Abstract
Liposuction is one of the most popular treatment modalities in aesthetic surgery with certain unique anaesthetic considerations. Liposuction is often performed as an office procedure. There are four main types of liposuction techniques based on the volume of infiltration or wetting solution injected, viz dry, wet, superwet, and tumescent technique. The tumescent technique is one of the most common liposuction techniques in which large volumes of dilute local anaesthetic (wetting solution) are injected into the fat to facilitate anaesthesia and decrease blood loss. The amount of lignocaine injected may be very large, approximately 35-55 mg/kg, raising concerns regarding local anaesthetic toxicity. Liposuction can be of two types according to the volume of solution aspirated: High volume (>4,000 ml aspirated) or low volume (<4,000 ml aspirated). While small volume liposuction may be done under local/monitored anaesthesia care, large-volume liposuction requires general anaesthesia. As a large volume of wetting solution is injected into the subcutaneous tissue, the intraoperative fluid management has to be carefully titrated along with haemodynamic monitoring and temperature control. Assessment of blood loss is difficult, as it is mixed with the aspirated fat. Since most obese patients opt for liposuction as a quick method to lose weight, all concerns related to obesity need to be addressed in a preoperative evaluation.
Keywords: Lignocaine, liposuction, tumescent, wetting solution
INTRODUCTION
Increased awareness about cosmetic surgery has made liposuction a popular plastic surgical operation. Liposuction is defined as removal of fat from deposits beneath the skin using a cannula with the assistance of a powerful vacuum. In the US, more than 341,000 liposuction procedures were performed in 2008.[1] However, there have been reports of adverse outcomes,[2–4] so the anaesthesiologist should understand the pathophysiology of obesity and fluid management during liposuction and be aware of the complications. In India, though the figures are not available but the popularity of this procedure is on the rise. In our hospital, a variety of liposuction procedures are being conducted on a regular basis, which vary from small volume liposuction of the arms to very large volume liposuction procedures of the abdomen and thighs [Figure 1]. A total of 273 liposuction procedures have been performed at our institution from 2008-2010 (3 years).
Figure 1.

Liposuction of abdomen and thighs
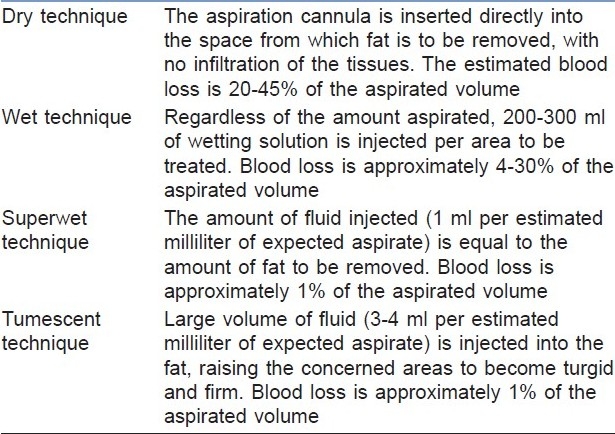
Four types of liposuction techniques have been described based on the volume of infiltration or wetting solution injected, viz dry, wet, superwet, and tumescent technique [Table 1]. The main difference between these techniques is the amount of infiltration done into the tissues and the resultant blood loss as a percentage of aspirated fluid. The tumescent technique is the most common of all liposuction techniques.
Table 1.
Types of liposuction techniques
HISTORICAL BACKGROUND
Liposuction was initiated in the 1970s in Italy. Here, fat removal was carried out with a blunt curette. This technique was modified in 1977 by a French surgeon, Yves Gerard Illouz, who added hyaluronidase and saline to emulsify the fatty tissue, and hence facilitate aspiration with the use of liposuction cannula. This was termed the ‘wet technique’ and was introduced to reduce blood loss during the procedure.[5–7]
However, it was Jeffery Klein (a dermatologist in the US) who described the ‘tumescent technique’ of liposuction in the mid-1980s, which is associated with decreased blood loss, thus making it possible to perform liposuction as a day care procedure.[8]
Tumescent technique
Klein coined the term ‘tumescent technique’. The word tumescence means ‘to swell’. In this technique, very large volumes of dilute local anaesthetic along with additives like epinephrine and sodium bicarbonate, are injected into the subcutaneous tissue to expand the tissues and make them firm, swollen, and turgid, i.e., the final endpoint of strong tissue turgor. This creates a plane from where suction of fat becomes easier, with lesser blood loss.[9]
Liposuction can be of two types: High volume (>4,000 ml aspirated) or low volume (<4,000 ml aspirated) according to the volume of aspiration carried out. Since there is potential for large fluid shifts secondary to the volume of tissue removed, with a risk of developing pulmonary oedema, high-volume liposuction is considered to be significantly more prone to complications than the original form of tumescent liposuction. Therefore, intravenous fluids should be used with extreme caution in high-volume liposuction procedures.[10–12]
Wetting solutions
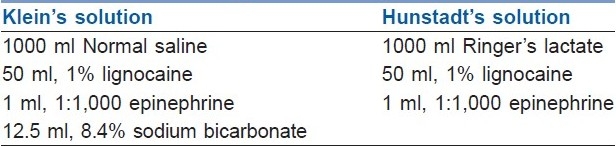
The most common wetting solutions are those proposed by Klein[8] and Hunstad[13] [Table 2]. Various constituents of wetting solutions are as follows–
Table 2.
