Abstract
Diversifying the health professional workforce and enhancing cultural competence are recommended for decreasing health disparities. We tested a structural equation model of the predictors of culturally competent behaviors in a mailed survey of three groups of underrepresented nurse practitioners (n = 474). Our model had good fit and accounted for 29% of the variance in culturally competent behaviors. Life experiences with diversity had direct effects on awareness/sensitivity and behaviors, and diversity training had a direct effect on behaviors. Cultural awareness/sensitivity mediated the relationship between life experiences with diversity and culturally competent behaviors; all paths remained after controlling for covariates. For unique experiences that contribute to work-place diversity, life experiences with diversity, and diversity training are important for culturally competent behaviors.
Keywords: advanced practice, culture diversity, discrimination/barriers to care, LISREL/SEM/path analysis
Enhancing cultural competence and expanding diversity among health professionals have been cited as two key strategies in the quest to decrease health disparities for persons of color and ethnic/cultural minorities (Fortier & Bishop, 2004; National Center for Cultural Competence, 2009; Smedley, Stith Butler, & Bristow, 2004). Providers, like the patients they care for, are diverse in their world views, their attitudes toward growing diversity in U.S. demographics, and their personal life experiences with diverse communities (Ahmann, 2002). Yet little is known about cultural competence knowledge, attitudes, and behaviors of underrepresented health care providers. The majority of U.S. nurse practitioners (NPs) are non-Hispanic White females, and in most studies of cultural competence non-Hispanic White participants are overrepresented. Research is needed to determine how workplace diversity translates into cultural competence among diverse groups; however, the limited number of NPs of color and male NPs has made access to these groups a sampling challenge (Goolsby, 2005; Smedley et al., 2004). The purpose of this study was to examine a model of culturally competent care in three underrepresented NP groups: Asian American men and women, African American/Black men and women, and non-Hispanic White men.
THREE-DIMENSIONAL PUZZLE MODEL OF CULTURALLY CONGRUENT CARE
A theoretical model of cultural competence and culturally congruent care (Schim, Doorenbos, Benkert, & Miller, 2007) informed the current study. The model uses the analogy of a three-dimensional jigsaw puzzle in which cultural competence elements come together at both the provider and patient levels. The provider level includes four components: (a) cultural diversity, (b) cultural awareness, (c) cultural sensitivity, and (d) culturally competent behaviors (CCBs). Cultural diversity is defined broadly and includes features of race/ethnicity, sexual orientation, socioeconomic status, physical and mental impairment (including HIV status), education, and terminal illness. Cultural awareness is a knowledge or cognitive construct. Knowledge of a culture or cultural group and the cognitive ability to explore cultural nuances are necessary to appreciate the profound effects culture has on healthcare. Cultural sensitivity is an affective or attitudinal construct. A clinician’s attitudes and receptivity to exploring the multiple dimensions of culture in both self and others are essential. Cultural competence is a behavioral construct. CCBs consist of actions taken in response to the exposure to cultural diversity, the comprehension of cultural awareness, and the attitudinal shifts in cultural sensitivity. Putting experience, knowledge, and attitude to work in patient encounters demonstrating CCBs is the desired outcome of professional education and development.
CULTURAL DIVERSITY EXPERIENCES AND CULTURAL COMPETENCE
Theoretically greater breadth of experience with diverse patients in the work setting should be associated with greater competence scores; however, research indicates that work experience/exposure alone does not consistently lead to enhanced cultural competence (Benkert, Pohl, & Coleman-Burns, 2004; Cooper Brathwaite, 2006; Smith-Campbell, 2005). In fact, Cooper Brathwaite (2006) found that years of work experience negatively correlated with cultural knowledge and competence. Schim et al. (2006) argued that simple measures of work experience with diversity may be insufficient to capture the full range of experiences and have recommended expanding measures to include life experiences and additional cultural categories (e.g., gay/transgender).
Life experiences with diverse groups have been found to enhance cultural competence. Although researchers have found that health professionals report feeling more knowledgeable about specific groups they have encountered in their work settings and more confident in their interactions (Hagman, 2006; Joseph, 2004; Kardong-Edgren et al., 2005; Sargent, Sedlak, & Martsolf, 2005), few researchers have described the distinct impact of one’s personal life experiences. What is known is that a lack of experiences with diversity can lead to a discrete and narrowly-defined understanding of and discomfort with cultural differences (Benkert et al., 2004; Ciesielka, Schumacher, Conway, & Penrose, 2005; Reeves & Fogg, 2006). A “total immersion” experience (or a concentrated life experience with diverse groups) can maximize cultural competence through a shift in attitudes and knowledge (Beach et al., 2005; Godkin & Savageau, 2001; Sargent et al., 2005), yet these interventions are time- and resource-intensive and difficult to justify beyond research or educational opportunities (Beach et al., 2005).
CULTURAL AWARENESS AND CULTURAL COMPETENCE
Evaluations of the effect of diversity training on knowledge (cultural awareness) of cultural groups have dominated the cultural competence literature (Beach et al., 2005; Cooper Brathwaite, 2006; Kardong-Edgren et al., 2005). Using the Cultural Competence Assessment (CCA), researchers (Doorenbos, Schim, Benkert, & Borse, 2005; Schim, Doorenbos, & Borse, 2005; Schim, Doorenbos, & Borse, 2006) have found that cultural awareness training enhanced cultural competence (awareness, sensitivity, and behaviors) among a variety of health professionals. From a set of independent variables, only prior diversity training was significantly associated with CCB (p = .011). The findings, however, have not been tested in a model beyond a single regression path (Schim et al., 2005).
CULTURAL SENSITIVITY AND CULTURAL COMPETENCE
Cultural sensitivity involves the recognition of personal attitudes, values, beliefs, and practices. Educational attainment, self-identified race/ethnicity, and diversity training explain a portion (11%) of the variance in cultural sensitivity (Schim et al., 2005; see also Schim et al., 2006). Yet, to date, researchers have not tested the assumption that cultural awareness and sensitivity mediate the path between training and behaviors. More work is needed to identify the paths to CCBs and ultimately to culturally congruent care.
For years, nursing writers have assumed that advocating a primary ethics of care orientation is synonymous with being patient centered and culturally competent (Black, 2005). Yet, nursing researchers have used simple measures of cultural attitudes as proxies for ethical beliefs, ignoring the totality of the person’s moral positions. An increasingly popular alternative to the ethics of care orientation is social justice. Social justice is a complex construct incorporating a communitarian philosophy focusing on community investment in health, equitable distribution of health care, and community-derived rationing models (Drevdahl, Kneipp, Canales, & Dorcy, 2001; Giddings, 2005; Reimer Kirkham, Van Hofwegen, & Hoe Harwood, 2005). One aspect of social justice is distributive justice, which denotes fair distribution of resources and burdens. No studies were found that evaluated the impact of distributive justice (or the broader concept of social justice) on cultural competence. Still, Schim, Benkert, Bell, Walker, and Danford (2007) suggested that social justice be considered a fifth meta-paradigm for nursing science. Recognizing this shifting paradigm, we sought to extend the current literature by separating cultural sensitivity from other ethical orientations (i.e., distributive justice).
