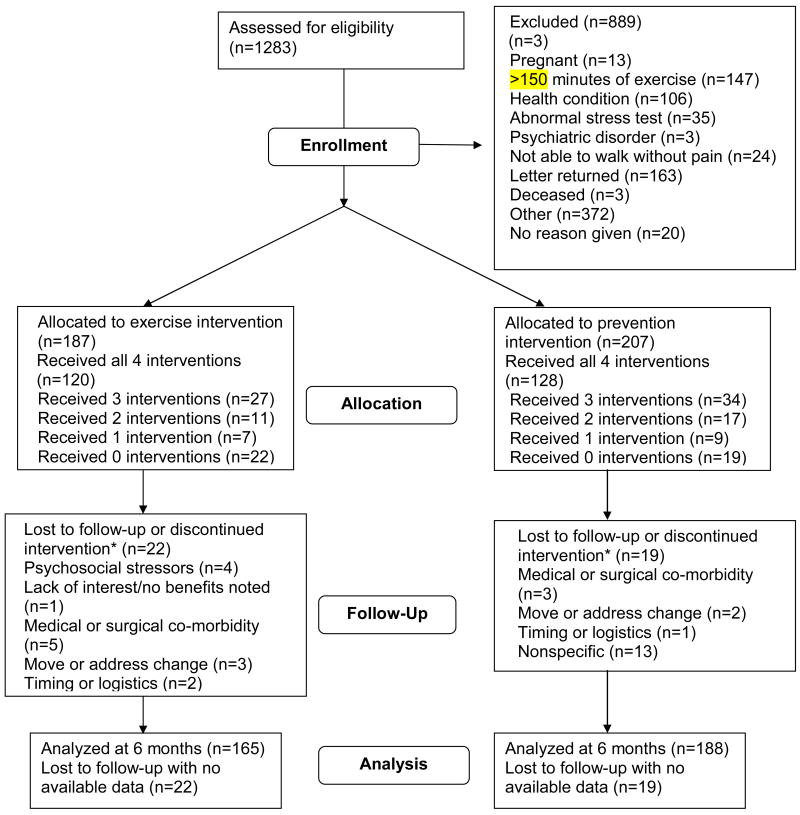
Potential participants (n=1283) completed a telephone screening interview to determine eligibility (Figure 1). Of these, 889 were ineligible, most commonly because of high baseline levels of exercise (n=147) and pre-existing health conditions (n=106). Others declined for nonspecific reasons (n=372, no further details available). The remaining 394 participants were enrolled and randomized to the intervention (n=187) and control (n=207) groups. Of the 394 participants, there were 41 drop-outs (22 intervention, and 19 control group) overall, with no differential drop-out between groups. The majority of drop-outs (26) were for nonspecific reasons including loss to follow-up; medical or psychosocial reasons given for other drop-outs are shown in Figure 1.
Figure 1. Flow diagram of participants in study.
*Participants were allowed to report multiple reasons for attrition.
Participant demographic characteristics
Participants were 69% female and 31% male. The intervention group had more females (p<0.01), African Americans (p<0.01), and was younger (mean age 44 years compared to 48 years, p<0.01) compared to the control group. Participants in the control group were more likely to be married. Both intervention and control groups were similar in terms of distribution of educational attainment, insurance coverage, and employment characteristics.
Participant health status characteristics
Control group participants were more likely to have high blood pressure and high cholesterol than the intervention participants. As Table 1 shows, participants in both groups had relatively high motivation to become more active and a majority in both groups reported trying to lose weight. Other health characteristics were similar between groups.
Table 1. Participant demographic characteristics*.
