Abstract
Aim
Nonadherent individuals are the most likely to avoid participating in research studies, thus limiting potential opportunities to develop evidence-based approaches for adherence enhancement. This mixed-method analysis evaluated factors related to adherence among 20 poorly adherent community mental health clinic patients with bipolar disorder (BD).
Methods
Illness experience was evaluated with qualitative interview. Quantitative assessments measured symptoms (Hamilton Depression Rating Scale, Young Mania Rating Scale, Brief Psychiatric Rating Scale), adherence behavior, and treatment attitudes. Poor adherence was defined as missing 30% or more of medication.
Results
Minorities (80%), unmarried individuals (95%), and those with substance abuse (65%) predominated in this nonadherent group of patients with BD. Individuals were substantially depressed (mean Hamilton Depression Rating Scale, 19.2), had at least some manic symptoms (mean Young Mania Rating Scale, 13.6), and had moderate psychopathology (mean Brief Psychiatric Rating Scale, 41.2). Rates of missed medications were 41% to 43%. Forgetting to take medications was the top reason for nonadherence (55%), followed by side effects (20%). Disorganized home environments (30%), concern regarding having to take long-term medications (25%) or fear of side effects (25%), and insufficient information regarding BD (35%) were relatively common. Almost one third of patients had individuals in their core social network who specifically advised against medication. Access problems included difficulty paying for medications among more than half of patients. Interestingly, patients reported good relationships with their providers.
Conclusions
Forgetting to take medication and problems with side effects are primary drivers of nonadherence. Lack of medication routines, unsupportive social networks, insufficient illness knowledge, and treatment access problems may likewise affect overall adherence. Complementary quantitative and qualitative data collection can identify reasons for nonadherence and may inform specific clinical approaches to enhance adherence.
1. Introduction
Psychotropic medications are a cornerstone of treatment for individuals with bipolar disorder (BD); however, nonadherence with prescribed medication is pervasive and is associated with negative outcomes, such as illness relapse [1,2]. Clinically relevant BD nonadherence has been defined as missing 20% to 30% or more of prescribed medication [3,4]. Two large Veterans Administration (VA) studies on treatment adherence of patients with bipolar disorder found that 46% to 48% of patients with bipolar disorder miss at least 20% of prescribed maintenance medication [5,6]. In these studies, predictors for missing at least 20% of prescribed BD medication treatments were younger age, unmarried status, minority ethnicity, and comorbid substance abuse or posttraumatic stress disorder [5,6]. Other predictors of treatment nonadherence in BD include male sex, poor social support, inadequate knowledge of BD, and health beliefs that are not consistent with maintaining long-term medication prophylaxis [3,7–9].
Most studies have not focused specifically on nonadherent populations with bipolar disorder, and few studies have further addressed these individuals’ perceptions of illness and treatment in relation to medication treatment adherence [7,8]. Patient-focused qualitative methods may shed valuable insights on patients’ beliefs about treatment [10]. Unless one understands why an individual may or may not adhere to prescribed BD medication treatment, it is difficult to develop interventions that address nonadherence. In addition, focusing on patients with BD who are known to be poorly adherent may provide invaluable information toward intervention development to improve care for BD subpopulations at greatest risk for poor health outcomes.
This is a mixed-method (qualitative and quantitative) characterization of reasons for treatment nonadherence among individuals known to be poorly adherent with medication treatment. The study used a standardized adherence cutoff, and all participants with BD were receiving care in a public sector mental health setting.
2. Methods
2.1. Population and procedures
Participants had type I or II BD confirmed by the Mini-International Neuropsychiatric Interview (MINI) [11], were receiving treatment at a community mental health clinic (CMHC), and were known to be poorly adherent. Poor adherence was defined as self-reporting missing 30% or more of medication within either the past week or past month using the Tablets Routine Questionnaire [3,12]. Adherence was also identified via pill counts. Additional study inclusion criteria were BD for at least 2 years duration and treatment with an antipsychotic agent or a mood stabilizer for at least 6 months. The study was approved by the local institutional review board.