SOCIAL DESIRABILITY ASSESSMENTS AND CULTURAL COMPETENCE
Self-report measurements of cultural competence may be influenced by social desirability (a desire to look good to others; Constantine & Ladany, 2000). Researchers have begun to use social desirability assessments to control for this variable in studies of cultural competence among multicultural counseling professionals and graduate students in training (Constantine & Ladany, 2000; Spanierman, Poteat, Wang, & Oh, 2008). We found no studies of NPs using social desirability as a confounder of self-reported cultural competence. Yet, as with most studies of nurses, participants in research of counseling professionals are predominantly non-Hispanic White females (Constantine & Ladany, 2000). One study using a small sample (n = 55) of practicing counselors and intern graduate students who were predominately non-Hispanic White females found that social desirability was positively correlated with one aspect of CCBs, relationship skills, but not with cultural competence in knowledge (or awareness) (Worthington, Mobley, Franks, & Tan, 2000). Female gender alone has been correlated with social desirability (Spanierman et al., 2008; Worthington et al., 2000), but few researchers have explored these correlations in any depth even among larger samples of non-Hispanic White participants (Spanierman et al., 2008; n = 311).
DEMOGRAPHICS AND CULTURAL COMPETENCE
Demographic assessments are obtained in studies of cultural competence, yet correlations between variables identified in these studies are inconsistent. Higher education among nurses has been positively associated with cultural competence (Cooper Brathwaite, 2006; Sargent et al., 2005); however, in one study higher education was associated with lower cultural self-efficacy (Hagman, 2006). Using the Schim-Doorenbos Cultural Competence Assessment (SD, CCA), researchers (Doorenbos & Schim, 2004; Schim et al., 2005, 2006) found higher education was associated with cultural competence knowledge, sensitivity, and behaviors; it is important to note that over 70% of their respondents had less than the master’s degree preparation characteristic of NPs. The studies primarily included certificate trained (i.e., nursing assistants), diploma, and associate and baccalaureate degree nurses.
Even less consistent is the association between cultural competence and gender and/or racial/ethnic background of NPs. Women rated their cultural competence sensitivity higher than men (Hagman, 2006; Joseph, 2004; Spanierman et al., 2008), but cultural competence knowledge levels were not associated with a particular gender. Still, few researchers studying cultural competence have included male providers or providers of color. In four studies of nurses with sample sizes sufficient to accept generalizability of the results (Hagman, 2006; Joseph, 2004; Schim et al., 2005, 2006); only two found an association between race/ethnicity and cultural competence (Hagman, 2006; Joseph, 2004).
Sexual orientation and income of NPs are rarely assessed despite the role these variables may play in cultural competence. We found no studies assessing these variables as predictors of cultural competence knowledge, sensitivity, or behaviors. There has been limited attention to sexual orientation in cultural competence training and education (Braye, Preston-Shoot, & Thorpe, 2007), which may explain why discomfort in caring for gay/lesbian and transgender individuals continues (Benkert, Tanner, Guthrie, Oakley, & Pohl, 2005).
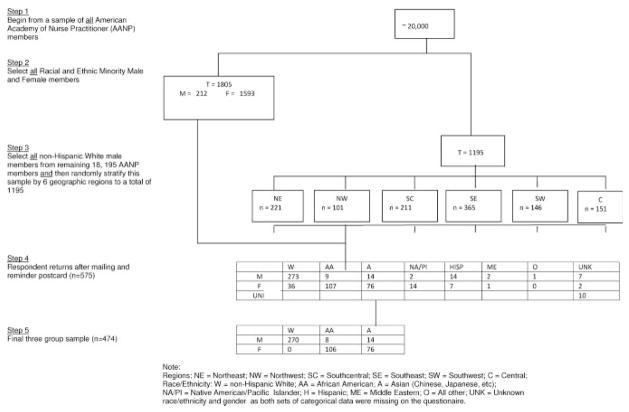
In summary, research on cultural competence among NPs is in its infancy. Little is known about the precursors, beyond formal diversity training, required to actualize CCBs in NPs. No researcher has tested a model of predictors for CCBs. Researchers have yet to test the model beyond single regression path assessments, perhaps because they studied small, relatively homogenous samples. Using the theoretical and empirical literature as a guide, the authors of the present study constructed a model to predict CCBs (Fig. 1). The model tests the following hypotheses in a unique sample of underrepresented NPs:
FIGURE 1.
Hypothesized model of cultural competence behavior among traditionally underrepresented NPs. The pathways from other covariates—sexual orientation, income, and age—were included in the model tested but omitted here to highlight predictions from the literature. Note: Key for variables and symbols. Age, age of participant; Income, annual income of participant; Sexual Orientation, self-identified sexual orientation of participant; Education, education of participant; Social Desirability, perceptions of need to provide socially desirable responses; Life Experience, life experiences with diverse individuals; Social Justice, perceptions of social justice beliefs; Diversity Training, amount of diversity training; Cultural Awareness, perceptions of cultural awareness; Cultural Competent Behaviors, perceptions of performing culturally competent behaviors in practice. Oval picture, latent variable.
Diversity training, social justice beliefs, and life experiences with diversity will have a positive effect on cultural awareness/sensitivity and CCBs.
Cultural awareness/sensitivity will mediate the positive effects of diversity training, social justice beliefs, and life experiences with diversity on CCBs.
These effects will hold up when controlling for social desirability, education, and the other covariates of sexual orientation, income, and age.
METHOD
Design
In this cross-sectional descriptive study, we analyzed survey data using structural equation modeling techniques (SEM). SEM was chosen because it can provide evidence of causality with cross-sectional data and it is an alternative to experimentation for examining hypothesized models (Byrne, 2001).
Procedures
The principal investigator and two research assistants mailed a questionnaire booklet, an information letter, and a pre-stamped return envelope to pre-identified American Academy of Nurse Practitioner (AANP) members; non-respondents were sent one reminder post card. The members were also sent lapel stickers as an incentive, and the first 100 respondents were entered into a drawing to receive a gift certificate equivalent to an early conference fee. Data were collected between September 2005 to March 2006.