| Variable | Category/Units | Total | Exercise | Prevention | P-value |
|---|---|---|---|---|---|
| Sex | Male | 31 | 20 | 42 | <0.01 |
| Female | 69 | 80 | 58 | ||
| Age * | Years | 46.4±11.4 | 44.1±11.2 | 48.4±11.1 | <0.01 |
| Race | African American | 59 | 68 | 50 | <0.01 |
| Caucasian | 36 | 27 | 44 | ||
| Other | 5 | 5 | 6 | ||
| Insurance coverage | Yes | 94 | 93 | 95 | 0.38 |
| No | 6 | 7 | 5 | ||
| Education | Some high school | 4 | 4 | 3 | 0.48 |
| High school grad | 16 | 17 | 16 | ||
| Some college | 32 | 34 | 29 | ||
| College grad | 48 | 45 | 52 | ||
| Employment | Employed for wages | 79 | 78 | 81 | 0.49 |
| Unable to work | 21 | 22 | 19 | ||
| Marital status | Married or living as married | 46 | 39 | 53 | 0.03 |
| Divorced | 13 | 17 | 9 | ||
| Widowed or separated | 11 | 12 | 10 | ||
| Never married | 30 | 32 | 28 | ||
| Income | < $25,000 | 15 | 17 | 13 | 0.35 |
| $25,000-<$35,000 | 14 | 15 | 13 | ||
| $35,000-<$50,000 | 22 | 25 | 20 | ||
| $50,000-<$75,000 | 16 | 16 | 16 | ||
| >=$75000 | 27 | 22 | 32 | ||
| I'm not sure | 6 | 5 | 6 | ||
| BMI * | kg/m2 | 30.4±7.2 | 30.7±6.9 | 30.0±7.5 | 0.34 |
| Attempting to Lose Weight | Yes | 66 | 68 | 65 | 0.60 |
| No | 34 | 33 | 35 | ||
| Stage of Change for Activity | Precontemplation | 13 | 9 | 17 | 0.08 |
| Contemplation | 47 | 51 | 42 | ||
| Preparation | 9 | 9 | 9 | ||
| Action | 31 | 31 | 32 |
mean ± standard deviation; all statistics are percentages otherwise
Primary outcome variable: 7-Day PAR
The follow-up PAR interview was completed by 89.6% of the participants at six months. Results indicated no significant differences between the intervention and control groups on the changes in minutes from baseline to six months. At six months, the intervention group increased their total minutes of physical activity by 133 minutes, while those in the control group had a mean increase of 99 minutes of physical activity (results not significant (p=0.39), even when adjusted for baseline and gender). There were no significant differences between groups when the changes in minutes were separated by total, moderate, or vigorous physical activity. Most physical activity minutes were reported as moderate-intensity. The findings did not qualitatively change in the secondary analysis utilizing multiple imputation. Dichotomizing total activity minutes at 6 months into >= 150 minutes or < 150 minutes, we found the odds of exercising the recommended amount to be marginally higher for the intervention group [odds ratio (confidence interval) = 1.41 (0.95, 2.08); p=0.09], adjusting for gender and baseline total activity minutes.
Exploratory analyses
We explored whether the intervention was differentially effective for subgroups according to gender, race, and baseline level of physical activity, which we divided in to quartiles from least active to most active. We did not observe a differential effect of the intervention between women and men (p=0.12), or white and black participants (p=0.54). We also did not find any differences between groups according to gender and race for moderate, vigorous, total, leisure, or non-leisure physical activity.
We constructed a model for change in total minutes of physical activity with the following predictors: baseline quartile, intervention, and the interaction between baseline quartile and intervention. This model first addressed whether the intervention effect depended upon baseline quartile by examining the interaction term, which was not significant (p=0.43). The main effect of baseline quartile, which addresses if baseline quartile is related to change in total minutes of physical activity, was highly significant (p < 0.0001). Also, we calculated the model-based means for each study group by baseline quartile. We found that the lower quartiles showed larger changes than the higher quartiles; however there was not a clear dose-response relationship, as quartile two actually had the largest increase in physical activity.
We performed additional analyses accounting for the imbalance in chronic diseases between intervention and control groups. Results showed that the chronic diseases had little impact on the estimate of the intervention effect. With chronic diseases included in the model, the difference in groups was 16.14 (p=0.68). Without chronic diseases included in the model, the difference was 15.67 (p=0.68).
Influence of intervention on theoretical constructs
We examined whether various psychosocial constructs important for physical activity behavior change, such as behavioral and cognitive processes, self-efficacy, and decisional balance, changed from baseline to six months. We adjusted for sex and baseline physical activity minutes statistically.
