Abstract
Purpose
The purpose of this study was to describe firsthand experiences with yoga as shared by adults with or at risk for type 2 diabetes and to examine their beliefs regarding maintenance of yoga practice over time.
Methods
In this qualitative study, 13 adults with or at risk for type 2 diabetes described their experiences with yoga and their beliefs regarding maintenance of yoga practice over time. Semistructured interviews occurred 16 to 20 months after completion of an 8-week yoga-based clinical trial.
Results
Themes of readiness for continuing yoga, environmental support for yoga, and integrating yoga emerged through data analysis.
Conclusions
Findings indicate that yoga is appealing to some individuals with diabetes, but maintaining yoga practice over time is a challenge. Diabetes educators may be able to support maintenance by discussing specific strategies with individuals who express interest in yoga practice.
According to a recent systematic review of the effects of yoga on clinical risk factors in adults with type 2 diabetes, multiple yoga-based intervention studies have documented improvement in a range of diabetes-related outcomes, including significant reductions in hemoglobin A1C, total cholesterol, body weight, and need for medication.1 Posited mechanisms by which yoga influences the body are (1) a reduction of sympathetic nervous system reactivity, thereby decreasing the inflammatory effects of accumulated stress, and (2) an activation of the parasympathetic response through vagal nerve stimulation, thereby elevating mood states and likewise diminishing negative neuroendocrine and inflammatory responses.1
Because of the associated induction of relaxation, self-awareness, and mindfulness, yoga practice confers psychological benefits as well, including reduced anxiety and depression.2 Specific mental health outcomes, including quality of life, stress, mood states, quality of sleep, self-esteem, overall psychological well-being, and treatment of substance abuse, improve with yoga practice, as reported in the literature.3–10
The health literature focused on yoga practice among individuals with diabetes includes reports of beneficial outcomes resulting from divergent intervention protocols. Some discuss the implementation of an intensive protocol of supervised residential yoga intervention.11–16 Others describe significant results with a protocol of weekly yoga sessions ranging from 8 weeks to 6 months; multiple studies described expectations for daily home practice.7,9,17–20 Regardless of the particular protocol, individuals who regularly practice yoga reap the greatest benefits; some consider consistency to be the most important factor in mind-body therapies.8
Despite the proliferation of yoga-based studies in recent years, few have examined the long-term benefits of yoga practice or the challenges of maintaining yoga practice over time. The purpose of this study was to describe firsthand experiences with yoga as shared by adults with or at risk for type 2 diabetes and to examine their beliefs regarding maintenance of yoga practice over time.
Methods
Study Design
The current qualitative study was a follow-up to 2 randomized controlled trials, one for men and women with type 2 diabetes (Diabetes and Yoga Study [DAYS]) and the other for healthy women at risk for diabetes and cardiovascular disease (Women’s Health and Yoga Study [WHYS]). Although the target population for these “parent studies” was different, the 2 studies had concurrent study enrollment and followed the same yoga intervention protocol. Further details regarding the DAYS and WHYS designs are described elsewhere.21–23
Human Subjects Protection
The University of Virginia Institutional Review Board for Health Sciences Research (IRB-HSR) approved the original study protocols and all protocol modifications for the current study, including guidelines for ensuring privacy and confidentiality. Written informed consent with approval for future contact was obtained from participants prior to study enrollment. Verbal consent to audio recording was obtained from interviewees prior to beginning the interviews.
Yoga Intervention: the Parent Studies
The DAYS and WHYS intervention protocol included 2 group sessions of supervised yoga instruction per week, in addition to expected home practice, over an 8-week period. The focus was Iyengar yoga, known for its gentle approach and emphasis on postures and breathing exercises easily tailored for beginners and those with or at risk for chronic illness.17,24 Iyengar yoga incorporates props such as blocks, belts, blankets, and chairs, offering support for yoga positions to prevent strain or overstretching.25An ideal role model for participants, the instructor began her study of Iyengar yoga late in life and had over 20 years of experience.
Each group session began in the late afternoon or early evening and lasted for 90 minutes. A typical session began with a brief discussion, during which participants shared concerns regarding home practice. The instructor transitioned into the yoga session by leading participants in standard yoga relaxation and centering poses (asanas), followed by active yoga exercises designed for beginners. Focused yoga breathing exercises (pranayama) were incorporated throughout the session. The instructor demonstrated modifications of yoga postures as necessary to minimize discomfort and/or prevent strain. Participants routinely used props to support positions that were difficult or uncomfortable. Toward the end of each session, the instructor led participants through a cool-down period, consisting of standard relaxation poses.
Sampling Methods for the Parent Studies
DAYS and WHYS participants were recruited through advertisements posted in community newspapers, university buildings, local venues, and medical offices. Inclusion criteria common to both trials were age range (45–80 years), postmenopausal status (for women), no yoga experience within the past year, and the ability to complete an 8-week gentle yoga program. Exclusion criteria for both trials were major orthopedic or neurological diagnoses, active joint or musculoskeletal pain, sleep apnea, and/or regular use of an assistive device.
