Abstract
Background
Atypical deglutition is exacerbated by stress and anxiety. Several therapeutic approaches have been employed to treat stress and anxiety disorders, ranging from typical psychopharmacological strategies to novel physical protocols, such as transcranial magnetic stimulation and radioelectric asymmetric conveyor (REAC) stimulation. The purpose of the present study was to test the efficacy of REAC brain stimulation in atypical deglutition.
Methods
The position of the lingual apex (Payne method), pattern of free deglutition, and subjective and objective impression of deglutition were evaluated in 128 outpatients suffering from atypical deglutition. Deglutition testing consisted of an operator holding down the lower lip, hence counteracting the strength exerted by the orbicularis muscle. All subjects were treated using two REAC brain stimulation protocols. Patients were assessed before treatment, immediately after treatment, and three months following the last cycle of REAC therapy.
Results
REAC stimulation led to an improvement in positioning of the lingual apex and a significant decrease of muscle involvement in all patients immediately after REAC treatment, and the improvement was maintained at three-month follow-up.
Conclusion
In the present study, the REAC therapeutic protocols led to normalization in lingual apex positioning and significant improvement in swallowing in all participants suffering from atypical deglutition.
Keywords: atypical deglutition, stress, anxiety, radioelectric asymmetric brain stimulation
Introduction
Atypical deglutition1–11 is a pathological phenomenon affecting an increasing number of people in the general population.12 AD is characterized by the persistence in adults of swallowing typical in infants. Several studies have investigated the etiology13–20 and treatment21– 24 of the condition. Despite few relevant references in the literature,25,26 it is well accepted that atypical deglutition is linked to several stress conditions and, as such, treatment has recently focused on stress and anxiety reduction. The purpose of the present study was to evaluate the efficacy of treatment using brain stimulation with a radioelectric asymmetric conveyor (REAC),27,28 specifically developed for progressive and long-term neuropsychophysical optimization of global brain function. It was hypothesized that the objective and subjective clinical picture of patients suffering from atypical deglutition may be significantly improved by reduction of stress using REAC brain stimulation.
Materials and methods
This naturalistic study29 was conducted in 128 patients suffering from atypical deglutition (68 males and 60 females) aged 9–27 years. Participants were referred by their dentists to the Rinaldi-Fontani Institute in Florence, Italy, which has specialized in the diagnosis and treatment of a broad range of stress-related disorders for over 20 years. Patients were dissatisfied with the results of their ongoing orthodontic treatment and had specifically requested nonorthodontic or nonpharmacological treatment. Patients were subjected to a preliminary clinical examination, including assessment of mimic muscle involvement in deglutition, lingual apex position by distribution of fluorescein in the mouth using the Payne method,30 and an objective assessment by the physician of deglutition ability by pinching and lowering of the patient’s lower lip to counteract the force exerted by the orbicularis muscle. After a baseline assessment, the first REAC brain stimulation protocol, ie, neuropostural optimization,31 was administered. This protocol, consisting of a single 500 msec pulse in a specific area of the ear located at the top of the lower third of the scapha, was specifically designed for reorganization of neuromuscular control. Clinical evaluation was repeated 10 minutes following REAC
During the second phase of the study, patients received the REAC treatment, ie, neuropsychophysical optimization, which is specifically designed for stress-related disorders.32–37 Neuropsychophysical optimization consists of a sequence of seven 500 msec pulses on seven reflex auricular points (vegetative, kidney, stomach, heart, occipital, hypothalamic, and prefrontal cortex points) in an attempt to reproduce the physiological response to stress. The neuropsychophysical optimization treatment cycle consisted of 18 therapy sessions, administered on alternate days. Clinical evaluations were repeated at the end of treatment and at a three-month follow-up visit. All procedures were carried out in accordance with the ethical principles for medical research involving human subjects laid down by the World Medical Association Declaration of Helsinki. Each patient or parent/guardian signed their written informed consent prior to entry into the study.
