Abstract
OBJECTIVES
Although several studies suggest that slow gait speed is a predictor of falls, it may also be a protective mechanism to prevent falls. Further, fast walking may precipitate falls. Therefore, we examined the relationship between gait speed and falls risk.
DESIGN
Longitudinal analysis of the association between gait speed and subsequent falls and analysis of gait speed decline as a predictor of future falls
SETTING
Population-based cohort study
PARTICIPANTS
763 community-dwelling elders underwent baseline assessments and were followed for falls. Of these, 600 completed an 18-month follow-up assessment to determine change in gait speed and were followed for subsequent falls.
MEASUREMENTS
Gait speed was measured during a 4-meter walk, falls data were collected from monthly post-card calendars, and covariates were collected from in-home and clinic visits.
RESULTS
There was a U-shaped relation between gait speed and falls with faster (≥1.3 m/s, incident rate ratio (IRR) = 2.12, 95% CI = 1.48 – 3.04) and slower speeds (<0.6 m/sec, IRR = 1.60, CI = 1.06 – 2.42) at highest risk compared to normal gait speeds (≥1.0 and < 1.3 m/sec). In adjusted analyses, slower gait speeds were associated with an increased risk ratio for indoor falls (for <0.6 m/sec, IRR = 2.17, CI = 1.33 – 3.55 and for ≥0.6 and <1.0 m/sec, IRR = 1.45, CI = 1.08 – 1.94). Faster gait speed was associated with an increased risk ratio for outdoor falls (IRR = 2.11, CI = 1.40 – 3.16). A gait speed decline of >0.15 m/sec/year predicted an increased risk for all falls (IRR = 1.86, CI = 1.15 – 3.01).
CONCLUSION
There is a non-linear relation between gait speed and falls with a greater risk of outdoor falls in faster walkers and greater risk of indoor falls in slow walkers.
BACKGROUND
As falls in older adults are associated with fractures, limited mobility, institutionalization, reduced quality of life, and excess mortality, there is a need for clinical predictors of falls that can be easily measured in clinical practice1–2. Several studies have reported that slow gait speed is an independent risk factor for falls3–7,8–12. Previous studies of falls that include gait speed as a predictor variable generally assume that it is linearly associated with falls, or stratify it into fast and slow categories using a variety of cut-points. Slow gait speed may be a marker of underlying co-morbidity that is responsible for falls, rather than an etiologic factor itself13. However, some investigators have suggested that slowing of gait is an adaptive mechanism to prevent slips, trips, and falls, thereby making it possible that a slow gait speed is actually associated with a reduced risk of falls14–15. Therefore, the relationship between gait speed and falls merits further study.
Using longitudinal data from the population-based MOBILIZE Boston Study, we examined the relationship between continuous and categorical measures of gait speed and the occurrence of falls. We hypothesized that there is a non-linear relationship between gait speed and falls, such that the highest rates of falls occur in 1) more physically active individuals with faster speeds who are more often exposed to environmental hazards outside their homes, and 2) less physically active individuals with slower gait speeds who may spend little time outdoors and are more likely to fall inside. In order to distinguish the role of gait speed in these two types of fallers, we examined indoor and outdoor falls in separate analyses. In a second analysis, we examined the hypothesis that a decline in gait speed over 18 months is associated with an increased risk of falls.
METHODS
Participants
Data were obtained from the MOBILIZE Boston Study (MBS), a population-based cohort study investigating novel risk factors for falls. Subjects (N = 763, age = 78 ± 5 years, 64% female, BMI = 27.3 ± 5.1 kg/m2) were assessed at baseline and 18-month follow-up visits for demographic, clinical, functional, and cognitive characteristics and were followed monthly for falls. A complete description of the MBS design and methods has been reported previously16–17. The analysis examining change in gait speed was limited to those participants who had data from the follow-up visit (N = 600). The study was approved by the Institutional Review Board of Hebrew SeniorLife, and all subjects provided written informed consent.