To be included in the DAYS, one additional criterion was necessary: an established medical diagnosis of type 2 diabetes for at least 6 months. Exclusion criteria specific to the DAYS were the use of insulin, any serious chronic comorbid conditions, any acute coronary symptoms within the past 6 months, and/or an artificial pacemaker. Additional inclusion criteria specific to the WHYS were female gender, having an inactive lifestyle (exercising less than 3 times per week), and having either overweight status (body mass index [BMI] ≥25), visceral adiposity (waist circumference ≥88 cm), or a first-degree relative with diabetes or essential hypertension. Exclusion criteria specific to the WHYS were insulin sensitivity (quantitative insulin sensitivity check index [QUICKI] >0.357), use of medications affecting carbohydrate metabolism, and/or any serious chronic conditions.
Three separate cohorts were enrolled and participated in the DAYS and WHYS over a 15-month time period. The current study involved a portion of yoga intervention participants (n = 13) from the first 2 cohorts of the DAYS and WHYS, those who consented to future contact and completed 15-month postintervention follow-up questionnaires (n = 63). Interviews occurred between 16 and 20 months after study completion, based on participant availability.
Sampling Methods for the Current Study
Participants who had agreed to future contact on their signed consent forms were mailed questionnaires at 3, 6, and 15 months postintervention. Those who responded to the 15-month postintervention assessment were potentially eligible for inclusion in the current study. To elicit in-depth information about the maintenance of yoga practice, the investigator used purposive sampling. Purposive sampling is a strategy denoting the selection of “information-rich cases” that can elucidate matters of fundamental importance to the purpose of the study.26(p230) Accordingly, the investigator did not include control participants in the sampling frame because their exposure to yoga differed significantly from that of the yoga intervention participants.
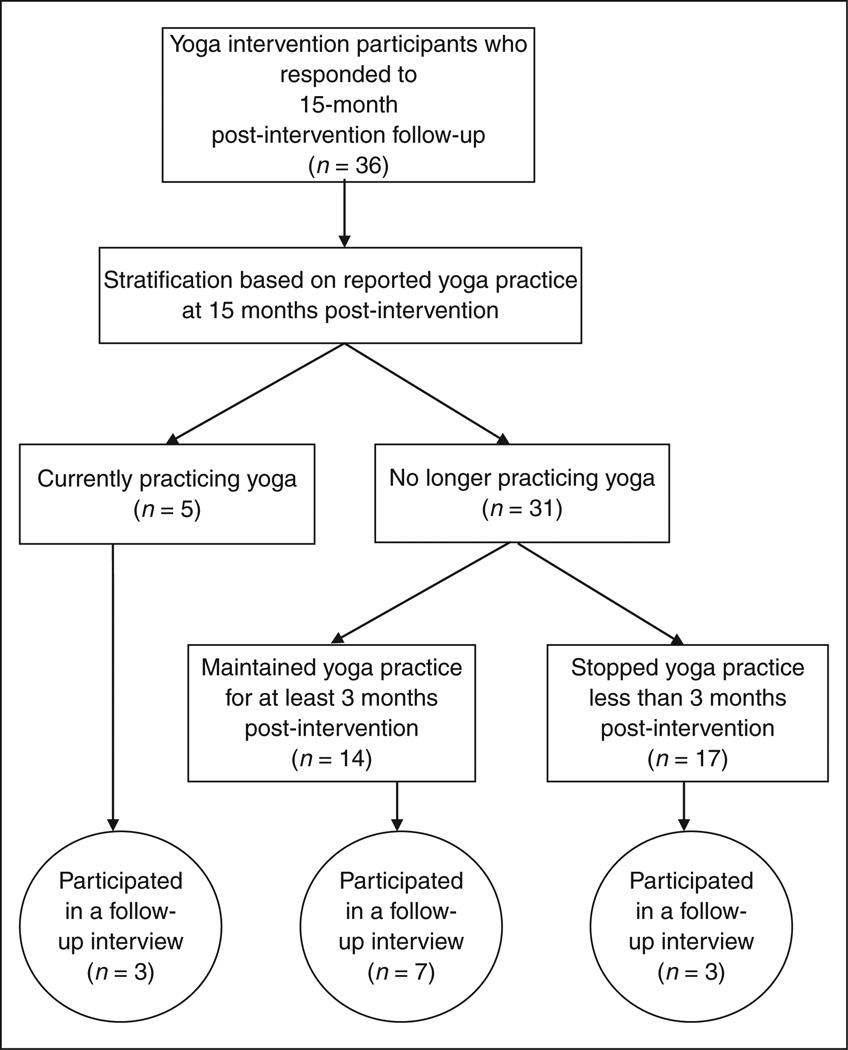
A total of 36 yoga intervention participants (88% of 41) returned the 15-month postintervention questionnaires. Stratification of the sampling frame by the reported duration of postintervention yoga practice narrowed the selection of interviewees even further. Individuals who reported practicing yoga at 15 months postintervention (n = 5) were classified as having long-term yoga practice, and those who practiced yoga for at least 3 months but fewer than 15 months postintervention were classified as having midterm yoga practice (n = 14). Individuals who stopped yoga prior to the 3-month postintervention follow-up assessment were classified as having short-term yoga practice (n = 17). See Figure 1 for a stratification flow diagram.
Figure 1.
Stratification flow diagram.
