Abstract
The overall goal of the global oximetry (GO) project was to increase patient safety during anaesthesia and surgery in low and middle income countries by decreasing oximetry costs and increasing oximetry utilisation. Results from the overall project have been previously published. This paper reports specifically on pilot work undertaken in four hospitals in one Indian State. The aim of this work was to assess the impact of increasing oximetry provision in terms of benefits to anaesthetists and in the identification of patient problems during anaesthesia, to identify training needs and to explore perceptions regarding barriers to more comprehensive oximetry coverage. Data collection was by interview with hospital staff, use of a log-book to capture data on desaturation episodes and a follow-up questionnaire at 10 months after the introduction of additional oximeters. Increasing oximetry utilisation in the four hospitals was viewed positively by the anaesthetic staff and enabled improvement in monitoring patients. Of the 939 monitored patients studied, 214 patients (23%) experienced a total of 397 desaturation episodes. For nearly half of the patients undergoing caesarean section under regional anaesthesia following a desaturation event supplementary oxygen was required. In 53 of the 379 female sterilisations (14%) desaturation episodes occurred and in eight patients, there were 17 episodes of desaturation due to obstruction. In the recovery room, 91 of the 939 patients were monitored using the oximeters with 12 patients (13%) requiring oxygen. This study has highlighted that pulse oximetry must be used even in patients having surgical procedures or caesarean section under regional or local anaesthesia as these procedures are associated with hypoxic episodes. Anaesthetists must ensure they are complying with the Indian Society of Anaesthesiologists monitoring standards for anaesthesia and ensure patients are monitored by pulse oximetry.
Keywords: Desaturation, hypoxic events, oximetry gap, patient safety, pulse oximetry
INTRODUCTION
Pulse oximetry is accepted as an essential part of anaesthesia practice[1] and early detection and correction of perioperative events through pulse oximetry monitoring is regarded as improving patient outcome.[2] Hypoxaemia is reduced by pulse oximetry monitoring in both operating room (OR) and recovery room (RR) settings.[3] Introducing pulse oximetry has been shown to reduced incidence of cardiac arrest[4] and decrease the unexpected postoperative admission rate to critical care.[5] Moller et al. found that oximetry monitoring was associated with a 19-fold increase in the diagnosed incidence of hypoxia from a study of 20802 patients.[6] A cochrane systematic review[7] used Moller et al.'s data and three other studies, and concluded that hypoxaemia was reduced in the pulse oximetry group in both OR and RR. Counter-intuitively it also concluded that pulse oximetry did not affect the outcome of anaesthesia.[7] This conclusion was, however, reached without taking into account all the relevant evidence from expert opinion and other sources[8] and convincing evidence is still not available to link improved outcomes with the use of pulse oximetry.
Anaesthesia societies and regulatory bodies in the UK, Australia and North America have long advocated mandatory usage of oximetry in anaesthesia.[9–11] The Indian Society of Anaesthesiologists (ISA) clearly state that ‘it is mandatory for oxygenation to be further monitored by Pulse Oximetry.[12] Anaesthetists may, however, see the pulse oximeter as essential technology yet not be able to use it or have access to one in their everyday practice. Kotur as recently as 2002, stated that in some parts of India, ‘the anaesthesiologist is expected to work with a bottle of ether and use the same two hands for monitoring pulse and blood pressure’.[13]
At world level, there was a drive in 1992 to develop global standards for safer practice including a recommendation for inclusion of pulse oximetry by the International Task Force on Anaesthesia Safety. These standards[14] were adopted by the World Federation of Societies of Anaesthesiologists (WFSA) in June 1992 and were recently updated.[15] However little has changed. This has been in part due to no accompanying action plan to get oximetry into global use until in 2004 The World Health Organisation (WHO) launched ‘The World Alliance for Patient Safety’ which has goals of coordinating, disseminating and accelerating improvements in patient safety worldwide. The WHO has more recently focused, in its ‘Safe Surgery Saves Lives’ initiative, on safer surgical care and safer anaesthesia.[16] Bringing in worldwide guidelines to make oximetry mandatory was one of the global oximetry (GO) project's early objectives[17] and during 2008, the WHO introduced a new global standard for perioperative care, including the words “… pulse oximeter attached and working.”[18]
THE GO PROJECT IN INDIA
This project was an initiative between the World Federation of Societies of Anaesthesiologists (WFSA), the Association of Anaesthetists of Great Britain and Ireland (AAGBI), and GE Healthcare. WFSA instructed its Safety and Quality of Practice Committee, in 2004, to establish a Global Oximetry project.[17] GO was then launched in 2006/2007 in four countries with widely varying cultures, politics, health systems and gross domestic products: Uganda, The Philippines, Vietnam and India. The overall goal of GO was to increase patient safety during anaesthesia and surgery in low and middle income countries by decreasing oximetry costs and increasing oximetry utilisation.[17,19] Walker et al. (2009) provided the overview results from the four countries, including the gap in oximetry provision.[19] This paper provides the additional individual results from the 4 hospital pilot sites in India collected during 2007-2008.
