Abstract
OBJECTIVE
The gut environment modulates the pathogenesis of type 1 diabetes (T1D), but how it affects autoimmunity toward pancreatic β-cells, a self-tissue located outside the intestine, is still unclear. In the small intestine, lamina propria dendritic cells (LPDCs) induce peripheral differentiation of FoxP3+ regulatory T (Treg) cells. We tested the hypothesis that the intestinal milieu impinges on human T1D by affecting differentiation of FoxP3+ Treg cells.
RESEARCH DESIGN AND METHODS
We collected duodenal biopsies of 10 T1D patients, 16 healthy subjects, and 20 celiac individuals and performed a fluorescent-activated cell sorter analysis to measure percentages of various immune cell subsets, including CD4+ and CD8+ T cells, NK cells, γδ T cells, CD103+CD11c+ LPDCs, and CD4+CD25+FoxP3+CD127− Treg cells. In parallel, we assessed the tolerogenic function (i.e., capacity to induce differentiation of FoxP3+ Treg cells) by LPDCs of T1D patients and control subjects.
RESULTS
Our analysis revealed a significant reduction in the percentage of intestinal CD4+CD25+FoxP3+CD127− Treg cells in T1D patients compared with healthy subjects (P = 0.03) and celiac individuals (P = 0.003). In addition, we found that LPDCs from T1D patients completely lacked their tolerogenic function; they were unable to convert CD4+CD25− T cells into CD4+CD25+FoxP3+CD127− Treg cells.
CONCLUSIONS
Our data indicate that T1D patients have a reduced number of intestinal FoxP3+ Treg cells as a result of their defective differentiation in the gut. These findings suggest that intestinal immune regulation is not only calibrated to tolerate commensal bacteria and food components but also is instrumental in maintaining immune tolerance toward pancreatic β-cells and preventing T1D.
Type 1 diabetes (T1D) is a destructive islet β-cell specific autoimmune disease resulting from a yet undefined interaction between genetic and environmental factors (1). A dramatic increase in T1D incidence was recorded in most developed countries in the past 40 years (e.g., a threefold increase in Western countries) (2,3). The steady and rapid increase in T1D incidence cannot be ascribed to genetic variations and, thus, it must be related to environmental changes. Environmental agents such as viral infections (i.e., enteroviruses and rotaviruses) (4,5), reactions to dietary antigens (i.e., cow’s milk and gluten) (6–8), and microbiota alterations (9) that act at the intestinal level have been observed in association with, or as risk factors for, the development of T1D. The observation that development of clinical diabetes in patients is preceded by intestinal alterations such as increased permeability, immune activation, and ultrastructural abnormalities of the epithelium (10–16) provides additional evidence on the crucial role of the gut environment in human T1D. Although existing evidence is suggestive of a causative link between the gut milieu and the pathogenesis of T1D, it is still unclear whether and by which mechanism(s) a dysfunction in the intestine promotes autoimmunity elsewhere (i.e., in the pancreatic β-cells) and if it does, how this process occurs.
Important immune regulatory mechanisms reside in the intestinal mucosa. FoxP3+ regulatory T (Treg) cells, a Treg cell subset that is instrumental to controlling T1D (17), arise centrally in the thymus and peripherally in the gut (18). Specifically, lamina propria CD103+CD11c+ dendritic cells (LPDCs) are responsible for extrathymic FoxP3+ Treg cell development and expansion (18,19). Considering the key immune regulatory role of FoxP3+ Treg cells, it is clear that their defective peripheral differentiation in the gut could lead to failure of self-tolerance and autoimmune disease, particularly in tissues such as pancreatic islets and lymph nodes that are directly connected to the intestinal mucosa and gut-associated lymphoid tissue (20).
Here we demonstrate that the extrathymic differentiation of FoxP3+ Treg cells by gut-resident CD103+CD11c+ dendritic cells (DCs) is selectively impaired in humans affected by T1D. Our findings indicate that organ-specific autoimmune diseases such as T1D could be initiated and possibly maintained by virtue of changes in peripheral FoxP3+ Treg cell differentiation and/or expansion in the gut.
RESEARCH DESIGN AND METHODS
Multiparametric fluorescent-activated cell sorter analysis.
