Abstract
Brachial plexus block via the axillary approach is problematic in patients with limited arm mobility. In such cases, the infraclavicular approach may be a valuable alternative. The purpose of our study was to compare axillary and infraclavicular techniques for brachial plexus block in patients undergoing forearm and hand surgeries. After obtaining institutional approval and written informed consent, 60 patients of American Society of Anaesthesiologists grade I or II scheduled for forearm and hand surgeries were included in the study and were randomly allocated into two groups. Brachial plexus block was performed via the vertical infraclavicular approach (VIB) in patients of Group I and axillary approach in Group A using a peripheral nerve stimulator. Sensory block in the distribution of individual nerves supplying the arm, motor block, duration of sensory block, incidence of successful block and various complications were recorded. Successful block was achieved in 90% of the patients in group I and in 87% of patients in group A. Intercostobrachial nerve blockade was significantly higher in group I. No statistically significant difference was found in sensory and motor blockade of other nerves. Both the approaches are comparable, but the VIB scores ahead of axillary block in terms of its ability to block more nerves. The VIB because of its easily identifiable landmarks, a comfortable patient position during the block procedure and the ability to block a larger spectrum of nerves should thus be considered as an effective alternative to the axillary approach.
Keywords: Axillary block, intercostobrachial nerve, musculocutaneous nerve, vertical infraclavicular block
INTRODUCTION
The axillary approach to block the brachial plexus has been widely used to provide anaesthesia for surgery of the forearm and hand. Its benefits include simplicity, reliable efficacy and safety.[1] However, its application may be difficult in patients with limited movement of the shoulder or arm, as in those with painful injuries.[2] Also, with the standard single injection axillary block, reliable musculocutaneous nerve (MCN) and radial nerve anaesthesia is limited by anatomical conditions[3] and success rates vary widely.
In 1995, Kilka and colleagues[4] introduced the vertical infraclavicular block. Favourable characteristics of this approach are less painful arm positioning for patients with fractures, reliability of the technique on the identification of easily palpable landmarks (even in obese patients) and the single injection block is time efficient. This technique is also advantageous for catheter based techniques compared to axillary approach.[2]
In our randomized controlled study, we compared a single injection vertical infraclavicular technique with a double injection axillary technique, for brachial plexus block in patients undergoing forearm and hand surgery using a combination of 2% lignocaine and 0.5% bupivacaine with the use of peripheral nerve stimulator (PNS).
METHODS
After obtaining approval from the institutional ethical committee and written informed consent, 60 patients classified as American Society of Anaesthesiologists (ASA) Grade I or II of either sex aged between 18 and 75 years scheduled for forearm and hand surgery were included in this study. Unwilling patients, patients with history of allergy to local anaesthetics, infection at local site of block, history of convulsions, bleeding disorders, cardiac, respiratory, renal or liver ailment, sensory neuropathy or motor deficit in the arm on which surgery is to be performed were excluded from the study. The patients were then allocated to receive the block either by vertical infraclavicular (group I, n=30) or axillary approach (group A, n=30) by permuted block randomization. All blocks were given by a senior anaesthesiologist using 40 ml of drug (20 ml of 0.5% bupivacaine + 10 ml of 2% lignocaine + 10 ml normal saline).
Vertical infraclavicular plexus block was achieved with the patient placed in supine position with forearm relaxed on the chest and his head turned to opposite side. Following landmarks were marked: 1) Ventral acromion process of scapula 2) Jugular fossa. The puncture site was established exactly midway between the above two landmarks, caudal and in immediate proximity of the clavicle. Following cutaneous local anaesthesia with 1 ml of 2% Lignocaine, the insulated needle (Braun® Stimuplex® Melsungen, Germany; 50 mm and 22G) was advanced in a strictly vertical direction perpendicular to the operation table, rather than the patient's skin. Using PNS (Braun® Stimuplex®, Melsungen, Germany; stimulation at 0.1 ms, ≤0.4 mA), nerve identification was done by observing an adequate motor response (flexion or extension at interphalengeal joints, wrist or elbow). Then, the total volume of drug was injected with repeated aspirations.