2.2. Measures
Study participants were evaluated using the Subjective Experience of Medication Interview Treatment Adherence Bipolar Disorder Version (SEMI TAD BD), a qualitative interview modified from the original SEMI [13]. The SEMI TAD BD focuses on (1) patient factors (explanatory model of illness, comfort with fund of knowledge, patterns of treatment adherence, stance toward medications in general, self-management behaviors, self-medications, sociability patterns with respect to bipolarity, occupational factors, and cultural factors), (2) environmental/social factors (home environment, social relations/psychosocial supports, and negative social effects), (3) provider/system factors (perceived helpfulness and communications with providers), (4) health beliefs (perceived illness severity, susceptibility to illness, and benefits of treatment), and (5) costs/burdens associated with treatment (medication regimen burden, side effects, stigma, affordability, and care access).
Most items in the SEMI TAD BD can be answered with a short response, for example, “Did you ever have difficulties with taking or remembering to take your medications in the past?” The question is then expanded to query individuals who respond affirmatively to further elaborate. At the conclusion of the semistructured interview, participants were asked to provide their opinion on their main reason for treatment nonadherence.
In addition to the SEMI TAD BD, quantitative assessments of bipolar symptoms and psychopathology (Hamilton Depression Rating Scale [HAMD] [14], Young Mania Rating Scale [YMRS] [15], Brief Psychiatric Rating Scale [BPRS] [16], Clinical Global Impression for use in Bipolar Disorder [17]) and key attitudinal standardized measures of bipolar treatment including the Attitude toward Mood Stabilizers Questionnaire (AMSQ) [3,18], the Drug Attitude Inventory (DAI) [19], and the Rating of Medication Influences (ROMI) [20] were conducted.
The AMSQ is a modification of the Lithium Attitudes Questionnaire [21], which evaluates an individual’s attitudes toward mood-stabilizing medication [3,18]. The AMSQ has 7 subscales representing key attitudinal domains including (1) opposition to prophylaxis, (2) denial of therapeutic effectiveness, (3) fear of side effects, (4) difficulty with medication routines, (5) denial of illness severity, (6) negative attitude toward drugs in general, and (7) lack of information about mood stabilizers [3,18,21]. Higher scores on each subscale represent more negative attitudes. The DAI is used to measure attitudes toward medication among individuals with serious mental illness [19]. The ROMI is a measure of attitudes toward medication treatment, which has been demonstrated to identify health beliefs and key reasons for medication nonadherence [1,18,22]. The ROMI contains 19 items that directly inquire about influences leading to adherence (9 items) and those leading to nonadherence (10 items).
2.3. Data analysis
Descriptive analysis was conducted using the demographic/clinical information and quantitative findings. The SEMI TAD BD was transcribed from the audiotapes in its entirety and entered into a software program, Atlas.ti (Scientific Software Development GmbH) [23], to be able to code and analyze the qualitative data systematically [24,25]. Narrative data from the SEMI TAD BD were coded into discrete themes and evaluated across participants for each thematic domain. Multirater consensus coding was conducted on an ongoing basis by the research team to continually refine and improve coding accuracy. For this analysis, 2 independent raters coded each SEMI question with resulting κ values in each domain ranging from 0.63 to 1.0 (environmental/social factors), 0.6 to 1.0 (patient factors related to illness experience), 0.69 to 1.0 (health belief factors), 1.0 all scores (provider/system factors), and 0.63 to 1.0 (costs/burden factors). The median κ score for each SEMI question was 1.0 (perfect agreement between raters).
3. Results
3.1. Quantitative findings
Table 1 illustrates demographic and standardized rating scale characteristics. Minorities (80%, n = 16), unmarried individuals (95%, n = 19), and those with substance abuse/use predominated. Substance abuse/use identification (65%, n = 13) was derived from the MINI, SEMI TAD BD, and ROMI to minimize substance abuse underreporting.
Table 1.
