Abstract
In 2009, a novel H1N1 influenza (pH1N1) virus caused the first influenza pandemic in 40 y. The virus was identified as a triple reassortant between avian, swine, and human influenza viruses, highlighting the importance of reassortment in the generation of viruses with pandemic potential. Previously, we showed that a reassortant virus composed of wild-type avian H9N2 surface genes in a seasonal human H3N2 backbone could gain efficient respiratory droplet transmission in the ferret model. Here we determine the ability of the H9N2 surface genes in the context of the internal genes of a pH1N1 virus to efficiently transmit via respiratory droplets in ferrets. We generated reassorted viruses carrying the HA gene alone or in combination with the NA gene of a prototypical H9N2 virus in the background of a pH1N1 virus. Four reassortant viruses were generated, with three of them showing efficient respiratory droplet transmission. Differences in replication efficiency were observed for these viruses; however, the results clearly indicate that H9N2 avian influenza viruses and pH1N1 viruses, both of which have occasionally infected pigs, have the potential to reassort and generate novel viruses with respiratory transmission potential in mammals.
Keywords: TRIG cassette, preparedness, infection, pathology, ecology
According to the World Health Organization, H9, together with H5 and H7 subtypes, are among the leading candidates for future influenza pandemics. H9N2 has been endemic in poultry populations across Eurasia since the mid 1990s (1–4). Avian H9 viruses display a typical avian host range; however, many recent isolates contain a leucine (L)—instead of glutamine (Q)—at position 226 in the receptor binding site of the HA protein, which facilitates preferential binding to sialic acid receptors in an α2,6 conformation (SAα2,6), typical of human influenza viruses. L226-containing H9N2 viruses show efficient replication in human airway epithelial cells and in the ferret model (5–7). Since the late 1990s, 12 cases of human H9N2 infection have been identified. In addition, H9N2 viruses have been isolated sporadically but consistently from pigs in Hong Kong special administrative region, China, and South Korea (8–10). Clinically, human H9N2 infections present as typical seasonal influenza infections, potentially allowing cases to go unreported and increasing the opportunities for the virus to transmit and reassort. Seroepidemiological studies indicate that human infections are more prevalent than reported (11–14). Experimentally, H9N2 surface genes reassorted with seasonal H3N2 internal genes have shown efficient transmission in a ferret model only after adaptation by serial passage and incorporation of amino acid changes on the surface and internal genes (15).
In Mexico in 2009, an H1N1 virus emerged from swine into the human population, quickly spread throughout the globe, and became the first pandemic virus in more than 40 y. This novel pandemic H1N1 (pH1N1) originated from a reassortment event involving human, swine, and avian influenza viruses. Recent studies indicate that this pH1N1 is present in swine populations and continues to reassort with other swine influenza viruses (16). The original swine triple reassortant virus, as well as the ensuing reassortant swine and the pH1N1, all contain the same internal gene cassette (17, 18). This triple reassortant internal gene (TRIG) cassette consists of the PB2 and PA from a North American avian virus, the PB1 from a human H3N2 seasonal virus, and the NP and NS from the classical swine H1N1. Many of the currently circulating swine viruses contain the TRIG cassette with a myriad of different surface genes. This finding has lead to the hypothesis that the TRIG cassette is a stable collection of internal genes that allows for easy surface switching (17). The continued presence of pH1N1 in swine, the propensity of pH1N1 to reassort with other influenza viruses, the occasional isolation of H9N2 viruses in swine and human populations, and the “humanization” of the receptor binding preference of H9 HA protein all underscore the real threat of a novel H9N2:pH1N1 reassortant with significant threat to the human population.
A novel pandemic virus must be antigenically distinct from currently circulating influenza viruses to have a naive population through which to spread (19). An H9N2:pH1N1 reassortant virus with a H9 surface protein on a pH1N1 backbone would be antigenically novel. The isolation of both subtypes of influenza from swine and humans makes it feasible that a natural reassortant between the two could occur. Here we describe the ability of four H9N2:pH1N1 reassortant viruses to infect and transmit in ferrets, an animal model that resembles human influenza infection and transmission. We found that these reassortant viruses can transmit by respiratory droplet transmission in ferrets, highlighting their pandemic potential.
