Abstract
OBJECTIVE
To describe diabetes prevalence in New York City by race/ethnicity and nativity.
RESEARCH DESIGN AND METHODS
Data were from the New York City 2002–2008 Community Health Surveys. Respondents were categorized on the basis of self-reported race/ethnicity and birth country: foreign-born South Asian (Indian subcontinent), foreign-born other Asian, U.S.-born non-Hispanic black, U.S.-born non-Hispanic white, and U.S.-born Hispanic. Diabetes status was defined by self-reported provider diagnosis. Multivariable models examined diabetes prevalence by race/ethnicity and birth country.
RESULTS
Prevalence among foreign-born South Asians was nearly twice that of foreign-born other Asians (13.6 vs. 7.4%, P = 0.001). In multivariable analyses, normal-BMI foreign-born South Asians had nearly five times the diabetes prevalence of comparable U.S.-born non-Hispanic whites (14.1 vs. 2.9%, P < 0.001) and 2.5 times higher prevalence than foreign-born other Asians (P < 0.001).
CONCLUSIONS
Evaluating Asians as one group masks the higher diabetes burden among South Asians. Researchers and clinicians should be aware of differences in this population.
More than 220 million people worldwide have diabetes, and an estimated 6 million are diagnosed annually (1,2). International studies have shown that South Asians (Indian subcontinent) appear to be at greater risk for diabetes than other ethnic groups (3). The few U.S. studies conducted report similar findings, but most were either not population-based, not current, or limited by a small sample size (4–6). Our study uniquely uses a recent population-based sample large enough to allow for subgroup prevalence estimation. Community studies, especially those in urban areas with large immigrant populations such as New York City, can provide insight into racial and ethnic disease patterns.
RESEARCH DESIGN AND METHODS
Data were from New York City’s annual Community Health Survey; years 2002–2008 were combined for this analysis, excluding 2005, when diabetes information was not collected. Data were weighted to account for probability of selection and nonresponse (7).
Respondents were considered to have diabetes if they reported ever being told by a health care professional that they had diabetes, excluding gestational diabetes. The Community Health Survey did not distinguish between type 1 and type 2 diabetes.
Race and nativity
The primary independent variable was a combination of self-reported race/ethnicity and place of birth, categorized into five mutually exclusive race/nativity groups: foreign-born South Asians, foreign-born other Asians, U.S.-born non-Hispanic whites, U.S.-born non-Hispanic blacks, and U.S.-born Hispanics.
BMI and other sociodemographic variables
Potential confounders for diabetes prevalence were identified by literature review (6,8–10) and were controlled for in the analysis. These included sex, marital status, education, employment, age-group, poverty level, insurance status, and having a primary care provider.
Diabetes prevalence by BMI category, calculated on the basis of self-reported height and weight, was explored. BMI was classified as normal weight (18.5 to <25 kg/m2), overweight (≥25 to <30 kg/m2), or obese (≥30 kg/m2). For foreign-born South Asians and other Asians, alternative Asian-specific BMI categorizations recommended by the World Health Organization were also applied: normal weight (18.5 to <23 kg/m2), overweight (≥23 to <27.5 kg/m2), and obese (≥27.5 kg/m2) (8,9). Respondents with BMI <18.5 kg/m2 were excluded from this analysis.
Statistical analysis
Diabetes prevalence estimates were assessed by race/nativity group, BMI category, and sociodemographic characteristics using two-sided t tests and statistical significance at an α level <0.05. Logistic regression models examined the association between reported diabetes and race/nativity and included the following variables on the basis of literature review: sex, marital status, education, poverty level, insurance status, having a primary care provider, employment status, and two interaction terms (race/nativity by age-group and race/nativity by BMI category). A similar model, substituting Asian-specific BMI categorizations for standard BMI categorizations among foreign-born South Asians and other Asians, was also developed. Model-adjusted prevalence estimates were obtained using predicted marginals. All analyses were conducted using SAS-callable SUDAAN 10.0 (Research Triangle Institute, Research Triangle Park, NC).
RESULTS
The final combined sample size was 54,326 (1,492 were excluded because of missing diabetes or race/nativity data).