Clinical characteristics of nonadherent patients with BD
| Frequency, n (%) | Mean (median) | SD | Range | |
|---|---|---|---|---|
| Age | 37 (36.5) | 12.14 | 18–59 | |
| Sex | ||||
| Female | 14 (70) | |||
| Race | ||||
| Euro-American | 4 (20) | |||
| African American | 14 (70) | |||
| American Indian/Native American | 1 (5) | |||
| Asian | 1 (5) | |||
| Marital status | ||||
| Single | 13 (65) | |||
| Married | 1 (5) | |||
| Separated | 1 (5) | |||
| Divorced | 5 (25) | |||
| Education (y) | 13 (12.0) | 2.12 | 9–16 | |
| Occupation | ||||
| Full time | 4 (20) | |||
| Part time | 2 (10) | |||
| Unemployed | 8 (40) | |||
| Other | 6 (30) | |||
| History of sexual abuse | 12 (60) | |||
| Substance abuse/dependence (current)a | 9 (45) | |||
| Bipolar type | ||||
| I | 13 (65) | |||
| II | 7 (35) | |||
| HAMD-17 | 19.20 (18.5) | 5.1 | 12–28 | |
| YMRS | 13.6 (14.5) | 7.28 | 3–35 | |
| BPRS | 41.2 (40) | 8.06 | 29–60 | |
| CGI-BP | ||||
| Mania | 3.8 (4.0) | 1.19 | 2–7 | |
| Depression | 4.7 (5.0) | 0.98 | 2–7 | |
| Overall bipolar illness | 4.4 (4.0) | 0.59 | 4–6 | |
| AMSQ total | 8.3 (8.0) | 4.13 | 2–16 | |
| Subscales mean (average per itemb) | ||||
| Opposition to prophylaxis | 1.35 (0.34) | 1.35 | 0–4 | |
| Denial of therapeutic effectiveness | 0.40 (0.20) | 0.68 | 0–2 | |
| Fear of side effects | 1.00 (0.50) | 0.73 | 0–2 | |
| Difficulty with medication routines | 2.65 (0.66) | 1.23 | 0–4 | |
| Denial of illness severity | 1.65 (0.55) | 0.88 | 0–3 | |
| Negative attitude toward drugs in general | 0.95 (0.32) | 0.76 | 0–2 | |
| Lack of information about mood stabilizers | 0.30 (0.30) | 0.47 | 0–1 | |
| DAI | 4.61 (4.0) | 2.78 | 0–9 | |
| Pill count, % missed | 40.86% | 30.66 | 7–100 | |
| TRQ | ||||
| Past month | 41% | 17.84 | 13–100 | |
| Past week | 43% | 17.43 | 14–100 | |
| ROMI | ||||
| Adherence | 16.25 (16.5) | 3.83 | 5–22 | |
| Nonadherence | 11.95 (12.5) | 3.96 | 3–21 | |
DAI indicates Drug Attitude Inventory (10-item version, scale calibrated 0–10 with 10 being more positive attitudes); HAMD-17, Hamilton Depression Rating Scale, 17-item version; CGI-BP, Clinical Global Impression for use in Bipolar Disorder; TRQ, Tablets Routine Questionnaire, % of pills missed in last month or week as noted; Pill count, adherence to medication determined by pill count (last month).
As defined by the MINI.
AMSQ subscales have varying numbers of items.
Individuals were substantially depressed (mean 17-item HAMD, 19.2; range, 12–28), had at least some manic symptoms (mean YMRS, 13.6; range, 3–35), and had moderate psychopathology (mean BPRS, 41.2; range, 29–60). Rates of missing prescribed medications were in the order of 41% to 43%. The AMSQ, DAI, and ROMI found generally negative attitudes toward medication and limited insight into illness.
The AMSQ subscales, mean values, and average item-response values per subscale are listed in Table 1. The highest average item-response values (more negative attitudes toward medication) were the subscales addressing difficulty with medication routines, denial of illness severity, and fear of medication side effects. Fig. 1 identifies the individual AMSQ item scoring, in terms of mean item-response value, and indicates the items that in particular have relatively high scores (more negative attitudes).
Fig. 1.
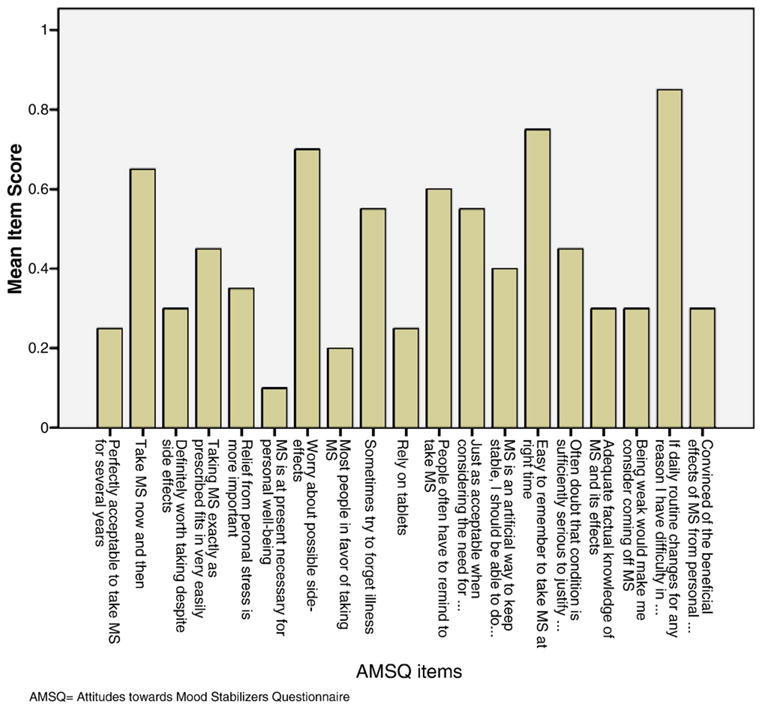
The AMSQ item mean scores among poorly adherent bipolar patients. Higher mean scores mean greater opposition/negative attitudes toward taking prescribed medication treatment for bipolar disorder.