Results
Generation of H9N2 and H9N1 Influenza Viruses with Internal Genes from pH1N1.
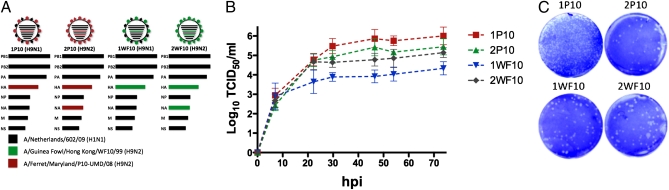
All four viruses were made with the pH1N1 internal genes (PB2, PB1, PA, NP, M, and NS) from A/Netherlands/602/2009 (H1N1) (20). The surface genes came from either A/guinea fowl/Hong Kong/WF10/1999 (H9N2) or from A/ferret/Maryland/P10_UMD/2008 (H9N2), herein referred to as WF10 and P10, respectively (15, 21). WF10 has a typical avian host range but has been shown to replicate efficiently in ferrets although transmission among ferrets occurs only with animals in direct contact (7, 15). The P10 virus is the result of 10 serial passages in ferrets of an avian-human H9N2:H3N2 reassortant containing the WF10 surface on a seasonal H3N2 (A/Memphis/14/1998) backbone (15). The P10 virus has two mutations in the HA (T189A in HA1 and G192R in HA2) and one in the NA (I28V) compared with the WF10. These amino acid changes were shown to be crucial for efficient and reproducible respiratory droplet transmission in ferrets (15). The four viruses generated in this report had P10 HA and NA (2P10), P10 HA and pH1N1 NA (1P10), WF10 HA and NA, (2WF10) or WF10 HA and pH1N1 NA (1WF10) (Fig. 1A).
Fig. 1.
Characteristics of H9N2:pH1N1 viruses in vitro. (A) Genes colored black come from pdmH1N1. Red genes originate from P10 (H9N2). Green genes are from WF10 (H9N2). (B) Replication of four reassortant viruses in MDCK cells. Six-well plates of confluent MDCK cells were inoculated with 0.1 multiplicity of infection of either 1P10 (red), 2P10 (green), 1WF10 (blue), or 2WF10 (black). Supernatants were harvested twice a day for 3 d and titered. Mean titer and SD were calculated. (C) Plaque morphology in MDCK cells for 1P10, 2P10, 1WF10, and 2WF10. Cells were infected with 1 × 10−6 dilution of stock virus except for the 1P10, in which a 1 × 10−5 dilution was used because of smaller plaque size.
Viruses grew to similar titers in Madin-Darby canine-kidney (MDCK) cells, from 106.5 to 107.2. However, 1WF10 showed slower growth indicated by lower titers at 24 h postinfection (Fig. 1B). Wan et al. (7) had previously compared the plaque morphology of wild-type WF10 to the seasonal H3N2 and the predecessor of the P10 virus, 2WF10:6M98. Seasonal H3N2 showed large plaques but WF10 formed pinpoint plaques (7). The 2WF10:6M98 and P10 plaques were of an intermediate size (15). The 1P10 showed pinpoint plaques similar to wild-type WF10 (Fig. 1C) (7, 15); 2P10, 1WF10, and 2WF10 formed plaques of intermediate size that were similar to the original 2WF10:6M98 or P10 viruses (Fig. 1C) (7, 15).
Infection, Pathology, Signs of Disease, and Transmission.