Requests for interviews began with participants who had long-term yoga practice. Of these 5 individuals, 3 agreed to participate (one of whom preferred to answer questions via e-mail), 1 declined (because of health problems), and 1 did not respond. Following that, 13 of the 14 individuals who had midterm yoga practice (one individual had health problems interfering with completion of the yoga intervention) were contacted. Of these 13 individuals, 7 agreed to participate, 4 declined (because of time constraints or health problems), and 2 did not respond.
For the individuals who reported short-term yoga practice, the investigator used a table of random numbers to determine the order of contact because there were no predetermined criteria by which to select individuals who had not maintained yoga. Interviews were requested from 6 of these individuals; 3 agreed, 2 did not respond, and 1 was unable to participate (because of distance).
Data Collection
At the DAYS and WHYS baseline assessment, each participant completed basic demographic forms, containing data such as age, gender, marital status, race/ethnicity, education, and employment. Follow-up questionnaires were administered by mail at 3, 6, and 15 months postintervention. One of these questionnaires contained a dichotomous (yes/no) response item regarding current yoga practice that was used for sampling purposes in the current study.
The primary mode of data collection in this qualitative study was face-to-face, semistructured interviews. The interview began with an assessment of the participant’s current yoga practice, followed by an inquiry regarding reasons for continuing or stopping yoga. Additional questions included the following: How would you describe a typical yoga session? What do you consider “regular” or consistent yoga practice? What makes you feel the best about doing yoga? What do you find most difficult about doing yoga on a regular basis? How would you say that practicing yoga has affected your overall lifestyle?
Each interview lasted approximately 30 to 45 minutes and was held at the participant’s chosen location. The interviews were audiotaped with the permission of the participants and transcribed verbatim into separate word-processing documents containing only study identification numbers and no personal identifiers. One participant preferred to communicate via e-mail; textual data from these e-mails were saved in a word-processing document with no personal identifiers.
Data Analysis
The investigator used the Statistical Package for the Social Sciences (SPSS) data analysis program27 (SPSS Inc, Chicago, Illinois) to calculate descriptive statistics from the DAYS and WHYS dataset, focusing on demographics and yoga practice reported at postintervention months 3, 6, and 15. Demographic differences between interviewees and noninterviewees were assessed using independent t tests and χ2 analyses, after having met the assumptions of normality and homogeneity of variance.
Each interview transcript was reviewed while listening to the corresponding audio file to confirm accuracy. Afterward, the investigator imported all of the documents into NVivo 7 (QSR International Pty Ltd, Doncaster, Victoria, Australia) to facilitate analysis.28 The textual data were read, reread, and organized into categories by the investigator, in accordance with Burnard’s staged thematic content analysis.29 Key words or phrases in each transcript were categorized by content, a process that generated many units of meaning, or codes.30 The iterative process of reading, analyzing, and coding led to the emergence of underlying meanings, known as latent content, or themes.30
Debate continues regarding the legitimacy of validation techniques in qualitative studies.31–33 Experts in qualitative inquiry describe validity in terms of trustworthiness, or the credibility of the study’s findings, which enhances confidence in the truth of the data and the analyst’s interpretation.33,34 Common threats to trustworthiness include social desirability bias and researcher bias.35 In the current study, the investigator integrated broad-based questions, assured confidentiality, and reminded participants that there were no right or wrong answers—all strategies to reduce the influence of social desirability bias.35 To reduce the influence of researcher bias, the investigator implemented 2 key strategies: (1) consultation with an experienced qualitative researcher to review the audit trail and analyze decisions about data interpretation, and (2) input from the interviewed participants during and after data analysis.
Using a process known as participant validation,31 the investigator asked the participants to review emergent themes and provide additional thoughts or criticisms regarding the extent to which the themes represented their experiences with yoga. Increasing reader access to primary data32 is another strategy to increase the trustworthiness of the findings. Toward that end, the investigator included participant quotes together with interpretative findings.
Results
Sample Characteristics
Demographic characteristics of interviewees are presented in Table 1. The average age of participants was 56 years, and the majority of interviewees were female. Most participants were white, married, and had completed 4 or more years of college. Interviewees (n = 13) were younger (P = .001) than the entire sample of 15-month postintervention respondents (n = 63), but there were no other differences between interviewees and noninterviewees (Table 2).
Table 1.
Sample Characteristics
| All | Long-Term* Yoga | Midterm* Yoga | Short-Term* Yoga | |
|---|---|---|---|---|
| N | 13 | 3 | 7 | 3 |
| Age, y | ||||
| Mean (standard deviation) | 56 (4) | 59 (3) | 53.4 (2.8) | 59 (3.6) |
| Range | 50–63 | 56–62 | 50–59 | 56–63 |
| Gender, n | ||||
| Female | 11 | 3 | 5 | 3 |
| Male | 2 | 0 | 2 | 0 |
| Marital status, n | ||||
| Not currently married | 7 | 2 | 3 | 2 |
| Currently married | 6 | 1 | 4 | 1 |
| Race/ethnicity, n | ||||
| White | 11 | 3 | 6 | 2 |
| Black | 2 | 0 | 1 | 1 |
| Education, n | ||||
| Fewer than 4 years of college | 3 | 1 | 1 | 1 |
| 4 years of college or more | 10 | 2 | 6 | 2 |
| Employment, n | ||||
| Not currently working | 5 | 2 | 1 | 2 |
| Retired | 3 | 1 | 0 | 2 |
| Homemaker | 1 | 1 | 0 | 0 |
| Unemployed | 1 | 0 | 1 | 0 |
| Currently working | 8 | 1 | 6 | 1 |
| Full time | 7 | 1 | 5 | 1 |
| Part time | 1 | 0 | 1 | 0 |
Long-term yoga = 15 or more months of yoga practice after completion of the study; midterm yoga = at least 3 months but fewer than 15 months of yoga practice after completion of the study; and short-term yoga = <3 months of yoga practice after completion of the study.