For behavioral processes of change, the mean processes of change score increased 0.53 on the Likert scale for intervention participants and 0.17 for control participants, representing improvements in overcoming barriers and consideration of benefits to exercise; the between-group difference adjusted for gender and baseline physical activity minutes was significant (p<0.01). For cognitive processes of change, the mean processes of change score increased 0.36 for intervention participants and 0.20 for control participants on the Likert scale, representing improvements in overcoming barriers and consideration of benefits to exercise; the between-group difference adjusted for gender and baseline was significant (p=0.03). For self-efficacy, the intervention group's score increased slightly more than the prevention group; however, these changes were not significant (p=0.10). The mean decisional balance score (a summary score weighing pros and cons in favor of deciding to exercise) increased very modestly for both groups and was not significant (p=0.71).
Adherence to intervention
We examined the frequency and extent to which participants received, read, and discussed the intervention materials—specifically, their tailored feedback reports—with their primary care physician. The intervention was designed to encourage patients to discuss physical activity with their primary care physician, though the intervention was mailed to their home and not provided in the office. The majority (73%) received the intervention materials, with no difference between groups (p=0.34). The vast majority in both intervention and control groups (87.2% and 89.3%, respectively, p=0.55) reported reading all or most of the materials. The control group was more likely to show (p<0.01) and discuss (p<0.01) the feedback document with their provider compared to intervention group participants. We also found that the likelihood of a participant discussing their reports with their physician increased as the baseline quartile of physical activity increased (i.e., more active participants were more likely to discuss their reports than less active participants). However, the size of the association (Kendall's Tau-b=0.13) was modest. Other more specific components of exercise counseling between participant and primary care physician-such as specifying the frequency, type, duration, or intensity of exercise, and putting the plan in writing—occurred infrequently and did not differ between groups.
Discussion
The primary goal of this study was to test the effect of tailored, computerized physical activity reports on patients' physical activity at six months. This study used an innovative computer program adapted from previous successful work.47 Our study targeted patients directly as a strategy to attempt to overcome patient-clinician counseling barriers to physical activity promotion in primary care visits.
Contrary to our hypotheses, we did not find significant changes in physical activity between intervention and control groups, contrasting with studies that have shown improvements.47-50 There are several possible reasons for the lack of effect. It is possible that participants under-reported physical activity on the initial telephone screen, over-reported on the baseline assessment, and/or actually changed their activity level from screening to baseline assessment. Other studies (Jumpstart47, Project STRIDE48;49) excluded those with greater than 90 minutes per week on the baseline assessment, to maximize enrollment of sedentary individuals. Our study chose a less restrictive exclusion criterion of 150 minutes per week in an effort to access a broader population and be consistent with recent evidence-based guidelines recommending 150 minutes per week of physical activity.51;52 Unfortunately, the higher cutoff resulted in more above-threshold individuals enrolled than anticipated. Though we instructed participants not to increase their activity between their initial screen and baseline assessment, many participants did so despite our efforts to use procedures similar to other studies' protocols.47-49 With more sedentary individuals, we might have detected a larger intervention effect.
Given the relatively active participants in this study, we were surprised how markedly participants increased their physical activity (133 minutes in the intervention group and 99 minutes in the control group). We considered whether participants were unwittingly prompted to change activity with questions from the baseline assessment or other unintentional physical activity prompts in study procedures. We attempted to embed physical activity questions in other general health questions to reduce their emphasis. However, it is possible that answering multiple surveys during the study period led to reactivity that enhanced physical activity. Participants, through informed consent and enrollment, were likely aware that the purpose of the study related to preventive health and was endorsed by their physician. It is possible that participants wanted to “please their doctor” during the study period by increasing their physical activity. Given the high percentage of participants with obesity and other chronic diseases amenable to physical activity who expressed motivation to change, participation in the study itself may have been motivating for both groups to change their activity. Clinical trial participants often increase their physical activity more than what would likely be observed in “real world” populations, especially for short-term studies (6 months or less).15;16;21 Previous studies have also shown control group participants typically increase their physical activity to some degree along with intervention groups.15;20 22;53;30;31
While our participants reported high rates of receiving and reading the computerized tailored reports, the frequency of discussing them with their physician was low overall, and lowest for the participants who were least active. The control group was significantly more likely to show and discuss them with their primary care provider than the intervention group. It is possible that the control group participants, having received information on specific preventive screening tests, found this information easier or more routine to bring up with their physician. Though these reports were not physical activity specific, perhaps the other preventive health information increased health promotion discussions that contributed to the change in the control group.