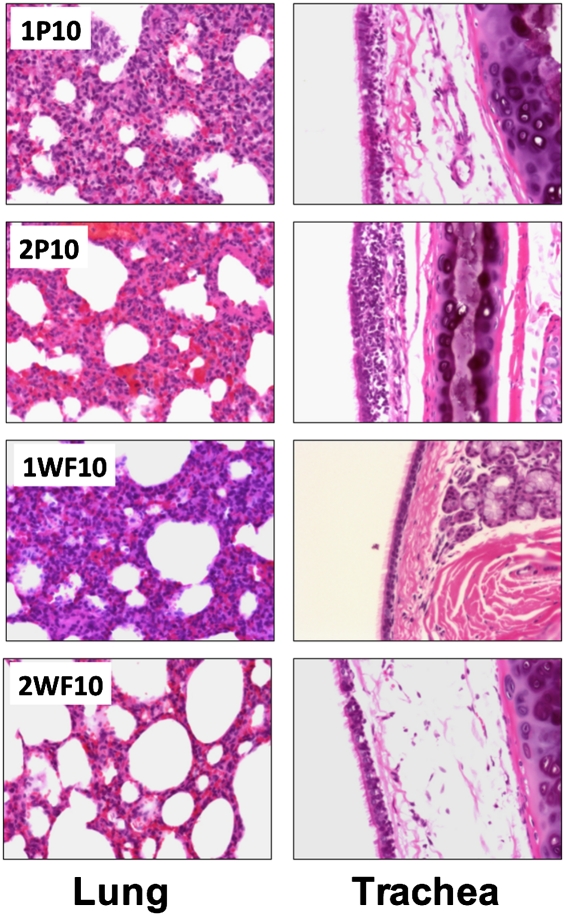
The four viruses established an infection in ferrets inoculated with 106 tissue culture infectious dose (TCID50) per ferret. Histopathological examination was performed on three H&E-stained sections of trachea and lung collected from directly inoculated ferrets at 3 and 5 days postinoculation (dpi) (Fig. 2). Virus infection in ferrets produced acute to subacute (5 dpi) tracheitis and bronchointerstitial pneumonia that was more severe at 5 dpi. The airways (trachea, bronchi, bronchioles) were minimally to mildly affected. It was in the alveolar spaces/interstitium where the lesions were most prominent. Acute to subacute bronchointerstitial pneumonia was characterized by expansion of the alveolar septae with fibrin, edema, and a mixed inflammatory infiltrate comprised of lymphocytes, plasma cells, and macrophages with fewer neutrophils. The lesions were moderate-to-severe in 1P10 and 2P10 (Fig. 2), with occasional foci of alveolar septal necrosis, multifocal hemorrhage, and alveolar hyaline membranes. In the 1P10 ferrets the inflammation was more severe, although there was less hemorrhage. The bronchointerstitial pneumonia was mild-to-moderate in 1WF10 and 2WF10 ferrets. Tracheal lesions consisted of minimal-to-mild acute inflammation characterized by submucosal edema with sparse inflammatory infiltrates. In 2WF10 ferrets the lesions were slightly more advanced as there was mild multifocal subacute tracheitis characterized by mild-to-moderate submucosal edema, with multifocal intraepithelial lymphoplasmacytic infliltrates with fewer neutrophils and macrophages. There was occasional individual epithelial cell necrosis, occasional cilia loss, and endothelial cell hypertrophy in the submucosal blood vessels.
Fig. 2.
Pathology produced by H9N2:pH1N1 viruses. Ferrets were inoculated with 1 × 106 TCID50 of either 1P10, 2P10, 1WF10, or 2WF10 and tissues were collected at 5 dpi. Samples were cut into 5-μm thick sections and stained using a standard H&E protocol by Histoserv Inc. (Magnification: 200×.)
NP viral antigen was localized by immunohistochemistry in lung and tracheal samples from 5 dpi. NP was clearly seen in the alveolar septae in regions characterized by interstitial pneumonia (Fig. S1). Areas of the lungs that did not show alveolar expansion, particularly in regions of the 2WF10-infected lung, did not show positive NP reaction. The airways, most notably the trachea (Fig. S1), showed far less NP production. Typically, virus in the trachea was mostly localized to the subepithelial mucosal layer, with infrequent localization to the epithelial layer. Virus was not located in the trachea of the WF10-infected ferrets and is consistent with the minimal pathology seen.