For the axillary approach we used a double injection technique in which the MCN was selectively stimulated in addition to any of the remaining three major nerves (median, ulnar and radial).The patient was placed in supine position with arm abducted at 90° and elbow flexed at 90°. The axillary artery was then palpated at the highest point in the axilla. After giving local anaesthesia, a 22 G insulated needle was attached to PNS using the same mode and current as in group I. First, the MCN was stimulated within the substance of coracobrachialis muscle observing arm flexion and 10 ml of the drug volume was injected to block it. Similarly, any one the major nerves (ulnar, median and radial) was stimulated within the axillary sheath as confirmed by the appropriate motor responses and the remaining volume (30 ml) of drug was injected.
Sensory evaluation was done by pin prick with a 23 G needle at an interval of 5, 10, 15, 20 and 30 minutes. The entire cutaneous innervation of upper limb i.e. musculocutaneous, radial, ulnar, median, medial cutaneous nerves of arm (MCNA) and forearm (MCNF) and intercostobrachial nerve (ICBN) were evaluated using the following scale:[5]
2 Normal sensation
1 Hypoasthesia
0 No sensation felt
A score of 0 was taken as time of onset of sensory block for that nerve. Site of surgical incision and sparing of incision site were noted.
Motor block was assessed after 5, 10, 15, 20 and 30 minutes after injection of the drug as per Lavoie and colleagues.[6]
0% - Flexion and extension in both the hand and arm against resistance
33% - Flexion and extension in both the hand and arm against gravity but not against resistance
66% - Flexion and extension movements in the hand but not in the arm
100% - No movement in the entire upper limb
Success rate was determined by Vester Anderson's criteria.[7] i.e., complete when there is Sensory block in the entire distribution of arm except axillary nerve and incomplete when nil or incomplete sensory block in some of these nerves, or failed block when there is absence of sensory block in all major nerves or presence of sensory block in only one of the nerves.
The need for intra-operative supplementary systemic medication or general anaesthesia and adverse effects (defined as: vessel puncture, seizure, new observed cardiac dysrhythmias, transcutaneous oxygen saturation lower than 90%, Horners’ syndrome, signs of local anaesthetic toxicity, unintentional paresthesias and pneumothorax) were recorded. During the surgical course, slight sedation (inj. midazolam 1-2 mg i.v) was administered if requested by the patient. In case of insufficient analgesia supplementation of block was done with inj. pentazocine (0.5 mg/kg) or inj. pentazocine (0.5 mg/kg) plus propofol infusion (50-75 mcg/kg/min). Failed blocks were converted to general anaesthesia. All patients were postoperatively monitored in the post anaesthesia care unit (PACU) for 1 h and thereafter discharged to their wards.
Post-operative pain at the incision site was assessed by visual analogue scale (VAS) and a score of more than 3 when recorded was taken as end point for duration of block and the patient was given supplementary analgesics i.e. Inj. Diclofenac Sodium 1-1.5 mg/kg intramuscular. The patients were followed up for development of pneumothorax or unintentional paresthesias.
Method of Statistical analysis
Sample size calculation was based on a projected difference of 20% in success rate among the two groups. Based on this, we calculated a sample size of minimum 30 patients per group, which would permit a type I error of alpha = 0.05 with a type II error of beta = 0.2 and a power of 0.8. The data was analyzed by using computer software Microsoft Excel and SPSS 12.0 for windows. Baseline comparability was ensured employing appropriate statistical tests. For statistical purposes the inter group comparison of sensory block was made after combining the patients who felt some sensation (sensory score 1 and 2) in one group and patients who felt no sensation (sensory score 0) in another group. Chi-square test was then employed to find the p-value at various time intervals. All analysis was two sided and a P -value of <0.05 was considered to be statistically significant.
RESULTS
There were no differences between the two groups with regard to height, weight, gender, age, duration of surgery or ASA grades. The average depth at which response was obtained was significantly greater in group I (3.87 cms) as compared to group A (2.58 cms) implying that the brachial plexus is superficial in axillary region than in infraclavicular region.