Types of wetting solution
Crystalloid solutions
In the tumescent solution, originally described by Klein, the local anaesthetic is diluted in 0.9% isotonic saline.[8] While isotonic saline as a diluent is associated with burning sensation upon injection, lactated Ringer's solution does not cause any burning sensation on injection and also reduces the sodium load. In our hospital, lactated Ringer's solution is used for dilution of the local anaesthetic.
Local anaesthetics
Lignocaine is the most commonly used local anaesthetic in tumescent solutions, the maximum dose of which along with adrenaline is considered to be 7 mg/kg. With the advent of tumescent anaesthesia, the maximum dose of lignocaine, when delivered in a tumescent solution may be significantly larger.[13–15] The recommended maximum dose of lignocaine is 55 mg/kg for most patients, with a range of 35-55 mg/kg in patients undergoing liposuction.[9,16] The concentration of lignocaine varies according to the vascularity of the area where liposuction is to be performed. In the more vascular or sensitive areas such as the breast and abdomen, the dose can be increased to 1,500 mg/L of normal saline.[17] The concentration is decreased to 500 mg/L of normal saline in less sensitive areas such as the thighs. Louis Habbema[18] has reported in a series of 3,430 liposuction procedures that a maximum lignocaine concentration of 500 mg/L of normal saline solution allows infusion of a large volume of wetting solution, without any risk of lignocaine toxicity.
The pharmacokinetics of tumescent lignocaine is studied by measuring the concentration of lignocaine in the blood and how this concentration changes over time. The toxicity of local anaesthetic is a function of its peak plasma concentration, which, in turn, depends on several factors including the total milligram per kilogram dose and the rate of systemic absorption and elimination. Peak levels of lignocaine and its active metabolite monoethylglycinexylidide occur in 8-32 hours after initial infiltration, but are well below the toxic concentration of 6 mg/L.[19–21]
Any factor that slows the rate of lignocaine absorption will reduce the peak lignocaine plasma level, and thus reduce the risk of lignocaine toxicity and permit larger doses of lignocaine to be used. These factors are subcutaneous fat, which has a relatively low volume of blood flow, dilute epinephrine, which produces a prolonged and profound degree of vasoconstriction and lignocaine itself, which is lipophilic and readily sequestered in fat cells.[22,23]
Lignocaine is cleared from the body by diethylation in the liver by 1A2 and 3A4 isoenzyme groups of the cytochrome (cyt) p450 families.[11] Drugs that inhibit 3A4 and cyt P450 system have the potential to affect the metabolism of lignocaine.[23] Hence, the dose of lignocaine needs to be reduced in patients who use medications that interfere with cytP450 system or patients on medications that effect hepatic blood flow. Monoethylglycinexylidide is a major active metabolite of lignocaine, which is similar in activity to the parent compound and can cause seizures at elevated levels. Approximately 10% of lignocaine is excreted unchanged in the urine.
Prilocaine and Articaine have also been used in tumescent solutions. Tumescent solution with prilocaine has not been associated with elevated plasma prilocaine levels or methemoglobinemia.[24,25]
Vasoconstrictors
Vasoconstrictors reduce blood circulation in the tissues, and thus delay the absorption of local anaesthetics. Adrenaline is the most commonly used vasoconstrictor, the recommended concentration in tumescent solution is 0.25-1 mg/L depending on the tissue vascularity. In the more vascular tissues, the concentration is 1 mg/L and is decreased to 0.5 mg/L in the less vascular areas of the body. The dose should not exceed 50μg/kg. If the maximum dose is anticipated to exceed, the procedure should be done in several stages.[8,26,27] Lalinde et al. used l-ornithine 8-vasopressin, instead of epinephrine, at a concentration of 0.01 IU/ml in chilled saline and concluded that blood loss with this technique was less than with conventional epinephrine.[28]
Buffers
Sodium bicarbonate is added to decrease the burning sensation associated with injection of the tumescent solution. Adding bicarbonate raises the pH of the solution, which increases the proportion of nonionized lipid soluble lignocaine, leading to a more rapid entry into the nerve cells.[29]
Anti-inflammatory additives
Steroids have a beneficial effect when added to the tumescent solution because of their anti-inflammatory effects and also their stabilizing action on the circulatory system.[8]
PHYSIOLOGICAL CHANGES DURING LIPOSUCTION
Hemodynamics
While small-volume liposuction may not be associated with major hemodynamic changes, it is the large-volume liposuction that results in alteration of hemodynamics.