Prevalence of diabetes
The estimated total age-adjusted prevalence of self-reported diagnosed diabetes among adult New Yorkers was 9.1% (Supplementary Table 1) and was significantly higher among foreign-born individuals than among U.S.-born individuals (10.2 vs. 8.5%, P < 0.001). There was variation by Asian region, with the prevalence among foreign-born South Asians (13.6%) nearly twice that of foreign-born other Asians (7.4%). Prevalence among foreign-born South Asians was also more than twice that of U.S.-born non-Hispanic whites (5.6%), but there were no significant differences in prevalence when compared with U.S.-born non-Hispanic blacks (11.8%) and U.S.-born Hispanics (14.4%). Foreign-born South Asians and U.S.-born Hispanics had a similar prevalence of diabetes (13.6 and 14.4%, respectively), yet by standard BMI cutoff points, 67.1% (95% CI 65.7–68.5) of U.S.-born Hispanics were overweight or obese compared with 45.6% (40.5–50.7) of foreign-born South Asians (data not shown).
At normal BMI, the prevalence of diabetes among foreign-born South Asians was more than five times higher than the prevalence among U.S.-born non-Hispanic whites (14.1 vs. 2.7%, Supplementary Table 1) and was significantly higher than the prevalence among all other racial/nativity groups (P < 0.05). This pattern was not seen in other BMI categories.
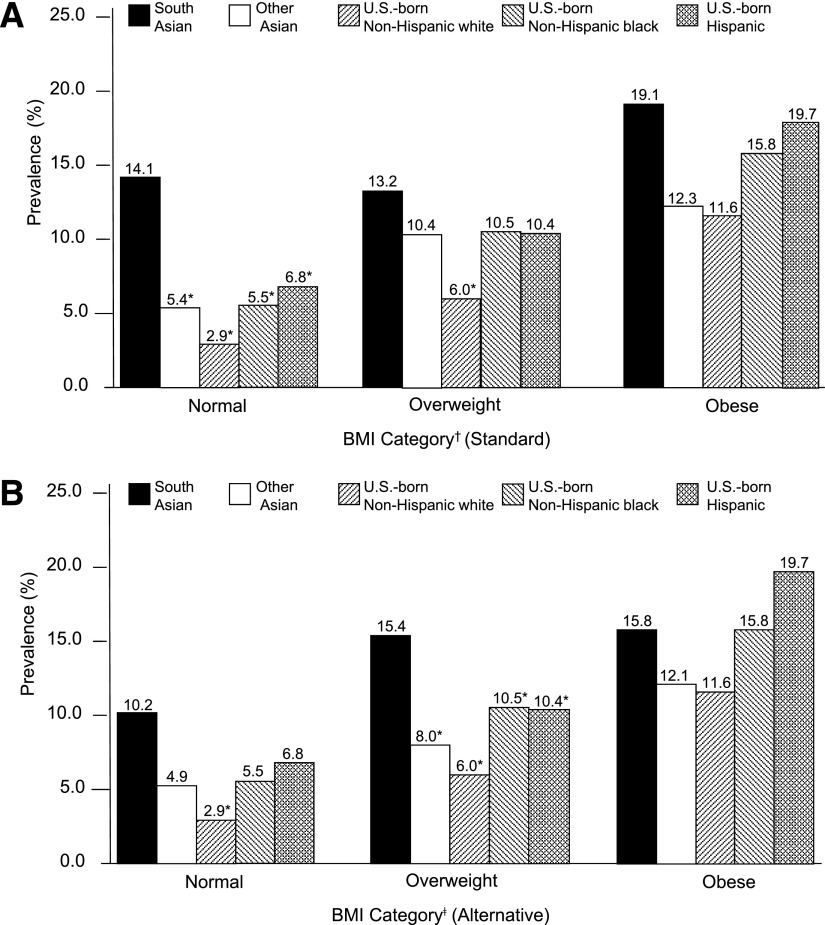
Model-adjusted prevalence of diabetes by age and BMI category
In a multivariable model using standard BMI cutoff points, diabetes prevalence among normal-BMI foreign-born South Asians remained significantly higher than the prevalence among all other race/nativity groups in the same BMI category. Diabetes prevalence among overweight-BMI foreign-born South Asians was significantly higher than the prevalence among overweight-BMI U.S.-born non-Hispanic whites (P < 0.05). However, in the obese-BMI category, there was no difference in diabetes prevalence between foreign-born South Asians and any other race/nativity group. When Asian-specific BMI categorizations were used, diabetes prevalence among normal-BMI foreign-born South Asians only remained significantly higher than the prevalence among U.S.-born non-Hispanic whites in the same BMI category; however, in the overweight-BMI category, diabetes prevalence among foreign-born South Asians increased to 15.4% and was significantly higher than the prevalence among all other race/nativity groups (Fig. 1).
Figure 1.