Sample
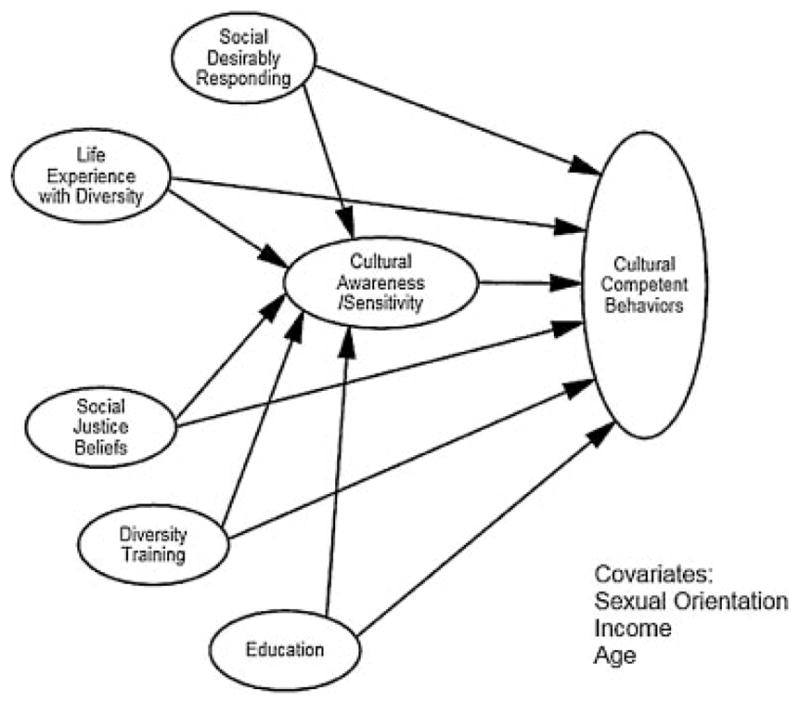
After receiving human subjects’ approval, the PI worked with the Director of Research at the AANP to develop a plan that would accomplish the study purpose of sampling for underrepresented groups and accommodate a budgetary limit of 3,000 participants. Briefly, the staff at AANP first identified from the total AANP membership (n = ~20,000) all members who did not self-identify as non-Hispanic White, which yielded 1,805 members who were from racial or ethnic minority groups. To achieve a total sample of 3,000 participants, 1,195 additional participants were needed; thus the AANP staff randomly selected from self-identified non-Hispanic White males a geographically stratified sample until 1,195 members were identified. Figure 2 provides a visual representation of the sampling strategy. The racial/ethnic minority members and the stratified random sample of non-Hispanic White male members who received the initial mailing totaled 2,840 (160 mailed packets were returned due to incorrect addresses). The response rate was just over 20%, with 575 participants responding to the mailing. Several respondents were removed prior to the final analysis: 24 because they were missing all three critical self-identification data points (race/ethnicity, gender, and sexual orientation), 40 because their racial or ethnic group size was insufficient for multi-group SEM analyses, and 37 because they self-identified as non-Hispanic White females. The final sample was 474 respondents from three underrepresented NP groups: non-Hispanic White men (n = 270), Asian American men and women (n = 90), and African American/Black men and women (n = 114). The final sample retained both men and women of Asian American and African American/Black descent because the subgroups would have been too small for the Multi-group SEM analyses. Mean age of respondents was 46.52 (range 26–74) years, and the majority (n = 459; 96.8%) had at least a master’s degree education. Demographics of the sample are presented in Table 1.
FIGURE 2.
Steps in the stratified sampling plan to the final sample retained for analysis (n = 474).
Table 1.
Sample Demographics and Diversity Experiences in Work and Life (n = 474)
| Variable | n (%) |
|---|---|
| Gender | |
| Male | 292 (61.6) |
| Female | 182 (38.4) |
| Race or ethnicity | |
| Non-Hispanic White males | 270 (57.0) |
| African American/Black males and females | 114 (24.0) |
| Asian/Hawaiian/Pacific Islander males and females | 90 (19.0) |
| Faith tradition | |
| Protestant | 234 (49.4) |
| Roman Catholic | 107 (22.6) |
| None | 105 (22.2) |
| Buddhist/Hindu | 16 (3.4) |
| Jewish | 9 (1.9) |
| Other (e.g., Greek Orthodox) | 3 (0.5) |
| Sexual orientation | |
| Straight/heterosexual | 428 (90.3) |
| Gay/all other | 46 (9.7) |
| Percent of NPs with some work exposure to: | |
| Non-Hispanic Black/African American | 457 (96.4) |
| Hispanic/Latino | 443 (93.5) |
| Arab American/Middle Eastern | 352 (74.3) |
| Native American | 301 (63.5) |
| Low income | 440 (92.8) |
| Mentally disabled | 429 (90.5) |
| Asian American | 423 (89.2) |
| Gay/transgender/lesbian | 419 (88.4) |
| Terminally ill | 391 (82.5) |
| HIV+ | 390 (82.3) |
| Homeless | 362 (76.4) |
| Percent of NPs with “a lot of” personal life experience witha | |
| Non-Hispanic Black/African American (n = 471)b | 297 (62.7) |
| Low income (n = 471) | 238 (50.2) |
| Asian American (n = 471) | 144 (30.4) |
| Terminally ill (n = 467) | 117 (24.7) |
| Gay/transgender/lesbian (n = 469) | 99 (20.9) |
| Mentally disabled (n = 469) | 93 (19.6) |
| Homeless (n = 470) | 82 (17.3) |
| HIV+ (n = 464) | 68 (14.3) |
| Arab American/Middle Eastern (n = 467) | 35 (7.4) |
| Native American (n = 468) | 33 (7.0) |
Hispanic/Latino category was inadvertently left off scale.
The total “n” responding to the life experience question varied by category. All respondents answered the work exposure categories.
Instruments
A booklet containing five questionnaires with 182 items included the following instruments: (a) Schim–Doorenbos Cultural Competence Assessment (S-D, CCA), (b) Rationing Health Care Resources Scale-Revised (RHCR-R), (c) Demographics/Diversity Training questions, (d) Life Experience Scale (LES), and (e) Marlowe-Crowne Social Desirability Scale-Form C (MCSDS-Form C). The set of instruments was pilot tested by 10 NPs, who found the entire set took 20–30 minutes to complete.
Schim–Doorenbos cultural competence assessment
The S-D, CCA instrument is designed to measure cultural awareness and sensitivity and CCBs. The Cultural Awareness and Sensitivity Subscale (CASS) measures cultural awareness (knowledge) and sensitivity with 12 items on a 7-point Likert-type scale (7 = strongly agree; 1 = strongly disagree). Two examples from the CASS include an awareness question and a sensitivity question: “I seek information on cultural needs when I identify new people in my work or school” and “I ask people to tell me about their own explanations of health & illness.” The CCB subscale of the S-D, CCA measures CCBs with 13 items on a 7-point Likert-type scale (7 = always; 1 = never). An example item from the CCB scale is: “I find ways to adapt my services to individual and group cultural preferences.” S-D, CCA internal consistency reliability has been reported at over .89, and αs for the CASS and CCB subscales have been reported from .72–.76 and .88–.93, respectively (Schim et al., 2005, 2006). Construct and content validity and test-retest reliability for the full S-D, CCA have been established (Doorenbos et al., 2005; Schim, Doorenbos, Miller, & Benkert, 2003). For the current sample, the Cronbach’s αs for the S-D, CCA; CASS; and CCB were .88, .64, and .92, respectively.