Gait Speed
Gait speed was measured twice during a 4-meter walk by a research nurse at baseline and follow-up visits. Subjects started the walk from a standing position at the beginning of the 4-meter path and were instructed to walk at their usual speed. The faster of the two speeds was selected from each visit for subsequent analyses as this value was assumed to better represent their usual speed after becoming accustomed to the experimental setting. The results were similar when the average of two gait speeds was used. To examine the relationship between baseline gait speed and falls, gait speed was used as a continuous variable or split into four groups based on the distribution of gait speeds in our cohort and data from the Task Force of the International Academy on Nutrition and Aging3,13: 1) slow: <0.6 m/sec, 2) mildly abnormal: ≥0.6 m/sec and <1.0 m/sec, 3) normal: ≥1.0 m/sec and <1.3 m/sec, and 4) fast: ≥1.3 m/sec.
The change in gait speed over 18 months was calculated by subtracting the follow-up visit gait speed from the baseline visit gait speed. To assess whether declines in gait speed predict falls, four levels of gait speed decline were examined: >0 to ≤0.05, >0.05 to ≤ 0.1, 0.1 to ≤0.15, and >0.15 m/sec/year. These cut-points were based on the distribution and anchor-based analyses by Perera et. al.18, which concluded that a small meaningful change for gait speed was 0.05 m/sec. To determine a clinically meaningful decline that clinicians could use to predict falls, we used multiples of the 0.05 m/sec change that encompassed the distribution of gait speed declines in the MBS cohort. Gait speed decline was also examined as a continuous variable in our statistical analyses.
Falls Assessment
Falls were tracked using monthly post-card calendars, in which participants recorded whether or not they experienced a fall on each day16,19. Participants were instructed to mail their calendars to the study center each month. If a calendar was not received, a participant was called to collect the falls calendar information by telephone. If a fall was reported on the calendar, a falls follow-up interview was conducted to determine whether the fall occurred outdoors or indoors. A fall was defined as unintentionally coming to rest on the ground or other lower level, not as a result of a major intrinsic event or an overwhelming external hazard. Any fall episodes not classified using this definition were reviewed by an adjudication panel.
Covariates
As the causes of falls are multi-factorial, we considered the following covariates that could have contributed to fall risk or confounded its relationship to gait speed11, 20: gender, height, race, age, education level, co-morbidity, vision, arthritis of the knee or hip, executive function, depression, number of medications, use of psychotropic medications, and physical activity as measured by the Physical Activity Score for the Elderly (PASE) [23].
Height was used as a covariate as it can influence gait speed. Age was categorized into 5-year age groups. Race was categorized as white or non-white. Education was dichotomized as less than or equal to a high school education and greater than a high school education. A Snellen eye chart was used to measure visual acuity in both eyes with corrective lenses. Good vision was defined as a score of greater than 40/100. The co-morbidity index was determined by the Self-Administered Comorbidity Questionnaire21. Number of medications and PASE scores22 were all examined as continuous variables. Executive function was assessed by the generation of word lists for animals and words beginning with the letters F,A and S, Depression was assessed using a modification of the 20-item Centers for Epidemiologic Studies Depression (CES-DR) scale23. Presence of osteoarthritis was assessed by trained nurses using the American College of Rheumatology (ACR) clinical criteria.24 All variables that were significantly associated with falls in a bivariate model and were significantly different among the three baseline gait speed groups (Table 1) were included in multivariate analyses to account for potential confounders.
Table 1.