REAC device
The REAC is a medical biostimulation device based on innovative technology.27,28 The frequency setting of the device (typically 2.4, 5.8, or 10.5 gHz) is selected by the operator for each specific protocol. Our protocol for this study used a frequency of 10.5 gHz, with a specific absorption rate of 7 μW/kg. The REAC pulse consisted of seven radiofrequency bursts of 500 msec each, applied by touching the metallic tip of the REAC probe to the ear pavilion according to the neuropostural optimization and neuropsychophysical optimization protocols. REAC stimulation has been shown to be an effective treatment for stress-related disorders, depression, and anxiety.32–37 The treatments are painless, noninvasive, and without adverse effects.
Results
At the baseline assessment, all patients showed varying degrees of muscle involvement in deglutition, especially with regard to the orbicularis muscle of the lips and the chin muscle. None of the patients examined could swallow when the operator pinched and pulled down the lower lip. All patients breathed almost exclusively through their mouths. Of the 128 patients who underwent the procedure, 37 showed placement of the lingual apex on the lower incisors, 44 showed placement between the lower and upper incisors, and 47 showed placement on the upper incisors during swallowing (Table 1). Furthermore, 77 patients demonstrated lateralization of positioning of the lingual apex, with 44 to the right and 33 to the left. After neuropostural optimization, there was a significant decrease in involvement of the mimic muscles during swallowing in all patients, both with regard to subjective perception and objective evaluation. All patients declared that swallowing was easier.
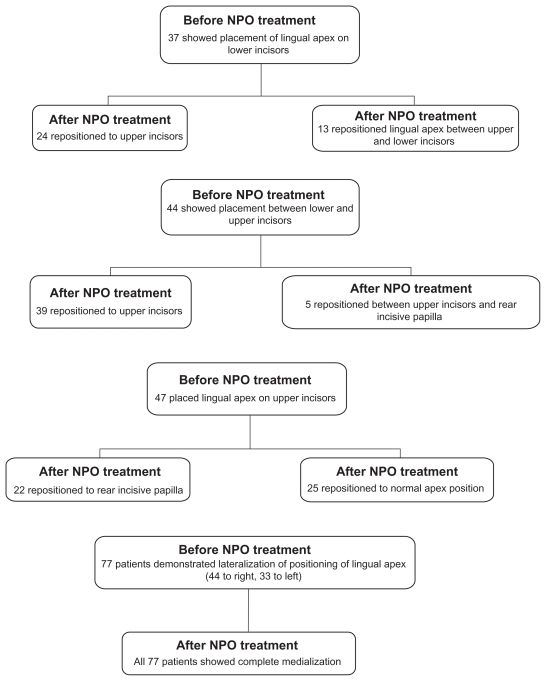
Table 1.
Treated groups and results
Abbreviation: NPO, neuropostural optimization.
After neuropostural optimization, 24 of the 37 patients who initially placed the lingual apex on the lower incisors then repositioned to the upper incisors, while the other 13 repositioned the lingual apex from the upper to the lower incisors. Of the 44 patients who placed the lingual apex between the upper and lower incisors at baseline, 39 repositioned to the upper incisors and five repositioned between the upper incisors and the rear incisive papilla. Of the 47 patients who initially placed the lingual apex on the upper incisors, 22 repositioned to the rear incisive papilla (Table 1 and Figure 1) and 25 to the normal apex position (Table 1 and Figure 2). All 77 patients with baseline lateralization of the lingual apex showed complete medialization with treatment (Figure 3). In addition, the previous atypical propulsive swallowing pattern normalized in 20 patients. All patients swallowed more easily when the physician pinched and lowered the lower lip. Lastly, breathing was improved in all patients. At three-month follow-up, lingual apex repositioning remained stable, with further slight improvement in the majority of patients.
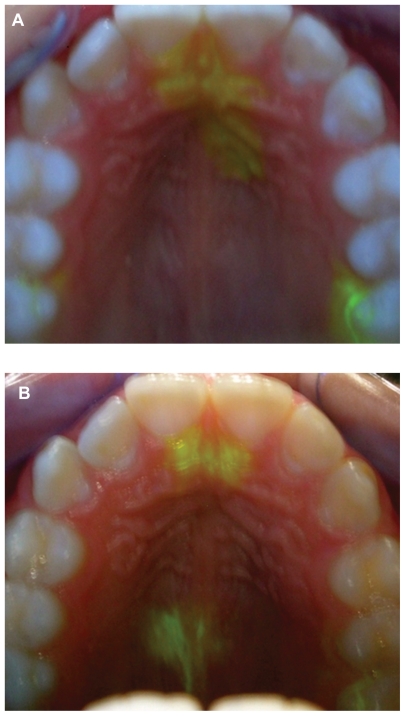
Figure 1.
