Abstract
Introduction
Klebsiella pneumoniae is in most cases a hospital-acquired infection and presents as pneumonia, septicemia and meningitis in patients with some predisposing factors, including prematurity, intravenous catheter, history of antibiotic therapy and intravenous nutrients.
Case presentation
A low-birth-weight, 33-day-old Caucasian girl with respiratory distress syndrome was admitted to our hospital. She developed septicemia, meningitis, polyarticular arthritis and osteomyelitis by nosocomial K. pneumoniae which was resistant to most antibiotics except ciprofloxacin. She was therefore treated with ciprofloxacin and co-trimoxazole for eight weeks. After completion of the treatment course, she completely improved with excellent weight gain and without any adverse effects during three years of follow-up.
Conclusion
In the resistant strain of K. pneumoniae, ciprofloxacin could be considered as a therapeutic option with the prospect of a good outcome, even in neonates and infants.
Introduction
Pneumonia is a type of infection that is most commonly caused outside the hospital by Klebsiella pneumoniae [1]. Mostly, K. pneumoniae is recognized as a hospital-acquired infection presenting as pneumonia, septicemia and meningitis in patients with some predisposing factors (including prematurity, intravenous catheter, history of antibiotic therapy and intravenous nutrients) [2,3]. In the rare patients with underlying conditions among newborns and older adults, K. pneumoniae may result in arthritis and osteomyelitis. All Klebsiella subtypes are resistant to ampicillin, especially multi-drug-resistant (MDR) subtypes which are resistant to the majority of antibiotics, except fourth-generation cephalosporins and carbapenems. Previously, patients with MDR subtype infections usually received first-generation cephalsporins and aminoglycosides.
Case presentation
A 33-day-old Caucasian girl was brought to the Tabriz Children's Hospital with poor breastfeeding, recurrent vomiting and anorexia. She was admitted with a primary diagnosis of septicemia.
She was born from a mother with pre-eclampsia through normal vaginal delivery at the 34th week of gestation, with a birth weight of 1670 g. Her Apgar scores at one and five minutes were five and six, respectively. During delivery and before admission to the Tabriz Children's Hospital, she had been hospitalized in the Talegani neonatal intensive care unit for prematurity, septicemia, respiratory distress syndrome and gastrointestinal bleeding. In Talegani Hospital, she had received antibiotic therapy, including ampicillin and gentamicin, then her medication was changed to cefotaxime and vancomycin, and finally her treatment continued with intravenous immunoglobulin, imipenem and ceftazidime.
Her physical examination revealed that she was pale, cachectic, anorexic and hypotonic, and her Moro and sucking reflexes were weak. She also exhibited grunting and had substernal and intercostal retraction. The patient's body weight, height and head circumference were 1700 g, 43 cm and 31 cm, respectively. Her vital signs, including pulse rate, respiratory rate, body temperature, O2 saturation under the oxygen hood and without using the oxygen hood were 158/min, 48/min, 38.6°C, 95% and 89%, respectively.
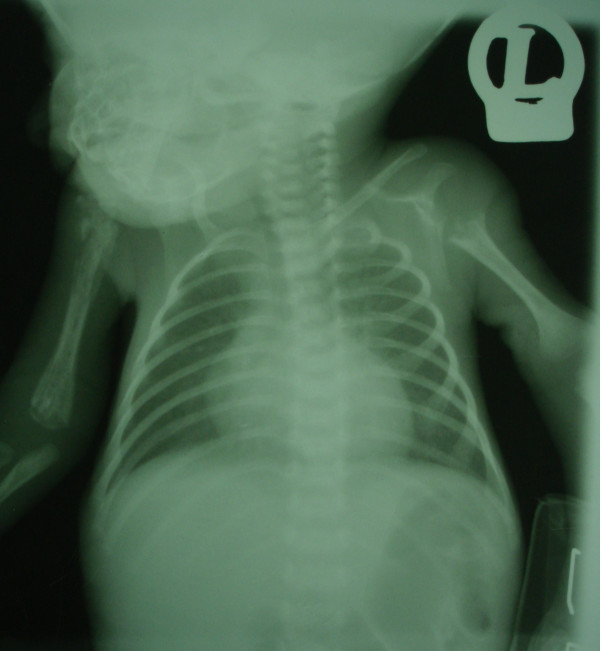
Her cerebrospinal fluid (CSF) was purulent, and CSF analysis showed 520 mg/dL protein; 16 mg/dL glucose; many white blood cells (WBCs), with 85% polymorphonuclear cells and 15% lymphocytes; and 25 red blood cells (RBCs)/mm3. The results of the other laboratory tests are shown in Table 1. In the CSF and blood culture, K. pneumonia was resistant to most of the antibiotics and sensitive only to ciprofloxacin and co-trimoxazole. Her chest X-ray showed bilateral humeral osteomyelitis and bilateral glenohumeral joint arthritis (Figure 1).