The aim of this work was to assess the impact of increasing oximetry provision in terms of benefits to anaesthetists and identification of patient problems during anaesthesia; to identify training needs; to explore perceptions regarding barriers to more comprehensive oximetry coverage and to determine a view on the desirable functionality for an ideal low cost oximeter.
STUDY LOCATION
Using individuals with a knowledge of India, one Indian state was selected as suitable for the pilot study since oximetry is in use but is severely under-supplied. An overall survey of all 50 public hospitals in state was conducted to investigate anaesthesia facilities and oximetry provision and requirements. The results of that complete survey were published by Walker et al. in 2009.[19] This report centres on the four hospitals in one Indian State specifically chosen for this pilot study. They were selected because they had a high turn out of surgical procedures, were undersupplied with oximeters and there was support and co-operation expressed for the project. Three were district hospitals each serving approximately 1–2 million population with 2–3 operating rooms (Hospitals A, B, and C) and one was the hub hospital and tertiary referral hospital for the State with 16 operating rooms (Hospital D). Permission to undertake and publish findings resulting from this work was given by the Commissioner, The Director General, Health Services for the chosen state.
METHODS
Through site visits and interviews with health professionals and managers in the four hospitals in July 2007, we collected information on the need for oximetry (existing oximetry provision; oximetry requirement; barriers to oximetry usage; training needs). In December 2007, staff at the four hospitals were provided with training and 12 donated oximetry units (TruSat, GE Healthcare). Each anaesthetist was asked to complete a one-page questionnaire on every patient in whom they used a donated oximeter to measure desaturation episodes. The study took place over a one month period during December 2007 to January 2008. The forms were first piloted by anaesthetic staff in one hospital, responses were taken into account and minor modifications made. An episode of desaturation was defined as oxygen saturation (SpO2)≤90% or a fall from baseline ≥4% (in those starting with a low SpO2), a definition determined in consultation with local anaesthetists.
Ten months after the introduction of the oximeters, lead anaesthetists in each hospital completed a follow-up questionnaire ascertaining their opinion on the performance of the donated oximeters and desired functionality of an ideal future low cost oximeter.
Data from the questionnaires were entered into Microsoft® Excel and analysed by descriptive statistics, using frequencies and percentages. The association between two variables such as desaturation events and type of anaesthesia was also analysed using descriptive statistics. The questions on performance and view of oximeters were assessed using a Likert scale and analysed using frequencies. Interview data relating to training and barriers to using oximeters with health professionals were content-analysed.
RESULTS
Barriers to using oximeters
The anaesthetists reported that there were no barriers to using the donated oximeters. In each hospital, there was a need for additional oximeters. The anaesthetists felt benefit when oximeters were available, whether in OR or RR settings. At site visits, anaesthetists and other key health professionals identified barriers regarding getting oximetry into their hospital as: Purchase cost; difficulties of procurement; maintenance cost.
