Abstract
Psychosocial outcome measures, which attempt to examine acne from the patient's perspective, have become increasingly important in dermatology research. One such measure is the Body Image Disturbance Questionnaire. The authors' primary aim was to determine the validity and internal consistency of the Body Image Disturbance Questionnaire in patients with acne vulgaris. The secondary aim was to investigate the relationship between body image disturbance and quality of life. This cross-sectional investigation included 52 consecutive acne patients presenting to an outpatient dermatology clinic. Subjects completed the Body Image Disturbance Questionnaire, Skindex-16, and other body image and psychosocial functioning measures. An objective assessment of acne was performed. The Body Image Disturbance Questionnaire was internally consistent and converged with other known body image indices. Body Image Disturbance Questionnaire scores also correlated with Skindex-16 scores, confirming that quality of life and body image are related psychosocial constructs. The Body Image Disturbance Questionnaire appears to be an accurate instrument that can assess appearance-related concern and impairment in patients with acne vulgaris. Limitations include a small sample size and the cross-sectional design.
Although many dermatological diseases are not life threatening, they pose a unique challenge to the human psyche. Cutaneous disease carries a distinctive psychosocial burden in that patients who suffer from these diseases are often unable to hide their condition from public scrutiny. Specifically, acne vulgaris is a ubiquitous disease with a known potential to cause significant psychological repercussions.1 Acne is the leading cause for visits to a dermatologist and affects more than 80 percent of adolescents.1 Acne can affect up to 50.9 percent of women and 42.5 percent of men throughout their 20s and can continue to occur throughout adulthood.2 Between 30 to 50 percent of adolescents experience psychological difficulties associated with acne, including body image concerns, embarrassment, social impairment, anxiety, frustration, anger, depression, and poor self-esteem.3 Additionally, suicidal ideation and suicide attempts related to the negative psychosocial impacts of acne have also been documented.4,5 Not only does acne result in emotional distress, the anxiety evoked by having acne can aggravate the skin condition itself, thereby creating a vicious cycle.6
Accordingly, psychosocial outcome measures have become increasingly important in dermatology research. Classical tools and techniques that objectively measure a subject's acne severity, such as counting the subject's acne lesions or grading acne on a scale, provide a unidimensional assessment. Grading a patient's acne based on lesion counts and an acne severity scale will result in a score that entirely fails to take into account the severity of the disease as perceived by the patient. On the other hand, psychosocial outcome measures attempt to examine acne from the subject's perspective, serving as a tool to quantify how this chronic skin disease can affect a person's thoughts, emotional well-being, and ability to function. It is essential for the physician to gauge the psychosocial impact a patient's acne has on his or her life, as this information will likely play a role in how aggressively the disease is treated and help establish treatment goals.
At the other extreme, such a tool might help identify those patients who suffer from a severe discrepancy between what the public sees and what the individual experiences, an example of which is body dysmorphic disorder (BDD). As formally defined by the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, BDD involves a preoccupation with an imagined physical defect; if a slight physical anomaly is present, the person's concern is markedly excessive.7 Consequently, patients who suffer from this condition, by definition, cannot have a clinically significant defect on exam. This subset of acne patients, which can reach as high as 21 percent in some office settings are more likely to report dissatisfaction with dermatological treatment, attempt suicide, and threaten healthcare providers both legally and physically.8–16 Due to the prevalence and severity of BDD, the need to identify BDD, quantify its severity, and properly treat the subpopulation of patients who have it is imperative.
Body image disturbance has been defined as “a persistent report of dissatisfaction, concern, and distress that is related to an aspect of appearance…[and] some degree of impairment in social relations, social activities, or occupational functioning.17 The Body Image Disturbance Questionnaire (BIDQ) quantifies the extent of body image impairment as a combination of dissatisfaction, distress, and dysfunction.17 In a previous nonclinical study of college students (220 females and 75 males), self-report measures, including the BIDQ, were administered, and the BIDQ demonstrated internal consistency and was free of impression-management response bias.18 The measure converged appropriately with other body image indices and correlated with depression, social anxiety, and eating disturbance.17 Although this supports the use of the BIDQ as a reliable and valid measure of body image disturbance in a nonclinical sample, the instrument had not yet been tested in a clinical population of patients suffering from dermatological disease. Measuring body image disturbance using an instrument such as the BIDQ will better enable physicians to understand and address the needs and concerns of their patients with acne. Furthermore, using the BIDQ as an outcome measure in clinical research will help investigators assess whether a given therapy has a meaningful effect on study patients.