Large-volume liposuction involves removal of more than 4 L (approximately 4 kg) of fat and fluid [Figure 2]. An increase in cardiac index, heart rate, mean pulmonary arterial pressure, stroke volume index, and right ventricular stroke work index, along with a decrease in mean arterial pressure and systemic vascular index has been observed during large-volume liposuction.[30]
Figure 2.

Lipoaspirate containing fat and fluid
Epinephrine, which is used in large doses routinely during liposuction, may be responsible for tachycardia and increased cardiac index.[31,32] The fall in mean arterial pressure and systemic vascular resistance is probably due to the effects of general anaesthesia and opioids used intraoperatively.[33] A reduced peripheral vascular resistance may also result due to the dominant action of epinephrine on β2 receptors of the vessels in skeletal muscle where blood flow increases.[34]
Thermoregulation
There is an increased risk of hypothermia in patients undergoing large volume liposuction.[30] Exposure of large body surface areas, infusion of large volumes of cold wetting solutions, long duration of procedure, general anaesthesia, heat loss during mechanical ventilation, ambient room temperature, and intravenous fluids all contribute to hypothermia in these patients. Complications like cardiac dysrhythmias, coagulopathies, oliguria, and electrolyte imbalance are worsened by hypothermia.
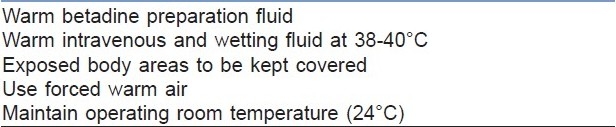
Both, the hemodynamic and thermoregulatory changes may persist for more than 24 hours after beginning of surgery.[33,34] Measures to prevent intraoperative hypothermia are listed in [Table 3].
Table 3.
Measures to prevent hypothermia
Preoperative assessment
A thorough preoperative assessment and optimization is essential since many obese patients opting for liposuction may be having other comorbidities like hypertension, diabetes mellitus (DM), coronary artery disease (CAD), deep vein thrombosis (DVT), and obstructive sleep apnea (OSA). Liposuction is contraindicated in patients with severe cardiovascular disease, coagulation disorder, and during pregnancy.[9]
A thorough history regarding use of all medications, vitamins, herbs, and anticoagulants should be documented, as they may affect blood clotting.[35] Most of these drugs should be stopped at least 2 weeks before surgery. Any medication that interferes with metabolism of lignocaine such as statins and calcium channel blockers should be either discontinued before liposuction, or the total dosage of lignocaine should be reduced.[8,9,23]
Preoperative investigations include a complete blood count with quantitative platelet assessment, prothrombin time, partial thromboplastin time, liver function tests, and pregnancy test for women of childbearing age.[36]
Premedication
The patients may be prescribed an anxiolytic, e.g., 0.25-0.5 mg alprazolam the night before and on the morning of surgery. Preoperative medication diminishes anxiety and the hemodynamic changes, e.g., tachycardia, hypertension, and arrhythmias associated with liposuction.[36] Clonidine, an a2 receptor agonist, is gaining popularity as a premedicant due to its sedative, anxiolytic, sympatholytic, and antisialagogue actions. The recommended oral dose of clonidine is 2-5 μg/kg.[37]
Perioperative thromboprophylaxis with low molecular weight heparin (LMWH) is essential in obese patients.[38]
Informed consent
An informed consent regarding the surgical procedure and anaesthesia technique is necessary.
ANAESTHESIA TECHNIQUE
Liposuction may be performed under local, regional, or general anaesthesia. No single anaesthesia technique has been proven to be superior over another. The technique of anaesthesia depends on both, the site and extent of liposuction and also patient preference. The anaesthetic technique will vary according to the areas being operated upon; arms, thighs, abdomen, or buttocks and the volume of liposuction being performed. Since these procedures are often performed as day care, it is important that there is fast recovery of psychomotor and cognitive functions ensuring early discharge of the patients.