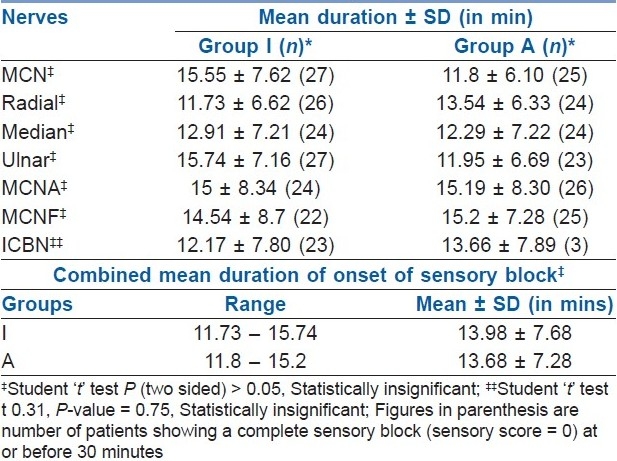
The mean duration of onset of sensory block was almost similar in both the approaches i.e. around 13.98±7.68 minutes in group I and 13.68±7.28 minutes in group A. No statistically significant difference was found on comparing the onset times of individual nerves in both the groups [Table 1].
Table 1.
Time of onset of sensory block of individual nerves in both groups
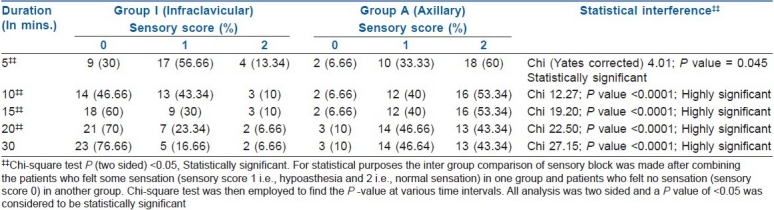
The musculocutaneous nerve (MCN) was blocked in 90% patients in the group I and in 97% of patients in group A at 30 minutes. Median and the medial cutaneous nerves of arm and forearm were blocked more in group A while the radial, ulnar, and intercostobrachial nerves were better blocked in group I. The differences between the two groups were however statistically insignificant except in case of ICBN, which was blocked significantly more in group I [Table 2]. On an average, more than 80% nerves were blocked in both the groups at 30 minutes.
Table 2.
Sensory blockade of intercostobrachial nerve at various time intervals
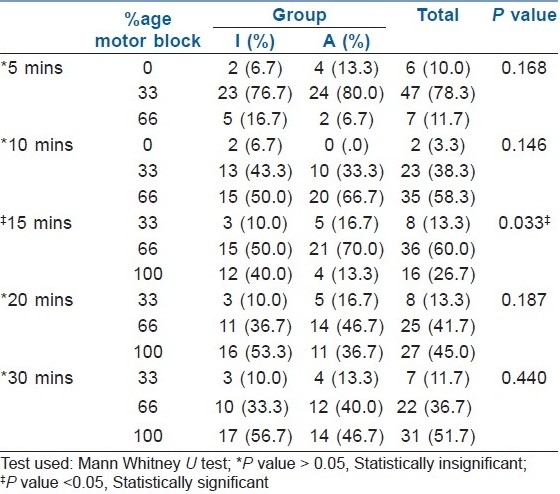
A 66-100% motor block was seen in 90% patients in infraclavicular group and 87% patients in axillary group at 30 mins. The difference was statistically insignificant [Table 3].
Table 3.
Evaluation of the degree of motor blockade at various time intervals in both groups
The mean duration of block in group I was 332±44 minutes and 338±43 minutes in group A. The difference was statistically insignificant. As per Vester Anderson's criteria , 90% patients in group I had a successful block which was higher than the 87% seen in group A but the difference was statistically insignificant. Also, the occurrence of failed block was more in group A (13%) compared to group I (10%). The difference again being statistically insignificant.
Accidental vascular puncture occurred in a significantly higher number of patients in group A (9 patients) as compared to group I (2 patients). No other complications or significant adverse effects appeared in both groups. A higher percentage of patients required supplementation in group A (23%) as compared to group I (20%). Also, 4 patients in group A required conversion to general anaesthesia compared to 3 in group I. But statistically these differences were insignificant.
DISCUSSION
Brachial plexus block is close to the ideal anaesthetic technique for upper limb surgeries for the patients, anaesthesiologists and surgeons. The axillary approach to the brachial plexus block enjoys great popularity as it is easy to perform and relatively safe. It is however problematic in patients with limited arm mobility. Also, with the standard single injection axillary block, reliable musculocutaneous nerve and radial nerve anaesthesia is limited by anatomical conditions[3] and success rates vary widely.