(A) Lingual apex positioned at upper incisors and (B) lingual apex repositioned to the rear incisive papilla.
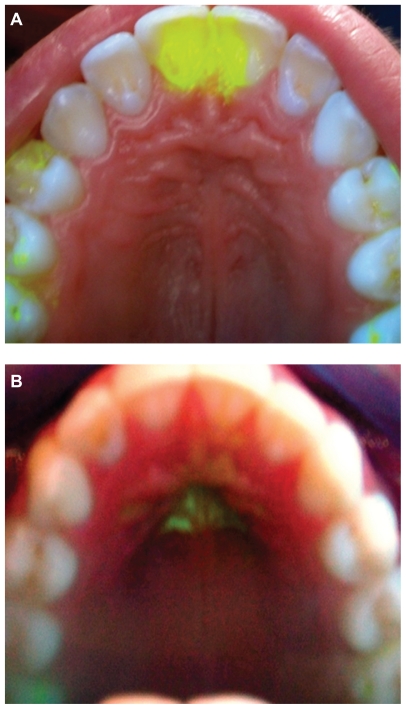
Figure 2.
(A) Lingual apex positioned at the upper incisors and (B) repositioning of the lingual apex to the normal lingual apex position.
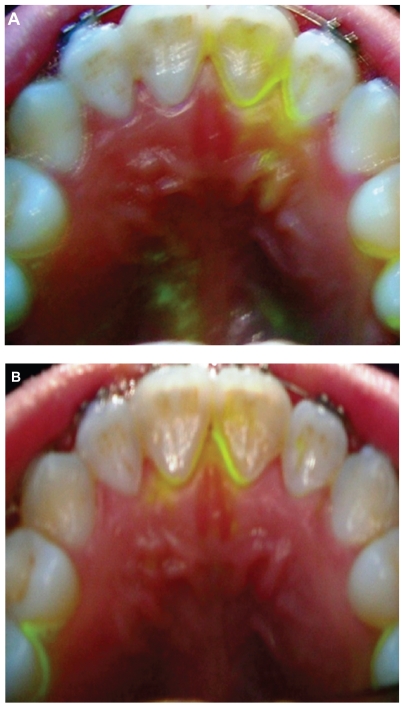
Figure 3.
(A) Lateralization of the lingual apex and (B) repositioning of the lingual apex to the middle position.
Conclusion
In the present study, the REAC therapeutic protocols (neuropostural optimization and neuropsychophysical optimization) led to normalization in lingual apex positioning and significant improvement in swallowing in all participants suffering from atypical deglutition. Global clinical amelioration of atypical deglutition was promisingly stable. The further improvement observed at three-month follow-up may be the result of a progressive normalization process, most likely related to synchronization of activity in the swallowing control areas of the brain.
Footnotes
Disclosure
Salvatore Rinaldi and Vania Fontani are the inventors of the radioelectric asymmetric conveyor.