Monitored anaesthesia care
This is a useful technique for small volume liposuction. Infiltration with vasoconstrictor and local anaesthetic reduces bleeding and provides intraoperative analgesia, respectively. Thus, it allows liposuction to be performed under light sedation, implying a short recovery time, earlier discharge, and low cost to the patient. However, if infiltration is not uniform, some areas will have a lack of analgesia, thus requiring more sedation.[14,15]
Sedation with midazolam (1-3 mg) and analgesia with fentanyl (25-50 mg) or remifentanil (12.5-25 mg) is commonly employed for small volume liposuction. Propofol (0.5-1 mg/kg) may be given intermittently for monitored anaesthesia care. Ketamine in low doses (0.25-0.5 mg/kg) along with midazolam decreases significantly the consumption of opioids in the intraoperative period and of analgesics in the postoperative period. Clonidine 2-5 mg/kg, is also a useful adjuvant in sedation techniques.[37,39,40]
Lumbar epidural anaesthesia
This is widely used to provide analgesia in abdominal liposuction. The quality of analgesia provided is superior to that provided by local infiltration. However, an extensive epidural blockade is frequently associated with hypotension and must be limited to patients with good cardiac reserve.[41]
Subarachnoid block
This is a useful technique for liposuction below the umbilical area. In these conditions, this technique is safe, low cost, and with few side effects. The quality of anaesthesia and muscular relaxation is excellent and administration of opioids in the subarachnoid space provides good analgesia in the first 24 hours of the postoperative period.[37]
General anaesthesia
This is recommended for large volume liposuction or if the patient desires it. Propofol is the induction agent of choice because of its pharmacokinetic profile and inherent antiemetic property, which ensures early recovery of the patient.[38] Airway can be maintained with a supraglottic device laryngeal mask airway, proseal LMA (PLMA) or I-gel. Muscle relaxation may be achieved with a nondepolarizing drug – atracurium, rocuronium, or vecuronium. Analgesia is provided by short-acting opioids such as fentanyl or remifentanil and infiltration of lignocaine in the subcutaneous tissue.[1,37]
Patient positioning
The usual position for surgery is supine. However, the position varies according to the area to be operated upon. Liposuction of buttocks and back of the thighs requires prone position.
Appropriate precautions should be taken to prevent pressure injuries by carefully padding the sensitive pressure points – face, breasts, iliac crest, and knees in the prone position, and elbows and heels in the supine position.
Care should be taken to avoid pressure on the brachial plexus and ulnar nerve. Protection of eyes with lubrication and padding and placing the head on a Gel Horseshoe Headrest is essential. Pneumatic compression devices are used for large-volume liposuction and for procedures lasting more than an hour, to prevents deep vein thrombosis (DVT).[18]
Monitoring
For small volume liposuction, standard ASA monitoring such as oxygen saturation (SpO2), noninvasive blood pressure (NIBP), end-tidal carbon dioxide (EtCO2,), electrocardiogram (ECG), and temperature monitoring suffice. Invasive monitoring such as central venous pressure and arterial blood pressure are required for large volume liposuction.[37] Monitoring hourly urine output is important to indicate the fluid homeostasis in the body. Grazer et al. have recommended overnight continuous monitoring in patients undergoing large volume liposuction.[42]
Intraoperative fluid administration
The intraoperative fluid maintenance in these patients is different from other surgeries. The aim of intravenous fluid administration is to replace the preoperative deficit and provide maintenance fluid. In these procedures after induction of anaesthesia, wetting solution is injected into the areas where liposuction is to be done. The total fluids received by the patient include intravenous fluids and the volume of wetting solution injected. The output includes the urine output and the aspirated fluid which includes fat, blood, and a portion of wetting solution. The difference between the fluid input and output is the residual volume that remains in the patient.
The majority of this residual volume comprises of wetting solution, which remains in the extravascular compartment. This fluid, which acts like an interstitial infusion, slowly gets absorbed into the intravascular compartment.[43,44] Thus, any excess fluid administered can easily produce fluid overload, which is an important cause for morbidity in these patients.[43]
In 1996, Trott et al. suggested guidelines for intraoperative fluid resuscitation. Patients having less than 4,000 ml of lipoaspirate removed received maintenance fluid only, whereas those having more than 4,000 ml of lipoaspirate removed received maintenance plus 0.25 ml of intravenous fluid for each milliliter aspirated over 4,000 ml. The intraoperative fluid volume ratio (volume of intravenous fluid plus infiltration solution divided by aspirate volume) was 2.1 for small-volume liposuction (<4,000 ml) and 1.4 for large volume liposuction (>4,000 ml). With this fluid management strategy, the patients appeared to be slightly overhydrated.[45]
To limit the degree of fluid overloading and possibility of pulmonary edema, Rohrich et al. modified the replacement fluid delivery at 0.25 ml of intravenous fluid for each milliliter aspirated over 5,000 ml. The intraoperative fluid volume ratio with this modification was 1.8 for small-volume aspirates (<5,000 ml) and 1.2 for large-volume aspirates (>5,000 ml).[46]
POSTOPERATIVE CARE
Monitoring should continue in the postoperative period for large-volume liposuction.