Table 2.
Comparison of Interviewees to Noninterviewees
| Interviewee | Noninterviewee | Group Difference (P Value) | |
|---|---|---|---|
| N | 13 | 50 | |
| Age, y | |||
| Mean (standard deviation) | 56.0 (4.0) | 61.7 (7.3) | .001 |
| Gender, n (%) | |||
| Female | 11 (84.6) | 44 (88.0) | .744 |
| Male | 2 (15.4) | 6 (12.0) | |
| Marital status, n (%) | |||
| Not currently married | 7 (53.8) | 20 (40.0) | .369 |
| Currently married | 6 (46.2) | 30 (60.0) | |
| Race/ethnicity, n (%) | |||
| White | 11 (84.6) | 41 (82.0) | .825 |
| Black or other ethnic minority | 2 (15.4) | 9 (18.0) | |
| Education, n (%) | |||
| Fewer than 4 years of college | 3 (23.1) | 11 (22.0) | .934 |
| 4 years of college or more | 10 (76.9) | 39 (78.0) | |
| Employment, n (%) | |||
| Not currently working | 5 (38.5) | 19 (38.0) | .976 |
| Retired | 3 (23.1) | 17 (34) | |
| Homemaker | 1 (7.7) | 1 (2.0) | |
| Unemployed | 1 (7.7) | 1 (2.0) | |
| Currently working | 8 (61.5) | 31 (62.0) | |
| Full time | 7 (53.8) | 21 (42.0) | |
| Part time | 1 (7.7) | 10 (20.0) |
Primary Themes
The following themes emerged from the processes of staged thematic content analysis: readiness for continuing yoga, environmental support for yoga, and integrating yoga. Hereinafter, the phrase “personal yoga practice” will denote yoga practiced outside of a group setting. In parentheses after each quote is the reported duration of postintervention yoga practice (short term, <3 months; midterm, at least 3 months; and long term, 15 months or more).
Theme 1: Readiness for Continuing Yoga
When asked to express primary reasons for continuing or stopping yoga, participants shared their motivation for practicing yoga and described specific barriers to yoga practice.
Motivation for yoga practice
Some participants were extrinsically motivated to practice yoga. One participant commented that “in terms of the private practice of yoga … I found I did that out of obligation” (short term). Others were motivated by the group format with hands-on instruction and accountability. One participant said, “Without the reinforcement of the class, I stopped doing it at home” (midterm). Another confessed, “I need discipline …. I’ll admit that … I’m just not good at it. I’ll do good for a while, then, okay, I got other things I can be doing besides this” (midterm).
In contrast, several participants described intrinsic motivation for yoga practice. One said, “My back feels so much better; I feel so much more relaxed. My muscles feel stronger” (long term). Another participant claimed, “I think [yoga] helped with my mood; I think it lifted my spirits …. I felt more upbeat and optimistic, and it was easier to cope with stress” (midterm). Still another said, “I feel so much healthier and have so much more energy as a result of [yoga]. And during the yoga program … I felt energized when I left …. I could move mountains” (short term).
In general, participants who reported continuing yoga practice expressed both intrinsic and extrinsic motivation for yoga, while those who stopped yoga practice primarily voiced extrinsic motivation. However, it appears that intrinsic motivation alone was not sufficient to maintain yoga practice over time, which makes it more difficult to generalize the influence of motivation on maintenance of yoga practice.
Specific barriers to yoga practice
For many participants, the perceived benefits of yoga practice did not outweigh the perceived barriers: lack of time, excessive cost, and personal inertia. One person said, “I wanna go back to it; I really do. Time is, for one thing. And the fact too that I’m just tired all the time. I am exhausted. Once I stop, literally, stop, I’m out; I’m gone, just like that …. [Work] doesn’t stop …. When you go home, there’s your next job” (midterm). Other participants expressed their desire for continued yoga instruction but indicated that the cost was prohibitive; none of the participants enrolled in a yoga class or participated in organized group yoga sessions after completing the study. Two participants stated that “expense was an issue” (midterm), and another commented, “If I could have found somewhere to go that was within my budget, I’d probably be doin’ it now. But, it’s not in my budget” (midterm). For one person, finding time was not an issue; the “problem was 30 dollars a session …. it is kind of expensive” (short term).
Some participants claimed that perceived barriers were merely an excuse for inaction. One individual admitted that “you make that kinda stuff up. I could’ve made time to do that …. I don’t know what the difficulty is; it seems so foolish to talk about it …. I’ve got to get past the thinking that I don’t have time to do [yoga]” (midterm). Another participant initially said that time was an issue because she worked late hours and weekends. However, toward the end of the interview, she claimed that “it’s just a matter of finding a time slot and sticking to it” (midterm).