References
- 1.Capozzi L, Negri PL. Atypical deglutition: clinico-therapeutic contribution. Ann Stomatol (Roma) 1966;15(4):249–270. Italian. [PubMed] [Google Scholar]
- 2.Casardi T, Ruju C, Melis MT. A method of phonetic re-education in cases of childhood atypical deglutition associated with orthodontic therapy. Dent Cadmos. 1984;52(Suppl 5):57–59. Italian. [PubMed] [Google Scholar]
- 3.Cohen FF, Vallado SY. Atypical deglutition. Rev Bras Odontol. 1978;35(1):21–24. Portuguese. [PubMed] [Google Scholar]
- 4.Farronato GP, Preteroti AM, Salvato A, Bruno E. Relation between skeletal open bite and atypical deglutition. Arch Stomatol (Napoli) 1982;23(1):53–74. Italian. [PubMed] [Google Scholar]
- 5.Jeanmonod A. Role of atypical deglutition in the development of masticatory apparatus dysfunction. Bull Acad Natl Chir Dent. 1988;34(34):35–40. French. [PubMed] [Google Scholar]
- 6.Miotti F, Ferro R, Crapisi S. Inter-incisal spaces and atypical deglutition: considerations on reflexes and parafunctions. G Stomatol Ortognatodonzia. 1984;3(3):452–455. Italian. [PubMed] [Google Scholar]
- 7.Riccioli GA. Certain cases of atypical deglutition (the tongue is an important factor in the etiopathogenesis of many dento-maxillary abnormalities) Mondo Odontostomatol. 1972;14(3):461–465. Italian. [PubMed] [Google Scholar]
- 8.Santini RM, Collarini M, Taboada N, Tosi R, Schiavelli H, de Batkis T. The morphologic changes in atypical deglutition. Rev Asoc Odontol Argent. 1968;56(1):23–25. Spanish. [PubMed] [Google Scholar]
- 9.Tani G. Atypical deglutition as a cause of the incidence of interincisor diastema. (Preliminary note) Riv Ital Stomatol. 1965;20(10):1258–1270. Italian. [PubMed] [Google Scholar]
- 10.Tenenbaum M, Berman GR. Atypical deglutition – myofunctional and mechanical therapy. Ortodoncia. 1971;35(69):30–45. Spanish. [PubMed] [Google Scholar]
- 11.Verkindere MT, Lodter C, Cadet D. Electromyographic studies of typical and atypical deglutition. Chir Dent Fr. 1984;54(264):51–55. France. [PubMed] [Google Scholar]
- 12.Monaco A, Cattaneo R, Spadaro A, Marchetti E, Barone A. Prevalence of atypical swallowing: a kinesiographic study. Eur J Paediatr Dent. 2006;7(4):187–191. [PubMed] [Google Scholar]
- 13.Garattini G, Crozzoli P, Grasso G. Etiopathogenesis and early treatment of malocclusions related to persistence of atypical deglutition. Mondo Ortod. 1991;16(2):149–156. Italian. [PubMed] [Google Scholar]
- 14.Machado AJ, Jr, Crespo AN. Radiographic position of the hyoid bone in children with atypical deglutition. Eur J Orthod. 2011 February 4; doi: 10.1093/ejo/cjq167. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 15.Sheppard IM, Sheppard SM. The relationship of vertical dimension of atypical swallowing with complete dentures. J Prosthet Dent. 1977;38(3):249–253. doi: 10.1016/0022-3913(77)90300-6. [DOI] [PubMed] [Google Scholar]
- 16.Stormer K, Pancherz H. Electromyography of the perioral and masticatory muscles in orthodontic patients with atypical swallowing. J Orofac Orthop. 1999;60(1):13–23. doi: 10.1007/BF01358712. [DOI] [PubMed] [Google Scholar]
- 17.Tosello DO, Vitti M, Berzin F. EMG activity of the orbicularis oris and mentalis muscles in children with malocclusion, incompetent lips and atypical swallowing. Part I. J Oral Rehabil. 1998;25(11):838–846. doi: 10.1046/j.1365-2842.1998.00322.x. [DOI] [PubMed] [Google Scholar]
- 18.Tosello DO, Vitti M, Berzin F. EMG activity of the orbicularis oris and mentalis muscles in children with malocclusion, incompetent lips and atypical swallowing. Part II. J Oral Rehabil. 1999;26(8):644–649. doi: 10.1046/j.1365-2842.1999.00409.x. [DOI] [PubMed] [Google Scholar]
- 19.Viti M, Mazza A, Malan R, Montaldo A. Introductory note on atypical deglutition. Parodontol Stomatol (Nuova) 1985;24(2):31–46. Italian. [PubMed] [Google Scholar]