Training requirements
Training needs regarding oximetry were assessed in the four study sites. A training manual designed for the GO subproject in Uganda was trialled in our hospitals. We found that the anaesthetists required no training on physiology or on the use of pulse oximeters., An anaesthetist may supervise two or more tables with a nurse attending and monitoring the patient. Nurses did need training but at a basic level. Female sterilisations are carried out in large numbers without the anaesthetist being present, the nurse alerting the anaesthetist, who may be in another operating room, to any patient difficulty.
Local need for pulse oximeters
The number of working oximeters in each hospital together with the estimated requirement, that is one oximeter per OR table to reach WHO global standards were: Hospital A: One working oximeter but required 5; Hospital B: One but required six; Hospital C: One but required three; and Hospital D: 15 working oximeters but requiring 24. There was a deficiency of between two and nine oximeters in the four hospitals, making the oximetry gap between 38% and 83%.
When oximeters were donated, this reduced the oximetry gap to 40%, 50%, 0% and 13% for Hospitals A, B, C and D, respectively.
Study of desaturation events
A log-book was used to study desaturation events in patients undergoing surgical procedures and in recovery. Donated pulse oximeters were introduced backed up by induction training for doctors and nurses. A total of 939 patient forms were returned, 848 about patient events in the OR and 91 about patient events in the RR. Hospitals A and B introduced oximeters into the OR only and followed 255 and 302 cases respectively. Hospital C followed 185 patients through the OR and studied only two cases in the RR. Hospital D studied oximeters in both OR and RR and followed 106 cases in the OR and 89 in the RR.
Of the 939 patients studied in total, 725 patients (77%) experienced no episodes of desaturation and 214 patients (23%) experienced one or more episodes of desaturation, resulting in a total of 397 episodes of desaturation. Oxygen was required in 125 patients (58%) who experienced 252 episodes of desaturation. There were 10 patients who experienced 20 episodes due to obstruction, 10 patients (8%) who experienced 13 episodes due to equipment fault or disconnection, 5 patients (4%) who experienced 10 episodes due to shivering and 67 (54%) patients had 102 episodes due artefacts. Three of these patients had different reasons for desaturation (e.g. artefact then disconnection).
In the 848 patients who were monitored in the OR most desaturation events requiring active intervention happened during regional anaesthesia (RA) 46% and general anaesthesia (GA) 43%. The main action required was administration of oxygen: In 76 of the 175 patients (43%) having RA and in 15 of the 37 patients (41%) having a GA. During local anaesthesia, 77 of 631 patients (12%) had a desaturation event and for 46 patients (7.3%) this was an artefact; 21 patients (3.3%) required oxygen, 8 patients (1%) had an airway obstruction and 2 (0.3%) patients had episodes of shivering.
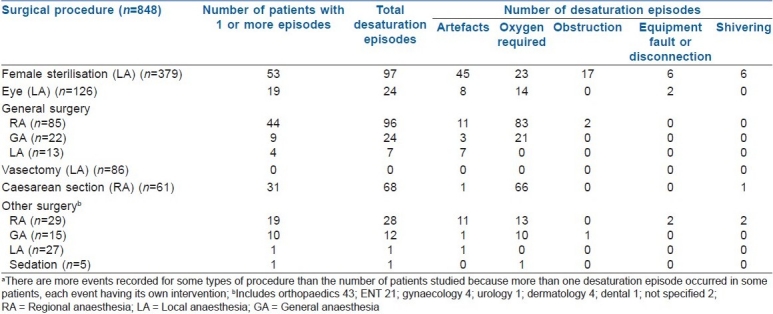
Table 1 provides details of the desaturation episodes in the OR by surgical procedure and type of anaesthesia. In the 61 patients who had a caesarean section, 31 patients (51%) had 68 desaturation episodes. Of the 85 patients undergoing general surgery by RA, 44 patients (52%) experienced 96 desaturation episodes (8 of these patients had 11 artefact episodes). In the 379 patients undergoing female sterilisation, 53 patients (14%) experienced 97 desaturation episodes; however in 27 of these patients, there were 45 artefacts [Table 1]. In the 126 patients undergoing eye surgery, 19 patients (15%) experienced 26 episodes of desaturation with 12 patients (10%) requiring active intervention in the form of oxygen or correction to equipment.