Pain relief
Since pre-emptive analgesia is provided by the local anaesthetic in tumescent liposuction, the requirement of analgesics in the intraoperative and postoperative period is minimal. By adding epinephrine to lignocaine, the duration of analgesia obtained from tumescent lignocaine can be extended by many hours. Non Steroidal Anti-inflammatory Drugs (NSAIDs) may also be prescribed for postoperative pain relief.
Early ambulation
Patients are asked to begin ambulation as soon as possible and lower extremity muscle-contracting exercises are to be encouraged, while they are in bed to minimize the risk of DVT and pulmonary embolus.
Complications
Liposuction, although done very often as a day care procedure has been associated with potential major complications, including a fatal outcome [Table 4]. The incidence and severity of complications depends on the setup where it is performed and more often when large volume liposuction is performed under general anaesthesia or combined with other major procedures like abdominoplasty.[47] The incidence is highest when performed in a physician's office setting followed by ambulatory surgery centers and least in the hospital operating rooms.[48–50] The incidence of mortality associated with liposuction is reported 0.003-0.02%.[48,49]
Table 4.
Complications following liposuction
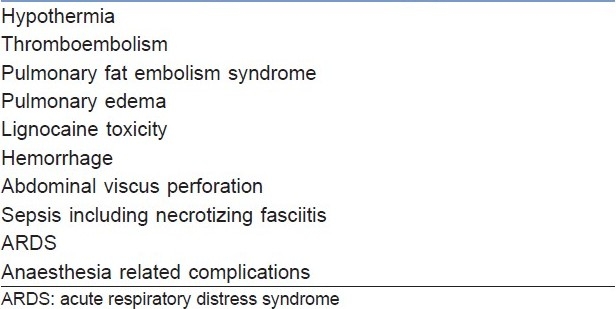
However, in a study by Hanke et al., no hospitalization and no blood transfusion was required in 15,336 cases of liposuction done under local anaesthesia using tumescent technique.[4]
The causes of death reported following liposuction have been cardiac arrest due to fluid overload, pulmonary edema, lignocaine toxicity, fat embolism, and acute respiratory distress syndrome (ARDS).
It is believed that all patients undergoing liposuction surgery experience a thromboembolic shower due to fat particles being dislodged during surgery,[51] resulting in pulmonary fat embolism syndrome.
Pulmonary edema and overhydration have been attributed to absorption of the tumescent solution from subcutaneous to the intravascular compartment. This is most often seen with large-volume liposuction. Postmortem records of post liposuction deaths have evidence of weight gain of several kilograms, resulting in overhydration and death.[48,50]
Large doses of lignocaine may impair cardiac contraction and conduction, resulting in fatal arrhythmias. High levels of circulating lignocaine levels in the blood have been seen as postmortem evidence.[52] A review of 72 cases between 1998 and 2002 have reported 23 deaths following liposuction, of which 10 deaths were under general anaesthesia with tumescent technique. Pulmonary embolism and abdominal viscous perforation were reported to be the two main causes of death.[2]
While addition of epinephrine to the wetting solution produces virtually a bloodless field, it may produce arrhythmias if the circulating levels are high.