Table 1.
Laboratory tests and results on admissiona
| Complete blood cell count | Biochemical analysis | Arterial blood gas | |||
|---|---|---|---|---|---|
| WBC count (cells/μL) | 6500 | FBG (mg/dL) | 42 | pH | 7.29 |
| Hb, g/Dl | 7.8 | Cr (mg/dL) | 0.5 | HCO3- (mmol/L) | 20 |
| Platelets, n/μL | 773 × 103 | BUN (mg/dL) | 24 | PCO2 (mmHg) | 43 |
| PMN cells, % | 51 | ||||
| Eosinophils, % | 1% | Electrolytes | Other | ||
| Lymphocytes, % | 24% | Na (mEa/L) | 136 | CRP | 2+ |
| Monocytes, % | 2% | K (mEa/L) | 45 | Blood group | A+ |
| Band cells, % | 21% | Ca (mg/dL) | 10.8 | ||
aWBC, white blood cells; Hb, hemoglobin; PMN, polymorphonuclear cells; CRP, C-reactive protein; Na, sodium; K, potassium; BUN, blood urea nitrogen; FPG, fasting plasma glucose; Ca, calcium.
Figure 1.
Chest X-ray obtained at the time of admission. Bilateral osteomyelitis in the humerus presented as osteolysis and involucrum. Also, there is sequestration because of osteonecrosis and a pathologic fracture in the proximal part of the humerus. Dislocation of right glenohumeral joint brings up the arthritis diagnosis. There is complete osteolysis in proximal metaphysis in the left humerus and arthritis in the left glenohumeral joint. The heart, lung and pleural space have a normal appearance, while the thymus is atrophic.
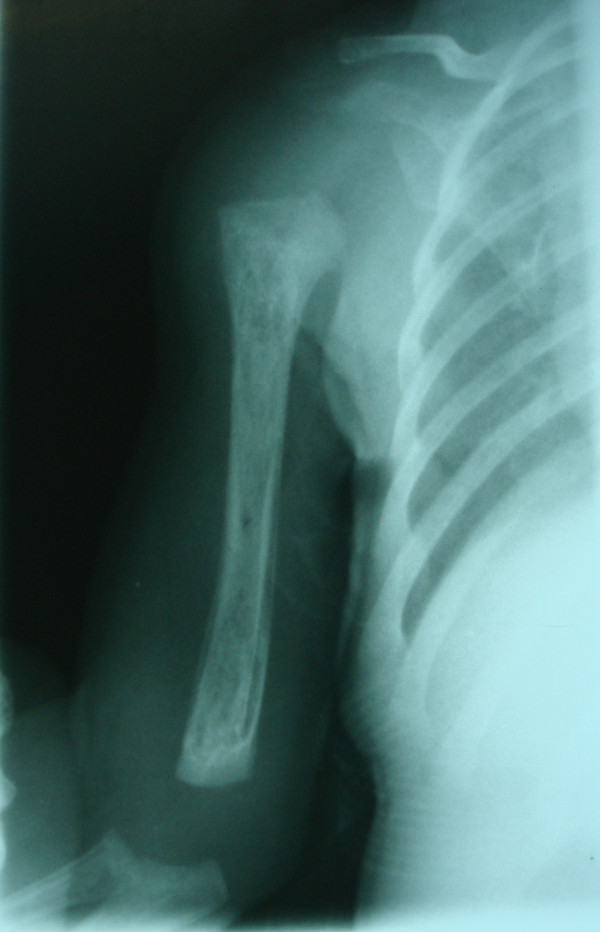
On the basis of the paraclinical evidence, diagnoses of K. pneumoniae septicemia, meningitis, arthritis and osteomyelitis were made, and a treatment protocol with a combination of intravenous ciprofloxacin and co-trimoxazole antibiotics was started (for 28 days). At the end of the intravenous treatment period, she weighed 2420 g, and her CSF analysis and culture were within normal range. Afterward, she was discharged with oral ciprofloxacin, co-trimoxazole and rifampicin for another 28-day period. Figures 2 and 3 show her chest X-rays obtained on the seventh and 28th days of oral antibiotic therapy, respectively. At the end of 28 days of oral antibiotic therapy (when the patient was 88 days old), her weight had reached 4250 g and normal glenohumeral joints and humerus bones were shown on her chest X-ray. During three years of follow-up, she had normal developmental milestones and was not readmitted to the hospital.