The present study, by design, had limited physician involvement and expectation to change their clinical counseling or provide study-specific activities. Minimizing clinician burden is advantageous to more feasibly recruit and retain a robust sample of physicians and their patients, given real-world constraints. Consequently, we were able to assess whether patients respond to direct targeting and whether direct targeting activates patients to discuss exercise with their physician. However, because of the low levels of discussion of the intervention materials with the physicians, our study cannot address the issue of whether physician counseling is effective. Other work54 examining tailored physician advice found no significant difference in patients' physical activity, perhaps because physicians did not uniformly distribute the written materials or discuss physical activity as intended by the study protocol. Similarly, our intervention may have been less effective due to less frequent discussion than intended with physicians.
Finally, since the intervention was developed and tailored based on the transtheoretical model, our null results raise the question of possible limitations of this model. Given the limitations of this study, we cannot be definitive on this point. However, the results do call into question the role of the transtheoretical model in this intervention.
Limitations and strengths
There are limitations of our study. First, our participants had higher baseline activity levels than anticipated and reported in previous studies; perhaps the intervention would have been more effective with a different (more sedentary) population. Since the intervention materials were geared towards sedentary patients, the intervention may not have been sufficiently matched to our participants' physical activity levels. Another important limitation is that cluster randomization was used, randomizing at the level of the physician; thus, some patient baseline characteristics were unbalanced in this sample. Randomization at the patient level would likely have resulted in more comparable distributions of patient demographics. We do not have the primary care provider's perspective on the degree to which the participants discussed their intervention materials with them. Therefore, clinician involvement may have been less robust than anticipated which also would have reduced the effect of the intervention.
Despite the limitations, there are several strengths of this study. First, it had a randomized controlled design and recruited patients from a relatively large (n=22) group of primary care practices. The study had a higher representation of African Americans than usually reported in this type of research. The high retention rate (89.6%) suggests that the intervention was well received. Despite not seeing differences between groups on physical activity, participants had large increases in physically activity within groups; we saw the largest increase in the most sedentary individuals at baseline which may be clinically significant and worthy of further study. This study also had a well-designed tracking mechanism to verify the dose received of intervention, and was designed to be more patient driven than clinician dependent.
Recommendations for research
Research on physical activity interventions in primary care should evaluate additional patient-clinician interventions for diverse groups and practice settings to discover effective strategies to target sedentary individuals. Research should also endeavor to develop optimal content of messages and/or channels (print-based, internet based) most likely to be effective, and engage clinicians to the fullest extent possible given their real-world constraints and competing demands.
Conclusion