Rationing health care resources scale
Although several instruments have been developed to measure ethical constructs both within and outside the discipline of nursing, no measure of social justice could be found. Foster and McLellan (1997) developed the RHCR to measure health care equity (i.e., fair distribution of the benefits, risks, and costs of health care resources) on a social justice continuum from libertarian (individual centric approach) to communitarian (population equality approach). The RHCR is theoretically based on the work of Leonard Fleck, professor of philosophy and ethics at Michigan State University, who is known for his work on distributive justice issues in health care. Respondents indicate the strength of their convictions regarding 18 items on a 4-point Likert-type scale (1 = strongly disagree; 4 = strongly agree). Permission was gained to use the questions on the RHCR as the basis for an instrument to measure health care equity, one aspect of social justice orientation in nurses. An example item from the scale states: “No one has a moral claim to preventive health care benefits, especially when there are more urgent unmet health needs in the society.” Due to a lack of psychometric testing for the RHCR, the authors conducted exploratory factor analyses and reliability testing on 551 participants from this study in a separate analysis (Bell & Benkert, n.d.). The results indicated a three-factor solution for the RHCR-R: Factor I: social justice and rights to care based on age, quality of life, and potential benefit of the care; Factor II: social justice and the nurse’s duty to the individual patient versus duty to the population; and Factor III: social justice and individual right to unlimited or futile care. After the exploratory factor analysis, the scale was statistically pared down to 9 items. (Deleted items did not load at .35 or greater; two examples were: “All rationing policy decisions ought to be a product of a public, visible decision-making process”, and “A reasonable moral criterion for assessing the relative priority of competing health needs would be the degree to which a specific intervention protects or restores equality of access to care.”) The 9 items remaining were both statistically and theoretically congruent. Retained items (one example from each of the three factors) included: “Nurses are morally obligated to do everything possible for their patients even if their patients have no just claim on the resources or other patients have a stronger claim to the same resources,” “It is morally reasonable to give greater priority to health interventions that delay death or restore health/functioning for the younger members of society,” and “No one has an unlimited right to health care.” Cronbach’s α for the shortened RHCR-R (9 items) in this study was an acceptable .73. Cronbach’s α was .68 for Factor I, .72 for Factor II, and .55 for Factor III. The shortened RHCR-R with all 9 items was used in this study.
Life experiences scale
The LES is measured with 13 items on a 4-point Likert-type scale (4 = a lot; 1 = none) and is an expanded version of the diversity exposure item used by Schim et al. (2005, 2006). The current study added categories of life exposure beyond the traditional racial and ethnic groups (e.g., Asian American). The questionnaire, for example, asks about life exposure to homeless individuals and mentally impaired individuals. The LES stem is the following question: “How much life experience have you had socializing with the following cultural groups?” The LES measures the respondents’ personal life experiences with diverse cultural groups (e.g., Native American, gay/transgender, mentally impaired). Summing items from the LES yields the overall score. Higher scores indicate higher levels of life experiences. Internal consistency reliability for the LES was .84 in this study. The total score mean for the LES was 36 (SD = 6.4, range 19–51).
Demographics/diversity training
Demographic questions included self-identified age, gender, education, income, faith tradition, sexual orientation (straight/heterosexual; gay/lesbian/homosexual; transgendered; other) and ethnicity/race. Two questions about employment were asked: the number of hours per week worked as an NP and the setting in which they practiced. Prior diversity training was assessed using a dichotomous yes/no item and a set of questions asking for a description of the type of training.
Marlowe–Crowne social desirability scale—Form C
The MCSDS-Form C (Reynolds, 1982) is a 13-item self-report instrument that assesses a type of social desirability (i.e., need for approval) using dichotomous (true/false) forced choice responses. Scores range from 0 to 13; higher scores represent greater need for approval. Evidence of construct validity for the MCSDS-Form C has been reported (Fischer & Fick, 1993; Loo & Thorpe, 2000), and internal consistency coefficients have ranged from .62 to .89. For the current sample, Cronbach’s α was .74.
Data Analysis
Frequencies and correlation matrices were calculated as preliminary analyses to determine whether there might be hypothesized interdependencies in the data. A median substitution process was used for missing education data (n = 2, .4%). We used multigroup structural equation modeling (MG-SEM) to test the hypothesized model (Fig. 1) and determine the consistency of paths across the three NP groups: African American/Black men and women, Asian American men and women and non-Hispanic White men (Jöreskog, 1971; Kline, 1998; Sörbom, 1974). Each latent construct shown in the figure was specified with a single indicator and with the variance of the error term fixed as suggested by Hayduk (1987, p. 118–122). The error term was determined by multiplying the variance in the indicator by 1 minus the reliability (see Table 2 for indicator reliability). All exogenous variables were allowed to freely correlate. The model was recursive, containing no reciprocal causation or feedback loops (Arbuckle & Wothke, 1999).
Table 2.
Correlations and Statistics for Variables Used in Three-Group Structural Equation Model of Cultural Competence Behaviors
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | — | |||||||||
| 2. Income | .02 | — | ||||||||
| 3. Education | .02 | .13** | — | |||||||
| 4. Sexual orientation | .02 | .01 | .19** | — | ||||||
| 5. LES-Life experiences | −.02 | .05 | .07 | .11** | — | |||||
| 6. Social justice beliefs (RHCR-R) | .05 | .08 | −.01 | .08 | −.08 | — | ||||
| 7. Diversity training | −.05 | .15** | .08 | .08 | .18*** | .02 | — | |||
| 8. CASS—Awareness/Sensitivity | −.004 | .01 | .11** | .12** | .16*** | −.05 | .05 | — | ||
| 9. Social desirability (MCSDS) | .05 | −.004 | .03 | −.14** | .03 | −.20*** | −.01 | .01 | — | |
| 10. CCB—Behaviors | .14** | .06 | .09* | .02 | .32*** | −.08 | .22*** | .25*** | .22*** | — |
| Statistic: | ||||||||||
| M or % where indicated | 46.52 | 4.41b | 2.04c | 9.18%d | 2.21 | 2.54 | —e | 5.52 | 7.31 | 4.68 |
| SD | 8.81 | .71 | .30 | .296 | .49 | .27 | —e | .41 | 3.02 | 1.02 |
| IC reliabilitya | — | — | — | — | .85 | .73 | — | .64 | .74 | .92 |
LES, Life Experiences Scale; CASS, Cultural Awareness and Sensitivity Scale; CCB, Cultural Competence Behavior Scale.
p ≤ .05;
p ≤ .01;
p ≤ .001.
IC reliability, internal consistency reliability, alpha, was determined for multi-item scales. Other variables were assumed to be measured without error.
Income was coded in 5 categories: 1 = <19,000; 2 = 20,000–34,999; 3 = 35,000–59,999; 4 = 60,000–79,999; 5 = 80,000, and up. The modal response category was 5 with 51.9% responses.