Descriptive characteristics of all subjects and different gait speed groups
| Descriptive Measure | All Participants (n=763) | Gait Speed Categories | p-value for trend | |||
|---|---|---|---|---|---|---|
| Slow (n=73) | Mildly abnormal (n=365) | Normal (n=265) | Fast (n=60) | |||
| < 0.6m/s | ≥ 0.6, < 1 m/s | ≥ 1.0, < 1.3 m/s | ≥ 1.3m/s | |||
| Age (years), mean ± SD | 78.1 ± 5.4 | 82.5 ± 5.2 | 78.7 ± 5.4 | 76.7 ± 4.8 | 75.5 ± 4.8 | <.0001 |
| Female, n (%) | 487 (64) | 54 (74) | 241 (66) | 161 (61) | 31 (52) | 0.03 |
| Caucasian, n (%) | 591 (78) | 44 (60) | 273 (75) | 222 (84) | 52 (87) | <.0001 |
| Height (m), mean ± SD | 1.64 ± 0.10 | 1.6 ± 0.1 | 1.63 ± 0.09 | 1.65 ± 0.1 | 1.7 ± 0.1 | <.0001 |
| Education > high school, n (%) | 500 (66) | 34 (47) | 212 (58) | 202 (76) | 52 (87) | <.0001 |
| Good vision (> 40/100), n (%) | 697 (92) | 55 (75) | 331 (91) | 253 (95) | 58 (97) | <.0001 |
| Physical activity, mean ± SD | 107.6 ± 70.9 | 58.5 ± 45.2 | 100.6 ± 67.5 | 122.7 ± 73.7 | 141.4 ± 67.2 | <.0001 |
| Co-morbidity, mean ± SD | 3.1 ± 1.6 | 3.9 ± 2.0 | 3.21 ± 1.6 | 2.72 ± 1.4 | 3.0 ± 1.6 | <.0001 |
| Total medications, mean ± SD | 6.0 ± 3.3 | 7.7 ± 3.3 | 6.38 ± 3.4 | 5.17 ± 2.8 | 5.3 ± 3.0 | <.0001 |
| Depression, n (%) | 51 (6.7) | 8 (11) | 33 (9) | 8 (3) | 2 (3) | 0.01 |
| Adjusted trails B, mean ± SD | 89.8 ± 63.8 | 122.8 ± 61 | 100.8 ± 68.2 | 71.9 ± 54.1 | 68.5 ± 48.5 | <.0001 |
| Knee OA, n (%) | 192 (25.2) | 26 (36) | 90 (25) | 64 (24) | 12 (20) | 0.15 |
| Psychotropic Meds, n (%) | 154 (20.2) | 13 (18) | 85 (23) | 42 (16) | 14 (23) | 0.12 |
| Word lists for letters f,a,s, , mean ± SD | 37± 15 | 31± 14 | 35± 14 | 39± 15 | 42± 13 | <.0001 |
| Animal list generation, mean ± SD | 16± 5 | 12± 4 | 15± 5 | 18± 5 | 17± 5 | <.0001 |
Analysis
Associations between categories of gait speed or gait speed declines and rates of falls were estimated using negative binomial regression models adjusted for the covariates listed above. Incidence rate ratios (IRR) and 95% confidence intervals (CI) were derived from the models. We also performed the same modeling using gait speed and gait speed decline as continuous variables. For indoor and outdoor falls, linearity assumptions were tested and the assumptions were met. Statistical significance was set at an alpha level of 0.05.
RESULTS
Sample Characteristics
763 participants were included in the analysis examining baseline gait speed and subsequent falls; 600 participants were included in the analysis of gait speed decline over 18 months and subsequent falls. Subject characteristics are shown in Table 1. The mean age of all participants at baseline was 78 ± 5 years, and the mean body mass index was 27.3 ± 5.1 kg/m2; 78% of participants were Caucasian, and 64% were female.