A theoretically based, tailored computerized physical activity intervention targeting adult primary care patients was feasible to accomplish with a high retention rate. However, computerized tailored physical activity reports did not significantly increase physical activity levels among ethnically and socioeconomically diverse adults in primary care. Further research is needed to determine optimal intervention content, delivery channel, dose, and the role of clinician involvement in primary care.
Table 2. Minutes of physical activity (baseline and at six months) for intervention and control groups.
Total PAR, leisure, and nonleisure minutes for moderate and vigorous activity, by group
| Total minutes (leisure and nonleisure) | ||||
|---|---|---|---|---|
| Variable | Time | Total Mean ± SD |
Intervention group Mean ± SD |
Control group Mean ± SD |
| Moderate activity, minutes per week | Baseline | 179.6 ± 265.5 | 163.0 ± 206.1 | 194.7 ± 309.2 |
| 6 months | 256.0 ± 304.1 | 260.6 ± 316.0 | 251.9 ± 360.8 | |
| Vigorous activity, minutes per week | Baseline | 31.4 ± 99.9 | 25.2 ± 73.5 | 36.9 ± 118.7 |
| 6 months | 47.0 ± 124.5 | 42.2 ± 119.4 | 51.2 ± 129.1 | |
| Total activity, minutes per week | Baseline | 211.0 ± 299.9 | 188.2 ± 224.2 | 231.6 ± 354.0 |
| 6 months | 303.0 ± 381.9 | 302.8 ± 347.3 | 303.1 ± 410.8 | |
| Leisure minutes of physical activity | ||||
| Variable | Time |
Total Mean ± SD |
Intervention group Mean ± SD |
Control group Mean ± SD |
| Moderate activity, minutes per week | Baseline | 95.9 ± 125.0 | 96.7 ± 121.9 | 95.2 ± 128.1 |
| 6 months | 152.2 ± 184.7 | 158.6 ± 188.0 | 146.6 ± 182.1 | |
| Vigorous activity, minutes per week | Baseline | 18.0 ± 54.2 | 17.7 ± 46.7 | 18.4 ± 60.3 |
| 6 months | 28.6 ± 89.2 | 29.4 ± 99.5 | 27.9 ± 79.4 | |
| Total activity, minutes per week | Baseline | 113.9 ± 132.3 | 114.4 ± 127.2 | 113.6 ± 137.0 |
| 6 months | 180.8 ± 213.6 | 188.0 ± 221.1 | 174.5 ± 207.3 | |
| Non-leisure minutes of physical activity | ||||
| Variable | Time |
Total Mean ± SD |
Intervention group Mean ± SD |
Control group Mean ± SD |
| Moderate activity, minutes per week | Baseline | 83.2 ± 232.0 | 66.3 ± 165.2 | 98.4 ± 278.4 |
| 6 months | 103.5 ± 296.4 | 101.6 ± 259.8 | 105.2 ± 325.8 | |
| Vigorous activity, minutes per week | Baseline | 13.3 ± 84.0 | 7.5 ± 52.1 | 18.6 ± 104.6 |
| 6 months | 18.3 ± 87.6 | 12.7 ± 62.9 | 23.3 ± 104.5 | |
| Total activity, minutes per week | Baseline | 96.5 ± 269.6 | 73.9 ± 183.8 | 117.0 ± 327.5 |
| 6 months | 121.9 ± 329.4 | 114.2 ± 269.8 | 128.6 ± 374.7 | |
Acknowledgments
We extend our sincere thanks and appreciation to the patients and physicians who participated in this project, and to all research staff who supported the implementation and data collection. This study was funded by the National Heart, Lung, and Blood Institute R01 HL067005 (PI: Sciamanna), clinicaltrials.gov identifier NCT00242658
Footnotes
Conflict of Interest Statement/Relevant Financial Relationships: The authors have no potential, perceived, or real conflicts of interest to report. The authors have no relevant financial relationships to report.
Reference List
- 1.Woodwell DA, Cherry DK. National Ambulatory Medical Care Survey: 2002 summary. Advance Data. 2004;346:1–44. [PubMed] [Google Scholar]
- 2.Ashenden R, Silagy C, Weller D. A systematic review of the effectiveness of promoting lifestyle change in general practice. Fam Pract. 1997;14:160–176. doi: 10.1093/fampra/14.2.160. [DOI] [PubMed] [Google Scholar]
- 3.Eaton CB, Menard LM. A systematic review of physical activity promotion in primary care office settings. British Journal of Sports Medicine. 1998;32:11–16. doi: 10.1136/bjsm.32.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Simons-Morton DG, Calfas KJ, Oldenburg B, Burton NW. Effects of interventions in health care settings on physical activity or cardiorespiratory fitness. American Journal of Preventive Medicine. 1998;15:413–430. doi: 10.1016/s0749-3797(98)00078-6. [DOI] [PubMed] [Google Scholar]
- 5.Godin G, Shephard R. An evaluation of the potential role of the physician in influencing community exercise behavior. American Journal of Preventive Medicine. 1990;4:225–229. doi: 10.4278/0890-1171-4.4.255. [DOI] [PubMed] [Google Scholar]