The principal aim of the present study was to validate the BIDQ in a clinical population of patients with acne vulgaris. A second aim was to examine the BIDQ and its correlation with measures of quality of life, specifically Skindex-16. The two tests were expected to show a correlation. However, the psychosocial constructs they measure, although related, are different and are not redundant. A third aim was to examine the hypothesis that patients with more severe acne would experience greater difficulty, citing more physical, social, and emotional impact than others with less severe acne.
Methods
Population and setting. A total of 52 subjects, 39 women and 13 men, with a recent clinical diagnosis of acne vulgaris were recruited to participate in this cross-sectional study. This convenience sample comprised consecutive patients, aged 13 to 54 years, presenting to an outpatient adult or pediatric general dermatology clinic in the summer of 2008. Patients were recruited from one of two settings: Kings County Hospital or Downstate Medical Center. Patient participation was voluntary, and no inducements were offered. Following the physician encounter, the patients were offered the opportunity to participate in the study. Only verbal consent was required based on the authors' institution's Internal Review Board requirements. Given that the only intervention made in this study was the administration of brief questionnaires, the risks associated with enrolling in the study were deemed minimal and verbal consent was recommended. Patients were excluded if they were not fluent in English or were unable to read.
Measures. Demographic questionnaire. For the purposes of this study, the authors created a questionnaire that inquired about demographic variables, including age, sex, and ethnicity.
BIDQ. The standard seven-item BIDQ17 was modified so that the term “defect” was substituted with “skin problem.” This modified version of the BIDQ consisted of the following seven items: 1A) concern about the appearance of your skin (yes or no response) and 1B) what are these concerns (circle all that apply): 1) my acne, 2) my mole(s), 3) my psoriasis, 4) aging skin (wrinkles, sun spots), and 5) other (with a space for patients to write in additional concerns); 2) mental preoccupation with the appearance of your skin (rated from 1=“not at all preoccupied” to 5 =“extremely preoccupied”); 3) experiences of emotional distress over “skin problem” (rated from 1=“no distress” to 5=“extreme and disabling”); 4) impairment in social, occupational, or other important areas of functioning due to skin problem (rated from 1=“no limitation” to 5=“extreme, incapacitating”); 5) interference with social life due to skin problem (rated from 1=“never” to 5=“very often”); 6) interference with schoolwork, job, or ability to function in your role (rated from 1=“never” to 5=“very often”); 7) avoidance of things because of skin problem (rated from 1=“never” to 5=“very often”).
The degree of body image disturbance was evaluated based on a mean of the responses to the scaled questions.2–7 No items were reverse scored, and higher scores reflect greater body image disturbance. Additionally, items 1B, 2, and 5 to 7 ask respondents for an open-ended clarification of responses (e.g., “What effect has your preoccupation with your skin problem had on your life?”).
Objective assessment of acne severity. Prior to onset of the study, the lead author (W.P.B.) trained the medical student (A.K.D.) in lesion identification and counting. Following each physician encounter, the latter investigator recruited subjects and graded their acne, remaining blind to each subject's history and therapeutic plan. Using the lesion count, the Investigator's Static Global Assessment (ISGA) Scale (Table 1) was used to assess acne severity.19 This global scale assesses facial acne on a scale from 0 to 5, ranging from skin that is completely clear (grade 0) to nearly full facial involvement with highly inflammatory lesions (grade 5). Subjects were further subcategorized into three groups based on severity—an ISGA global acne grade of 0 or 1 was considered “none to mild,” a grade of 2 or 3 was categorized as “moderate” acne, and grades 4 and 5 were considered “severe.”
TABLE 1.