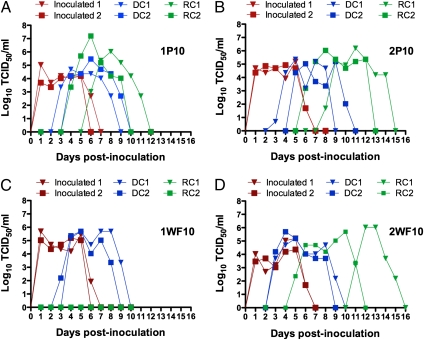
The four viruses grew to similar titers in inoculated (DI) ferrets and were cleared in a similar time frame (Fig. 3, red lines). Additionally, all four viruses were able to transmit to direct contact (DC) ferrets (Fig. 3, blue lines), which shed virus and cleared the infection in a similar fashion. Differences were seen, however, in the respiratory contact (RC) ferrets (Fig. 3, green lines). Only three viruses were able to transmit in RC ferrets. Differences were apparent in the efficiency of respiratory droplet transmission. The 1P10 transmitted the fastest (4–6 dpi) and grew to the highest titers of any of the RC groups (Fig. 3A). The 2P10 transmitted slower (6–8 dpi) and grew to slightly lower titers (Fig. 3B). The 1WF10 failed to transmit to ferrets via respiratory droplets (Fig. 3C). Finally, the 2WF10 showed a more diverse transmission profile (Fig. 3D). The first RC ferret became positive for infection 6 d before the other RC, but the virus grew to a lower titer. Ferrets lost weight and had at least 1 d of observed fever (Table S1), with the exception being the two RC ferrets for the 1WF10 virus that did not become infected. Additional signs of disease observed included increase in sneezing, mild depression, and mild diarrhea. Despite the small number of animals used, our studies clearly show significant compatibility between the HA of H9 influenza viruses and the pH1N1 backbone to produce pathology and transmission in the ferret model.
Fig. 3.
Nasal wash titers from DI, DC, and RC ferrets. Ferrets (red lines) were infected with 1× 106 TCID50 of 1P10 (A), 2P10 (B), 1WF10 (C), or 2WF10 (D). At 1 dpi, one inoculated ferret was moved to a clean isolator with a naive ferret in direct contact (DC, blue lines). Additionally, another naive ferret was placed in the same isolator in a manner such that no direct contact was possible, only respiratory droplet contact (RC, green lines). Nasal washes were collected daily and titered in MDCK cells. Each virus was tested in duplicate.
Molecular Changes Associated with Transmission.
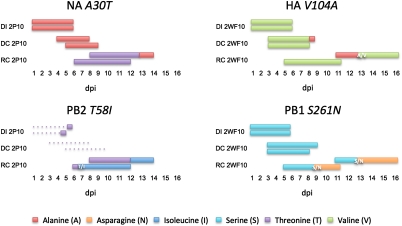
Nasal washes from RC ferrets on the day of peak shedding were passed once in MDCK cells and then sequenced to determine if genetic changes had arisen that could account for differences seen in titer and transmission between and within the infected groups. The virus recovered from 1P10 was found to have accrued no mutations in the ferrets. The 2P10 showed two nonsynonymous mutations that were identical in the two RC ferrets. The alanine residue at position 30 of the NA protein was mutated to a threonine (A30T) and the threonine residue at position 58 of PB2 was altered to an isoleucine (T58I). The 2WF10 also showed two nonsynonymous mutations. Serine at position 261 of the PB1 was changed to an asparagine (S261N) and was seen in both RC ferrets. Finally, valine at position 104 of the HA protein was switched to alanine (V104A). The V104A mutation was only seen in the 2WF10 RC ferret with significantly reduced speed of transmission (Fig. 3D, green line with triangle).