Theme 2: Environmental Support for Yoga
Environmental issues were commonly mentioned by participants as they considered factors that facilitated or interfered with yoga. Aspects of the physical and social environment played a role in maintaining personal yoga practice.
Physical environment
None of the participants who reported continuing yoga practice chose to enroll in a formal yoga class or any form of organized group yoga; each of them described a home- or work-based physical environment. Although most participants practiced yoga in rooms that had another function, such as an office, guest bedroom, or living room, one participant actually dedicated space specifically for yoga practice, referring to it as a “special room in my home for yoga and meditation” (long term). Others complained of limited space at home and indicated that the spacious, peaceful atmosphere of the yoga studio was more conducive to the complete experience of yoga. However, one participant described strategies to minimize distractions and create space, facilitating relaxation and the ability to focus on yoga: “I have a small, small house. And I have dogs. So I have to go where they aren’t. Because you get on the floor and you are going to get a nose in the ear or the eye or get licked or chewed on. So I go into the living room just because I can cut out any of the other distractions … and I can move [furniture] to the side enough to get what I need for wall space. But it’s not a big space …. it’s enough to get by” (midterm).
Another participant, who lamented that she had gotten out of the habit of practicing yoga regularly at home, emphasized the freedom of yoga by saying, “Yoga—you can do anywhere. You know, there’s no equipment involved. You don’t have to have someone to do it with. You can do it alone if you need to be doing it alone” (midterm).
Social environment
The social environment played an influential role in the practice of yoga over time, based on the volume of text describing the social dimensions of yoga. Several participants valued the emotional support they found in the group sessions, which may have fostered the maintenance of yoga over time. One individual vividly recounted: “You know, it’s funny, the last day many of us cried …. I made several friends in there …. It was just that personal. And I never anticipated that. I thought it would be, you go in there and everybody in your own place, your little outfit on …. I never expected that we’d come away having made good friends and concern for each other …. I really did enjoy this a lot. And it’s over …. can I do it again?” (long term).
None of the participants decided to enroll in a yoga class following the study, but reflections on the social support and social milieu of the 8-week intervention indicated a genuine longing for the connection or bond of solidarity they felt with others in the study. One participant explained that personal yoga practice at home was unsatisfying because it could not replicate the experience of group yoga: “… there was some type of commonality, spirit maybe, between the people who were in that session. It was safe …. It was okay to be me. And it was a place where other people were doing the same thing. And I try to do it in the guest bedroom where it’s quiet, but still just knowing you’re in an environment by yourself … I couldn’t replicate that same ambience, being with other people who were focused there for a purpose, the same purpose …. And I guess that’s why I really haven’t continued it at home” (midterm).
For some participants, the instrumental support they received from others during the study was equally important. Group yoga was particularly helpful to them because others could evaluate the accuracy of their positioning. As one person commented, “You got the support, and you got somebody else looking at you doing [yoga] and … if you’re in a pose where it’s not benefiting you doing it, then they could probably see it, and they could tell [you]” (midterm).
Theme 3: Integrating Yoga
Participants who maintained yoga practice over time were able to adapt yoga to meet their needs, desires, and lifestyle. While some participants reported enjoying yoga in everyday life, others reported that yoga was an “all-or-nothing” experience. As participants described typical yoga-based activity, an array of definitions for personal yoga practice emerged.
Enjoying yoga
Descriptions of yoga revealed the manner in which participants had integrated the experience of yoga. One participant described the end of a yoga session as a “coming into home kind of feeling” and summarized yoga as “just smooth and calm and graceful … a marvelous addition to my life” (long term). The extent to which participants integrated aspects of yoga into everyday life, whether stretching poses, meditation, or breathing, was a marker for maintenance. One participant identified poses that were enjoyable and avoided those that were burdensome: “I gave up the ones [yoga poses] that were difficult for me and only occasionally go back to my materials to look for something new. I feel the ones I have are enough, as I do this more for relaxation than fitness …. [I] pretty much do what my body wants to do …. In addition, I just think yoga while at home … meaning I watch how I stand, sit, and move most of the time. It feels very useful” (long term).
All or nothing
Some participants articulated a strict, seemingly inflexible definition of yoga practice that may have led to decreased maintenance over time. One person stated, “[yoga] has to be at least 30 minutes …. you have to keep practicing and practicing those poses until you get them perfect. That takes time …. So I will go back and keep working and working until they are perfected” (midterm). Other participants explained that yoga practice is essentially “all or nothing” (midterm) or “it’s kinda like an all or none” (midterm).
A conflict was apparent for the “all-or-nothing” participants because they admitted that such an austere definition of yoga contradicted the yoga instruction they received during the study. For example, one participant, when asked to describe a consistent yoga practice, replied, “One thing I like about yoga is there’s not this, ‘you’ve gotta do it for an hour.’ I remember [yoga instructor] would say, ‘Just do this’ or ‘wake up and just do this pose for 5 minutes, 30 seconds, whatever, and don’t beat yourself up that you haven’t done a 30-minute thing.’ So I could see how it could be incorporated … [but] I still have that ‘if you don’t do it perfectly, then you’re not [doing it]’” (midterm).