Investigator's Static Global Assessment
| GRADE 0 | Normal, clear skin with no evidence of acnevulgaris |
| GRADE 1 | Skin almost clear: rare noninflammatory lesions present, with rare noninflamed papules (papules must be resolving and may be hyperpigmented, though not pink-red) requiring no further treatment in the investigator's opinion |
| GRADE 2 | Some noninflammatory lesions are present, with few inflammatory lesions (papules/pustules only, no nodulocystic lesions) |
| GRADE 3 | Noninflammatory lesions predominate, with multiple inflammatory lesions evident: Several to many comedones and papules/pustules, and there may or may not be one small nodulocystic lesion |
| GRADE 4 | Inflammatory lesions are more apparent: Many comedones and papules/pustules, there may or may not be a few nodulocystic lesions |
| GRADE 5 | Highly inflammatory lesions predominate: Variable number of comedones, many papules/ pustules and nodulocystic lesions |
Skindex-16. The 16-item Skindex-1620 is an instrument that assesses quality of life in patients with skin disease. It is a brief version of the original 29-item Skindex that measures skin symptoms, effects of skin condition on emotions, and effects on physical and/or social functioning. Greater scores for the Skindex-16 indicated that patients felt more bothered by their skin condition, which in turn impacted the three domains of functioning and overall quality of life.20
Multidimensional Body Self-Relations Questionnaire-Appearance Scales (MBSRQ-AS). The MBSRQ-AS (Cash 2004; Body-image assessments: Manuals and questionnaires; available at www.body-images.com) comprises 34 items scored on a 1 to 5 scale and examines attitudinal body image evaluation. This study used two subscales of the MBSRQ— the nine-item Body Areas Satisfaction Scale (BASS) to assess dissatisfaction-satisfaction with particular body areas or aspects of body areas (e.g., face, hair color, lower torso) and the seven-item Appearance Evaluation (AE) to evaluate feelings of physical attractiveness or unattractiveness, measuring overall body image. A greater score on the MBSRQ-BASS indicated that the patient was more satisfied with particular aspects of his/her body and/or overall appearance.21
The Center for Epidemiologic Studies Depression Scale (CES-D). The CES-D22 is a 20-item measure that assesses depressive symptomatology in the general population in the past week using a 0 to 3 scale.22
Fear of Negative Evaluation Scale (FNE). The FNE23 is a 12-item measure that uses a 1 to 5 scale to assess aspects of social-evaluative anxiety, such as distress, avoidance, and expectations. Fear of negative evaluation involves social anxiety, being overly concerned with others' opinions, hiding from the negative feelings of their unfavorable impressions, and avoiding situations where there is potential evaluation.23
Statistical analyses. Means (±SD) and/or frequencies were used to describe baseline demographic variables. Due to the modifications the authors made to the BIDQ, they wanted to ensure that the modified version was still reliable and valid, and therefore included some other measures (MBSRQ, FNE, CES-D) to assess concurrent validity. To assess the validity of the BIDQ, Pearson correlation coefficients were used to measure correlations between the BIDQ and the series of established measures of body image and psychosocial functioning (MBSRQ-BASS, MBSRQ-AE, FNE, and the CES-D).
Poorer body image may be correlated with dissatisfaction with appearance and specific aspects of appearance, depression, and greater fear of negative evaluation, which was assessed by measuring Pearson correlation coefficients between the BIDQ and established measures of body image and psychosocial functioning (MBSRQ-BASS, MBSRQ-AE, CES-D and FNE, respectively). Poorer body image and poorer quality of life might also be correlated, which was assessed by determining the Pearson correlation coefficient between the BIDQ and Skindex-16. Internal consistency was measured by determining Cronbach's alpha for the seven-item BIDQ. Finally, open-ended responses were coded and reported as simple percentages based on acne severity.
Results
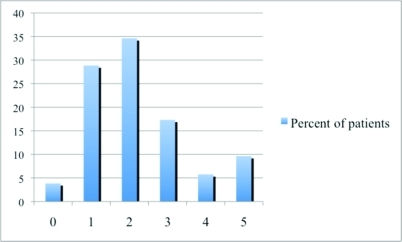
Of the 57 patients approached to participate in the study, five (8.7%) refused to participate. A total of 52 patients with acne (75% female) presenting for dermatological treatment participated in the study. As shown in Table 2, the mean age of all patients was 23.8 years (SD=9.3; median=21.5). Based on global assessment, 3.85 percent of patients had an ISGA score of zero; 28.85 percent of patients had a score of one; 34.15 percent had a score of two; 17.31 percent of patients had a score of three; 5.77 percent had a score of four; and 9.62 percent of patients had a score of five (Figure 1).
TABLE 2.