The incidence of wound infection and sepsis is very low after liposuction. There are few case reports of peritonitis following bowel perforation and necrotizing fasciitis after liposuction procedure.[53,54]
CONCLUSION
Liposuction is a popular procedure for reducing excessive fat from the body. It is associated with major hemodynamic changes, especially in large-volume liposuction surgery. Anaesthesia for these procedures requires a thorough understanding of the physiological changes and likely complications associated with them. Meticulous monitoring and strict adherence to guidelines for intraoperative fluid therapy ensures a good outcome.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Stephan PJ, Kenkel JM. Updates and advances in liposuction. Aesthetic Surg J. 2010;30:83–97. doi: 10.1177/1090820X10362728. [DOI] [PubMed] [Google Scholar]
- 2.Lehnhardt M, Homann HH, Daigelev A, Hauser J, Palka P, Steinau HU. Major and lethal complications of liposuction: A review of 72 cases in Germany between 1998 and 2002. Plast Reconstr Surg. 2008;121:396e–403e. doi: 10.1097/PRS.0b013e318170817a. [DOI] [PubMed] [Google Scholar]
- 3.Rigel DS, Wheeland RG. Deaths related to liposuction. N Engl J Med. 1999;341:1001–2. [PubMed] [Google Scholar]
- 4.Hanke CW, Coleman WP., 3rd Morbidity and mortality related to liposuction. Questions and answers. Dermatol Clin. 1999;17:899–02. doi: 10.1016/s0733-8635(05)70137-6. [DOI] [PubMed] [Google Scholar]
- 5.Fischer A, Fischer G. First surgical treatment for molding body's cellulite with three 5mm incisions. Bull Int Acad Cosmet Surg. 1976;3:75–9. [Google Scholar]
- 6.Coleman WP., 3rd The history of liposuction and fat transplantation in America. Dermatol Clin. 1999;17:723–27. doi: 10.1016/s0733-8635(05)70121-2. [DOI] [PubMed] [Google Scholar]
- 7.Illouz YG. History and current concepts of liposuction. Clin Plast Surg. 1996;23:721–30. [PubMed] [Google Scholar]
- 8.Klein JA. The tumescent technique for liposuction surgery. Am J Cosmet Surg. 1987;4:263–7. [Google Scholar]
- 9.Coleman WP, 3rd, Glogau RG, Klein JA, Moy RL, Narins RS, Chuang TY, et al. Guidelines of care for liposuction. J Am Acad Dermatol. 2001;45:438–47. doi: 10.1067/mjd.2001.117045. [DOI] [PubMed] [Google Scholar]
- 10.Klein JA. Clinical biostotistics of safety. In: Klein JA, editor. Tumescent liposuction. Tumescent anaesthesia and microcannular liposuction. St Louis: Mosby; 2000. pp. 27–31. [Google Scholar]
- 11.Albin R, De Campo T. Large volume liposuction in 181 patients. Aesthetic Plast Surg. 1999;23:5–15. doi: 10.1007/s002669900235. [DOI] [PubMed] [Google Scholar]
- 12.Sommer B. Advantages and disadvantages of TLA. In: Hanke CW, Sommer B, Sattler G, editors. Tumescent Local Anaesthesia. Berlin: Springer-Verlag; 2001. pp. 47–51. [Google Scholar]
- 13.Hunstad JP. Tumescent and syringe liposuction: A logical partnership. Aesthetic Plast Surg. 1995;19:321–33. doi: 10.1007/BF00451658. [DOI] [PubMed] [Google Scholar]
- 14.Mantse L. Liposuction under local anaesthesia: A retrospective analysis of 100 patients. J Dermatol Surg Oncol. 1987;13:1333–8. doi: 10.1111/j.1524-4725.1987.tb03578.x. [DOI] [PubMed] [Google Scholar]
- 15.Lillis PJ. Lipopsuction surgery under local anaesthesia: Limited blood loss and minimal lidocaine absorption. J Dermatol Surg Oncol. 1988;14:1145–8. doi: 10.1111/j.1524-4725.1988.tb03472.x. [DOI] [PubMed] [Google Scholar]
- 16.Ostad A, Kageyama N, Moy RL. Tumescent anaesthesia with a lidocaine dose of 55mg/kg is safe for liposuction. Dermatol Surg. 1996;22:921–7. doi: 10.1111/j.1524-4725.1996.tb00634.x. [DOI] [PubMed] [Google Scholar]
- 17.Klein JA. Anaesthetic formulations of tumescent solutions. Dermatol Clin. 1999;17:751–9. doi: 10.1016/s0733-8635(05)70124-8. [DOI] [PubMed] [Google Scholar]
- 18.Habbema L. Efficacy of tumescent local anaesthesia with variable lidocaine concentration in 3430 consecutive cases of liposuction. J Am Acad Dermatol. 2010;62:988–94. doi: 10.1016/j.jaad.2009.09.004. [DOI] [PubMed] [Google Scholar]