Defining yoga
Participants varied in their definition of consistent yoga practice, but most focused on the time commitment, specifying that it would require more time than they usually set aside. Comments ranged from “it should be done every day” (midterm) to “at least two or three times a week” (the most common response from participants). Participants hesitated to say that they practiced yoga unless they devoted time for a focused session, as they had during the study. Although having reported stopping yoga shortly after the study ended, one participant clarified, “I don’t do the official named positions. I do a modified version for me …. I have my music [gets up and turns on the stereo] … just turn it on and will for about five minutes do this and do it three or four times a day [while at work] …. I have all kinds of yoga books. But because I’m not consistent, I don’t consider myself as practicing” (short term). Another participant reported stopping yoga after the study was over, but when reflecting on the benefits of stress reduction, she said, “I find the breathing exercises particularly beneficial …. Long term, it has been the breathing exercises and the ability to erase stress when I feel like, ‘hey, this is too much going on here, too much pressure’” (short term).
A handful of participants referred to the manifold effects of yoga that they had experienced in all aspects of life, a phenomenon that one described as “being yoga” (midterm): “When I get out of bed more quickly, I thank my yoga for making that possible. If I get down on the floor … and I can get up and I’m not creeping and crawling across the room trying to grab onto something to get up, I can thank yoga for making that possible …. yoga has a direct impact on many of the things in my life ….” (long term). Over half of the participants (n = 7) revealed patterns of yoga integration when discussing daily yoga “stretches” or describing favorite yoga poses (“mountain” pose, “dead man’s” pose, and “legs up the wall” pose were commonly stated favorites). Others (n = 2) said they appreciated the benefits of yoga but substituted other forms of physical activity, particularly walking at lunch break or hiking, in its place.
Conclusions
Based on the findings from this qualitative study, it is clear that yoga practice is an appealing and beneficial form of stress reduction and physical activity for some individuals with or at risk for type 2 diabetes. However, when the instructor’s guidance and the social support of fellow group members were removed after the study ended, most individuals tapered down their yoga practice and eventually stopped. Almost all of the participants shared a desire to begin yoga again, but common barriers were lack of time and budget constraints, a finding also described in a recent qualitative study of the barriers and benefits of yoga practice.36
Although only 3 participants identified themselves as practicing yoga at 15 months postintervention, most reported the integration of yoga elements into their everyday life up to 20 months postintervention, adapting particularly meaningful aspects of yoga to fit their needs and lifestyles. What remains unclear is the attainable benefit resulting from the integration of yoga elements as opposed to consistent yoga practice, whether privately or in a group.
Limitations
The current qualitative study findings were based upon 13 participants, which is a small sample with limited generalizability. However, as described earlier, qualitative research is more concerned with trustworthiness than generalizability to other populations.33,34 Stratified purposive sampling based on reported duration of postintervention yoga practice was intended to separate yoga maintainers from nonmaintainers, a difficult task because many individuals had integrated aspects of yoga into their lives, although they reported having stopped yoga months earlier. The measurement of yoga practice may have contributed to this problem; a dichotomous yes/no response limited participant options for description. Moreover, there was no clear distinction between personal yoga practice and group yoga practice on the questionnaire, although the difference between the two became obvious during the interviews.
Another limitation of this purely qualitative study is that there was no concurrent examination of objective diabetes-related clinical outcomes, such as A1C. Studies have indicated that improved clinical outcomes may motivate behavior change.37 It is possible that improved A1C values, for example, could enhance motivation for yoga practice, if individuals attribute such improvement to yoga practice. However, the long-term influence of this motivation is uncertain.
Implications for Practice
Iyengar yoga and other forms of gentle yoga may be an ideal fit for individuals with diabetes or prediabetes who want to increase their physical activity level and their ability to manage stress. However, findings from the current study indicate that maintaining yoga practice presents a challenge similar to that of other forms of lifestyle change. As such, it would be beneficial for diabetes educators to discuss potential maintenance strategies with individuals who express interest in yoga practice. Based on the findings from this study, such strategies would include making arrangements for continued yoga instruction, obtaining the accountability and support of a significant other, and integrating yoga into the established daily routine.
Implications for Research
Findings from this study underscore the need for further research designed to enhance the long-term maintenance of yoga practice for optimal promotion of health and prevention of disease. While evidence supporting the efficacy of yoga for diabetes prevention and control will likely continue to expand, the other cornerstones of research necessary for translation to practice—namely, the reach, adoption, and maintenance of a given intervention—are relatively scarce in the health literature.38,39
The design of future studies could include sampling among naturally occurring groups of varying sizes, such as significant other dyads, multigenerational families, neighborhoods, or church congregations. Likewise, a select number of participants could receive additional training and resources to become peer leaders who could coordinate the continuation of group yoga, thereby promoting maintenance of yoga practice over time. To advance the evidence base for clinical practice, researchers can implement and evaluate resourceful protocols such as the rerandomization of study participants to specific maintenance programs upon completion of the intervention, an approach used in the Mediterranean Lifestyle Program, a randomized controlled trial among women with type 2 diabetes.40
Improvements in measurement are necessary as well, beginning with attempts to standardize the assessment of personal yoga practice. The DAYS and WHYS intervention was designed using a group format; therefore, it is possible that the participants’ preference for group yoga may have been an artifact of the group design. Additional possibilities for future research include feasibility studies using various approaches to individual or self-paced yoga instruction.