Baseline characteristics of patients with acne vulgaris
| TOTAL STUDY PATIENTS | 52 |
| Male | 13 (25%) |
| Female | 39 (75%) |
| MEAN AGE, Y (SD) | 23.8 (9.3) |
| ETHNICITY | |
| Black or African American | 34 (65.38%) |
| Caucasian | 14 (26.92%) |
| Hispanic or Latino origin | 4 (7.69%) |
| Asian or Pacific Islander | 3 (5.77%) |
| American Indian or Alaskan Native |
0 (0%) |
Figure 1.
Percent of patients based on acne severity
Measures. The mean score of Skindex-16 was 40.33±24.323. The mean scores of the MBSRQ-BASS and AE were 3.56±0.831 and 3.58±0.933, respectively. The mean score of the CES-D was 15.37±10.622 and the mean score of the FNE measure was 34.10±9.900.
Internal consistency and results of the BIDQ. The internal consistency of the BIDQ was demonstrated with a Cronbach alpha of 0.920. BIDQ scores of the entire sample averaged 2.49 and ranged from 1.0 to 5.0 (SD=1.08)
Construct validity. Pearson correlation coefficients between the BIDQ scores and the MBSRQ-BASS and MBSRQ-AE scores were measured to evaluate construct validity. Table 3 provides the Pearson correlation coefficients between the BIDQ and known measures of body image (MBSRQ-BASS and MBSRQ-AE). The Pearson correlation coefficients were −0.354 and −0.369, with p values of .010 and .007, respectively.
TABLE 3.
Correlations of the BIDQ with measures of body image and psychosocial functioning
| VARIABLE | PEARSON CORRELATION COEFFICIENT | P VALUE |
|---|---|---|
| Body image evaluation/affect Body Areas Satisfaction Scale Appearance Evaluation |
−.354 −.369 |
.010* .007* |
| Social-evaluative anxiety | .231 | .099 |
| Psychosocial functioning Depression | .390 | .004* |
| Quality of Life measure Skindex | 0.562 | .000* |
p = 0.01
Convergent validity. People with body image disturbance should also report greater fear of negative evaluation and greater levels of depression.17 Convergent validity of the BIDQ was measured by calculating the Pearson correlation coefficient between the BIDQ and CES-D (0.390; p = 0.004) (Table 3) and confirmed the expected relationship between depression and body image disturbance. Subjects with greater body image disturbance reported greater FNE (Pearson correlation coefficient=0.231 [Table 3]), although this trend did not reach statistical significance (p = 0.099).
Body image and quality of life. BIDQ scores also significantly correlated with Skindex-16 scores such that greater body image disturbance related to acne was associated with a poorer quality of life (Pearson correlation coefficient=0.562; p = 0.000 [Table 3]).
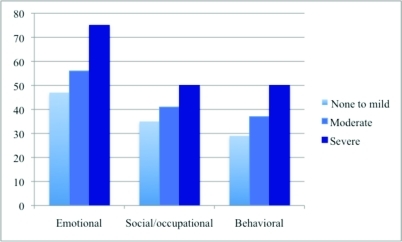
Qualitative findings. Each of the hand-written responses that subjects provided to the BIDQ's open-ended questions was coded as representing an emotional, social/occupational, and/or behavioral response to that subject's acne. In addition, one response could be categorized in more than one category. Among patients with no to mild acne, 47 percent experienced an emotional impact due to their acne, 35 percent experienced a social/occupational impact, and 29 percent modified their behavior as a result of their acne. Among patients with moderate acne, 56 percent experienced an emotional impact due to their acne, 41 percent experienced a social/occupational impact, and 37 percent modified their behavior as a result of their acne. Among patients with severe acne, 75 percent experienced an emotional impact due to their acne, 50 percent experienced a social/occupational impact, and 50 percent modified their behavior as a result of their acne. Furthermore, as acne severity increased, the frequency of all three types of responses to the open-ended questions increased (Figure 2).
Figure 2.
BIDQ qualitative findings
Representative examples of responses to open-ended questions were summarized in Table 4. The left hand column includes less extreme examples and behavioral modifications reported by subjects. The right hand column includes more extreme examples of each of the three categories. Demographic characteristics (age, sex, acne grade) of each respondent were included after each open-ended response. The specific examples illustrate the spectrum of psychosocial repercussions.
TABLE 4.