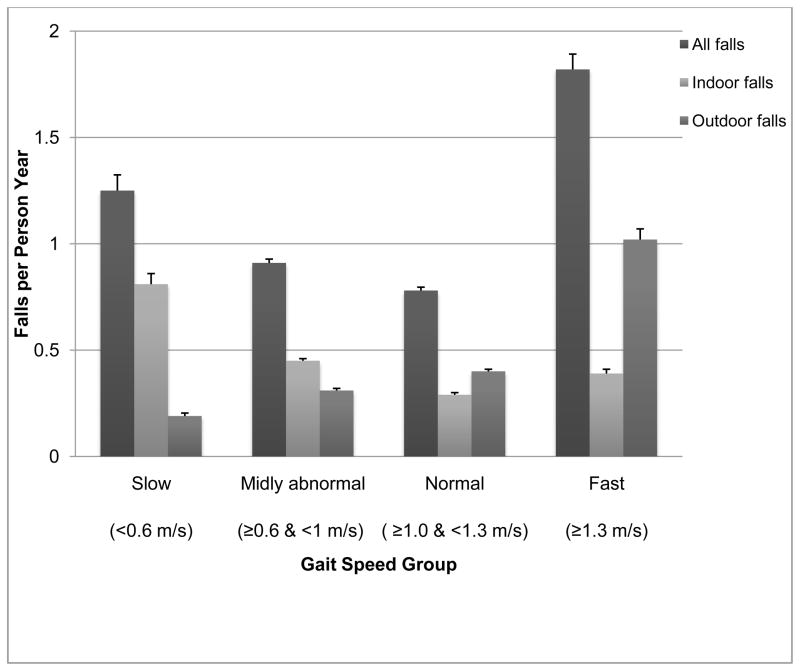
Non-linear Relationship between Gait Speed and Falls
Figure 1 illustrates the rate of falls per person per year as a function of gait speed category and location of falls, adjusted for potential confounders. For all falls, a non-linear U-shaped relationship is apparent; both extremes of walking speed show higher rates of falls compared to those in the middle categories. When stratified by indoor/outdoor location of falls, slower gait is related to an increased rate of indoor falls, whereas faster gait is related to an increased rate of outdoor falls (Table 2). The opposite slope of the relation between gait speed and fall rates for these two locations of falls accounts for the U-shaped relationship between gait speed and all falls.
Figure 1.
Relationship between gait speed groups and falls rates, stratified by location of falls.
Data are adjusted for age, race, height, education, vision, PASE score, co-morbidity, number of medications, depression, Knee Osteoarthritis, and executive function
Table 2.
Relationship between gait speed groups and falls rates
| All Falls | Indoor Falls | Outdoor Falls | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bivariate model | IRR+ | 95% CI | p-value | IRR+ | 95% CI | p-value | IRR+ | 95% CI | p-value | |||
| Slow (< 0.6 m/s) | 1.55 | 1.09 | 2.20 | 0.01 | 2.59 | 1.71 | 3.94 | <.0001 | 0.49 | 0.30 | 0.86 | 0.01 |
| Mildly abnormal (≥ 0.6 and < 1 m/s) | 1.15 | 0.92 | 1.43 | 0.21 | 1.54 | 1.17 | 2.03 | <0.01 | 0.78 | 0.60 | 1.02 | 0.07 |
| Normal (≥ 1 and < 1.3 m/s) | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Fast (≥ 1.3 m/s) | 2.22 | 1.55 | 3.17 | <.0001 | 1.26 | 0.79 | 2.03 | 0.33 | 2.53 | 1.68 | 3.83 | <.0001 |
| Multivariate model* | ||||||||||||
| Slow (< 0.6 m/s) | 1.60 | 1.06 | 2.42 | 0.03 | 2.17 | 1.33 | 3.55 | <0.01 | 0.80 | 0.45 | 1.44 | 0.46 |
| Mildly abnormal (≥ 0.6 and < 1 m/s) | 1.20 | 0.95 | 1.52 | 0.13 | 1.45 | 1.08 | 1.94 | 0.01 | 0.99 | 0.74 | 1.32 | 0.95 |
| Normal (≥ 1 and < 1.3 m/s) | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Fast (≥ 1.3 m/s) | 2.12 | 1.48 | 3.04 | <.0001 | 1.26 | 0.79 | 2.02 | 0.34 | 2.11 | 1.40 | 3.16 | <0.01 |
Multivariate model is adjusted for age, race, height, education, vision, PASE score, co-morbidity, number of medications, depression, Osteoarthritis, and executive function (word generation letters f, a, s and animal list generation).