Education was coded 1 = Bachelors, 2 = Masters, 3 = PhD; The modal response category was Masters with 90.3% responses.
Sexual orientation was coded 1 for non-heterosexual orientation and zero otherwise.
Diversity training is a dichotomous variable.
The initial model included each of the potential covariates (sexual orientation, income, and age) in addition to the pathways shown. Education, although often considered a covariate, was treated as a latent construct as opposed to a covariate because most studies of cultural competence and education have found them to be correlated, whereas the relationships of other covariates (e.g., age) to dependent variables are less clear. The structure paths were unconstrained so different path coefficients could be estimated in each of the groups simultaneously. The covariate pathways (sexual orientation, income, and age) were initially constrained to 0 in each group. This allowed for the possibility of a different structural model in each group and for potential covariates to contribute to model misfit.
The primary analysis was carried out on the variance covariance matrix and using maximum likelihood (ML) estimation (AMOS 18). Modification indices (Lagrange multipliers) were used to empirically identify potentially important paths not specified in the a priori model. Because ML assumes multivariate normality among endogenous variables, bootstrapping was used to estimate statistical significance of path coefficients in addition to the standard ML asymptotic statistics. The bootstrap procedure estimates variability in parameter estimates from the data itself by resampling with replacement (Bollen & Stine, 1990; Efron & Tibshirani, 1993). Standard errors thus derived do not depend on multivariate normality as ML estimates do. Overall model fit was evaluated using the comparative fit index (CFI), root mean square error of approximation (RMSEA), and analysis of standardized residuals. The CFI is a measure of relative fit ranging from 0 for the worst fitting model possible to 1 for a model with perfect fit. Models with CFI of .90 or larger are considered to have a good fit to the data; however, recently simulation researchers recommended a higher value of .95 (Hu & Bentler, 1999), as used in the current study. The RMSEA fit statistic ranges from 0 to infinity with a value of 0 indicating exact fit. Small values of .08 or less indicate acceptable fit and values of .05 or less indicate good fit. The chi-square statistic for the model and other details of the analysis strategy are reported with the results, including degrees and freedom and probability value.
RESULTS
The three groups of underrepresented NPs had had a variety of diversity experiences in both their work and personal lives (see Table 1). The majority of NPs had work experiences with every major racial and ethnic group in the U.S. with over 90% reporting exposure to the top four racial/ethnic groups (non-Hispanic White, African American/Black, Hispanic/Latino, and Asian American). The majority also reported significant work exposure to socially and economically diverse groups. The majority of NPs reported that they had completed some form of cultural diversity training (n = 411, 86.7%). The most frequent sources of training were their nursing education (n = 162, 29%) and employer sponsored offerings (n = 113, 21%).
Personal life experiences with diversity were more limited. As expected, most respondents (93%) reported “a lot” of life experiences with the U.S. majority culture (non-Hispanic White). Significantly fewer had “a lot” of life experience with other racial/ethnic, social, or economically disadvantaged groups. The greatest amount of life experiences with diverse populations were with African American/Black racial groups (62.7%) and low income individuals (50.2%), followed by Asian American ethnic groups (30.4%).
Table 2 shows the correlation matrix for the variables used in the model testing and reports the means, standard deviations, and intra-class correlations for the primary variables. Education, sexual orientation (gay/lesbian; transgender; other), and life experiences with diversity were all significantly and positively correlated with cultural awareness/sensitivity. Age, education, life experiences with diversity, diversity training, and social desirability were all significantly and positively correlated with CCBs.
Since social justice beliefs were not correlated with the major outcome variable (CCBs), we conducted a bivariate analysis between each of the RHCR-R factors and the SD, CCA, CAS and CCB (data not in Table 2). Factor I scores were negatively correlated with the CAS and CCB scales (p < .01); however, Factor I scores were not significantly correlated with the total scale (S-D, CCA), although the direction was negative. Factor II and Factor III scores were negatively correlated with the CCB scale (p < .01); no other significant correlations were found.
Model Testing
A MG-SEM was specified to test the pathways shown in Figure 1 and determine their consistency across the three NP groups (African American/Black men and women, Asian American men and women, non-Hispanic White males). The model fit was good (χ2 = 26.33, df = 18, p = .09, CFI = .96, RMSEA = .03; Hu & Bentler, 1999), indicating that the general form was adequate. The hypothesis of identical path coefficients in all three groups of underrepresented NPs was tested by comparing the chi-square difference between a model with all structural paths freely estimated and a model in which all structural paths were fixed equal across groups. The model with freely estimated paths will always fit better because best fitting path coefficients are determined for each path in each group, but we wondered if an increase in misfit due to constraining the pathways would be larger than could be expected by chance alone. Constraining the pathways to be equal across groups did not result in a significant decrease in model fit (chi-square difference of 28.48, df = 22, was not significant, p > .05). Therefore the same model with the same path coefficients was accepted as adequate for all three groups.
Model reduction was accomplished by assessing the path coefficients and systematically deleting paths with the smallest critical ratio (indicating non-significance) that could justifiably be removed (based on theory). Additionally, modification indices were examined to see if paths not originally in the model would improve the model fit (Arbuckle & Wothke, 1999; Kline, 1998). Five variables and two regression paths were withdrawn from the model. Sexual orientation, income, and age were omitted because modification indices did not justify removing the zero restriction; education and social justice were omitted because the paths associated with these variables did not meet the critical ratios. The relationships between social desirability and cultural awareness/sensitivity and between diversity training and cultural awareness/sensitivity did not reach the significance level; both paths were dropped from the model. The fit of this model was excellent (χ2 = 12.07, df = 19, p = .64, CFI = 1.0, RMSEA < .01). The standardized path coefficients differed slightly across the groups. To obtain the final model statistics, a single group model was estimated. This model also fit the data well (χ2 = .263, df = 3, p = .97, CFI = 1.0, RMSEA < .01). Figure 3 shows the path structure of the final model and the standardized path coefficients; all coefficients in the model are significant (p < .05). The model accounted for 29% of the variance in CCBs but only 4% of the variance in cultural awareness/sensitivity. As expected, cultural awareness/sensitivity partially mediated the effect of life experiences with diversity on CCBs (indirect path = .19 * .23, p < .01). After controlling for social desirability, each of the other structural variables was significantly related to CCBs. The only predictor of cultural awareness was life experience with diversity.
FIGURE 3.
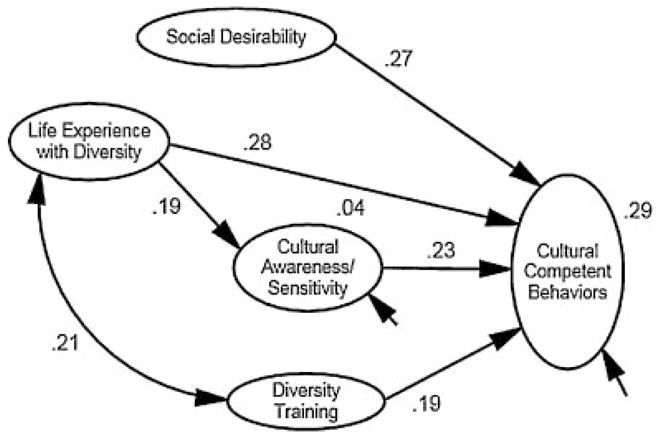
Final structural equation model of cultural competent behavior among traditionally underrepresented NPs (n = 474). All coefficients are significant (p < .05).