Qualitative data: Open-ended responses
| EMOTIONAL DISTRESS | |
|---|---|
| LESS EXTREME (AGE, SEX, ACNE GRADE) | MORE EXTREME (AGE, SEX, ACNE GRADE) |
| “I've just been more self-conscious.” (29, F, acne grade 1) “I simply pay more attention at who notices my acne.” (24, F, acne grade 0) “It doesn't really bother me but I seethe acne and feel it. Like I'll stop and think about it.” (18, M, acne grade 3) |
“I used to cry… people would say things to me. Once a woman told me to go to a church where they would ‘purify me.’ It made life very difficult.” (22, F, acne grade 1) “At times it makes me feel sad, embarrassed, ugly, discriminated against, insecure.” (27, F, acne grade 5) “Anger, loss of interest” (20, M, acne grade 3) |
| SOCIAL/OCCUPATIONAL REPERCUSSIONS | |
| LESS EXTREME (AGE, SEX, ACNE GRADE) | MORE EXTREME (AGE, SEX, ACNE GRADE) |
| “I don't like going to the beach much.” (16, M, acne grade 1) “Apprehensive about going out when I have acne breakouts.” (28, F, acne grade 2) “At times when we had meetings, I would shy away from giving presentations.” (35, F, acne grade 3) “While in school, I try to cover my outbreaks whenever possible, distracting me occasionally from my school task.” (16, M, acne grade 3) |
“I don't leave my house to go anywhere as often as I use to.” (43, F, acne grade 2) “I'll avoid talking to people on a day where my skin looks really bad.” (15, F, acne grade 1) “I do not go out to social events at all.” (27, F, acne grade 5) “I avoid anything that meant I wouldn't be able to wear makeup. I definitely felt like my face looked ugly… I felt like I had a disease on my face.” (22, F, acne grade 1) |
| BEHAVIORAL MODIFICATIONS | |
| LESS EXTREME (AGE, SEX, ACNE GRADE) | MORE EXTREME (AGE, SEX, ACNE GRADE) |
| “I always try to keep my hands washed and clean.” (17, M, acne grade 2) “I avoid certain foods (like ice cream).” (24, F, acne grade 4) |
“I feel the need to cover my skin a lot, hide my face if I can.” (18, F, acne grade 4) “I stopped looking in the mirror for awhile.” (25, F, acne grade 3) “Wear hats all the time.” (30, M, acne grade 1) |
Discussion
The current study provides evidence supporting the validity and internal consistency of the BIDQ for use among acne patients. The BIDQ converged appropriately with other body image indices. BIDQ scores also correlated with Skindex-16 scores, confirming that quality of life and body image are related psychosocial constructs. Based on these results, the BIDQ appears to be an accurate instrument that can be used to assess appearance-related concern and impairment in patients with acne vulgaris.
The BIDQ is a comprehensive yet brief self-report instrument designed to measure body image disturbance. This instrument was initially developed by revising the items of a clinical screening instrument, the Body Dysmorphic Disorder Questionnaire (BDDQ), to permit continuous scoring.24 A dermatology-specific version of the BDDQ, the Body Dysmorphic Disorder Questionnaire–Dermatology Version was recently used to assess appearance concerns and their impact on functioning in daily life among acne patients.8 Of those patients who had clinically significant acne on exam, and thereby could not meet criteria for a diagnosis of BDD, almost half reported levels of preoccupation, distress, and impairment commensurate with patients who have BDD.8 Given this high level of body image disturbance among acne patients who have clinically evident acne on exam, it became obvious that a tool was needed to gauge these symptoms among all acne patients. A more appropriate tool to assess body image disturbance among all patients, crossing the full spectrum of disease severity, is the BIDQ.
In the current study, the BIDQ correlated with established measures of body image (the MBSRQ-BASS and MBSRQ-AE), demonstrating that the BIDQ measures what it is meant to measure, and therefore possesses construct validity. To assess convergent validity, BIDQ scores were compared to other measures with which body image disturbance would be expected to correlate. First, subjects who suffer from body image disturbance are likely to also suffer from depressed mood. As suspected, the BIDQ correlated with the CES-D, a measure of depressed mood. It was suspected that subjects who suffered from body image disturbance would also report greater FNE. Although this trend was evident, it did not reach statistical significance.
The authors had hypothesized that quality of life and body image disturbance would be correlated. Poor body image may result in depression, social anxiety and inhibition, and poor self-esteem, illustrating the impact of body image perception on quality of life.25–27 As expected, scores from the BIDQ and Skindex-16 correlated, reaching a very high statistical significance (p = 0.000).