- 6.Kreuter MW, Chheda SG, Bull FC. How does physician advice influence patient behavior? Evidence for a priming effect. Archives of Family Medicine. 2000;9(5):426–33. doi: 10.1001/archfami.9.5.426. [DOI] [PubMed] [Google Scholar]
- 7.Washingotn DUPHS, editor. US Preventive Services Task Force. Clinician's handbook for preventive services. 2nd. International Medical Publishing; 2005. 1998. [Google Scholar]
- 8.Walsh JM, Swangard DM, Davis T, McPhee SJ. Exercise counseling by primary care physicians in the era of managed care. American Journal of Preventive Medicine. 1999;16:307–313. doi: 10.1016/s0749-3797(99)00021-5. [DOI] [PubMed] [Google Scholar]
- 9.Eakin EG, Glasgow RE, Riley KM. Review of primary care-based physical activity intervention studies: effectiveness and implications for practice and future research. J Fam Pract. 2000;49:158–168. [PubMed] [Google Scholar]
- 10.Goldstein MG, Whitlock EP, DePue J, Planning Committee of the Addressing Multiple Behavioral Risk Factors in Primary Care Project Multiple behavioral risk factor interventions in primary care. Summary of research evidence. American Journal of Preventive Medicine. 2004;27:61–79. doi: 10.1016/j.amepre.2004.04.023. [DOI] [PubMed] [Google Scholar]
- 11.Yarnall KS, Pollak KI, Ostbye T, Krause KM, Michener JL. Primary care: is there enough time for prevention? Am J Public Health. 2003;93:635–641. doi: 10.2105/ajph.93.4.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Writing Group for the Activity Counseling Trial Research Group. Effects of physical activity counseling in primary care: The Activity Counseling Trial: A randomized controlled trial. JAMA. 2001;286:677–687. doi: 10.1001/jama.286.6.677. [DOI] [PubMed] [Google Scholar]
- 13.Pinto BM, Goldstein MG, Ashba J, Sciamanna CN, Jette A. Randomized controlled trial of physical activity counseling for older primary care patients. American Journal of Preventive Medicine. 2005;29:247–255. doi: 10.1016/j.amepre.2005.06.016. [DOI] [PubMed] [Google Scholar]
- 14.Imperial Cancer Research Fund OXCHECK Study Group. Effectiveness of health checks conducted by nurses in primary care: final results of the OXCHECK study. BMJ. 1995;310:1099–1104. [PMC free article] [PubMed] [Google Scholar]
- 15.Swinburn BA, Walter LG, Arroll B, Tilyard MW, Russell DG. The green prescription study: a randomized controlled trial of written exercise advice provided by general practitioners. Am J Public Health. 1998;88:288–291. doi: 10.2105/ajph.88.2.288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Calfas KJ, Long BJ, Sallis JF, Wooten WJ, Pratt M, Patrick K. A controlled trial of physician counseling to promote the adoption of physical activity. Prev Med. 1996;25:225–233. doi: 10.1006/pmed.1996.0050. [DOI] [PubMed] [Google Scholar]
- 17.Stevens W, Hillsdon M, Thorogood M, McArdle D. Cost-effectiveness of a primary care based physical activity intervention in 45-74 year old men and women: a randomised controlled trial. British Journal of Sports Medicine. 1998;32:236–241. doi: 10.1136/bjsm.32.3.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Burton LC, Paglia MJ, German PS, Shapiro S, Damiano AM. The effect among older persons of a general preventive visit on three health behaviors: smoking, excessive alcohol drinking, and sedentary lifestyle. The Medicare Preventive Services Research Team. Prev Med. 1995;24:492–497. doi: 10.1006/pmed.1995.1078. [DOI] [PubMed] [Google Scholar]
- 19.Dowell AC, Ochera JJ, Hilton SR, et al. Prevention in practice: results of a 2-year follow-up of routine health promotion interventions in general practice. Fam Pract. 1996;13:357–362. doi: 10.1093/fampra/13.4.357. [DOI] [PubMed] [Google Scholar]
- 20.Logsdon DN, Lazaro CM, Meier RV. The feasibility of behavioral risk reduction in primary medical care. American Journal of Preventive Medicine. 1989;5:249–256. [PubMed] [Google Scholar]
- 21.Lewis BS, Lynch WD. The effect of physician advice on exercise behavior. Prev Med. 1993;22:110–121. doi: 10.1006/pmed.1993.1008. [DOI] [PubMed] [Google Scholar]