As a final step in assessment of model fit, we examined standardized residuals and computed bootstrapped estimates of path coefficients. Standardized residuals were all less than .5 in absolute value. Bootstrapped estimates of bias in path estimates were also very small (p < .005).
The study examined whether life experiences with diversity, diversity training, cultural awareness/sensitivity, social justice beliefs, social desirability, and selected demographic variables predicted CCBs among three groups of NPs typically underrepresented in the United States. Age, education, life experiences with diversity, diversity training, social desirability, and cultural awareness/sensitivity were positively correlated with CCBs in bivariate analyses. In addition, education, non-heterosexual orientation, and life experiences with diversity were all significantly correlated with cultural awareness/sensitivity. Our three hypotheses were partially supported, and the final model had good fit for all three underrepresented groups of NPs.
Our first hypothesis that diversity training, social justice beliefs, and life experiences with diversity would have positive effects on cultural awareness/sensitivity and CCBs was partially supported. Life experiences with diversity had direct effects on cultural awareness/sensitivity and CCBs, and diversity training had a direct effect on CCBs but did not directly affect cultural awareness/sensitivity. Diversity training was related to life experiences with diversity, which was then associated with cultural awareness/sensitivity. Social justice beliefs did not remain in the final model for either a direct or indirect path. The second hypothesis was partially supported. Cultural awareness/sensitivity only mediated the relationship between life experiences with diversity and CCBs. The final hypothesis, that these effects would hold up when controlling for social desirability, education, and other covariates, was supported.
DISCUSSION
Similar to findings with mostly homogenous (non-Hispanic White) samples, diversity training was an important predictor of CCBs in this unique group of NPs. Prior cultural competence (diversity) training has a significant impact on CCBs (Schim et al., 2005, 2006). Although diversity training could use further evaluation (Beach et al., 2005; Price et al., 2005), the results of our study suggest that diversity training is an important predictor of CCBs even among culturally diverse and underrepresented health care providers. The indirect path to CCBs from diversity training through life experiences with diversity needs further exploration in both a traditional (non-Hispanic White) and unique sample of NPs. The relationship between training and life experiences may be via a non-recursive path in which training affected life experiences and vice versa.
The impact of experiences with diversity on cultural competence awareness/sensitivity and CCBs is a new contribution to the state of the science. Previous research linking life experience to cultural competence has been qualitative and limited to the influence on personal attitudes (Ekblad, Martilla, & Emilsson, 2000; Reeves & Fogg, 2006). We could find no study linking life experiences to CCBs. Our findings may indicate that life experiences may influence comfort with diversity, which can translate into comfort with behaviors. These findings are important because life experiences have been associated with willingness to serve underserved populations (Krouse & Nauta, 2005). With growing primary care shortages (Bodenheimer & Pham, 2010), the findings could reinforce educational program policies that require clinical experiences with a residency component in underserved and diverse communities to enhance life experiences with diversity and CCBs. A cost effective educational and federal policy could target graduate nursing students who have the requisite life experiences and are comfortable with diversity toward National Health Service Corps Scholarship and Loan Repayment funding. These policies have the potential to improve recruitment and retention in underserved areas and provide local communities with a more culturally competent and effective workforce.
The lack of a path between distributive justice beliefs and cultural competence awareness/sensitivity or CCBs was unexpected. Although theoretically plausible, higher social justice beliefs were not associated with higher cultural competence levels (Miller et al., 2009). One explanation is related to a measurement issue. As a new instrument, the RHCR-R may not be measuring the concept as we envisioned (Foster & McClellan, 1997). Further construct validity testing is warranted. Another potential explanation was that this unique group of NPs held conflicting views on factors within the instrument (Factor I: right to care based on age, quality of life, and potential benefit of the care; Factor II: the nurses’ duty to the individual patient versus duty to unknown others (the population); and Factor III: individual right to unlimited or futile care). A correlation matrix supported the latter explanation. The psychometric data also resulted in theoretically contrary findings (e.g., persons of color and those working in public health had lower distributive justice scores; Bell & Benkert, n.d.).
The positive correlation between gay/lesbian and transgender sexual orientation and two predictors (life experiences with diversity and cultural awareness/sensitivity) of CCBs is a new finding. No other studies were found linking this important personal identity concept to cultural competence. The finding expands the literature related to cultural competence by confirming that health professional diversity (and the associated life experiences) may be an important precursor to cultural competence awareness/sensitivity and behaviors (Ekblad et al., 2000). Similar to other underrepresented health professional groups, the primarily gay (self-identified) male NPs may advance to increased CCBs through a different “life experiences” pathway.
This is the first documented report of an association between cultural competence and social desirability in NPs, and more specifically a unique sample of NPs. The results are similar to studies of multicultural counseling professionals, most of whom were non-Hispanic White females. Similarly, social desirability was positively correlated with CCBs but not with cultural competence awareness/sensitivity (Constantine & Ladany, 2000; Worthington et al., 2000). It may be that those employed in the helping professions have more “need for approval” when being asked about behaviors on culturally sensitive topics (Burkard and Knox, 2004) than when asked about attitudes. Attitudes are more implicit, and therefore hidden, and may be less influenced by measures of social desirability. Female gender was likewise correlated with social desirability (Worthington et al., 2000).
These new findings can provide guidance for cultural competence training, particularly with underrepresented health professionals. The model provided good fit for all groups, suggesting that the model is applicable across these three groups of NPs. The training, however, may need to be tailored to an individual’s personal life experiences (Ekblad et al., 2000; Schim et al., 2006). The subtle yet important differences in self-identification and life experience obviate a “cookie cutter” cultural categorizations approach. The findings argue that the recent training programs that advocate a self-assessment followed by a curriculum tailored to the participant (Ekblad et al., 2000; National Center for Cultural Competence, 2009) might be the most beneficial (and cost effective) avenue for delivering this information.
Limitations
Two limitations are issues of generalizability and measurement of a key predictor. The study was purposefully sampled to enhance inclusion of NPs of color and male NPs, which limits generalizability to a select group of practicing NPs. Generalizability may also be affected by the response rate; although adequate for national sampling surveys, the length of the survey booklet (182 items) may have limited the responses to those interested in the topic or motivated by the incentives. Finally, the cultural awareness/sensitivity scale and the social justice scale (i.e., the RCHR-R) had a few limitations. The coefficient alpha for the CASS (.64; Doorenbos et al., 2005) was in the low to moderate range in this study, thus restricting the available variance, and the effects of social justice scale (RHCR-R) on cultural competence will require further study.