Qualitative investigations provide a more detailed view into the ways that acne impacts the lives of patients. Written testimonials provided by subjects in this study complemented and corroborated the numeric responses. In the subjects studied, acne appears to induce substantial emotional distress, while also having social, occupational, and behavioral repercussions. Furthermore, regardless of the severity of acne, subjects were most likely to provide examples of emotional distress. This is consistent with findings of a prior study in which dermatology patients (not just acne patients) were asked the ways in which their skin bothered them the most and 65 percent of these mentions pertained to “emotions,” most commonly being worry and concern about appearance.20
Interestingly, among the patients with a clinical diagnosis of acne who at the time of their visit had no to mild acne, almost half reported emotional impacts as a result of their acne, approximately one-third experienced a social/ occupational impact, and nearly 30 percent reported behavioral modification as a result of their acne. This demonstrates the significant impact of acne in all three domains even among patients with no to mild disease.
This study has several limitations. First, the sample size is small and the study population does not necessarily reflect all patients with acne. More than a majority of patients were female and as such, more information is needed about male patients. Although this study was not designed to measure a correlation between acne severity and BIDQ score, a larger study would allow for such investigation. Furthermore, the cross-sectional design of this study did not permit for an assessment of test-retest reliability of the BIDQ. It would be interesting to see whether the BIDQ reflects changes in acne severity over time. However, the BIDQ was found to have good test-re-test reliability in a nonclinical population.18 A prospective study in which BIDQ scores were measured throughout a course of acne therapy would help determine whether the scale does indeed reflect such changes in disease severity, and would also assess whether subjects who suffer from greater body image disturbance are more likely to comply with a prescribed therapeutic regimen.
Psychosocial measures, such as the BIDQ, will enhance our understanding of the impact of acne and capture treatment outcomes from patient perspectives. Such measures may facilitate the tailoring of specific treatments to best correspond with the goals of the patient and the physician. Just as importantly, the BIDQ may help to identify patients who may benefit from dermatological treatment modalities in conjunction with psychiatric medication and/or counseling.
References
- 1.Pawin H, Chivot M, Beylot C, et al. Living with acne. A study of adolescents' personal experiences. Dermatology. 2007;215:308–314. doi: 10.1159/000107624. [DOI] [PubMed] [Google Scholar]
- 2.Collier C, Harper JC, Cafardi JA, et al. The prevalence of acne in adults 20 years and older. JAmAcad Dermatol. 2008;58:56–59. doi: 10.1016/j.jaad.2007.06.045. [DOI] [PubMed] [Google Scholar]
- 3.Baldwin HE. The interaction between acne vulgaris and the psyche. Cutis. 2002;70:133–139. [PubMed] [Google Scholar]
- 4.Cotterill JA, Cunliffe WJ. Suicide in dermatological patients. BrJ Dermatol. 1997;137:246–250. doi: 10.1046/j.1365-2133.1997.18131897.x. [DOI] [PubMed] [Google Scholar]
- 5.Gupta MA, Gupta AK. Depression and suicidal ideation in dermatology patients with acne, alopecia areata, atopic dermatitis, and psoriasis. Br J Dermatol. 1998;139:846–850. doi: 10.1046/j.1365-2133.1998.02511.x. [DOI] [PubMed] [Google Scholar]
- 6.Koblenzer CS. Psychodermatology of women. Clin Dermatol. 1997;15:127–141. doi: 10.1016/s0738-081x(96)00115-0. [DOI] [PubMed] [Google Scholar]
- 7.American Psychiatric Association. 4th ed. Washington D.C.: American Psychiatric Association; 2000. Diagnostic and statistical manual of mental disorders. [Google Scholar]