The vertical infraclavicular approach introduced by Kilka and colleagues[4] is the most proximal infraclavicular approach to the brachial plexus. In this approach, the brachial plexus is blocked at the cord level, which is expected to result in a wider dermatomal distribution of anaesthesia than the axillary approach.
In this study, we compared the efficacy of axillary and vertical infraclavicular approaches to brachial plexus block using a peripheral nerve stimulator. In order to overcome the anatomical disability of axillary approach in being unreliable in blocking MCN, we used a double injection technique[6] in which the MCN was selectively stimulated in addition to any of the remaining three major nerves. MCN blockade was comparable between both groups in our study. Contradictory results were obtained by Karpal and colleagues[8] and Fleishmann and colleagues[9] who in their respective studies described a higher MCN block in the infraclavicular approach compared to the axillary approach. The higher frequency of MCN blockade in the axillary approach in our study is due to selective stimulation of MCN. In the infraclavicular approach, the blockade ranges between 70-100%,[9,10] which is comparable with our study.
The radial nerve blockade seen with the axillary approach varies from 60-97% in the double injection techniques.[11,12] These results are similar to those found by us. Blockade of radial nerve achieved by us in the infraclavicular group is comparable to earlier studies.[9,10] Heid and colleagues[10] described the blockade of radial nerve in infraclavicular approach (VIB) to be significantly more than that in the axillary approach. In our study too, the blockade of radial nerve was more in group I than in group A, but the difference was not significant. Median, ulnar, MCNA and MCNF nerves were comparably blocked by both the approaches in our study. Our results are in accordance with those of the earlier authors.[2,9] Though Fleishmann and colleagues[9] documented a significantly higher block of MCNF by the VIB as compared to the axillary approach, but results similar to ours were found by Heid and colleagues.[10]
None of the previous studies to the best of our knowledge have compared the extent of blockade in the distribution of ICBN while comparing the axillary and VIBes. Blockade of ICBN provides at least a theoretical advantage of better tourniquet tolerance. Authors differ in their views regarding the blockade of ICBN in the VIB. Some authors believe that the ICBN is blocked in the infraclavicular block[13,14] while others disagree.[15] In our study, we found that the ICBN was blocked in 76.66% of patients at 30 minutes in group I, which was significantly higher to 10% success rate seen in group A [Table 2]. Bigeleisen and colleagues[16] while comparing two techniques of infraclavicular block found that the ICBN is blocked in 77-87% of the patients. These findings are similar to those found by us.
The results of our study suggest that on an average, 85% of four major nerves (MCN, Median, Radial and Ulnar) are blocked completely in both the groups at 30 minutes. Results comparable to ours have been found by other authors.[17,18] Very few studies have analysed onset times of individual nerves while comparing the two approaches. In our study, we found that the differences in the onset time of sensory block of individual nerves were insignificant. Our finding is supported by the findings of the study done by Ertug and colleagues.[2] However, the comparisons of onset time between various studies are limited by inconsistent definitions. The type of local anaesthetic, temperature of the drug and the anatomic site all influence the onset time.[10]
Different methods of assessment of motor blockade have been used by various authors making inter-study comparisons difficult. However, technically similar grades of motor blockade were found in higher number of patients in some studies[15,19] while others had comparable outcomes.[20,21]
No statistically significant difference was found between the duration of sensory block in both the approaches. The duration of block by both approaches achieved by us is comparable with earlier studies.[9,22] Using VIB, longer block durations were documented by Kilka and colleagues[4] (3–20 hours with an average of 8 hours) and Arcand and colleagues[23] (434 ± 16 minutes).