- 22.Kinmonth AL, Wareham NJ, Hardeman W, et al. Efficacy of a theory-based behavioural intervention to increase physical activity in an at-risk group in primary care (ProActive UK): a randomised trial. Lancet. 2008;371:41–48. doi: 10.1016/S0140-6736(08)60070-7. [DOI] [PubMed] [Google Scholar]
- 23.Eakin EG, Lawler SP, Vandelanotte C, Owen N. Telephone interventions for physical activity and dietary behavior change: a systematic review. American Journal of Preventive Medicine. 2007;32:419–434. doi: 10.1016/j.amepre.2007.01.004. [DOI] [PubMed] [Google Scholar]
- 24.Fjeldsoe BS, Marshall AL, Miller YD. Behavior Change Interventions Delivered by Mobile Telephone Short-Message Service. American Journal of Preventive Medicine. 2009;36:165–173. doi: 10.1016/j.amepre.2008.09.040. [DOI] [PubMed] [Google Scholar]
- 25.Rhodes K, Lauderdale D, Stocking C, Howes D, Roizen M, Levinson W. Better health while you wait:a controlled trial of a computer-based intervention for screening and health promotion in the emergency department. Emergency Medicine. 2001;37:284–291. doi: 10.1067/mem.2001.110818. [DOI] [PubMed] [Google Scholar]
- 26.Strecher V, Shiffman S, West R. Randomized controlled trial of a web-based computer-tailored smoking cessation program as a supplement to nicotine patch therapy. Addiction. 2005;100:682–688. doi: 10.1111/j.1360-0443.2005.01093.x. [DOI] [PubMed] [Google Scholar]
- 27.Napolitano MA, Fotheringham M, Tate D, et al. Evaluation of an internet-based physical activity intervention: a preliminary investigation. Annals of Behavioral Medicine. 2003;25:92–99. doi: 10.1207/S15324796ABM2502_04. [DOI] [PubMed] [Google Scholar]
- 28.McKay H, King D, Eakin EG, Seeley J, Glasgow RE. The diabetes network Interent-based physical activity intervention: a randomized pilot study. Diabetes Care. 2001;24:1328–1334. doi: 10.2337/diacare.24.8.1328. [DOI] [PubMed] [Google Scholar]
- 29.Joseph CL, Peterson E, Havstad S, et al. A web-based, tailored asthma management program for urban African-American high school students. American Journal of Respiratory & Critical Care Medicine. 2007;175:888–895. doi: 10.1164/rccm.200608-1244OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Spittaels H, DeBourdeaudhuij I, Brug J, Vandelanotte C. Effectiveness of an online computer-tailored physical activity intervention in a real-life setting. Health Education Research. 2007;22:385–396. doi: 10.1093/her/cyl096. [DOI] [PubMed] [Google Scholar]
- 31.Kroeze W, Werkman A, Brug J. A systematic review of randomized trials on the effectiveness of computer-tailored education on physical activity and dietary behaviors. Ann Behav Med. 2006;31:205–223. doi: 10.1207/s15324796abm3103_2. [DOI] [PubMed] [Google Scholar]
- 32.Bladay G, Berra K, Golding L, Gordon N, Mahler D, Myers D, et al. In: ACSM's Guidelines for Exercise Testing and Prescription. 6th. Franklin B, Whaley M, Howley E, editors. New York: Lippincott, Williams, and Wilkins; 2000. [Google Scholar]
- 33.Marcus BH, Bock BC, Pinto BM, Forsyth LH, Roberts MB, Traficante RM. Efficacy of an individualized, motivationally-tailored physical activity intervention. Annals of Behavioral Medicine. 1998;20:174–180. doi: 10.1007/BF02884958. [DOI] [PubMed] [Google Scholar]
- 34.Marcus BH, Emmons KM, Simkin-Silverman LR, et al. Evaluation of motivationally tailored vs. standard self-help physical activity interventions at the workplace. American Journal of Health Promotion. 1998;12:246–253. doi: 10.4278/0890-1171-12.4.246. [DOI] [PubMed] [Google Scholar]
- 35.Marcus BH, Napolitano MA, King AC, et al. Telephone versus print delivery of an individualized motivationally tailored physical activity intervention: Project STRIDE. Health Psychol. 2007;26:401–409. doi: 10.1037/0278-6133.26.4.401. [DOI] [PubMed] [Google Scholar]
- 36.Marcus BH, Rossi JS, Selby VC, Niaura RS, Abrams DB. The stages and processes of exercise adoption and maintenance in a worksite sample. Health Psychol. 1992;11:386–395. doi: 10.1037//0278-6133.11.6.386. [DOI] [PubMed] [Google Scholar]