Directions for Future Research
The conceptual model provides compelling evidence that diversity training in underrepresented NPs, similar to majority NPs, is an important antecedent to CCBs. The impact of life experiences with diversity warrants further study to determine which experiences make the most difference in CCBs so that training can target the most effective (and cost effective) experiences. The existing training rarely goes beyond attitudinal and knowledge components of cultural competence (Beach et al., 2005), thus more research is needed that follows participants over time to monitor changes in actual behaviors. Consistent with the perspectives of Musolino et al. (2010), understanding and eliminating the disparities in health care will require researchers and educators to enhance interest in diversity and face to face encounter experiences in curricula. Research is needed to understand how curricula can be tailored to the needs of the participant, and researchers should go beyond surveys of professionals to field investigations of patients’ perceptions following providers’ cultural competence training. Increasing workplace diversity is a critical solution for diminishing health disparities. Our results also suggest that among underrepresented health care providers, training will require attention to a similar yet expanded set of predictors in order to achieve a culturally competent workforce.
Acknowledgments
This Research was partially supported by a Faculty Research Incentive Award from Wayne State University College of Nursing and National Institute for Nursing Research funding (NINR R21NR010896-01A1). The authors thank the research assistants who helped with survey mailing, data collection, and data input: Wilfred Allen, Anita Manns, Sheila Morrisette, E. Frank Thompson, and Sarah Witkopf. The authors also thank the manuscript reviewers for their careful and thoughtful review.
References
- Ahmann E. Developing cultural competence in health care settings: National Center for Cultural Competence. Pediatric Nursing. 2002;28:133–137. [PubMed] [Google Scholar]
- Arbuckle JL, Wothke W. Amos 4.0: User’s guide. Chicago, IL: Smallwaters Corporation; 1999. [Google Scholar]
- Beach MC, Price EG, Gary TL, Robinson KA, Gozu A, Palacio A, et al. Cultural competence: A systematic review of health care provider educational interventions. Medical Care. 2005;43(4):356–373. doi: 10.1097/01.mlr.0000156861.58905.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell SE, Benkert R. Development of an instrument to measure distributive justice: One element of social justice orientation. Manuscript in preparation 2011 [Google Scholar]
- Benkert R, Pohl JM, Coleman-Burns P. Creating cross-racial primary care relationships in a nurse-managed center. Journal of Cultural Diversity. 2004;11:88–99. [PubMed] [Google Scholar]
- Benkert R, Tanner C, Guthrie B, Oakley D, Pohl JM. Cultural competence of nurse practitioner students: A consortium’s experience. Journal of Nursing Education. 2005;44:225–233. doi: 10.3928/01484834-20050501-05. [DOI] [PubMed] [Google Scholar]
- Black RM. Intersections of care: An analysis of culturally competent care, client centered care, and the feminist ethic of care. Work. 2005;24:409–422. [PubMed] [Google Scholar]
- Bodenheimer T, Pham HH. Primary care: Current problems and proposed solutions. Health Affairs. 2010;29:799–805. doi: 10.1377/hlthaff.2010.0026. [DOI] [PubMed] [Google Scholar]
- Bollen KA, Stine R. Direct and indirect effects: Classical and bootstrap estimates of variability. Sociological Methodology. 1990;20:115–140. [Google Scholar]
- Braye S, Preston-Shoot M, Thorpe A. Beyond the classroom: Learning social work law in practice. Journal of Social Work. 2007;7(3):322–340. [Google Scholar]
- Burkard AW, Knox S. Effect of therapist color-blindness on empathy and attributions in cross-cultural counseling. Journal of Counseling Psychology. 2004;51:387–397. [Google Scholar]
- Byrne BM. Structural equation modeling with AMOS. Mahwah, NJ: Erlbaum; 2001. [Google Scholar]
- Ciesielka DJ, Schumacher G, Conway A, Penrose J. Implementing and evaluating a culturally-focused curriculum in a collaborative graduate nursing program. International Journal of Nursing Education Scholarship. 2005;2:6. doi: 10.2202/1548-923x.1124. Available at: http://www.bepress.com/ijnes/vol2/iss1/art6/ [DOI] [PubMed] [Google Scholar]
- Constantine MG, Ladany N. Self-report multicultural counseling competence scales: Their relation to social desirability attitudes and multi-cultural case conceptualization ability. Journal of Counseling Psychology. 2000;47:155–164. [Google Scholar]
- Cooper Brathwaite A. Influence of nurse characteristics on the acquisition of cultural competence. International Journal of Nursing Education Scholarship. 2006;3(1):Article 3. doi: 10.2202/1548-923X.1173. Available at: http://www.bepress.com/ijnes/vol3/iss1/art3/ [DOI] [PubMed] [Google Scholar]
- Doorenbos AZ, Schim SM. Cultural competence in hospice. American Journal of Hospice and Palliative Medicine. 2004;21:28–32. doi: 10.1177/104990910402100108. [DOI] [PubMed] [Google Scholar]
- Doorenbos AZ, Schim SM, Benkert R, Borse NN. Psychometric evaluation of the Cultural Competence Assessment Instrument among health care providers. Nursing Research. 2005;54:324–331. doi: 10.1097/00006199-200509000-00006. [DOI] [PubMed] [Google Scholar]
- Drevdahl D, Kneipp SM, Canales MK, Dorcy KS. Reinvesting in social justice: A capital idea for public health nursing? Advances in Nursing Science. 2001;24(2):19–31. doi: 10.1097/00012272-200112000-00004. [DOI] [PubMed] [Google Scholar]
- Efron B, Tibshirani R. An introduction to the bootstrap. New York, NY: Chapman & Hall/CRC; 1993. [Google Scholar]
- Ekblad S, Marttila A, Emilsson M. Cultural challenges in end-of-life care: Reflections from focus groups’ interviews with hospice staff in Stockholm. Journal of Advanced Nursing. 2000;31:623–630. doi: 10.1046/j.1365-2648.2000.01318.x. [DOI] [PubMed] [Google Scholar]
- Fischer DG, Fick C. Measuring social desirability: Short forms of the Marlowe-Crowne Social Desirability Scale. Educational and Psychological Measurement. 1993;53:417–424. [Google Scholar]
- Fortier JP, Bishop D. Setting the agenda for research on cultural competence in health care: Final report (Contract No.: 00T061242) Rockville, MD: U.S. Department of Health and Human Services Office of Minority Health and Agency for Healthcare Research and Quality; 2004. Retrieved from Agency for Healthcare Research and Quality. Available at: http://www.ahrq.gov/research/cultural.htm. [Google Scholar]