- 19.Hunstad JP. Liposuction of hips and thighs. In: Evans G, editor. Operative plastic surgery. New York: McGraw Hill; 2000. pp. 93–125. [Google Scholar]
- 20.Rohrick RJ, Beran SJ. Is Liposuction Safe? Plast Recontr Surg. 1999;104:819–22. doi: 10.1097/00006534-199909030-00033. [DOI] [PubMed] [Google Scholar]
- 21.Kenkel JM, Lipschitz AH, Shepherd G, Armstrong VW, Streit F, Oellerich M, et al. Pharmacokinetics and safety of lidocaine and monoethylglycinexylidide in liposuction: A microdialysis study. Plast Reconstr Surg. 2004;114:516–24. doi: 10.1097/01.prs.0000128423.84607.61. [DOI] [PubMed] [Google Scholar]
- 22.Rubin JP, Bierman C, Rosow CE, Arthur GR, Chang Y, Courtiss EH, et al. The tumescent technique: The effect of high tissue pressure and dilute epinephrine on absorption of lidocaine. Plast Reconstr Surg. 1999;103:990–6. [PubMed] [Google Scholar]
- 23.Kucera IJ, Lambert BA, Klein JA, Watkins RG, Hoover JM, Kaye AD. Liposuction: Contemporary issues for the anesthesiologist. J Clin Anesth. 2006;18:379–87. doi: 10.1016/j.jclinane.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 24.Lindenblatt N, Belusa L, Tiefenbach B, Schareck W, Olbrisch RR. Prilocaine plasma levels and methemoglobinemia in patients undergoing tumescent liposuction involving less than 2,000 ml. Aesthetic Plast Surg. 2004;28:435–40. doi: 10.1007/s00266-004-0009-5. [DOI] [PubMed] [Google Scholar]
- 25.Grossmann M, Sattler G, Pistner H, Oertel R, Richter K, Schinzel S, et al. Pharmacokinetics of articaine hydrochloride in tumescent local anaesthesia for liposuction. J Clin Pharmacol. 2004;44:1282–9. doi: 10.1177/0091270004269014. [DOI] [PubMed] [Google Scholar]
- 26.Burk RW, 3rd, Guzman-Stein G, Vasconez LO. Lidocaine and epinephrine levels in tumescent technique liposuction. Plast Reconstr Surg. 1996;97:1379–84. doi: 10.1097/00006534-199606000-00009. [DOI] [PubMed] [Google Scholar]
- 27.Samdal F, Amland PF, Bugge JF. Blood loss during suction – assisted lipectomy with large volumes of dilute adrenaline. Scand J Plast Reconstr Surg Hand Surg. 1995;29:161–5. doi: 10.3109/02844319509034333. [DOI] [PubMed] [Google Scholar]
- 28.Lalinde E, Sanz J, Ballesteros A, Elezabeitia J, Mesa F, Bazán A, et al. Effect of L-Ornithine 8-Vasopressin on Blood Loss During Liposuction. Ann plast surg. 1995;34:613–8. doi: 10.1097/00000637-199506000-00008. [DOI] [PubMed] [Google Scholar]
- 29.Smith SL, Hodge JA, Lawrence N, Badame AJ, Coleman WP., 3rd The importance of bicarbonate in large volume anaesthetic preparations. Revisting the tumescent formula. J Dermatol Surg Oncol. 1992;18:972–5. doi: 10.1111/j.1524-4725.1992.tb02769.x. [DOI] [PubMed] [Google Scholar]
- 30.Kenkel JM, Lipschitz AH, Luby M, Kallmeyer I, Sorokin E, Appelt E, et al. Hemodynamic physiology and thermoregulation in liposuction. Plast Reconstr Surg. 2004;114:503–13. doi: 10.1097/01.prs.0000132676.19913.a3. [DOI] [PubMed] [Google Scholar]
- 31.Goldberg M, Arawanow H, Jr, Smith AA, FABER M. Pheochromocytoma and essential hypertensive vascular disease. AMA Arch Intern Med. 1950;86:823–36. doi: 10.1001/archinte.1950.00230180028003. [DOI] [PubMed] [Google Scholar]
- 32.Anderson KE, Bende M. Adrenoceptors in the control of human nasal mucous blood flow. Ann Otol Rhinol Laryngol. 1984;93:179–82. doi: 10.1177/000348948409300216. [DOI] [PubMed] [Google Scholar]
- 33.Christopherson R, Glavan N, Norris EJ, Beattie C, Rock P, Frank SM, et al. Control of blood pressure and heart rate in patients randomized to epidural or general anaesthesia for lower extremity vascular surgery. J Clin Anesth. 1996;8:578–84. doi: 10.1016/s0952-8180(96)00139-0. [DOI] [PubMed] [Google Scholar]
- 34.Hoffman BB. Catecholamines, sympathomimetic drugs and adrenergic receptors antagonists. In: Hardman JG, Limbird LE, Gilman AG, editors. Goodman and Gillman's. The pharmacologic basis of therapeutics. 10th edition. New York: Professional McGraw-Hill; 2001. pp. 215–68. [Google Scholar]