To confirm that these changes had occurred during transmission in ferrets and not in tissue culture cells, sequencing at the site of the mutations was performed on viral RNA samples obtained directly from nasal washes from every positive sample (Fig. 4). The NA A30T mutation in the RC2P10 group was found in both ferrets on the first day virus was shed. There was a reversion to wild-type (A30) on the final 2 d of shedding for one RC ferret, but the other consistently shed virus with the mutation (T30) on all days. The mutation was never detected in the DI or DC ferrets. The PB2 T58I mutation of the RC2P10 group arose posttransmission for both RC ferrets. Likewise, the PB1 S261N mutation in the RC2WF10 ferrets appeared days after transmission. The HA V104A mutation seen in only one RC2WF10 ferret occurred in the DC2WF10 ferret associated with it on the last day of shedding (9 dpi). The RC2WF10 ferret began shedding virus with the A104 11 dpi, but on 13 dpi shed a mixed population and fully reverted to wild-type (V104) for the final 2 d of shedding.
Fig. 4.
Amino acid mutations during transmission of H9N2:pH1N1 viruses. Sequences from virus-positive nasal washes were generated for every ferret at the site in which a mutation was observed during peak shedding compared with the wild-type virus. Solid lines indicate days in which sequences were performed. Dotted lines indicated days in which viruses were detected but no sequences were generated (PB2 T58I DI and DC 2P10). Amino acids are indicated in color. A/V, T/I, and S/N indicate mixed virus population on the date shown.
Discussion
In this study we tested the compatibility between the HA of an H9 subtype influenza virus and the rest of genes from a prototypical pH1N1. Our results indicate that the pH1N1 and a wild-type avian H9N2 are compatible for reassortment and capable of creating viruses with the ability to infect and transmit via respiratory contact in ferrets. Previous results indicate that an H9N2:H3N2 (2WF10:6M98) reassortant could infect and transmit to DC ferrets. However, transmission to RC ferrets only occurs after serial passage and adaption in ferrets (P10) (15). Interestingly, we show that the wild-type WF10 surface genes in the background of the pH1N1 virus can infect and transmit to RC ferrets with no need of adaption, which is consistent with our previous observations on the efficient transmission of pH1N1 viruses in the ferret model. Nevertheless, adapting the H9N2 surface genes to ferrets results in viruses with more efficient transmission profiles, similar upper respiratory tract pathology, and increased lung pathology. These results are significant because they show that the adaptive changes identified on the surface of the P10 virus do provide a transmission advantage in more than one virus background.
It is also notable to compare the 1WF10 and the 2WF10 viruses. These viruses differ only in the origin of their NA segment. The 1WF10 (pH1N1 NA) shows reduced titer (Fig. 1) compared with the 2WF10 (H9N2 NA). Additionally, the mismatched surface proteins of the 1WF10 caused a phenotypic change in respiratory transmission (Fig. 3). This finding indicates that the 2WF10 virus with surface genes of shared origin is more fit than the 1WF10 with surface genes of mixed origin. However, and perhaps more importantly, because the 1P10 (H9N1) virus showed the fastest transmission profile of all four viruses, it also suggests that just two amino acid changes (P10 mutations T189A in HA1 and G192R in HA2 compared with WF10), provide the necessary balance between HA and NA activities to improve viral fitness and transmission. This phenomenon has been seen in pandemic viruses before. The 1957 H2N2 pandemic arose from a reassortment in which both surface genes were replaced with an avian set of surface genes; however, the H3 HA of avian origin was perfectly compatible with the N2 NA from the human strain in the 1968 H3N2 pandemic (22, 23).
These results also support the idea that the TRIG cassette confers an infection/transmission advantage to a virus regardless of surface genes. The H9N2 with seasonal H3N2 internal genes could not transmit to respiratory contacts. However, the same surface genes with the TRIG cassette transmitted via respiratory contact. These results are consistent with the fact that, after 80 y as the dominant subtype in swine population in North America, the classic swine H1N1 was replaced in a few years by an assortment of TRIG viruses.