Acknowledgments
This research was supported in part by the University of Virginia Institute on Aging, grant numbers R21-AT-0002982 and 1-K01-AT-004108 from the National Center for Complementary and Alternative Medicine (NCCAM) and the Office of Women’s Health (OWH), and grant number T32-AT-000052 from NCCAM. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the University of Virginia, NCCAM, OWH, or the National Institutes of Health. Without the exceptional transcription of Mrs Karen Johnson, neither data analysis nor article development would have been possible. We are deeply grateful for her time and attention to detail.
References
- 1.Innes KE, Vincent HK. The influence of yoga-based programs on risk profiles in adults with type 2 diabetes mellitus: a systematic review. eCAM. 2007;4:469–486. doi: 10.1093/ecam/nel103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Somani SM, Bhat SG, Bera TK, Hollinger MA. Pharmacological aspects of yoga. In: Somani SM, editor. Pharmacology in Exercise and Sports. Boca Raton: CRC Press; 1996. [Google Scholar]
- 3.Brazier A, Mulkins A, Verhoef M. Evaluating a yogic breathing and meditation intervention for individuals living with HIV/AIDS. Am J Health Promot. 2006;20:192–195. doi: 10.4278/0890-1171-20.3.192. [DOI] [PubMed] [Google Scholar]
- 4.Brown RP, Gerbarg PL. Sudarshan Kriya yogic breathing in the treatment of stress, anxiety, and depression. Part I: neurophysiologic model. J Altern Complement Med. 2005;11:189–201. doi: 10.1089/acm.2005.11.189. [DOI] [PubMed] [Google Scholar]
- 5.Brown RP, Gerbarg PL. Sudarshan Kriya yogic breathing in the treatment of stress, anxiety, and depression. Part II: clinical applications and guidelines. J Altern Complement Med. 2005;11:711–717. doi: 10.1089/acm.2005.11.711. [DOI] [PubMed] [Google Scholar]
- 6.Manjunath NK, Telles S. Influence of yoga and Ayurveda on self-rated sleep in a geriatric population. Indian J Med Res. 2005;121:683–690. [PubMed] [Google Scholar]
- 7.Oken BS, Zajdel D, Kishiyama S, et al. Randomized, controlled, six-month trial of yoga in healthy seniors: effects on cognition and quality of life. Altern Ther Health Med. 2006;12:40–47. [PMC free article] [PubMed] [Google Scholar]
- 8.Rice BI. Mind-body interventions. Diabetes Spectrum. 2001;14:213–217. [Google Scholar]
- 9.Roth B, Creaser T. Mindfulness meditation-based stress reduction: experience with a bilingual inner-city program. Nurse Pract. 1997;22:150–152. 154, 157 passim. [PubMed] [Google Scholar]
- 10.Woolery A, Myers H, Sternlieb B, Zeltzer L. A yoga intervention for young adults with elevated symptoms of depression. Altern Ther Health Med. 2004;10:60–63. [PubMed] [Google Scholar]
- 11.Agte VV, Tarwadi K. Sudarshan Kriya yoga for treating type 2 diabetes: a preliminary study. Altern Complement Ther. 2004;10:220–222. [Google Scholar]
- 12.Jain SC, Uppal A, Bhatnagar SO, Talukdar B. A study of response pattern of non-insulin dependent diabetics to yoga therapy. Diabetes Res Clin Pract. 1993;19:69–74. doi: 10.1016/0168-8227(93)90146-v. [DOI] [PubMed] [Google Scholar]
- 13.Malhotra V, Singh S, Tandon OP, Madhu SV, Prasad A, Sharma SB. Effect of yoga asanas on nerve conduction in type 2 diabetes. Indian J Physiol Pharmacol. 2002;46:298–306. [PubMed] [Google Scholar]
- 14.Malhotra V, Singh S, Singh KP, et al. Study of yoga asanas in assessment of pulmonary function in NIDDM patients. Indian J Physiol Pharmacol. 2002;46:313–320. [PubMed] [Google Scholar]
- 15.Singh S, Malhotra V, Singh KP, Madhu SV, Tandon OP. Role of yoga in modifying certain cardiovascular functions in type 2 diabetic patients. J Assoc Physicians India. 2004;52:203–206. [PubMed] [Google Scholar]
- 16.Kosuri M, Sridhar GR. Yoga practice in diabetes improves physical and psychological outcomes. Metab Syndr Relat Disord. 2009;7:515–517. doi: 10.1089/met.2009.0011. [DOI] [PubMed] [Google Scholar]
- 17.DiBenedetto M, Innes KE, Taylor AG, et al. Effect of a gentle Iyengar yoga program on gait in the elderly: an exploratory study. Arch Phys Med Rehabil. 2005;86:1830–1837. doi: 10.1016/j.apmr.2005.03.011. [DOI] [PubMed] [Google Scholar]
- 18.Williams KA, Petronis J, Smith D, et al. Effect of Iyengar yoga therapy for chronic low back pain. Pain. 2005;115:107–117. doi: 10.1016/j.pain.2005.02.016. [DOI] [PubMed] [Google Scholar]