IRR: Incidence Rate Ratio
Characteristics of Subjects with Different Gait Speeds
Group characteristics for the four categories of gait speed are described in Table 1. Compared to the other groups, slower walkers were more likely to be female, non-white, and less well educated, with poorer vision, lower physical activity, more co-morbidities, and greater number of medications. Slow walkers were also more likely to be depressed and have poor executive function as assessed by the adjusted trails B test and word or animal list generation. Faster walkers were more likely to be white and male. They were taller and had more education and physical activity than the other groups. Faster walkers also were more likely to have declines in gait speed over 18 months follow-up.
Predictive Models for Indoor, Outdoor, and All Falls
Table 2 describes the relationship between gait speed groups and 1) all falls, 2) indoor falls, and 3) outdoor falls. With regard to all falls, both the slow and fast gait speeds are associated with an increased risk of falls, with incidence rate ratios (IRRs) of 1.60 (95% CI = 1.06 – 2.42) and 2.12 (95% CI = 1.48 – 3.04), respectively in the multivariate model. When falls are separated into those that occur indoor vs. outdoor, slow gait speed is independently associated with indoor falls (IRR = 2.17, 95% CI = 1.33 – 3.55) in the multivariate model, whereas fast gait speed is independently associated with outdoor falls (IRR = 2.11, 95% CI =1.40 – 3.16) in the multivariate model.
When gait speed was included as a continuous variable in both unadjusted and adjusted regression models with indoor or outdoor fall rates as the outcome, similar results were obtained. In the adjusted model, continuous gait speed was positively associated with outdoor fall rates (IRR=2.55, 95% CI = 1.45 – 4.49), and negatively associated with indoor fall rates (IRR = 0.49, 95% CI = 0.27 – 0.87).
Decline in Gait Speed Predicts Falls
To examine whether a decline in gait speed over 18 months can predict falls, we used falls after the 18-month follow-up visit as the outcome. This analysis adjusted for falls between the baseline and 18-month follow-up visit and the same covariates used in the previous analysis.
As shown in Table 3, only a gait speed decline of more than 0.15 m/sec/year was predictive of falls (IRR = 1.86, 95%, CI = 1.15 – 3.01 in the fully adjusted model). Stratifying the analyses by indoor versus outdoor falls location revealed a similar relationship only for indoor falls. When the average of two gait speed trials was analyzed instead of the faster of the two trials, the results were also similar (IRR = 1.97, CI = 1.23 – 3.17 for a gait speed decline >0.15 m/sec/year).
Table 3.
Multivariate Model* for the Relationship between Gait Speed Decline and Subsequent Falls
| Decline in Gait Speed (meters/sec./year) | All Falls | Indoor Falls | Outdoor Falls | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| IRR+ | 95% CI | p-value | IRR+ | 95% CI | p-value | IRR+ | 95% CI | p-value | ||||
| None (n=262) | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| > 0 and ≤ 0.05 (n=160) | 1.11 | 0.81 | 1.51 | 0.51 | 1.13 | 0.77 | 1.65 | 0.53 | 1.15 | 0.78 | 1.70 | 0.47 |
| > 0.05 and ≤ 0.1 (n=90) | 0.84 | 0.56 | 1.24 | 0.37 | 0.67 | 0.40 | 1.12 | 0.13 | 0.99 | 0.61 | 1.61 | 0.97 |
| > 0.1 and ≤ 0.15 (n=40) | 1.23 | 0.70 | 2.15 | 0.47 | 1.73 | 0.94 | 3.17 | 0.08 | 0.60 | 0.24 | 1.48 | 0.27 |
| > 0.15 m/s per year (n=48) | 1.86 | 1.15 | 3.01 | 0.01 | 2.07 | 1.20 | 3.57 | 0.01 | 1.13 | 0.56 | 2.29 | 0.73 |
Multivariate model is adjusted for age, race, height, education, vision, PASE score, co-morbidity, number of medication, depression, Knee Osteoarthritis, and executive function (word generation letters f, a, s and animal list generation), and falls between the baseline and 18 month follow-up visit.