Pathologically, these viruses are similar to the seasonal strains of human influenza. The infected lungs show mild-to-moderate bronchointerstitial pneumonia similar to what is seen with seasonal H3N2 (24), seasonal H1N1, and pH1N1 (25, 26) infections in ferrets. Tracheal pathology was again similar to pathology seen in typical human virus infections (24–26). Recently, Sun et al. determined the growth characteristics and pathology associated with 127 H9 containing H9N2:pH1N1 reassortants in mice (27). Although ∼25% of these ressortants showed similar pathology to either parental virus, about 10% showed pathogenicity higher than either virus. These results and ours highlight the potential for a H9:pH1N1 reassortant virus with increased pathogenicity and respiratory transmissibility.
Although amino acid changes were identified in RC contact ferrets for some of these viruses, it is unlikely that these changes were determinants for transmission because they were not found in nasal washes from DI or DC ferrets. We do not know if these four artificially created reassortants would be created during a coinfection in the field. It is unknown if these reassortants would be the most fit or if some other combination would be more suitable. It needs to be determined if these or some other reassortant virus would out-compete either parental virus in a naive host and what effects preexisting immunity would have. These experiments were performed in ferrets, a model of human infection, but other intermediate species, such as swine or poultry, might act as better hosts for reassortment. Our results highlight the need to develop better H9N2 surveillance in both swine and humans as these viruses continue to show features consistent with pandemic potential.
Materials and Methods
Viruses and Cells.
The reverse genetic systems for WF10 (H9N2), P10 (H9N2), and pH1N1 viruses have been previously described (28). The plasmid set for pH1N1 was kindly provided by Ron A. Fouchier, Erasmus Medical Center, Rotterdam, The Netherlands. The viruses were generated by reverse genetics as previously reported (28). Virus stocks were produced in MDCK cells. Full-length sequencing of viral stocks was performed to verify gene combinations and later for mutation analysis of respiratory droplet contact samples. Sequences were generated using the Big Dye Terminator v3.1 Cycle Sequencing kit 1 in a 3500 Genetic Analyzer (Applied Biosystems).
Four reassortant viruses were generated: the 1WF10 virus encodes the HA from WF10 and the remaining seven genes from pH1N1; the 2WF10 virus contains the HA and NA from WF10 and the remaining six genes of pH1N1; the 1P10 virus contains the HA from (P10) and the other seven genes from pH1N1, whereas the 2P10 contains the HA and NA genes from P10 and the remaining six genes from pH1N1. The median TCID50 of each virus as well as titers for the growth curve experiments was determined in MDCK cells.
Plaque Assays.
Briefly, confluent MDCK cell monolayers in six-well plates were infected with 10-fold dilutions of virus for 1 h at 37 °C. Cells were washed twice with PBS and covered with an overlay of modified Eagle's medium containing 0.9% agar, 0.02% BSA, 1% glutamine, and 1 μg/mL trypsin. After 3 d of incubation at 37 °C, 5% CO2, the overlays were removed and the cells were stained with Crystal violet.
Infection and Transmission in Ferrets.
Infection and transmission were carried out as described previously (7). Complete description of the experimental approach in ferrets is provided in SI Materials and Methods. Briefly, 3- to 7-mo-old ferrets were used in which a temperature transponder was introduced. Transmission studies were performed in an ABSL3+ facility in wire cages inside HEPA-filtered isolators (7). Animal studies were approved by the Animal Care and Use Committee of the University of Maryland (protocol RO-09-93). Each experiment consisted of three ferrets in duplicate for each virus. One ferret was inoculated intranasally (DI) with 106 TCID50 of virus. At 1 dpi, two naive ferrets were added to the cage. One ferret was added in direct contact (DC) with the DI ferret, and the second naive ferret was added to the other half of the cage separated by two layers of thin wire mesh allowing only respiratory contact (RC). Body weight and temperature were measured daily and nasal washes were collected for 14 dpi (except where noted). Nasal washes were collected as described (7) and tested for virus by FluDetect (Synbiotics Corp.), aliquoted, and stored at −80 °C until use. Seroconversion was detected at 14 dpi. Two additional ferrets were infected with each virus for pathology and virus localization at 3 and 5 dpi.