- 19.Yang K, Bernardo LM, Sereika SM, Conroy MB, Balk J, Burke LE. Utilization of 3-month yoga program for adults at high risk for type 2 diabetes: a pilot study. Evid Based Complement Alternat Med. 2009 Aug 18; doi: 10.1093/ecam/nep117. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Skoro-Kondza L, Tai SS, Gadelrab R, Drincevic D, Greenhalgh T. Community based yoga classes for type 2 diabetes: an exploratory randomised controlled trial. BMC Health Serv Res. 2009;9:33–40. doi: 10.1186/1472-6963-9-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Innes K, Selfe T, Taylor AG, Cottingham S, Hasan S, Alexander G. Effects of a gentle Iyengar yoga program on glucose tolerance and related indices of cardiovascular disease risk in adults with type 2 diabetes. Int J Yoga Therapy. 2008;18:34–35. [Google Scholar]
- 22.Innes K. The potential benefits of yoga therapy for the prevention and control of diabetes and cardiovascular disease: evidence, possible pathways, and future directions; Paper presented at: North American Research Conference on Complementary & Integrative Medicine; Minneapolis, Minnesota: 2009. May 12–15, [Google Scholar]
- 23.Innes K. Potential role of yoga therapy for the reduction of cardiovascular disease risk and diabetes management; Paper presented at: Symposium on Yoga Therapy and Research; Los Angeles, California: 2009. Mar 5–8, [Google Scholar]
- 24.Kolasinski SL, Garfinkel M, Tsai AG, Matz W, Van Dyke A, Schumacher HR. Iyengar yoga for treating symptoms of osteoarthritis of the knees: a pilot study. J Altern Complement Med. 2005;11:689–693. doi: 10.1089/acm.2005.11.689. [DOI] [PubMed] [Google Scholar]
- 25.Garfinkel M, Schumacher HR., Jr Yoga. Rheum Dis Clin North Am. 2000;26:125–132. doi: 10.1016/s0889-857x(05)70126-5. [DOI] [PubMed] [Google Scholar]
- 26.Patton MQ. Qualitative Research and Evaluation Methods. 3rd ed. Thousand Oaks, California: Sage Publications; 2002. [Google Scholar]
- 27.SPSS: The Predictive Analytics Company. [Accessed March 16, 2009];SPSS statistics: 2009. Available at: http://www.spss.com/statistics/ [Google Scholar]
- 28.QSR International. [Accessed February 20, 2009];NVivo. Available at: http://www.qsrinternational.com/products_nvivo.aspx. [Google Scholar]
- 29.Burnard P. A method of analysing interview transcripts in qualitative research. Nurse Educ Today. 1991;11:461–466. doi: 10.1016/0260-6917(91)90009-y. [DOI] [PubMed] [Google Scholar]
- 30.Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24:105–112. doi: 10.1016/j.nedt.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 31.Silverman D. Interpreting Qualitative Data: Methods for Analysing Talk, Text, and Interaction. 2nd ed. Thousand Oaks, California: Sage Publications; 2001. [Google Scholar]
- 32.Wolcott HF. Transforming Qualitative Data: Description, Analysis, and Interpretation. Thousand Oaks, California: Sage Publications; 1994. [Google Scholar]
- 33.Sandelowski M, Barroso J. Reading qualitative studies. Int J Qualitative Methods. 2002;1:74–108. [Google Scholar]
- 34.Cochrane Qualitative Research Methods Group. Quality appraisal of qualitative studies. [Accessed March 9, 2009]; Available at: http://www.joannabriggs.edu.au/cqrmg/documents/Quality%20Appraisal%20of%20Qualitative%20Studies.pps. [Google Scholar]
- 35.Polit DF, Beck CT. Nursing Research: Principles & Methods. 7th ed. Philadelphia: Lippincott Williams & Wilkins; 2004. [Google Scholar]
- 36.Atkinson NL, Permuth-Levine R. Benefits, barriers, and cues to action of yoga practice: a focus group approach. Am J Health Behav. 2009;33:3–14. doi: 10.5993/ajhb.33.1.1. [DOI] [PubMed] [Google Scholar]
- 37.Parkin CG, Hinnen D, Campbell RK, Geil P, Tetrick DL, Polonsky WH. Effective use of paired testing in type 2 diabetes: practical applications in clinical practice. Diabetes Educ. 2009;35:915–927. doi: 10.1177/0145721709347601. [DOI] [PubMed] [Google Scholar]
- 38.Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. 1999;89:1322–1327. doi: 10.2105/ajph.89.9.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Glasgow RE, Lichtenstein E, Marcus AC. Why don’t we see more translation of health promotion research to practice? Rethinking the efficacy-to-effectiveness transition. Am J Public Health. 2003;93:1261–1267. doi: 10.2105/ajph.93.8.1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Barrera MJ, Strycker LA, MacKinnon DP, Toobert DJ. Social-ecological resources as mediators of two-year diet and physical activity outcomes in type 2 diabetes patients. Health Psychology. 2008;27:S118–S125. doi: 10.1037/0278-6133.27.2(Suppl.).S118. [DOI] [PubMed] [Google Scholar]