Table 1.
Action and interpretation of desaturation episodes in the operating room by surgical procedure and type of anaesthesiaa
Recovery patients (91 patients)
Most patients (n=89) monitored in recovery came from Hospital D. There were 23 patients (26%) who experienced 35 desaturation episodes, 14 of which were artefacts (11 patients). The majority of these patients (n=20, 22%) had undergone general surgery with three patients having undergone either an orthopaedic or neurosurgical procedure. Thirteen of 91 patients (14%) required an active intervention with 12 patients (13%) requiring supplemental oxygen and one patient whose desaturation episodes were artefact followed by shivering.
Performance of and views about oximeters
Ten months after the 12 oximeters had been provided, all but one (which had not functioned from the start) were reported to be still functioning with three probes having to be replaced. The anaesthetists found the donated units easy to use and to be reliable, sturdy and portable.
In their view the key features required for an ideal future low cost pulse oximeter included long battery life, ease of use, ease of charging, durability and ability to continue working well when blood pressure was low. Having the additional functionality of electrocardiogram (ECG) and Non Invasive Blood pressure (NIBP) were seen as important.
In areas of anaesthesia practice such as in the ‘tubectomy’ room (female sterilisation) and in recovery where pulse oximetry had not been introduced before, it was seen as being of great value and doctors told us that it should become common practice. The main benefits for the anaesthetists were being able to detect hypoxia early and feeling more comfortable during practice. Reduced stress was cited, in particular where anaesthetists worked single-handed. The oximeter also enabled one anaesthetist to monitor better two operations at the same time and prompted nurses to report problems more quickly to the anaesthetist.
DISCUSSION
This project in India has focussed on investigating the oximetry gap in operating rooms and assessing the impact of increasing oximetry provision in four hospitals, together with training needs. We also explored the perceptions regarding barriers to more comprehensive oximetry coverage.
There was an oximetry gap in the four hospitals in the Indian state. This situation is due principally to inadequate numbers of oximeters being provided in the first place and the existence of units over their recommended lifespan which were either awaiting repair, away for repair or not working due to a lack of system in place for probe resupply. The main reasons for undersupply of units are cost; difficulty procuring oximeters, failure to purchase or enforce annual maintenance contracts and systems for resupplying probes, and the lack of an agreed guideline or standard in the State hospitals. In the overall survey report by Walker et al. (2009) they commented that the 65% oximetry gap in the Indian State was similar to Uganda (64%) but better than Binh Dinh Vietnam (76%).[19]
This work in the one Indian State has shown that there was near-total acceptance of the need for oximetry by health professionals and a high level of demand. Thus the Minimum Mandatory Monitoring Standards[12] adopted by the ISA making oximetry mandatory would be expected to be well received and find high levels of acceptance amongst anaesthetists.
Training needs in pulse oximetry were found to be different in the countries involved in the GO project.[19] A survey in the UK revealed a lack of knowledge about pulse oximetry and its interpretation among junior doctors and nursing staff.[20] There has been considerable training of anaesthetists and anaesthetic assistants in Uganda in pulse oximetry.[21] However, in the participating hospitals in India, the lead anaesthetists report that there was no training need on pulse oximetry for their medically qualified staff, but for nurses monitoring patients there were basic training needs which were easily met through training provided by the lead anaesthetist.