Studies were approved by the ethics committee of the San Raffaele Scientific Institute, Milan, Italy, and all participants signed an informed consent before any data collection or study procedure. Duodenal biopsies (two to three from each individual), obtained during an esophago-gastro-duodenal endoscopy, were collected in 10% RPMI and rapidly processed. Mucus and epithelial cells were removed from the tissue by incubation with 1 mmol/L dithiothreitol and 5 mmol/L EDTA in calcium- and magnesium-free Hanks’ balanced salt solution (HBSS) for 15 min at 37°C. Tissue samples were washed with HBSS; digested with 1 mg/mL collagenase A (Roche Diagnostics Ltd., Indianapolis, IN) in HBSS supplemented with calcium, magnesium, and 5 units/mL DNase I (Roche Diagnostics Ltd.) for 1 h at 37°C; and mechanically disrupted by gentle pipetting until dissociation was complete. After incubation, intestinal cells released from the tissue samples were passed through a 70 μm cell strainer and washed with complete 10% RPMI 1640 medium. Peripheral blood mononuclear cells (PBMCs) were isolated by Ficoll gradient and washed in HBSS. Intestinal cells and PBMCs were assessed for viability by trypan blue exclusion and stained with Pacific Blue–conjugated anti-human CD4, Alexa Fluor-488–conjugated anti-human FOXP3, PE-Cy7–conjugated anti-human CD25, and APC-conjugated anti-human CD127 (all from BD Biosciences, San Jose, CA). To stain for the FOXP3 intracellular marker, cells were first stained with the monoclonal antibodies against surface molecules, fixed and permeabilized (fix/perm solutions kit, BD Pharmingen, San Diego, CA), and then stained with anti-FOXP3 monoclonal antibody. Data were acquired using fluorescent-activated cell sorter (FACS)Canto System II (3 laser system, Becton Dickinson, Franklin Lakes, NJ) and analyzed by using the FACSDiva software (BD Biosciences). In parallel samples, intestinal cells were stained with PercP-Cy5–conjugated anti-human CD11c, Pacific Blue–conjugated anti-human CD4, APC-conjugated anti-human NKG2D, FITC-conjugated anti-human TCRδ1, and AmCyan-conjugated anti-human CD3 monoclonal antibodies to analyze various gut immune cell subsets. To measure expression of the CD103 marker on the various gut lymphocyte subsets, cells were simultaneously stained with Pacific Blue–conjugated anti-CD4, APC-Cy7–conjugated anti-CD8, AmCyan-conjugated anti-CD3, PE-Cy5–conjugated anti-CD11c, and PE-conjugated anti-CD103 (all from BD Biosciences).
Suppression assay.
Intestinal cells were isolated from the mucosa of duodenal fragments surgically removed from individuals affected by gastric carcinoma. PBMCs were collected from healthy blood donors. CD4+CD25+ Treg cells were isolated by magnetic sorting (Human CD4+CD25+ Regulatory T Cell Selection Kit, Miltenyi Biotec, Bergisch Gladbach, Germany). CFSE-stained CD4+CD25− T effector (Teff) cells (either from blood or intestinal cells) were cultured at 1:1 ratio with 105 intestinal or blood purified CD4+CD25+FoxP3+CD127− Treg cells and stimulated with coated anti-human CD3 (10 μg/mL) and soluble anti-CD28 (1 μg/mL; BD Biosciences) monoclonal antibodies in the presence of recombinant human interleukin (rhIL)-2 (50 units/mL; BD Biosciences) and irradiated PBMCs. Proliferation of Teff cells was measured by mean of CFSE dilution using FACS analysis over a culture period of 3 days.
Conversion assay.