- Foster LW, McLellan LJ. Moral judgments in the rationing of health care resources: A comparative study of clinical health professionals. Social Work in Health Care. 1997;25(4):13–36. doi: 10.1300/J010v25n04_02. [DOI] [PubMed] [Google Scholar]
- Giddings LS. Health disparities, social injustice, and the culture of nursing. Nursing Research. 2005;54:304–312. doi: 10.1097/00006199-200509000-00004. [DOI] [PubMed] [Google Scholar]
- Godkin MA, Savageau JA. The effect of a global multiculturalism track on cultural competence of preclinical medical students. Family Medicine. 2001;33:178–186. [PubMed] [Google Scholar]
- Goolsby MJ. 2004 AANP National Nurse Practitioner Sample Survey, Part I: An overview. Journal of the American Academy of Nurse Practitioners. 2005;17:337–3341. doi: 10.1111/j.1745-7599.2005.00060.x. [DOI] [PubMed] [Google Scholar]
- Hagman LW. Cultural self-efficacy of licensed registered nurses in New Mexico. Journal of Cultural Diversity. 2006;13:105–112. [PubMed] [Google Scholar]
- Hayduk LA. Structural equation modeling with LISREL: Essentials and advances. Baltimore, MD: John Hopkins University Press; 1987. [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Jöreskog KG. Simultaneous factor analysis in several populations. Psychometrika. 1971;36:409–426. [Google Scholar]
- Joseph HJ. Attitudes and cultural self-efficacy levels of nurses caring for patients in army hospitals. Journal of National Black Nurses Association. 2004;15(1):5–16. [PubMed] [Google Scholar]
- Kardong-Edgren S, Bond ML, Schlosser S, Cason C, Jones ME, Warr R, et al. Cultural attitudes, knowledge, and skills of nursing faculty toward patients from four diverse cultures. Journal of Professional Nursing. 2005;21:175–182. doi: 10.1016/j.profnurs.2005.04.001. [DOI] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. New York, NY: Guilford Press; 1998. [Google Scholar]
- Krouse TMD, Nauta MM. Values, motivations, and learning experiences of future professionals: Who wants to serve underserved populations? Professional Psychology, Research and Practice. 2005;36:688–694. [Google Scholar]
- Loo R, Thorpe K. Confirmatory factor analyses of the full and short versions of the Marlowe-Crowne Social Desirability Scale. The Journal of Social Psychology. 2000;140:628–635. doi: 10.1080/00224540009600503. [DOI] [PubMed] [Google Scholar]
- Miller MJ, Sendrowitz K, Connacher C, Blanco S, de la Pena CM, Bernardi S, Morere L. College students’ social justice interest and commitment: A social-cognitive perspective. Journal of Counseling Psychology. 2009;56:495–507. [Google Scholar]
- Musolino GM, Burkhalter ST, Crookston B, Ward RS, Harris RM, Chase-Cantarini S, et al. Understanding and eliminating disparities in health care: Development and assessment of cultural competence for interdisciplinary health professionals at the University of Utah—A 3-year investigation. Journal of Physical Therapy Education. 2010;24(1):25–36. [Google Scholar]
- National Center for Cultural Competence. The compelling need for cultural and linguistic competence. Georgetown University Center for Child and Human Development; 2009. Available at: http://nccc.georgetown.edu/foundations/need.html. [Google Scholar]
- Price EG, Beach MC, Gary TL, Robinson KA, Gozu A, Palacio A, et al. A systematic review of the methodological rigor of studies evaluating cultural competence training of health professionals. Academic Medicine. 2005;80:578–586. doi: 10.1097/00001888-200506000-00013. [DOI] [PubMed] [Google Scholar]
- Reeves JS, Fogg C. Perceptions of graduating nursing students regarding life experiences that promote culturally competent care. Journal of Transcultural Nursing. 2006;17:171–178. doi: 10.1177/1043659605285410. [DOI] [PubMed] [Google Scholar]
- Reimer Kirkham S, Van Hofwegen L, Hoe Harwood C. Narratives of social justice: Learning in innovative clinical settings. International Journal of Nursing Education Scholarship. 2005;2(1):28. doi: 10.2202/1548-923x.1166. Available at: http://www.bepress.com/ijnes/vol2/iss1/art28/ [DOI] [PubMed] [Google Scholar]
- Reynolds WM. Development of reliable and valid short forms of the Marlowe-Crowne social desirability scale. Journal of Clinical Psychology. 1982;38:119–125. [Google Scholar]
- Sargent SE, Sedlak CA, Martsolf DS. Cultural competence among nursing students and faculty. Nurse Education Today. 2005;25:214–221. doi: 10.1016/j.nedt.2004.12.005. [DOI] [PubMed] [Google Scholar]
- Schim SM, Benkert R, Bell SE, Walker DS, Danford CA. Social justice: Added metaparadigm concept for urban health nursing. Public Health Nursing. 2007;24:73–80. doi: 10.1111/j.1525-1446.2006.00610.x. [DOI] [PubMed] [Google Scholar]
- Schim SM, Doorenbos AZ, Benkert R, Miller J. Culturally congruent care: Putting the puzzle together. Journal of Transcultural Nursing. 2007;18:103–110. doi: 10.1177/1043659606298613. [DOI] [PubMed] [Google Scholar]
- Schim SM, Doorenbos AZ, Borse NN. Cultural competence among Ontario and Michigan healthcare providers. Journal of Nursing Scholarship. 2005;37:354–360. doi: 10.1111/j.1547-5069.2005.00061.x. [DOI] [PubMed] [Google Scholar]
- Schim SM, Doorenbos AZ, Borse NN. Cultural competence among hospice nurses. Journal of Hospice & Palliative Nursing. 2006;8:302–307. doi: 10.1177/1049909106292246. [DOI] [PubMed] [Google Scholar]
- Schim SM, Doorenbos AZ, Miller JE, Benkert R. Development of a cultural competence assessment instrument. Journal of Nursing Measurement. 2003;11:29–40. doi: 10.1891/jnum.11.1.29.52062. [DOI] [PubMed] [Google Scholar]
- Smedley BD, Stith Butler A, Bristow LR, editors. In the nation’s compelling interest: Ensuring diversity in the health care workforce. Washington, DC: National Academies Press; 2004. [PubMed] [Google Scholar]
- Smith-Campbell B. Health professional students’ cultural competence and attitudes toward the poor: The influence of a clinical practicum supported by the National Health Service Corps. Journal of Allied Health. 2005;34:56–62. [PubMed] [Google Scholar]
- Sörbom D. A general method for studying differences in factor means and factor structure between groups. British Journal of Mathematical and Statistical Psychology. 1974;27:229–239. [Google Scholar]
- Spanierman LB, Poteat VP, Wang Y, Oh E. Psychosocial costs of racism to White counselors: Predicting various dimensions of multicultural counseling competence. Journal of Counseling Psychology. 2008;55:75–88. [Google Scholar]
- Worthington RL, Mobley M, Franks RP, Tan JA. Multicultural counseling competencies: Verbal content, counselor attributions, and social desirability. Journal of Counseling Psychology. 2000;47:460–468. [Google Scholar]