- 20.Wilson EM, Green JR. Coordinative organization of lingual propulsion during the normal adult swallow. Dysphagia. 2006;21(4):226–236. doi: 10.1007/s00455-006-9053-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ciavarella D, Mastrovincenzo M, Sabatucci A, Parziale V, Chimenti C. Effect of the enveloppe linguale nocturne on atypical swallowing: surface electromyography and computerised postural test evaluation. Eur J Paediatr Dent. 2010;11(3):141–145. [PubMed] [Google Scholar]
- 22.Giuca MR, Pasini M, Pagano A, Mummolo S, Vanni A. Longitudinal study on a rehabilitative model for correction of atypical swallowing. Eur J Paediatr Dent. 2008;9(4):170–174. [PubMed] [Google Scholar]
- 23.Levrini A. Atypical deglutition and functional myotherapy. Mondo Ortod. 1977;19(3):24–48. Italian. [PubMed] [Google Scholar]
- 24.Louis P. The dentist and the speech therapist. A team for diagnosis and treatment of atypical deglutition. Inf Dent. 1991;73(35):3045–3052. French. [PubMed] [Google Scholar]
- 25.Weinberg LA. An evaluation of stress in temporomandibular joint dysfunction-pain syndrome. J Prosthet Dent. 1977;38(2):192–207. doi: 10.1016/0022-3913(77)90287-6. [DOI] [PubMed] [Google Scholar]
- 26.Hebling SR, Cortellazzi KL, Tagliaferro EP, et al. Relationship between malocclusion and behavioral, demographic and socioeconomic variables: a cross-sectional study of 5-year-olds. J Clin Pediatr Dent. 2008;33(1):75–79. doi: 10.17796/jcpd.33.1.3457qg88w37h2405. [DOI] [PubMed] [Google Scholar]
- 27.Rinaldi S, Fontani V, inventors; Rinaldi S, Fontani V, assignees. Radioelectric asymmetric conveyer for therapeutic use. EP1301241 (B1) US patent. 2006 October 11;
- 28.Rinaldi S, Fontani V, inventors; Rinaldi S, Fontani V, assignees. Radioelectric asymmetric conveyer for therapeutic use. 7,333,859. US patent. 2001
- 29.Leichsenring F. Randomized controlled versus naturalistic studies: a new research agenda. Bull Menninger Clin. 2004;68(2):137–151. doi: 10.1521/bumc.68.2.137.35952. [DOI] [PubMed] [Google Scholar]
- 30.Fabaron JP, Nadau R. The Payne method of the use of black light in the current diagnosis of atypical deglutition. Orthod Fr. 1976;47(0):157–161. French. [PubMed] [Google Scholar]
- 31.Sulsente AR. Ottimizzazione Neuro Posturale di un Gruppo di Sciatori d’elite [Neuropostural optimization in a group of elite skiers] [thesis] Corso di Laurea in Scienze delle Attività Motorie e Sportive, Università degli Studi di Verona, Italy, Università degli Studi di Verona; 2008. [Google Scholar]
- 32.Castagna A, Rinaldi S, Fontani V, Aravagli L, Mannu P, Margotti ML. Does osteoarthritis of the knee also have a psychogenic component? Psycho-emotional treatment with a radio-electric device vs intraarticular injection of sodium hyaluronate: an open-label, naturalistic study. Acupunct Electrother Res. 2010;35(1–2):1–16. doi: 10.3727/036012910803860968. [DOI] [PubMed] [Google Scholar]
- 33.Collodel G, Moretti E, Fontani V, et al. Effect of emotional stress on sperm quality. Indian J Med Res. 2008;128(3):254–261. [PubMed] [Google Scholar]
- 34.Mannu P, Rinaldi S, Fontani V, Castagna A, Lotti Margotti M. Radio electric treatment vs escitalopram in the treatment of panic disorders associated with major depression: an open-label, naturalistic study. Acupunct Electrother Res. 2009;34:135–149. doi: 10.3727/036012909803861040. [DOI] [PubMed] [Google Scholar]
- 35.Rinaldi S, Fontani V, Aravagli L, Margotti ML. Psychological and symptomatic stress-related disorders with radio-electric treatment: psychometric evaluation. Stress Health. 2009 Published Online: January 20, 2010. [Google Scholar]
- 36.Rinaldi S, Fontani V, Aravagli L, Mannu P. Psychometric evaluation of a radio electric auricular treatment for stress related disorders: a double-blinded, placebo-controlled controlled pilot study. Health Qual Life Outcomes. 2010;8(1):31. doi: 10.1186/1477-7525-8-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rinaldi S, Fontani V, Moretti E, et al. A new approach on stress-related depression and anxiety: neuro-psycho- physical-optimization with radio electric asymmetric-conveyer. Indian J Med Res. 2010;132:189–194. [PubMed] [Google Scholar]