Supplementary Material
Acknowledgments
We thank Troy Sutton, Lindomar Pena, and Yonas Araya for their help with animal studies; Jianqiang Ye for assistance with the ELISA assays; Amy Vincent for her assistance with the immunohistochemistry protocol; and Theresa Wolter-Marth and Andrea Ferrero for coordination of animal studies. This research was funded by Grants 1U01CI000355-01 from the Centers for Disease Control and Prevention-Department of Health and Human Services and 2007-04981 from the National Institute of Food and Agriculture-US Department of Agriculture, and Contract HHSN266200700010C from the National Institute of Allergy and Infectious Diseases-National Institutes of Health, and a Cooperative Agreement from the US Department of Agriculture-Agricultural Research Service.
Footnotes
The authors declare no conflict of interest.
This article is a PNAS Direct Submission.
This article contains supporting information online at www.pnas.org/lookup/suppl/doi:10.1073/pnas.1108058108/-/DCSupplemental.
References
- 1.Alexander DJ. A review of avian influenza in different bird species. Vet Microbiol. 2000;74:3–13. doi: 10.1016/s0378-1135(00)00160-7. [DOI] [PubMed] [Google Scholar]
- 2.Lee CW, et al. Sequence analysis of the hemagglutinin gene of H9N2 Korean avian influenza viruses and assessment of the pathogenic potential of isolate MS96. Avian Dis. 2000;44:527–535. [PubMed] [Google Scholar]
- 3.Naeem K, Ullah A, Manvell RJ, Alexander DJ. Avian influenza A subtype H9N2 in poultry in Pakistan. Vet Rec. 1999;145:560. doi: 10.1136/vr.145.19.560. [DOI] [PubMed] [Google Scholar]
- 4.Perk S, et al. Ecology and molecular epidemiology of H9N2 avian influenza viruses isolated in Israel during 2000–2004 epizootic. Dev Biol (Basel) 2006;124:201–209. [PubMed] [Google Scholar]
- 5.Matrosovich MN, Krauss S, Webster RG. H9N2 influenza A viruses from poultry in Asia have human virus-like receptor specificity. Virology. 2001;281:156–162. doi: 10.1006/viro.2000.0799. [DOI] [PubMed] [Google Scholar]
- 6.Wan H, Perez DR. Amino acid 226 in the hemagglutinin of H9N2 influenza viruses determines cell tropism and replication in human airway epithelial cells. J Virol. 2007;81:5181–5191. doi: 10.1128/JVI.02827-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wan H, et al. Replication and transmission of H9N2 influenza viruses in ferrets: Evaluation of pandemic potential. PLoS ONE. 2008;3:e2923. doi: 10.1371/journal.pone.0002923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maines TR, et al. Pathogenesis of emerging avian influenza viruses in mammals and the host innate immune response. Immunol Rev. 2008;225(1):68–84. doi: 10.1111/j.1600-065X.2008.00690.x. [DOI] [PubMed] [Google Scholar]
- 9.Peiris JS, et al. Cocirculation of avian H9N2 and contemporary “human” H3N2 influenza A viruses in pigs in southeastern China: Potential for genetic reassortment? J Virol. 2001;75:9679–9686. doi: 10.1128/JVI.75.20.9679-9686.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Peiris M, et al. Human infection with influenza H9N2. Lancet. 1999;354:916–917. doi: 10.1016/s0140-6736(99)03311-5. [DOI] [PubMed] [Google Scholar]
- 11.Jia N, et al. Increased sensitivity for detecting avian influenza-specific antibodies by a modified hemagglutination inhibition assay using horse erythrocytes. J Virol Methods. 2008;153:43–48. doi: 10.1016/j.jviromet.2008.06.016. [DOI] [PubMed] [Google Scholar]
- 12.Guo Y, Li J, Cheng X. Discovery of men infected by avian influenza A (H9N2) virus. (Translated from Chinese) Chinese Journal of Experimental and Clinical Virology. 1999;13:105–108. [PubMed] [Google Scholar]