3.2. Qualitative findings
3.2.1. Self-identified primary reasons for medication nonadherence
Consistent with findings from the quantitative measures, forgetting to take medications was the top self-reported reason for nonadherence (55%). On the qualitative assessment, patients identified side effects (20%) as the second most common reason for nonadherence. Other reasons included not wishing to take medications for the rest of one’s life and desire to experience manic symptoms.
3.2.2. Environmental/Social factors
Although 55% (n = 11) of individuals described their living place as easygoing, almost one third (n = 3) described their homes as tense, unpleasant, or disorganized (n = 6). Social contact was deemed inadequate by 35% (n = 7) of participants, and 35% (n = 7) did not feel there were individuals in their social network with whom they could talk freely about their illness. Half of the individuals (n = 10) noted that there was someone in their support network who reminded them to take medications, but almost one third (n = 6) had individuals who specifically advised against medications.
One participant described her experience with being told not to take medications, “My mother said I should think about it and try to use…reason and creativity instead of the medication.”
Another participant noted, “Some people don’t believe in them [medication] and they voice that opinion.”
3.2.3. Patient factors related to illness experience
Just over one third (n = 7) of individuals felt that they did not have enough information about BD. Most (70%, n = 14) of the individuals noted that they had difficulty taking or remembering to take medications and at times did not believe in taking pills (65%, n = 13).
One participant described forgetting her medications, “I don’t say I am not going to take it today because I feel good. It’s just because I forget to take it.”
Another participant described how ambivalence regarding need for medication and forgetting to take medications both contributed to her nonadherence, “One thing was I was trying to see if I could go without taking them, but the other thing was that it’s not that I decide not to take them—well, maybe I do.…I don’t remember if I took them, so rather than double-take them, I’ll just do without them…”
Another participant noted that her twice-daily medication regimen contributed to difficulty remembering, “It would be better for me to be able to take once a day than to remember to take twice a day and which ones to take twice a day.”
Individuals had a variety of methods to help them remember to take medications, including putting them in a consistent/specific place (35%, n = 7), labeling or writing reminders, taking medications at a consistent/specific time (15%, n = 3), or some combinations of multiple methods (5%, n = 1). Two thirds of individuals (65%, n = 13) reported that religion or spirituality was important to their coping with illness. Alcohol was used by 45% (n = 9), and recreational drugs were used by 25% (n = 5), with slightly differing proportions of individuals admitting to using/abusing substances depending on the format of the interview questions.
3.2.4. Health belief factors
Most individuals perceived that their BD treatments had helpful effects on overall mood (75%, n = 15,), functional level (70%, n = 14), and stress levels (80%, n = 16), although individuals also noted problems with their medications, such as not liking having to take medications in the first place (25%, n = 5) or the possibility of long-term or unknown side effects (25%, n = 5). More than half (55%, n = 11) reported that they did not feel like they had any personal power or control over their illness.
One participant described how she viewed the effects of medication, “I feel…kind of foggy and cloudy, but the advantages of taking them is better than the set-backs so it’s worthwhile.”
3.2.5. Provider/System factors
Nearly all individuals reported a good relationship with their treatment provider (95%, n = 19), and most (75%, n = 15) had no difficulty communicating with their provider.
3.2.6. Costs/Burdens
Individuals encountered a variety of barriers to taking medications, including a perception that they had an excessive number of prescribed medications (25%, n = 5), an excessive dose of medications (20%, n = 4), and access problems including inability to pay for medications (60%, n = 12) or get transportation to appointments (35%, n = 7). Burdensome side effects included multiple physical complaints (25%, n = 5) or specific problems, such as drowsiness (15%, n = 3).