Varying rates of block success have been documented by various authors. However, the definition of “success” appears inconsistent. Some have defined success as analgesia in the distribution of nerves innervating the surgical site only[5] while others have defined it in terms of ability to perform surgery or operability.[4,24] This makes the inter-study comparison of success rates unreliable. Using Vester-Andersen's Criteria,[7] we achieved a success rate of 90% using VIB. Though the criteria varied, our success rate is comparable to that achieved by other authors.[6,15] Higher success rates with ICB have been reported if selective stimulation of posterior cord is sought.[25] Using multiple injection technique (3 or 4 injection techniques) can further increase the success rate with both the approaches,[26] however concerns have been raised regarding patient comfort during performance of these techniques.[27] No statistically significant difference was found between the success rates of infraclavicular and axillary approaches, which is in accordance with the results of other studies.[1,28] Results contradictory to ours were found by Heid and colleagues,[10] who documented a better success with VIB than with the axillary approach.
Waiting longer than 30 min may improve analgesia,[29] but is inconvenient in a busy operating theatre. Supplementation of patchy analgesia with drugs was preferred over the use of additional injections or waiting for longer periods. Both higher[30] and lower[4] requirement of supplementation as compared to our study have been described by previous authors using VIB or the axillary approach.[12,31] While comparing the infraclavicular and axillary approaches, Koscielniak-Nielsen and colleagues[26] and Heid and colleagues[10] found the differences in supplementation requirements to be statistically insignificant, thus supporting our findings.
In our study, no serious complications occurred. The most common complication was vascular puncture which was seen in significantly higher number of patients in group A. A higher rate of vessel puncture in axillary group as compared to the infraclavicular group was also found in their comparative study by Ertug and colleagues.[2] No other complications were observed by us or brought to our attention. After vertical infraclavicular plexus block, pneumothorax is possible but only a few case reports have been published. Complications of VIB can be avoided by exact adherence to the anatomic landmarks and the use of short needles with a puncture depth not exceeding 4 cm.[32]
Although the outcome assessment in our study was unblinded, the fact that no effort was made for selective nerve stimulation in either group and the endpoint that was accepted as indicating proper needle position was constant, provides objective evidence that there was no attempt, deliberate or otherwise, to influence the results of this study during the performance of the blocks. Blinded assessment too assures that there is not an opportunity to direct the study results. Also, the assessment of motor blockade was done using clearly defined objective criteria.
CONCLUSION
We have demonstrated that both techniques provide adequate surgical anaesthesia for upper limb surgeries. Both the approaches are equally efficacious as far as the onset of sensory block, extent of motor blockade, success rate, duration of block (analgesia) and supplementation required are concerned. The VIB because of its easily identifiable landmarks, a comfortable patient position during the block procedure and ability to block a larger spectrum of nerves should be thus considered as an effective alternative to the axillary approach.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Rettig HC, Gielen MJ, Boersma E, Klein J. A comparison of vertical infraclavicular and axillary approaches for brachial plexus anaesthesia. Acta Anaesthesiol Scand. 2005;49:1501–8. doi: 10.1111/j.1399-6576.2005.00816.x. [DOI] [PubMed] [Google Scholar]