In India, where a large number of surgical procedures are undertaken each day pulse oximetry has provided for these anaesthetists what they perceive as safer practice. This issue of safer practice using oximetry is well documented. Runciman in 1993 showed in a qualitative analysis of 2000 incidents, a reduction in the incidence of cardiac arrest when pulse oximetry was used.[6]
Safety in anaesthesia improved considerably in the second half of the last century with much of the improvement in anaesthesia-related mortality occurring by the mid 1980s.[22] This was before the introduction of pulse oximetry. A review in 1992 concluded that pulse oximetry probably had contributed to increasing the safety of anaesthesia.[23] A critical incident study of perioperative events in 1987 found that the pulse oximeter warned of a life-threatening problem in 5% of all anaesthetics.[24] We found that the highest percentage of active intervention by the anaesthetist was required for operations involving regional anaesthesia (46%) than for general anaesthesia (43%). For patients undergoing caesarean sections by RA, 51% required intervention by the anaesthetist. It was also of interest that even in those patients having minor surgical procedures under local anaesthesia, desaturation events occurred in 12% of patients with positive intervention required for 10% of eye procedures and for 7% of female sterilisations. These procedures in India are carried out in large numbers and part of national programmes of work (e.g. cataract surgery and maternal health programmes), emphasizing the need for optimum safety at all time. In some hospitals, the anaesthetic practice for patients undergoing regional and local anaesthesia is to give both a sedative and an analgesic in a premedication room before surgery, which may have precipitated some desaturation episodes.
We believe that by having additional oximeters in the four hospitals there was earlier detection of many desaturation events. A review in the late 1980s of 1175 anaesthetic-related malpractice claims found that 31.5% of the negative outcomes could have been prevented by having additional monitors.[25]
The donated oximeters enabled two hospitals to introduce oximeters into the recovery room, where 14% of cases required intervention by the anaesthetist. It is possible that our study might have reduced morbidity in these patients. Morris et al. found that 14% of inpatients developed at least transient hypoxaemia during recovery.[26] In a single-blind study of 202 adults in the recovery room following elective surgery, despite administration of nasal oxygen, 55% of patients demonstrated decreases to SpO2 <91% at some time before discharge.[27] Recovery is an important area for pulse oximeters to be used. It has previously been found that up to 30% of perioperative deaths occur during recovery, largely because of cardiovascular or respiratory problems.[28]
The benefits of using oximetry when focussing on patient outcome have not been proven.[7] This would be difficult to establish without a very large randomised controlled trial.[5,29] As the incidence of severe adverse clinical outcomes following anaesthesia is low, sample size requirements would be high[30] and, it has been argued, unfeasible.[8] Potts et al, showed that randomized control trials (RCTs)may be unsuitable research questions and argued that when an intervention is life saving and there is a clear potential benefit from the intervention, better evidence should not be awaited before moving from research to practice.[31] In India, it is important to understand the risks of not using oximetry and the benefits of using oximetry rather than delaying implementing this technology while waiting for the perfect ‘gold standard’ evidence.
The anaesthetists’ requirements for an ideal oximeter for use within their practice have been explored. These included low cost, additional functions such as NIBP and ECG, a long-battery life, audible and visible alarm with high and low limits and spare probes. These requirements were also identified in Uganda and Vietnam, two other sites involved in the GO project.[19]
Limitations in our study include the lack of baseline data, a short (one month) data collection period and data only being obtained from patients attached to donated oximeters. The study may not have included every patient receiving surgery in some of the hospitals.