Figure 2.
Chest X-ray obtained on the seventh day of oral anti-biotic therapy. The lytic lesions in the proximal and distal metaphysis in the right humerus are shown.
Figure 3.
Chest X-ray showing complete resolution of symptoms at the end of anti-biotic therapy.
Discussion
Prolonged hospital stay, decreased gestational age, prolonged use of broad-spectrum antibiotics and inadequacy of some basic facilities and staffing carry the risk of introduction of resistant hospital pathogens [4-6]. In the present case, all of the above-mentioned factors, combined with prematurity, predisposed the neonate to a higher risk of contracting nosocomial K. pneumoniae arthritis, osteomyelitis, septicemia and meningitis, although the common cause of osteoarthritis is Gram-positive cocci [7].
Adeyemo et al. [8] reported an outbreak of bone infections associated with neonatal septicemia by K. pneumoniae in 12 neonates over a six month period at the Special Care Baby Unit, University College Hospital, Ibadan, Nigeria. All patients had septic arthritis, 10 of them had osteomyelitis and 50% had multiple-joint involvement.
Hospital-acquired K. pneumoniae has been reported to be resistant to multiple antibiotics [8,9]. In addition, Ghahramani and Nahaie [10] showed that K. pneumoniae is the most common cause of septicemia in the neonatal ward of the Tabriz Al-Zahra Gynecology and Obstetrics Referral Hospital in Tabriz, Iran.
The parenteral third-generation cephalosporins appear to be a major therapeutic advance in the treatment of K. pneumoniae [11], but reports of highly resistant strains that produce plasmid-mediated, extended-spectrum β-lactamases influenced therapeutic outcomes again [12]. Evidence revealed that K. pneumoniae infection, especially the nosocomial type, is resistant to the majority of antibiotics except for ciprofloxacin and ofloxacin [13]. In the present case report, the isolated K. pneumoniae was resistant to most of the antibiotics except ciprofloxacin and co-trimoxazole. Therefore, these two antibiotics were used in the treatment protocol. Because of the quinolone cartilage toxicity potential in experimental juvenile animal models, the use of ciprofloxacin among children has been restricted [13,14]. However, recent data from Bayer's ciprofloxacin clinical trials database indicate that the role of fluoroquinolones in the treatment of certain serious infections in children does not appear to be compromised by safety concerns when used appropriately [15]. In such cases, when a micro-organism is resistant to all antibiotics except ciprofloxacin, a dosage of 15 mg/kg/day to 30 mg/kg/day is advised in neonates [16].
After completion of the treatment course, our patient completely improved and achieved normal developmental milestones and weight gain, without adverse effects or hospital readmission during three years of follow-up.
Conclusion
In neonates with delivery problems, prematurity, low birth weight and prolonged hospital admission, nosocomial K. pneumoniae should be considered in the differential diagnosis of septicemia, arthritis, osteomyelitis and meningitis. Considering the multi-drug resistance of nosocomial K. pneumoniae and sensitivity to quinolones, ciprofloxacin, when used appropriately, should be considered a therapeutic option with good outcomes in patients with serious infections with resistant strains of K. pneumoniae, even in neonates and infants.
Abbreviations
CSF: cerebrospinal fluid; MDR: multi-drug-resistant.
Consent
Written informed consent was obtained from the patient's next-of-kin for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
ZG, HH and SG collected the patient data and participated in the patient's hospitalization and treatment process. NN was a major contributor in writing the manuscript. JST helped to revise and edit the manuscript. All authors read and approved the final manuscript.
Contributor Information
Ziaaedin Ghorashi, Email: Dr_ziaaden_ghorashi@yahoo.com.
Nariman Nezami, Email: Dr.nezami@gmail.com.
Hamideh Hoseinpour-feizi, Email: Hoseinpourh@tbzmed.ac.ir.
Sona Ghorashi, Email: Sona_ghoreishi@hotmail.com.
Jafar Sadegh Tabrizi, Email: tabrizijs@tbzmed.ac.ir.
Acknowledgements
The authors acknowledge the parents of the patient for their collaboration and consent.