One participant described how side effects impacted her general health and her relationships with others, “I don’t like the side effects. I don’t like how people judge me because I’m on medication and I’ve gained over 100 lb in less than a year.”
Finally, the group was evenly split among those who believed that mental illness is associated with stigma (n = 9, 45%) and those who did not feel there was stigma related to having a mental illness (n = 9, 40%). Only half of the group (n = 10) noted that they routinely shared information regarding their mental diagnosis with others.
One participant described the impact of stigma, “I’m kind of embarrassed about it because a lot of people get afraid.”
4. Discussion
This mixed-method analysis evaluated patients with BD receiving treatment in a public sector mental health setting using a standardized adherence cutoff. Quantitative analysis suggested that difficulties with medication routines, worry about medication side effects, and denial of illness severity were the most important contributors to negative attitudes toward BD medications. Qualitative findings characterized the strong effect of forgetting on nonadherence, the impact of such side effects as sedation and weight gain, and belief that medications were not really needed. Although the quantitative results provided information on general constructs related to nonadherence, qualitative findings provided perspective on specific processes leading to nonadherence.
Consistent with the published literature on clinical characteristics that predict treatment nonadherence, minorities and individuals with less social support predominated [6,7]. Individuals were generally at least moderately symptomatic with substantial manic and/or depressive symptoms. Manic symptoms in particular have been noted to be associated with treatment nonadherence in populations with bipolar disorder [26] and could have contributed to some of the perceived denial of illness severity (or need for medications) seen in our sample. Depression could have contributed to social isolation or lack of engagement in care that precipitated or worsened nonadherence.
Standardized measures of adherence attitudes, such as the AMSQ and ROMI, can be helpful in identifying patients with BD and groups of patients at risk for nonadherence, and it has been suggested that use of multiple measures should be implemented given the various factors that might contribute to adherence [4,27]. Reasons for adherence and reasons for nonadherence as identified by separate subscales of the ROMI were relatively similar in our sample, in contrast to what has been reported in adherent populations with bipolar disorder [22], where there are more marked contrasts in reasons for adherence vs nonadherence (advantage favoring adherence). Attitudes toward medications as measured by total mean AMSQ scores in these poorly adherent patients with bipolar disorder were within the range of total mean AMSQ scores (6.8–9.0) identified in other studies of poorly adherent individuals with bipolar disorder [3,22].
Semistructured qualitative analysis provided further elaboration on factors identified in the quantitative assessment as adherence barriers and identified some additional factors that are potential facilitators or barriers to adherence. The qualitative information provided a contextual description of adherence barriers upon which to formulate possible clinical approaches that can enhance adherence in high-risk patients. Forgetting medications and side effects were primary reasons for not taking prescribed medications. Home settings were perceived by one third of individuals as tense or disorganized, whereas social networks were perceived to be nonsupportive or even directly antagonistic to medication adherence.
Psychosocial interventions intended to enhance treatment adherence in bipolar populations need to address individual/unique psychosocial needs [9,28]. The data from our nonadherent sample suggest that special attention to establishing medication routines (for example, identification of optimum strategies as to where medications are stored, when or how they should be taken, and possibly use of technology-assisted devices) might be particularly helpful. Education and engagement of significant others regarding need for medication maintenance in the treatment of bipolar illness could potentially transform some treatment adversaries into treatment allies. In other instances, where the social network is adamantly opposed to medication treatment, the patient with BD might benefit from additional sources that are supportive of pharmacotherapy, for example, consumer advocacy groups such as the Depression and Bipolar Support Alliance [29].
One third of the sample did not feel that they knew enough about BD and BD treatment, and this may have led to an underappreciation of the severity of illness. This emphasizes the importance of psychoeducation, which is known to promote illness self-management [30,31].
Most individuals in this sample had a variety of methods to try and cope with illness and treatment, including spiritual approaches or self-medication with drugs or alcohol. This suggests a strong role for integrating existing and/or available supports into the pharmacological and psychotherapeutic treatment plan, including consideration of the individual’s spiritual orientation and facilitation of entry into concurrent substance abuse treatment. Individuals who are resistant to or not yet ready to enter substance abuse treatment might benefit from psychosocial approaches that address the negative effects of substance abuse on treatment outcomes, especially when integrated in a provider-patient relationship that includes regular and frequent contact [32,33].