- 13.Butt KMSG, et al. Human infection with an avian H9N2 influenza A virus in Hong Kong in 2003. J Clin Microbiol. 2005;43:5760–5767. doi: 10.1128/JCM.43.11.5760-5767.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith GJ, et al. Origins and evolutionary genomics of the 2009 swine-origin H1N1 influenza A epidemic. Nature. 2009;459:1122–1125. doi: 10.1038/nature08182. [DOI] [PubMed] [Google Scholar]
- 15.Sorrell EM, Wan H, Araya Y, Song H, Perez DR. Minimal molecular constraints for respiratory droplet transmission of an avian-human H9N2 influenza A virus. Proc Natl Acad Sci USA. 2009;106:7565–7570. doi: 10.1073/pnas.0900877106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vijaykrishna D, et al. Reassortment of pandemic H1N1/2009 influenza A virus in swine. Science. 2010;328:1529. doi: 10.1126/science.1189132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ma WKR, Kahn RE, Richt JA. The pig as a mixing vessel for influenza viruses: Human and veterinary implications. J Mol Genet Med. 2008;3:158–166. [PMC free article] [PubMed] [Google Scholar]
- 18.Vincent ALMW, Ma W, Lager KM, Janke BH, Richt JA. Swine influenza viruses a North American perspective. Adv Virus Res. 2008;72:127–154. doi: 10.1016/S0065-3527(08)00403-X. [DOI] [PubMed] [Google Scholar]
- 19.Smith GJ, et al. Dating the emergence of pandemic influenza viruses. Proc Natl Acad Sci USA. 2009;106:11709–11712. doi: 10.1073/pnas.0904991106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Munster VJ, et al. Pathogenesis and transmission of swine-origin 2009 A(H1N1) influenza virus in ferrets. Science. 2009;325:481–483. doi: 10.1126/science.1177127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Perez DR, et al. Role of quail in the interspecies transmission of H9 influenza A viruses: Molecular changes on HA that correspond to adaptation from ducks to chickens. J Virol. 2003;77:3148–3156. doi: 10.1128/JVI.77.5.3148-3156.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Scholtissek C, Rohde W, Von Hoyningen V, Rott R. On the origin of the human influenza virus subtypes H2N2 and H3N2. Virology. 1978;87:13–20. doi: 10.1016/0042-6822(78)90153-8. [DOI] [PubMed] [Google Scholar]
- 23.Wagner R, Matrosovich M, Klenk HD. Functional balance between haemagglutinin and neuraminidase in influenza virus infections. Rev Med Virol. 2002;12:159–166. doi: 10.1002/rmv.352. [DOI] [PubMed] [Google Scholar]
- 24.Memoli MJJB, et al. Recent human influenza A/H3N2 virus evolution driven by novel selection factors in addition to antigenic drift. J Infect Dis. 2009;200:1232–1241. doi: 10.1086/605893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Munster VJ, et al. Pathogenesis and transmission of swine-origin 2009 A(H1N1) influenza virus in ferrets. Science. 2009;325:481–483. doi: 10.1126/science.1177127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rowe TLA, et al. Modeling host responses in ferrets during A/California/07/2009 influenza infection. Virology. 2010;401:257–265. doi: 10.1016/j.virol.2010.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sun Y, et al. High genetic compatiblity and increased pathologenicity of reassortants derived from avian H9N2 and pandemic H1N1/2009 influenza viruses. Proc Natl Acad Sci USA. 2011;108:4164–4169. doi: 10.1073/pnas.1019109108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hoffmann E, Neumann G, Kawaoka Y, Hobom G, Webster RG. A DNA transfection system for generation of influenza A virus from eight plasmids. Proc Natl Acad Sci USA. 2000;97:6108–6113. doi: 10.1073/pnas.100133697. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.