- 8.Bowe WP, Leyden JJ, Crerand CE, et al. Body dysmorphic disorder symptoms among patients with acne vulgaris. J Am Acad Dermatol. 2007;57:222–230. doi: 10.1016/j.jaad.2007.03.030. [DOI] [PubMed] [Google Scholar]
- 9.Mackley CL. Body dysmorphic disorder. Dermatol Surg. 2005;31:553–558. doi: 10.1111/j.1524-4725.2005.31160. [DOI] [PubMed] [Google Scholar]
- 10.Crerand CE, Phillips KA, Menard W, Fay C. Nonpsychiatric medical treatment of body dysmorphic disorder. Psychosomatics. 2005;46:549–555. doi: 10.1176/appi.psy.46.6.549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sarwer DB. Awareness and identification of body dysmorphic disorder by aesthetic surgeons: results of a survey of American Society for Aesthetic Plastic Surgery members. Aesthetic Surg J. 2002;22:531–535. doi: 10.1067/maj.2002.129451. [DOI] [PubMed] [Google Scholar]
- 12.Phillips KA. Body dysmorphic disorder: the distress of imagined ugliness. Am J Psychiatry. 1991;148:1139–1149. doi: 10.1176/ajp.148.9.1138. [DOI] [PubMed] [Google Scholar]
- 13.Phillips KA. The Broken Mirror: Understanding and Treating Body Dysmorphic Disorder. New York: Oxford University Press; 1996. [Google Scholar]
- 14.Phillips KA, McElroy SL, Keck PE, Jr, et al. Body dysmorphic disorder: 30 cases of imagined ugliness. Am J Psychiatry. 1993;150:302–308. doi: 10.1176/ajp.150.2.302. [DOI] [PubMed] [Google Scholar]
- 15.Sarwer DB, Crerand CE, Gibbons LM. The Art of Aesthetic Surgery: Principles and Techniques. St. Louis: Quality Medical Publishing; 2006. [Google Scholar]
- 16.Veale D, Boocock A, Gournay K, et al. Body dysmorphic disorder: a survey of fifty cases. Br J Psychiatry. 1996;169:196–201. doi: 10.1192/bjp.169.2.196. [DOI] [PubMed] [Google Scholar]
- 17.Cash T, Phillips K, Santos M, Hrabosky J. Measuring “negative body image”: validation of the Body Image Disturbance Questionnaire in a nonclinical population. Body Image. 2004;1:363–372. [Google Scholar]
- 18.Cash T, Grasso K. The norms and stability of new measures of the multidimensional body image construct. Body Image. 2005;2:199–203. doi: 10.1016/j.bodyim.2005.03.007. [DOI] [PubMed] [Google Scholar]
- 19.Shalita AR, Myers JA, Krochmal L, et al. The safety and efficacy of clindamycin phosphate foam 1% versus clindamycin phosphate topical gel 1% for the treatment of acne vulgaris. J Drugs Dermatol. 2005;4:48–56. [PubMed] [Google Scholar]
- 20.Chren MM, Lasek RJ, Sahay AP, Sands LP. Measurement properties of Skindex-16: a brief quality-of-life measure for patients with skin diseases. J Cutaneous Med Surg. 2001;5:105–110. doi: 10.1007/BF02737863. [DOI] [PubMed] [Google Scholar]
- 21.Brown TA, Cash TF, Mikulka PJ. Attitudinal body image assessment: factor analysis of the Body-Self Relations Questionnaire. J Pers Assess. 1990;55:135–144. doi: 10.1080/00223891.1990.9674053. [DOI] [PubMed] [Google Scholar]
- 22.Radloff L. The CES-D Scale: a self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- 23.Leary M. A brief version of the fear of negative evaluation scale. Personality and Social Psychology Bulletin. 1983;9:371–376. [Google Scholar]
- 24.Dufresne R, Phillips KA, Vittorio CC, Wilkel CS. A screening questionnaire for body dysmorphic disorder in a cosmetic dermatologic surgery practice. Dermatol Surg. 2001;27:457–462. doi: 10.1046/j.1524-4725.2001.00190.x. [DOI] [PubMed] [Google Scholar]
- 25.Noles S, Cash TF, Winstead BA. Body image, physical attractiveness, and depression. J Consult Clin Psychol. 1985;53:88–94. doi: 10.1037//0022-006x.53.1.88. [DOI] [PubMed] [Google Scholar]
- 26.Cash T, Fleming EC. The impact of body image experiences: development of the body image quality of life inventory. Int J EatDisord. 2002;31:455–460. doi: 10.1002/eat.10033. [DOI] [PubMed] [Google Scholar]
- 27.Powell M, Hendricks B. Body schema, gender, and other correlates in nonclinical populations. Genet Soc Gen Psychol Monogr. 1999;125:333–412. [PubMed] [Google Scholar]