In conclusion, this study has shown that pulse oximetry must be used for all patients undergoing surgery or caesarean section even under regional or local anaesthesia as these procedures are associated with a number of hypoxic episodes. Anaesthetists should comply with the ISA standards monitoring standards for anaesthesia. The additional pulse oximeters were of benefit to anaesthetists and also enabled better quality of care for patients due to rapid response by the anaesthetist. Pulse oximetry has been described as the ‘last line of defence in avoiding ventilation mishaps and resulting catastrophic outcomes’[32] or as one anaesthetist in this study said ‘having an oximeter is like having a skilled pair of hands’.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Eichorn JH. Pulse oximetry as a standard of practice in anaesthesia. Anesthesiology. 1993;78:423–6. [PubMed] [Google Scholar]
- 2.Pedersen T, Moller AM, Pedersen BD. Pulse oximetry for perioperative monitoring: Systematic review of randomized controlled trials. Anesth Analg. 2003;96:426–31. doi: 10.1097/00000539-200302000-00024. [DOI] [PubMed] [Google Scholar]
- 3.Moller JT, Jensen PF, Johannessen NW, Espersen K. Hypoxaemia is reduced by pulse oximetry monitoring in the operating theatre and in the recovery room. Br J Anaesth. 1992;68:146–50. doi: 10.1093/bja/68.2.146. [DOI] [PubMed] [Google Scholar]
- 4.Runciman WB. Qualitative versus quantitative research-balancing cost, yield and feasibility. Anaesth Intensive Care. 1993;21:502–5. doi: 10.1136/qhc.11.2.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cullen DJ, Nemeskal AR, Cooper JB, Zaslavsky A, Dwyer MJ. Effect of pulse oximetry, age, ASA physical status on the frequency of patients admitted unexpectedly to a postoperative intensive care unit and the severity of their anaesthesia-related complication. Anesth Analg. 1992;74:181–4. doi: 10.1213/00000539-199202000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Moller JT, Johannessen NW, Espersen K, Ravlo O, Pedersen BD, Jensen PF, et al. Randomized evaluation of pulse oximetry in 20,802 patients: II: Perioperative events and postoperative complications. Anesthesiology. 1993;78:445–53. doi: 10.1097/00000542-199303000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Pedersen T, Dyrlund Perdersen B, Møller AM. Pulse oximetry for perioperative monitoring. Cochrane Database of Systematic Reviews. 2003;3:CD002013. doi: 10.1002/14651858.CD002013. [DOI] [PubMed] [Google Scholar]
- 8.Runciman B, Merry A, Walton M. Safety and Ethics in Healthcare: A guide to getting it right. Hampshire: Ashgate Publishing Limited; 2007. pp. 135–56. [Google Scholar]
- 9.Anaesthesia Patient Foundation [homepage on the Internet] Indianapolis: Faculty of Anaesthetists, Royal Australasian College of Surgeons. Policy statement June 1988. Monitoring during anaesthesia (Australia) 2008. [Last cited on 2010 October 7]. Available from: http://www.apsf.org/newsletters/html/1988/fall/#article%2011 .
- 10.Recommendations for standards of monitoring during anaesthesia and recovery. 4th ed. London: AAGBI; 2007. Association of Anaesthetists of Great Britain and Ireland; pp. 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Standards for basic anesthetic monitoring. Park Ridge Illinois: ASA; 2005. American Society of Anesthesiologists; pp. 1–3. [Google Scholar]
- 12.Monitoring standards for providing anaesthesia. India: ISA; [Last cited on 2010 June 20]. Indian Society of Anaesthesiologists [homepage on the Internet] no date. Available from: http://www.isaweb.in/moniter_std.asp . [Google Scholar]
- 13.Kotur PF. Monitoring and the anaesthesiologist.Editorial. Indian J Anaesth. 2002;46:244–5. [Google Scholar]
- 14.International Task Force on Anaesthesia Safety. Eur J Anaesthesiol. 1993;10:12–5. [Google Scholar]
- 15.World Federation of Societies of Anaesthesiologists ([homepage on the Internet] International Standards for a Safe Practice of Anaesthesia. 2008. [Last cited on 2010 June 10]. World Federation of Societies of Anaesthesiologists. Available from: http://anaesthesiologists.org/en/safety/ 2008-international-standards-for-a-safe-practiceof-anaesthesia.html .
- 16.World Health Organisation [homepage on the Internet] World Alliance for Patient Safety. 2007. [Last cited on 2010 June 20]. Available from: http://www.who.int/patientsafety/about/en/index.html .