- 37.Plimpton S, Root J. Materials and strategies that work in low literacy health communication. Public Health Rep. 1994;109:86–92. [PMC free article] [PubMed] [Google Scholar]
- 38.Stone EG, Morton SC, Hulscher ME, et al. Interventions that increase use of adult immunization and cancer screening services: a meta-analysis. Ann Intern Med. 2002;136:641–651. doi: 10.7326/0003-4819-136-9-200205070-00006. [DOI] [PubMed] [Google Scholar]
- 39.Dunn AL, Marcus BH, Kampert JB, Garcia ME, Kohl HW, III, Blair SN. Comparison of lifestyle and structured interventions to increase physical activity and cardiorespiratory fitness: a randomized trial. JAMA. 1999;281:327–334. doi: 10.1001/jama.281.4.327. [DOI] [PubMed] [Google Scholar]
- 40.Dunn AL, Garcia ME, Marcus BH, Kampert JB, Kohl HW, Blair SN. Six-month physical activity and fitness changes in Project Active, a randomized trial. Med Sci Sports Exerc. 1998;30:1076–1083. doi: 10.1097/00005768-199807000-00009. [DOI] [PubMed] [Google Scholar]
- 41.Sallis JF, Haskell WL, Wood PD, et al. Physical activity assessment methodology in the Five-City Project. Am J Epidemiol. 1985;121:91–106. doi: 10.1093/oxfordjournals.aje.a113987. [DOI] [PubMed] [Google Scholar]
- 42.Hayden-Wade HA, Coleman KJ, Sallis JF, Armstrong C. Validation of the telephone and in-person interview versions of the 7-day PAR. Med Sci Sports Exerc. 2003;35:801–809. doi: 10.1249/01.MSS.0000064941.43869.4E. [DOI] [PubMed] [Google Scholar]
- 43.Blair SN, Haskell WL, Ho P, et al. Assessment of habitual physical activity by a seven-day recall in a community survey and controlled experiments. Am J Epidemiol. 1985;122:794–804. doi: 10.1093/oxfordjournals.aje.a114163. [DOI] [PubMed] [Google Scholar]
- 44.Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: toward an integrative model of change. Journal of Consulting & Clinical Psychology. 1983;51(3):390–5. doi: 10.1037//0022-006x.51.3.390. [DOI] [PubMed] [Google Scholar]
- 45.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System survey questionnaire. Atlanta, GA: Department of Health and Human Services, Centers for Disease Control and Prevention; 2004. [Google Scholar]
- 46.Schafer JL. Analysis of Incomplete Multivariate Data. New York: Chapman and Hall; 1997. [Google Scholar]
- 47.Napolitano MA, Whiteley JA, Papandonatos G, et al. Outcomes from the women's wellness project: a community-focused physical activity trial for women. Prev Med. 2006;43:447–453. doi: 10.1016/j.ypmed.2006.06.011. [DOI] [PubMed] [Google Scholar]
- 48.Marcus BH, Lewis BA, Williams DM, et al. A comparison of Internet and print-based physical activity interventions. Arch Intern Med. 2007;167:944–949. doi: 10.1001/archinte.167.9.944. [DOI] [PubMed] [Google Scholar]
- 49.Marcus BH, Napolitano MA, King AC, et al. Examination of print and telephone channels for physical activity promotion: Rationale, design, and baseline data from Project STRIDE. Contemporary Clinical Trials. 2007;28:90–104. doi: 10.1016/j.cct.2006.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Eakin E, Reeves M, Lawler S, et al. Telephone counseling for physical activity and diet in primary care patients. American Journal of Preventive Medicine. 2009;36:142–149. doi: 10.1016/j.amepre.2008.09.042. [DOI] [PubMed] [Google Scholar]
- 51.American College of Sports Medicine. ACSM's Guidelines for exercise testing and prescription. Baltimore: Lippincott, Williams, & Wilkins; 2006. [Google Scholar]
- 52.United States Department of Health and Human Services. The 2008 Physical Activity Guidelines for Americans. 2008 [Google Scholar]
- 53.Stern MJ, Gorman PA, Kaslow L. The group counseling v exercise therapy study. A controlled intervention with subjects following myocardial infarction. Arch Intern Med. 1983;143:1719–1725. [PubMed] [Google Scholar]
- 54.Marshall AL, Booth ML, Bauman AE. Promoting physical activity in Australian general practices: a randomised trial of health promotion advice versus hypertension management. Patient Educ Couns. 2005;56:283–290. doi: 10.1016/j.pec.2004.03.002. [DOI] [PubMed] [Google Scholar]