Consistent with some other reports, many of these nonadherent individuals with BD did not feel as though they had personal control over their illness [34]. Although most individuals perceived medications as being helpful, with specific beneficial effects on mood, functional status, and stress levels, this was balanced by concerns about current or potential problems. Promoting health beliefs that support appropriate pharmacotherapy, empowering patients to take control of their illness, and confronting inaccurate health beliefs via psychosocial interventions could improve treatment adherence among individuals who feel powerless with respect to their BD [30,35].
In spite of their nonadherence with prescribed medications, most individuals in the study presented here noted that they had good relationships with the prescribing clinicians—these patients liked their physicians but not the drugs their physicians prescribed. In contrast, Zeber et al [32] have reported that medication adherence is related to therapeutic alliance, with better adherence seen when clinicians regularly review progress and encourage contact. The study did not collect information on specific clinician follow-up frequency for study patients; however, the typical follow-up interval for patients at the CMHC is every 1 to 2 months.
It is possible that the nonadherent patients in our study sample represented a group of individuals who had good therapeutic alliance but selectively elected to not take recommended medications. The study did not also collect information on the providers, and thus, it is not clear how candid the patients were with providers regarding their nonadherence. It is possible that the mental health care providers of these individuals were under the impression that their patients were fully adherent. It has been well demonstrated in the psychiatric literature that clinicians’ assessments of treatment adherence are generally poor. For example, a study of patients with schizophrenia demonstrated that technology-assisted methods such as Medication Event Monitoring Systems (MEMS) classified 48% of schizophrenic patients as nonadherent, whereas clinician ratings failed to classify even one patient as nonadherent [36].
Finally, there were numerous factors that poorly adherent individuals identified as barriers to treatment, which are known to be associated with suboptimal treatment adherence [37]. Medication side effects are a major factor that affects general health, quality of life, and relationships with others. It is critical that clinicians actively seek input from patients on perceived side effects and the relative burden of side effects.
A major problem for nearly two thirds of individuals was inability to pay for medications at least some of the time. Difficulty in paying for medications might have been related to the high rate of unemployment (40%), which could be associated with limited financial resources and/or lack of health insurance. In addition, although the study site CMHC was on a public bus line and had evening and weekend hours, accessing transportation to clinic appointments was a problem for one third of the group. Other barriers to treatment involved perceived burden of number or amounts of pills prescribed.
Limitations of the study include small sample size, single-site study setting, and reliance on imprecise measures of adherence (self-report and pill counts). Individuals at the most extreme of treatment nonadherence (complete treatment dropouts) are not represented in this sample. In addition, the qualitative assessment used in this study was developed based on the principle investigator’s preliminary data regarding barriers and facilitators to care as well as the extant published literature. It is possible that a more comprehensive interview might have yielded additional factors that motivate or impede treatment adherence. We believe that a mixed-method approach, even with such a small sample as is presented here, strengthens the validity of our findings. As noted by Sherman and Strang [38], in synthesizing quantitative and qualitative results, numerical results are linked to patients’ experiences and descriptions that articulate and communicate study findings more effectively.
5. Conclusions
Both quantitative measures, such as the AMSQ and ROMI, and qualitative approaches can be useful in identifying nonadherence and reasons for nonadherence.
Poorly adherent patients with BD identify forgetting to take medication and problems with side effects as primary drivers of nonadherence. However, personal, sociocultural, and economic factors may likewise affect overall adherence.
Potential approaches to improve adherence among patients with BD include measures to provide additional structure to the home setting, medication dosing simplification, technology-assisted prompts, education/intervention with family members, interaction with spiritual advisors, facilitation of substance abuse treatment, psychoeducation on BD and BD treatments, and preemptive and candid discussion between providers and patients regarding expected side effects from medications and how these might be best managed.
Acknowledgments
This research was supported by NIMH R34 5R34MH078967, P.I.: M. Sajatovic.
Footnotes
Portions of this article have been presented at the American Psychiatric Association annual meeting in San Francisco, CA, USA, May 2009 and the 9th World Congress of Biological Psychiatry, Paris, France, June 2009.