- 2.Ertug Z, Yegin A, Ertem S, Sahin N, Hadimioglu N, Dösemecİ L, et al. Comparison of two different techniques for brachial plexus block: infraclavicular versus axillary technique. Acta Anaesthesiol Scand. 2005;49:1035–9. doi: 10.1111/j.1399-6576.2005.00756.x. [DOI] [PubMed] [Google Scholar]
- 3.Partridge BL, Katz J, Benirschke K. Functional anatomy of the brachial plexus sheath: implications for anesthesia. Anesthesiology. 1987;66:743–7. doi: 10.1097/00000542-198706000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Kilka HG, Geiger P, Mehrkens HH. Infraclavicular vertical brachial plexus blockade: A new technique of regional anesthesia. Anesthesist. 1995;44:339–44. doi: 10.1007/s001010050162. [DOI] [PubMed] [Google Scholar]
- 5.Miniville V, Amathieu R, Luc N, Gris C, Fourcade O, Samii K, et al. Infraclavicular brachial plexus block versus humeral approach: Comparison of anaesthetic time and efficacy. Anesth Analg. 2005;101:1198–2001. doi: 10.1213/01.ane.0000169336.25423.72. [DOI] [PubMed] [Google Scholar]
- 6.Lavoie J, Martin R, Te’trault JP, Côté DJ, Colas MJ. Axillary plexus block using a peripheral nerve stimulator: Single or multiple injections. Can J Anaesth. 1992;39:583–6. doi: 10.1007/BF03008322. [DOI] [PubMed] [Google Scholar]
- 7.Vester-Andersen T, Christiansen C, Sorense M, Eriksen C. Perivascular axillary block 1: blockade following 40 ml 1% mepivacaine with adrenaline. Acta Anaesthesiol Scand. 1982;26:519–23. doi: 10.1111/j.1399-6576.1982.tb01811.x. [DOI] [PubMed] [Google Scholar]
- 8.Kapral S, Jandrasits O, Schabernig C, Likar R, Reddy B, Mayer N, et al. Lateral infraclavicular plexus block vs.axillary block for hand and forearm surgery. Acta Anaesthesiol Scand. 1999;43:1047–52. doi: 10.1034/j.1399-6576.1999.431013.x. [DOI] [PubMed] [Google Scholar]
- 9.Fleischmann E, Marhofer P, Greher M, Waltl B, Sitzwohl C, Kapral S. Brachial plexus anaesthesia in children: lateral infraclavicular vs axillary approach. Paediatr Anaesth. 2003;13:103–8. doi: 10.1046/j.1460-9592.2003.01023.x. [DOI] [PubMed] [Google Scholar]
- 10.Heid F, Jage J, Guth M, Bauwe N, Brambrink A. Efficacy of vertical infraclavicular block vs.modified axillary plexus block: a prospective, randomized, observer blinded study. Acta Anaesthesiol Scand. 2005;49:677–82. doi: 10.1111/j.1399-6576.2005.00701.x. [DOI] [PubMed] [Google Scholar]
- 11.Coventry DM, Barker KF, Thomson M. Comparison of two neurostimulation techniques for axillary brachial plexus blockade. Br J Anaesth. 2001;86:80–3. doi: 10.1093/bja/86.1.80. [DOI] [PubMed] [Google Scholar]
- 12.Liu FC, Liou JT, Tsai YF, Li AH, Day YY, Hui YL, et al. Efficacy of Ultrasound-Guided Axillary Brachial Plexus Block: A Comparative Study with Nerve Stimulator-Guided Method. Chang Gung Med J. 2005;28:396–402. [PubMed] [Google Scholar]
- 13.Blumenthal S, Nadig M, Borgeat A. Combined infraclavicular plexus block with suprascapular nerve block for humeral head surgery in a patient with respiratory failure: Is an alternative approach really the best option for lungs. [In reply to letter to the editor]? Anesthesiology. 2004;100:190–1. doi: 10.1097/00000542-200401000-00033. [DOI] [PubMed] [Google Scholar]
- 14.Raj P, Montgomery SJ, Nettles D, Jenkins MT. Infraclavicular Brachial Plexus Block- Anew approach. Anesth Analg. 1973;52:897–904. [PubMed] [Google Scholar]
- 15.Desroches J. The infraclavicular brachial plexus block by the coracoid approach is clinically effective: An observational study of 150 patients. Can J Anaesth. 2003;50:253–7. doi: 10.1007/BF03017794. [DOI] [PubMed] [Google Scholar]
- 16.Bigeleisen P, Wilson M. A comparison of two techniques for ultrasound guided infraclavicular block. Br J Anaesth. 2006;96:502–7. doi: 10.1093/bja/ael024. [DOI] [PubMed] [Google Scholar]