- 35.Broughton G, 2nd, Crosby MA, Coleman J, Rohrich RJ. Use of herbal supplements and vitamins in plastic surgery: A practical review. Plast Reconstr Surg. 2007;119:48e–66e. doi: 10.1097/01.prs.0000252661.72071.8d. [DOI] [PubMed] [Google Scholar]
- 36.Mysore V. Tumescent liposuction: Standard guidelines of care. Indian J Dermatol Venereol Leprol. 2008;74:S54–60. [PubMed] [Google Scholar]
- 37.Regatieri FL, Masquera MS. Liposuction anaesthesia techniques. Clin Plastic Surg. 2006;33:27–37. doi: 10.1016/j.cps.2005.08.003. [DOI] [PubMed] [Google Scholar]
- 38.Greets WH, Bergqvist D, Pineo GF, Heit JA, Samama CM, Lassen MR, et al. Prevention of venous thromboembolism: American College of Chest Physicians evidence–based practice guidelines. Chest. 2008;133:381s–453s. doi: 10.1378/chest.08-0656. [DOI] [PubMed] [Google Scholar]
- 39.MacKenzie N, Grant IS. Propofol for intravenous sedation. Anaesthesia. 1987;42:3–6. doi: 10.1111/j.1365-2044.1987.tb02936.x. [DOI] [PubMed] [Google Scholar]
- 40.Bauer KP, Dom PM, Ramirez AM, O’Flaherty JE. Preoperative intravenous midazolam: Benefits beyond anxiolysis. J Clin Anesth. 2004;16:177–83. doi: 10.1016/j.jclinane.2003.07.003. [DOI] [PubMed] [Google Scholar]
- 41.Knize DM, Fishell R. Use of preoperative subcutaneous “wetting solution” and epidural block anaesthesia for liposuction in the office- based surgical suite. Plast Reconstr Surg. 1997;100:1867–74. doi: 10.1097/00006534-199712000-00035. [DOI] [PubMed] [Google Scholar]
- 42.Grazer FM, De Jong RH. Fatal outcomes from liposuction: Census survey of cosmetic surgeons. Plast Reconstr Surg. 2000;105:436–48. doi: 10.1097/00006534-200001000-00070. [DOI] [PubMed] [Google Scholar]
- 43.Sommer B. Advantages and disadvantages of TLA. In: Hanke CW, Sommer B, Sattler G, editors. Tumescent local anaesthesia. New York: Springer; 2001. pp. 47–51. [Google Scholar]
- 44.Pitman GH, Aker JS, Tripp ZD. Tumescent liposuction.A surgeon's perspective. Clin Plast Surg. 1996;23:633–41. [PubMed] [Google Scholar]
- 45.Trott SA, Beran SJ, Rohrich RJ, Kenkel JM, Adams WP, Jr, Klein KW. Safety considerations and fluid resuscitation in liposuction.An analysis of 53 consecutive patients. Plast Reconstr Surg. 1998;102:2220–9. doi: 10.1097/00006534-199811000-00063. [DOI] [PubMed] [Google Scholar]
- 46.Rohrich R, Leedy J, Swamy R, Brown SA, Coleman J. Fluid resuscitation in liposuction: A retrospective review of 89 consecutive patients. Plast Reconstr Surg. 2006;117:431–5. doi: 10.1097/01.prs.0000201477.30002.ce. [DOI] [PubMed] [Google Scholar]
- 47.Hughes CE., 3rd Reduction of liposuction risks and mortality: An ASAPS survey. Aesthetic Surg J. 2001;21:120–7. doi: 10.1067/maj.2001.115166. [DOI] [PubMed] [Google Scholar]
- 48.Rao RB, Ely SF, Hoffman RS. Deaths related to liposuction. N Eng J Med. 1999;240:1471–5. doi: 10.1056/NEJM199905133401904. [DOI] [PubMed] [Google Scholar]
- 49.Teimourian, Rogers WB., 3rd A national survey of complications associated with suction lipectomy: A comparative study. Plast Recontr Surg. 1989;84:628–31. [PubMed] [Google Scholar]
- 50.Gillard MD, Coates N. Tumescent liposuction complicated by pulmonary edema. Plast Reconstr Surg. 1997;99:215–9. doi: 10.1097/00006534-199701000-00032. [DOI] [PubMed] [Google Scholar]
- 51.Hunstad JP. Body contouring in the obese patient. Clin Plast Surg. 1996;23:647–70. [PubMed] [Google Scholar]
- 52.De Jong RH, Grazer FM. “Tumescent” liposuction alert: Deaths from lidocaine cardiotoxicity. Am J Forensic Med Pathol. 1999;20:101. doi: 10.1097/00000433-199903000-00024. [DOI] [PubMed] [Google Scholar]
- 53.Sharma D, Dalencourt G, Bitterly T, Benotti PN. Small intestinal perforation and necrotizing fasciitis after abdominal liposuction. Aesthetic Plast Surg. 2006;30:712–6. doi: 10.1007/s00266-006-0078-8. [DOI] [PubMed] [Google Scholar]
- 54.Mallappa M, Rangaswamy M, Badiuddin MF. Small intestinal perforation and peritonitis after liposuction. Aesth Plast Surg. 2007;31:589–92. doi: 10.1007/s00266-007-0050-2. [DOI] [PubMed] [Google Scholar]