References
- 1.American Psychiatric Association. Practice guideline for the treatment of patients with bipolar disorder (revision) Am J Psychiatry. 2002;159:1–50. [PubMed] [Google Scholar]
- 2.Lingam R, Scott J. Treatment non-adherence in affective disorders. Acta Psychiatr Scand. 2002;105:164–72. doi: 10.1034/j.1600-0447.2002.1r084.x. [DOI] [PubMed] [Google Scholar]
- 3.Scott J, Pope M. Nonadherence with mood stabilizers: prevalence and predictors. JClinPsychiatry. 2002;63:384–90. doi: 10.4088/jcp.v63n0502. [DOI] [PubMed] [Google Scholar]
- 4.Velligan DI, Weiden PJ, Sajatovic M, et al. The expert consensus guideline series: adherence problems in patients with serious and persistent mental illness. J Clin Psychiatry. 2009;70(Suppl 4):1–46. [quiz 47-8] [PubMed] [Google Scholar]
- 5.Sajatovic M, Valenstein M, Blow FC, et al. Treatment adherence with antipsychotic medications in bipolar disorder. Bipolar Disord. 2006;8:232–41. doi: 10.1111/j.1399-5618.2006.00314.x. [DOI] [PubMed] [Google Scholar]
- 6.Sajatovic M, Valenstein M, Blow F, et al. Treatment adherence with lithium and anticonvulsant medications among patients with bipolar disorder. Psychiatr Serv. 2007;58:855–63. doi: 10.1176/ps.2007.58.6.855. [DOI] [PubMed] [Google Scholar]
- 7.Berk M, Berk L, Castle D. A collaborative approach to the treatment alliance in bipolar disorder. Bipolar Disord. 2004;6:504–18. doi: 10.1111/j.1399-5618.2004.00154.x. [DOI] [PubMed] [Google Scholar]
- 8.Sajatovic M, Jenkins JH, Cassidy KA, Muzina DJ. Medication treatment perceptions, concerns and expectations among depressed individuals with type I bipolar disorder. J Affect Disord. 2009;115:360–6. doi: 10.1016/j.jad.2008.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Depp CA, Moore DJ, Patterson TL, et al. Psychosocial interventions and medication adherence in bipolar disorder. Dialogues Clin Neurosci. 2008;10:239–50. doi: 10.31887/DCNS.2008.10.2/cadepp. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Clatworthy J, Bowskill R, Rank T, et al. Adherence to medication in bipolar disorder: a qualitative study exploring the role of patients’ beliefs about the condition and its treatment. Bipolar Disord. 2007;9:656–64. doi: 10.1111/j.1399-5618.2007.00434.x. [DOI] [PubMed] [Google Scholar]
- 11.Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. [quiz 34-57] [PubMed] [Google Scholar]
- 12.Peet M, Harvey NS. Lithium maintenance: 1. A standard education programme for patients. Br J Psychiatry. 1991;158:197–200. doi: 10.1192/bjp.158.2.197. [DOI] [PubMed] [Google Scholar]
- 13.Jenkins JH, Strauss ME, Carpenter EA, et al. Subjective experience of recovery from schizophrenia-related disorders and atypical antipsychotics. Int J Soc Psychiatry. 2005;51:211–27. doi: 10.1177/0020764005056986. [DOI] [PubMed] [Google Scholar]
- 14.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Young RC, Biggs JT, Ziegler VE, Meyer DA. A rating scale for mania: reliability, validity and sensitivity. Br J Psychiatry. 1978;133:429–35. doi: 10.1192/bjp.133.5.429. [DOI] [PubMed] [Google Scholar]
- 16.Overall JE, Gorham DR. The Brief Psychiatric Rating Scale. Psychol Rep. 1962;10:799–812. [Google Scholar]
- 17.Guy W. Clinical global impressions. In: Guy W, editor. ECDEU assessment manual for psychopharmacology. Rockville, MD: Department of Health, Education, and Welfare, DHEW; 1976. pp. 76–338. [Google Scholar]
- 18.Adams J, Scott J. Predicting medication adherence in severe mental disorders. Acta Psychiatr Scand. 2000;101:119–24. doi: 10.1034/j.1600-0447.2000.90061.x. [DOI] [PubMed] [Google Scholar]
- 19.Awad AG. Subjective response to neuroleptics in schizophrenia. Schizophr Bull. 1993;19:609–18. doi: 10.1093/schbul/19.3.609. [DOI] [PubMed] [Google Scholar]
- 20.Weiden P, Rapkin B, Mott T, et al. Rating of Medication Influences (ROMI) scale in schizophrenia. Schizophr Bull. 1994;20:297–310. doi: 10.1093/schbul/20.2.297. [DOI] [PubMed] [Google Scholar]
- 21.Harvey NS. The development and descriptive use of the lithium attitudes questionnaire. J Affect Disord. 1991;22:211–9. doi: 10.1016/0165-0327(91)90067-3. [DOI] [PubMed] [Google Scholar]
- 22.Sajatovic M, Ignacio RV, West JA, et al. Predictors of nonadherence among individuals with bipolar disorder receiving treatment in a community mental health clinic. Compr Psychiatry. 2009;50:100–7. doi: 10.1016/j.comppsych.2008.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Muhr T. Atlas.ti software development. 1993 www.atlasti.com.