IRR: Incidence Rate Ratio
DISCUSSION
This longitudinal population-based study has three important findings: First, there was a non-linear, U-shaped relationship between gait speed and falls in community-dwelling older adults such that those with the faster and slower gait speeds were at highest risk of falls. Second, this relationship may be explained by the fact that slower walkers are less active, generally sicker, and more likely to fall inside, while faster walkers are more active and more likely to fall outside, presumably where they are exposed to environmental hazards. Finally, a decline in gait speed was an important predictor of future falls.
Our results are consistent with a previous study by Speechley and Tinetti25, which demonstrated that high and low functioning elderly people fall, but under different circumstances. Since we were unable to determine the precise cause of falls, and the cause is often multi-factorial, we can only speculate about the reasons for the different location of falls in fast and slow walkers. Unfortunately, we were unable to accurately determine the time spent indoors versus outdoors for study participants. As those with faster gait were more active than the other groups, they may have been taking greater risks in the outdoor environment. For the age range of the MOBILIZE Boston study (64–97), the faster walkers may have physical expectations that exceed their ability. Seen in their lower PASE Scores, slower-walkers are limited in their physical activity and in turn may reduce their outdoor exposure time. As a result, they may not have the same opportunity to fall outdoors as the fast-walkers. Individuals with normal walking speed may have achieved a safe balance between their expectations when outdoors and their ability to maneuver indoors, putting them at the lowest risk for falls.
Slow gait is well accepted to be associated with falls risk5, 7–8, 10, 12, 26–28, yet with few exceptions15,25 the medical literature has not emphasized the falls risk associated with fast gait. In older age, a fast gait may be a liability for an individual who does not exercise caution when navigating new terrain.
This study has also identified a relationship between a decline in gait speed and falls. The reduction in gait speed may signal a loss of physical functioning, the onset of disease, or the deterioration of motor control centers in the frontal lobe29. Although a previous statistical analysis by Perera et al18 suggested that a decline of 0.05 m/sec was a “meaningful change” when compared to self-reported ratings by community-dwelling older adults, this decline did not include a time frame and was not prospectively validated against clinical outcomes such as fall rates. Our study identified a clinically meaningful decline of 0.15 m/sec/year that can be used by clinicians to identify elderly people at risk of future falls.
This study has several limitations. The gait speed at which people were walking when they actually fell is not known. As a result, we cannot claim that a slow or fast gait speed was the direct cause of the event. Although subjects received an in-depth baseline assessment that detailed their activity levels, we were unable to construct accurate measures for the time an individual spent outdoors. Such a variable would be useful in determining whether outdoor exposure time was related to the risk of outdoor falls.
As gait speed is an easily tested measure, our study suggests that it may be a useful marker for assessing falls risk in both slower and faster walking individuals. Tracking gait speed over time may also be helpful as declines may identify people at greater risk of falls and associated injury. This study also demonstrates that the indoor or outdoor location of a fall is an important distinction that should be considered in future studies, particularly those that include gait speed as a predictor.
Acknowledgments
The authors wish to thank the loyal participants of the MOBILIZE Boston study for making this study possible. The study was funded by grants P01-AG004390, R01-AG026316, and R37-AG25037 from the National Institute on Aging, Bethesda, MD. Lien Quach was supported in part by a minority supplement to R37-AG25037. Dr. Lipsitz holds the Irving and Edyth S. Usen and Family Chair in Geriatric Medicine at Hebrew SeniorLife.