References
- Donnenberg MS. In: Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 6. Mandell GL, Bennett JE, Dolin R, editor. II. New York: Elsevier/Churchill Livingstone; 2005. Enterobacteriaceae; pp. 2567–2586. [Google Scholar]
- Feigin RD Cherry J Demmler-Harrison GJ Kaplan SL Feigin and Cherry's Textbook of Pediatric Infectious Diseases 20045Philadelphia: Saunders; 4417819 [Google Scholar]
- Asensio A, Oliver A, González-Diego P, Baquero F, Pérez-Díaz JC, Ros P, Cobo J, Palacios M, Lasheras D, Cantón R. Outbreak of a multiresistant Klebsiella pneumoniae strain in an intensive care unit: antibiotic use as risk factor for colonization and infection. Clin Infect Dis. 2000;30:55–60. doi: 10.1086/313590. [DOI] [PubMed] [Google Scholar]
- Yalaz M Arslanoğlu S Çetin H Aydemir Ş Tünger A Akısü M Kültürsay N Evaluation of culture-proven sepsis in a level III NICU: a two year analysis Adnan Menderes Üniversitesi Tip Fakültesi Dergisi 200455–9.21119461 [Google Scholar]
- Turkish Neonatal Society; Nosocomial Infections Study Group. Nosocomial infections in neonatal units in Turkey: epidemiology, problems, unit policies and opinions of healthcare workers. Turk J Pediatr. 2010;52:50–57. [PubMed] [Google Scholar]
- Cordero L, Rau R, Taylor D, Ayers LW. Enteric gram-negative bacilli bloodstream infections: 17 years' experience in a neonatal intensive care unit. Am J Infect Control. 2004;32:189–195. doi: 10.1016/j.ajic.2003.07.004. [DOI] [PubMed] [Google Scholar]
- Nelson JD, Koontz WC. Septic arthritis in infants and children: a review of 117 cases. Pediatrics. 1966;38:966–971. [PubMed] [Google Scholar]
- Adeyemo AA, Akindele JA, Omokhodion SI. Klebsiella septicemia, osteomyelitis and septic arthritis in neonates in Ibadan, Nigeria. Ann Trop Pediatr. 1993;13:285–289. doi: 10.1080/02724936.1993.11747661. [DOI] [PubMed] [Google Scholar]
- Westbrook GL, O'Hara CM, Roman SB, Miller JM. Incidence and identification of Klebsiella planticola in clinical isolates with emphasis on newborns. J Clin Microbiol. 2000;38:1495–1497. doi: 10.1128/jcm.38.4.1495-1497.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghahramani P, Nahaie MR. Klebsiella sepsis in neonates admitted to Al-Zahra Hospital, Tabriz. Med J Tabriz Univ Med Sci. 2002;35:69–73. [Google Scholar]
- Tang LM, Chen ST, Hsu WC, Chen CM. Klebsiella meningitis in Taiwan: an overview. Epidemiol Infect. 1997;119:135–142. doi: 10.1017/S0950268897007930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith CE, Tillman BS, Howell AW, Longfield RD, Jorgensen JH. Failure of ceftazidime-amikacin therapy for bacteremia and meningitis due to Klebsiella pneumoniae producing an extended-spectrum β-lactamase. Antimicrob Agents Chemother. 1990;34:1290–1293. doi: 10.1128/aac.34.6.1290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akindele JA, Rotilu IO. Outbreak of neonatal Klebsiella septicemia: a review of antimicrobial sensitivities. J Med Sci. 1997;26:51–53. [PubMed] [Google Scholar]
- Ingham B, Brentnall DW, Dale EA, McFadzean JA. Arthropathy induced by antibacterial fused N-alkyl-4-pyridone-3-carboxylic acids. Toxicol Lett. 1977;1:21–26. doi: 10.1016/0378-4274(77)90016-9. [DOI] [Google Scholar]
- Grady R. Safety profile of quinolone antibiotics in the pediatric population. Pediatr Infect Dis J. 2003;22:1128–1132. doi: 10.1097/01.inf.0000101994.25947.12. [DOI] [PubMed] [Google Scholar]
- Nicholson JF, Pesce MA. In: Nelson Textbook of Pediatrics. 17. Behrman RE, Kliegman R, Jenson HB, editor. Philadelphia: Saunders; 2004. Laboratory medicine, drug therapy and reference tables; pp. 2393–2505. [Google Scholar]