- 24.Luborsky MR. The identification and analyses of themes and patterns. In: Gubrium J, Snakar A, editors. Qualitative methods in aging research. New York: Sage Publications; 1993. pp. 189–210. [Google Scholar]
- 25.Good B. Medicine, rationality & experience. Cambridge, MA: Cambridge University Press; 1994. [Google Scholar]
- 26.Copeland LA, Zeber JE, Salloum IM, et al. Treatment adherence and illness insight in veterans with bipolar disorder. J Nerv Ment Dis. 2008;196:16–21. doi: 10.1097/NMD.0b013e318160ea00. [DOI] [PubMed] [Google Scholar]
- 27.Sajatovic M, Velligan DI, Weiden PJ, et al. Measurement of psychiatric treatment adherence. J Psychosom Res. 2009 doi: 10.1016/j.jpsychores.2009.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Berk M, Hallam K, Lucas N, et al. Early intervention in bipolar disorders: opportunities and pitfalls. Med J Aust. 2007;187:S11–14. doi: 10.5694/j.1326-5377.2007.tb01328.x. [DOI] [PubMed] [Google Scholar]
- 29.Depression and Bipolar Support Alliance/DBSA: website homepage. Depression and Bipolar Support Alliance/DBSA: website homepage. 2009 March 30; Available at: www.dbsalliance.org.
- 30.Bauer MS, Kilbourne AM, Greenwald DE, et al. Overcoming bipolar disorder: a comprehensive workbook for managing your symptoms and achieving your life goals. Oakland, CA: New Harbinger Publications, Inc; 2008. [Google Scholar]
- 31.Colom F, Vieta E, Martinez, Aran A, et al. A randomized trial on the efficacy of group psychoeducation in the prophylaxis of recurrences in bipolar patients whose disease is in remission. Arch Gen Psychiatry. 2003;60:402–7. doi: 10.1001/archpsyc.60.4.402. [DOI] [PubMed] [Google Scholar]
- 32.Zeber JE, Copeland LA, Good CB, et al. Therapeutic alliance perceptions and medication adherence in patients with bipolar disorder. J Affect Disord. 2008;107:53–62. doi: 10.1016/j.jad.2007.07.026. [DOI] [PubMed] [Google Scholar]
- 33.Horsfall J, Cleary M, Hunt GE, Walter G. Psychosocial treatments for people with co-occurring severe mental illnesses and substance use disorders (dual diagnosis): a review of empirical evidence. Harv Rev Psychiatry. 2009;17:24–34. doi: 10.1080/10673220902724599. [DOI] [PubMed] [Google Scholar]
- 34.Darling CA, Olmstead SB, Lund VE, Fairclough JF. Bipolar disorder: medication adherence and life contentment. Arch Psychiatr Nurs. 2008;22:113–26. doi: 10.1016/j.apnu.2008.02.004. [DOI] [PubMed] [Google Scholar]
- 35.Sachs GS. Psychosocial interventions as adjunctive therapy for bipolar disorder. J Psychiatr Pract. 2008;14(Suppl 2):39–44. doi: 10.1097/01.pra.0000320125.99423.b7. [DOI] [PubMed] [Google Scholar]
- 36.Byerly M, Fisher R, Whatley K, et al. A comparison of electronic monitoring vs. clinician rating of antipsychotic adherence in out-patients with schizophrenia. Psychiatry Res. 2005;133:129–33. doi: 10.1016/j.psychres.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 37.Sajatovic M, Biswas K, Kilbourne AK, et al. Factors associated with prospective long-term treatment adherence among individuals with bipolar disorder. Psychiatr Serv. 2008;59:753–9. doi: 10.1176/ps.2008.59.7.753. [DOI] [PubMed] [Google Scholar]
- 38.Sherman LW, Strang H. Experimental ethnography: the marriage of qualitative and quantitative research. Ann Am Acad Polit Soc Sci. 2004;595:204–22. [Google Scholar]