References
- 1.Cesari M, Kritchevsky SB, Newman AB, et al. Added value of physical performance measures in predicting adverse health-related events: results from the Health, Aging And Body Composition Study. J Am Geriatr Soc. 2009 Feb;57(2):251–259. doi: 10.1111/j.1532-5415.2008.02126.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Studenski S, Perera S, Wallace D, et al. Physical performance measures in the clinical setting. J Am Geriatr Soc. 2003 Mar;51(3):314–322. doi: 10.1046/j.1532-5415.2003.51104.x. [DOI] [PubMed] [Google Scholar]
- 3.Abellan van Kan G, Rolland Y, Andrieu S, et al. Gait speed at usual pace as a predictor of adverse outcomes in community-dwelling older people an International Academy on Nutrition and Aging (IANA) Task Force. J Nutr Health Aging. 2009 Dec;13(10):881–889. doi: 10.1007/s12603-009-0246-z. [DOI] [PubMed] [Google Scholar]
- 4.Cesari M, Kritchevsky SB, Penninx BW, et al. Prognostic value of usual gait speed in well-functioning older people--results from the Health, Aging and Body Composition Study. J Am Geriatr Soc. 2005 Oct;53(10):1675–1680. doi: 10.1111/j.1532-5415.2005.53501.x. [DOI] [PubMed] [Google Scholar]
- 5.Montero-Odasso M, Schapira M, Soriano ER, et al. Gait velocity as a single predictor of adverse events in healthy seniors aged 75 years and older. J Gerontol A Biol Sci Med Sci. 2005 Oct;60(10):1304–1309. doi: 10.1093/gerona/60.10.1304. [DOI] [PubMed] [Google Scholar]
- 6.Woo J, Ho SC, Yu AL. Walking speed and stride length predicts 36 months dependency, mortality, and institutionalization in Chinese aged 70 and older. J Am Geriatr Soc. 1999 Oct;47(10):1257–1260. doi: 10.1111/j.1532-5415.1999.tb05209.x. [DOI] [PubMed] [Google Scholar]
- 7.Luukinen H, Koski K, Laippala P, Kivela SL. Predictors for recurrent falls among the home-dwelling elderly. Scand J Prim Health Care. 1995 Dec;13(4):294–299. doi: 10.3109/02813439508996778. [DOI] [PubMed] [Google Scholar]
- 8.Campbell AJ, Borrie MJ, Spears GF. Risk factors for falls in a community-based prospective study of people 70 years and older. J Gerontol. 1989 Jul;44(4):M112–117. doi: 10.1093/geronj/44.4.m112. [DOI] [PubMed] [Google Scholar]
- 9.Campbell AJ, Robertson MC, Gardner MM. Elderly people who fall: identifying and managing the causes. Br J Hosp Med. 1995 Nov-Dec;54(10):520–523. [PubMed] [Google Scholar]
- 10.Chu LW, Chi I, Chiu AY. Incidence and predictors of falls in the chinese elderly. Ann Acad Med Singapore. 2005 Jan;34(1):60–72. [PubMed] [Google Scholar]
- 11.Cummings SR, Nevitt MC. Falls. N Engl J Med. 1994 Sep 29;331(13):872–873. doi: 10.1056/NEJM199409293311310. [DOI] [PubMed] [Google Scholar]
- 12.Dargent-Molina P, Favier F, Grandjean H, et al. Fall-related factors and risk of hip fracture: the EPIDOS prospective study. Lancet. 1996 Jul 20;348(9021):145–149. doi: 10.1016/s0140-6736(96)01440-7. [DOI] [PubMed] [Google Scholar]
- 13.Studenski S. Bradypedia: is gait speed ready for clinical use? J Nutr Health Aging. Dec. 2009;13(10):878–880. doi: 10.1007/s12603-009-0245-0. [DOI] [PubMed] [Google Scholar]
- 14.Nutt JG, Marsden CD, Thompson PD. Human walking and higher-level gait disorders, particularly in the elderly. Neurology. 1993 Feb;43(2):268–279. doi: 10.1212/wnl.43.2.268. [DOI] [PubMed] [Google Scholar]
- 15.Kelsey JL, Prill MM, Keegan TH, et al. Reducing the risk for distal forearm fracture: preserve bone mass, slow down, and don’t fall! Osteoporos Int. Jun. 2005;16(6):681–690. doi: 10.1007/s00198-004-1745-8. [DOI] [PubMed] [Google Scholar]