- 17.Neuburger M, Kaiser H, Rembold-Schuster I, Landes H. Vertical infraclavicular block of the brachial plexus - a clinical study to the reliability of a new method for plexus anaesthesia of the upper extremity. Anaesthesist. 1998;47:595–9. doi: 10.1007/s001010050601. [DOI] [PubMed] [Google Scholar]
- 18.Fuzier R, Fourcade O, Pianezza A, Gilbert ML, Bounes V, Olivier M. A Comparison between double-injection axillary brachial plexus block and midhumeral block for emergency upper limb surgery. Anesth Analg. 2006;102:1856–8. doi: 10.1213/01.ane.0000216281.62141.9d. [DOI] [PubMed] [Google Scholar]
- 19.Borgeat A, Ekatrodamis G, Dumont C. An evaluation ofthe infraclavicular block via a modified approach of the Raj technique. Anesth Analg. 2001;93:436–41. doi: 10.1097/00000539-200108000-00040. [DOI] [PubMed] [Google Scholar]
- 20.Koscielniak-Nielsen ZJ, Horn A, Nielsen PR. Effect of arm position on the effectiveness of perivascular axillary nerve block. Br J Anaesth. 1995;74:387–91. doi: 10.1093/bja/74.4.387. [DOI] [PubMed] [Google Scholar]
- 21.Trehan V, Srivastava U, Kumar A, Saxena S, Singh CS, Darolia A. Comparison of two approaches of infraclavicular block for orthopedic surgery below mid humerus. Indian J anaesth. 2010;54:210–4. doi: 10.4103/0019-5049.65362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Waltl B, Greher M, Kabon B, Marhofer P, Karpal S. Comparison of lateral infraclavicular plexus block vs.axillary block for trauma surgery of forearm and hand in pediatric patients. Anesthesiology. 2001;95:A1235. [Google Scholar]
- 23.Arcand G, Williams SR, Chouinard P, Boudreault D, Harris P, Ruel M, et al. Ultrasound-Guided Infraclavicular Versus Supraclavicular Block. Anesth Analg. 2005;101:886–90. doi: 10.1213/01.ANE.0000159168.69934.CC. [DOI] [PubMed] [Google Scholar]
- 24.Schroeder LE, Horlocker TT, Schroeder DR. The efficacy of axillary block for surgical procedures about the elbow. Anesth Analg. 1996;83:747–51. doi: 10.1097/00000539-199610000-00015. [DOI] [PubMed] [Google Scholar]
- 25.Lecamwasam H, Mayfield J, Rosow L, Chang Y, Carter C, Rosow C. Stimulation of the Posterior Cord Predicts Successful Infraclavicular Block. Anesth Analg. 2006;102:1564–8. doi: 10.1213/01.ane.0000205750.58424.b2. [DOI] [PubMed] [Google Scholar]
- 26.Handoll HH, Koscielniak-Nielsen ZJ. Single, double or multiple injection techniques for axillary brachial plexus block for hand, wrist or forearm surgery. Cochrane Database Syst Rev. 2006;1:CD003842. doi: 10.1002/14651858.CD003842.pub2. [DOI] [PubMed] [Google Scholar]
- 27.Hu P, Harmon D, Frizelle H. Patient comfort during regional anaesthesia. J Clin Anaesth. 2007;19:67–74. doi: 10.1016/j.jclinane.2006.02.016. [DOI] [PubMed] [Google Scholar]
- 28.Koscielniak-Nielsen ZJ, Rasmussen H, Hesselbjerg L, Nielsen TP, Gürkan Y. Infraclavicular block causes less discomfort than axillary block in ambulatory patients. Acta Anaesthesiol Scand. 2005;49:1030–4. doi: 10.1111/j.1399-6576.2005.00708.x. [DOI] [PubMed] [Google Scholar]
- 29.Vester-Andersen T, Husum B, Lindeburg T, Borrits L, Gothgen I. Perivascular axillary block IV: Blockade following 40, 50, or 60 ml mepivacaine 1% with adrenaline. Acta Anaesthesiol Scand. 1984;28:99–105. doi: 10.1111/j.1399-6576.1984.tb02020.x. [DOI] [PubMed] [Google Scholar]
- 30.Gaertner E, Estebe JP, Zambia A, Cuby C, Macaire P. Infraclavicular plexus block: multiple injection versus single injection. Reg Anesth Pain Med. 2002;27:590–4. doi: 10.1053/rapm.2002.36456. [DOI] [PubMed] [Google Scholar]
- 31.Sites BD, Beach ML, Spence BC, Wiley CW, Shiffrin J, Hatrman GS, et al. Ultrasound guidance improves the success rate of a perivascular axillary plexus block. Acta Anaesthesiol Scand. 2006;50:678–84. doi: 10.1111/j.1399-6576.2006.01042.x. [DOI] [PubMed] [Google Scholar]
- 32.Neuburger M, Kaiser H, Uhl M. Biometric data on risk of pneumothorax from vertical infraclavicular brachial plexus block.A magnetic resonance imaging study. Anaesthesist. 2001;50:511–6. doi: 10.1007/s001010100170. [DOI] [PubMed] [Google Scholar]