- 17.Thoms GM, McHugh GA, O’Sullivan E. The global oximetry initiative. Anaesthesia. 2007;62:75–7. doi: 10.1111/j.1365-2044.2007.05305.x. [DOI] [PubMed] [Google Scholar]
- 18.World Health Organisation [homepage on the Internet] Safe Surgery Saves Lives: The Second Global Patient Safety Challenge. 2008. [Last cited on 2010 June 20]. Available from: www.who.int/patientsafety/challenge/safe.surgery/en/
- 19.Walker IA, Merry AF, Wilson IH, McHugh GA, O’Sullivan E, Thoms GM, et al. Global oximetry: An international anaesthesia quality improvement project. Anaesthesia. 2009;64:1051–60. doi: 10.1111/j.1365-2044.2009.06067.x. [DOI] [PubMed] [Google Scholar]
- 20.Stoneham MD, Saville GM, Wilson IH. Knowledge about pulse oximetry among medical and nursing staff. Lancet. 1994;344:1339–42. doi: 10.1016/s0140-6736(94)90697-1. [DOI] [PubMed] [Google Scholar]
- 21.Hodges SC, Mimumbi C, Okell M, McCormick BA, Walker IA, Wilson IH. Anaesthesia services in developing countries: Defining the problems. Anaesthesia. 2007;62:4–11. doi: 10.1111/j.1365-2044.2006.04907.x. [DOI] [PubMed] [Google Scholar]
- 22.Orkin FK. Patient monitoring during anesthesia as an exercise in technology assessment. In: Saidman LJ, Smith NT, editors. Monitoring in Anesthesia. 3rd ed. Boston MA: Butterworth-Heinemann; 1993. pp. 439–55. [Google Scholar]
- 23.Severinghaus JW, Kelleher JF. Recent developments in pulse oximetry. Anesthesiology. 1992;76:1018–38. doi: 10.1097/00000542-199206000-00024. [DOI] [PubMed] [Google Scholar]
- 24.McKay WP, Noble WH. Perioperative critical incidents detected by pulse oximeter. Can J Anaesth. 1987;34:570–1. doi: 10.1007/BF03010621. [DOI] [PubMed] [Google Scholar]
- 25.Tinker JH, Dull DL, Caplan RA, Ward RJ, Cheney FW. Role of monitoring devices in prevention of anesthetic mishaps: A closed claims analysis. Anesthesiology. 1989;71:541–6. doi: 10.1097/00000542-198910000-00010. [DOI] [PubMed] [Google Scholar]
- 26.Morris RW, Buschman A, Warren DL, Philip JH, Raemer DB. The prevalence of hypoxemia detected by pulse oximetry during recovery from anesthesia. J Clin Monit. 1988;4:16–20. doi: 10.1007/BF01618102. [DOI] [PubMed] [Google Scholar]
- 27.Moller JT, Wittrup M, Johansen SH. Hypoxemia in the postanesthesia care unit: An observer study. Anesthesiology. 1990;73:890–5. doi: 10.1097/00000542-199011000-00016. [DOI] [PubMed] [Google Scholar]
- 28.Harrison GG. Deaths attributable to anaesthesia. A 10-year survey. Br J Anaesth. 1978;80:1041–6. doi: 10.1093/bja/50.10.1041. [DOI] [PubMed] [Google Scholar]
- 29.Moller JT, Pedersen T, Rasmussen LS, Jensen PF, Pedersen BD, Ravlo O, et al. Randomized evaluation of pulse oximetry in 20,802 patients: I: Design, demography, pulse oximetry failure rate, and overall complication rate. Anesthesiology. 1993;78:436–44. doi: 10.1097/00000542-199303000-00006. [DOI] [PubMed] [Google Scholar]
- 30.Thoms GM, Orkin FK, McHugh GA. Epidemiology and Health Services Research. In: Healy TEJ, Cohen PJ, editors. Wiley WD, Churchill-Davidson's A Practice of Anaesthesia. 7th ed. London: Edward Arnold; 2003. pp. 1353–74. [Google Scholar]
- 31.Potts M, Prata N, Walsh J, Grossman A. Parachute approach to evidence based medicine. BMJ. 2006;333:701–3. doi: 10.1136/bmj.333.7570.701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stemp LI, Ramsay MA. Pulse OX Last Line of Defense. [Last cited on 2010 June 20];ASA Newsletter (Letters to the Editor) 2006 Feb;70(2) Available from: http://www.asahq.org/Newsletters/2006/02-06/lte02_06.html . [Google Scholar]