- 16.Leveille SG, Kiel DP, Jones RN, et al. The MOBILIZE Boston Study: design and methods of a prospective cohort study of novel risk factors for falls in an older population. BMC Geriatr. 2008;8:16. doi: 10.1186/1471-2318-8-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Samelson EJ, Kelsey JL, Kiel DP, et al. Issues in conducting epidemiologic research among elders: lessons from the MOBILIZE Boston Study. Am J Epidemiol. 2008 Dec 15;168(12):1444–1451. doi: 10.1093/aje/kwn277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Perera S, Mody SH, Woodman RC, Studenski SA. Meaningful change and responsiveness in common physical performance measures in older adults. J Am Geriatr Soc. 2006 May;54(5):743–749. doi: 10.1111/j.1532-5415.2006.00701.x. [DOI] [PubMed] [Google Scholar]
- 19.Hannan MT, Gagnon MM, Aneja J, et al. Optimizing the tracking of falls in studies of older participants: comparison of quarterly telephone recall with monthly falls calendars in the MOBILIZE Boston Study. Am J Epidemiol. 2010 May 1;171(9):1031–1036. doi: 10.1093/aje/kwq024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Deandrea S, Lucenteforte E, Bravi F, Foschi R, La Vecchia C, Negri E. Risk Factors for Falls in Community-dwelling Older People: A Systematic Review and Meta-analysis. Epidemiology. 2010 Jun 25; doi: 10.1097/EDE.0b013e3181e89905. [DOI] [PubMed] [Google Scholar]
- 21.Sangha O, Stucki G, Liang MH, Fossel AH, Katz JN. The Self-Administered Comorbidity Questionnaire: a new method to assess comorbidity for clinical and health services research. Arthritis Rheum. 2003 Apr 15;49(2):156–163. doi: 10.1002/art.10993. [DOI] [PubMed] [Google Scholar]
- 22.Washburn RA, Smith KW, Jette AM, Janney CA. The Physical Activity Scale for the Elderly (PASE): development and evaluation. J Clin Epidemiol. 1993 Feb;46(2):153–162. doi: 10.1016/0895-4356(93)90053-4. [DOI] [PubMed] [Google Scholar]
- 23.Eaton WW, Muntaner C, Smith C, Tien A, Ybarra M, Maruish MEe, editors. The use of psychological testing for treatment planning and outcomes assesment. 3. 3 Mahway, NJ: Lawrence Erlbaum Assoc Inc; 2004. Center for Epidemiologic Studies Depression Scale: Review and Revision (CESD and CESD-R) [Google Scholar]
- 24.Altman R, Asch E, Bloch D, et al. Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association. Arthritis Rheum. 1986;29:1039–1049. doi: 10.1002/art.1780290816. [DOI] [PubMed] [Google Scholar]
- 25.Speechley M, Tinetti M. Falls and Injuries in Frail and Vigorous Community Elderly Persons. J Am Geriatrics Soc. 1991;39:46–52. doi: 10.1111/j.1532-5415.1991.tb05905.x. [DOI] [PubMed] [Google Scholar]
- 26.Biderman A, Cwikel J, Fried AV, Galinsky D. Depression and falls among community dwelling elderly people: a search for common risk factors. J Epidemiol Community Health. 2002 Aug;56(8):631–636. doi: 10.1136/jech.56.8.631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lipsitz LA, Jonsson PV, Kelley MM, Koestner JS. Causes and correlates of recurrent falls in ambulatory frail elderly. J Gerontol. 1991 Jul;46(4):M114–122. doi: 10.1093/geronj/46.4.m114. [DOI] [PubMed] [Google Scholar]
- 28.Wolfson L, Whipple R, Amerman P, Tobin JN. Gait assessment in the elderly: a gait abnormality rating scale and its relation to falls. J Gerontol. 1990 Jan;45(1):M12–19. doi: 10.1093/geronj/45.1.m12. [DOI] [PubMed] [Google Scholar]
- 29.Ble A, Volpato S, Zuliani G, et al. Executive function correlates with walking speed in older persons: the InCHIANTI study. J Am Geriatr Soc. 2005 Mar;53(3):410–415. doi: 10.1111/j.1532-5415.2005.53157.x. [DOI] [PubMed] [Google Scholar]