Prevalence of self-reported diabetes diagnosis among adults aged ≥18 years, New York City, 2002–2008, by BMI category, adjusted for age, sex, marital status, education, poverty level, insurance status, having a primary care provider, and employment status. Prevalence calculated using standard BMI categorizations (A) and Asian-specific BMI categorizations, applied only to South Asians and other Asians (B). *P < 0.05 compared with South Asians. †Standard: normal BMI, 18.5 to <25 kg/m2; overweight BMI, 25 to <30 kg/m2; obese BMI, ≥30 kg/m2. ‡Asian-specific: normal BMI, 18.5 to <23 kg/m2; overweight BMI, 23 to <27.5 kg/m2; obese BMI, ≥27.5 kg/m2.
CONCLUSIONS
We found diabetes prevalence to be significantly higher among foreign-born South Asians in New York City when compared with the prevalence among foreign-born other Asians and U.S.-born non-Hispanic whites, even after adjusting for sociodemographic and risk factors. However, foreign-born South Asians had a higher reported prevalence of diabetes at lower BMI levels than all other races/nativities, independent of socioeconomic status, suggesting that standard BMI cutoff points do not adequately encompass risks related to overweight and obesity in the Asian population.
Using Asian BMI cutoff points, the distribution of diabetes prevalence by BMI category among foreign-born South Asians shifted to a pattern more similar to that seen in the other race/nativity groups. However, the burden of disease remained high among foreign-born South Asians regardless of BMI category.
Study limitations include reliance on self-reported data, incomplete data on length of stay in the U.S., and an inability to disaggregate Asians born in the U.S. into subgroups.
Our study suggests that combining all foreign-born Asians into one category masks the larger disease burden among foreign-born South Asians. Physicians should consider screening some Asian subgroups for diabetes regardless of weight category.
Supplementary Material
Acknowledgments
No potential conflicts of interest relevant to this article were reported.
L.S.G., S.Y., and S.E.P. researched data, contributed to discussion, and wrote, reviewed, and edited the manuscript. C.C.W. researched data, contributed to discussion, and reviewed and edited the manuscript.
The authors thank Lorna Thorpe of the City University of New York and Bonnie Kerker, Jennifer Norton, James Hadler, Carolyn Greene, Elizabeth Waddell, Shadi Chamany, John Jasek, Colleen Quinn, and Margaret Millstone, all of the New York City Department of Health and Mental Hygiene, for their careful review of the manuscript.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc11-0088/-/DC1.
C.C.W. is currently affiliated with ICF International, Fairfax, Virginia.
S.Y. is no longer affiliated with the New York City Department of Health and Mental Hygiene, New York, New York.
References
- 1.World Health Organization. Diabetes fact sheet [Internet]. Available from http://www.who.int/mediacentre/factsheets/fs312/en/. Accessed 13 August 2010
- 2.King H, Aubert RE, Herman WH. Global burden of diabetes, 1995-2025: prevalence, numerical estimates, and projections. Diabetes Care 1998;21:1414–1431 [DOI] [PubMed] [Google Scholar]
- 3.Tziomalos K, Weerasinghe CN, Mikhailidis DP, Seifalian AM. Vascular risk factors in South Asians. Int J Cardiol 2008;128:5–16 [DOI] [PubMed] [Google Scholar]
- 4.Venkataraman R, Nanda NC, Baweja G, Parikh N, Bhatia V. Prevalence of diabetes mellitus and related conditions in Asian Indians living in the United States. Am J Cardiol 2004;94:977–980 [DOI] [PubMed] [Google Scholar]
- 5.Mohanty SA, Woolhandler S, Himmelstein DU, Bor DH. Diabetes and cardiovascular disease among Asian Indians in the United States. J Gen Intern Med 2005;20:474–478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rajpathak SN, Gupta LS, Waddell EN, et al. Elevated risk of type 2 diabetes and metabolic syndrome among Asians and South Asians: results from the 2004 New York City HANES. Ethn Dis 2010;20:225–230 [PubMed] [Google Scholar]
- 7.New York City Department of Health and Mental Hygiene. Community Health Survey: methodology [Internet]. Available from http://www.nyc.gov/html/doh/html/survey/chs-methods.shtml. Accessed 12 August 2010
- 8.Mokdad AH, Ford ES, Bowman BA, et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA 2003;289:76–79 [DOI] [PubMed] [Google Scholar]
- 9.Van Wye G, Kerker BD, Matte T, et al. Obesity and diabetes in New York City, 2002 and 2004. Prev Chronic Dis 2008;5:A48. [PMC free article] [PubMed] [Google Scholar]
- 10.Thorpe LE, Upadhyay UD, Chamany S, et al. Prevalence and control of diabetes and impaired fasting glucose in New York City. Diabetes Care 2009;32:57–62 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.