LPDCs or blood monocyte–derived DCs (BMDCs) were obtained by culturing the adherent cell fraction (2 h adherence at 37°C 5% CO2) of total intestinal cells or PBMCs for 10 days in the presence of rhIL-4 (20 units/mL; Miltenyi Biotec) and recombinant human granulocyte-macrophage colony-stimulating factor (rhGM-CSF; 10 units/mL; Miltenyi Biotec). LPDCs were collected with 5 mmol/L EDTA/PBS, extensively washed with cold PBS, and stained with anti-PE-Cy5–conjugated anti-CD11c and PE-conjugated anti-CD103 monoclonal antibodies to assess their CD11c+CD103+ tolerogenic phenotype through FACS analysis. Next, 5 × 103 CD11c+CD103+ LPDCs or CD11c+CD103− BMDCs were cultured at 1:10 ratio (DC to T cells) with 5 × 104 autologous naive CD4+CD25− T cells isolated from PBMCs by magnetic selection (Human CD4+CD25+ Regulatory T Cell Selection Kit, Miltenyi Biotec). CD4+CD25− T cells were stimulated with soluble anti-human CD3 monoclonal antibody (1 μg/mL) in the presence of rhIL-2 (400 units/mL; BD Biosciences) and recombinant human transforming growth factor-β (rhTGF-β; 5 ng/mL; R&D Systems, Minneapolis, MN). After 4 days, cells were collected and stained with monoclonal antibodies anti-CD4-Pacific Blue, anti-CD25-PE-Cy7, anti-CD127-APC, and anti-FOXP3-Alexa Fluor-488 (after fixation and permeabilization), and the percentage of CD4+CD25+FoxP3+CD127− Treg cells obtained after stimulation with different DCs was measured by FACS analysis.
Statistical analysis.
Statistical differences were calculated with PRISM 4.0 software (GraphPad) using an unpaired, two-tailed t test. Differences between multiple groups were evaluated by ANOVA. Data were considered statistically significant when P values were < 0.05.
RESULTS
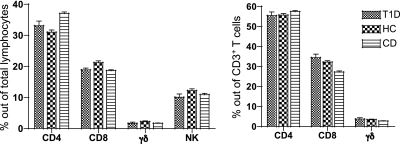
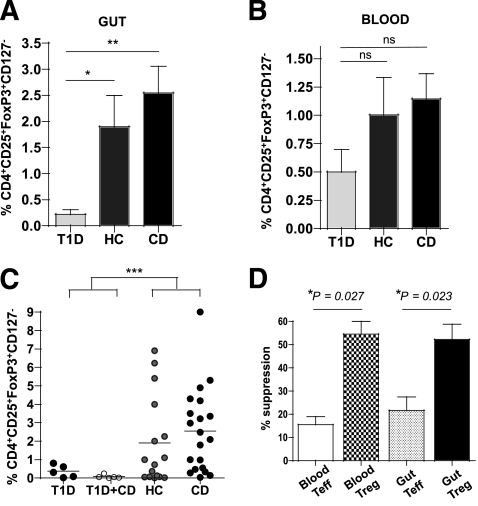
To test whether the gut environment impinges on human T1D by altering intestinal immune regulation, we analyzed the immune cell compartment in the small-intestinal mucosa and for comparison, peripheral blood of T1D patients, healthy control (HC) subjects, and individuals affected by celiac disease (CD). We obtained duodenal biopsies and blood samples from 46 individuals, including 10 patients with T1D, 16 HC subjects, and 20 individuals with CD. Age, sex, and clinical information for each group are summarized in Table 1. Our multiparametric FACS analysis showed that the percentages of various immune cell subsets, including CD4+ T cells, CD8+ T cells, NK cells, and γδ T cells, in the lamina propria of the intestinal mucosa were similar among the three groups (Fig. 1). Conversely, FACS analysis of CD4+CD25+FoxP3+CD127− Treg cells (Supplementary Fig. 1) revealed a significant reduction in the percentages of Treg cells out of total lymphocytes residing in the small-intestinal mucosa of T1D patients compared with HC subjects (P = 0.03) and individuals with CD (P = 0.003) (Fig. 2A). The difference between T1D patients and control groups was evident also when CD4+CD25+FoxP3+CD127− Treg cell percentages out of CD4+ T cells (rather than total lymphocytes), percentages of CD4+CD25+ Treg cells out of CD4+ T cells, and Treg/Teff cell ratio were considered (Supplementary Figs. 2 and 3). The quantitative defect observed in T1D patients regarded exclusively FoxP3+ Treg cells residing in the gut. In fact, the number of CD4+CD25+FoxP3+CD127− Treg cells in PBMCs of T1D patients was comparable to that of control subjects (P > 0.05) (Fig. 2B), in accordance with previous reports (21). Because a high percentage of T1D patients were also affected by CD (50%) (Supplementary Table 1), to exclude the possibility that the celiac condition influenced the percentage of CD4+CD25+FoxP3+CD127− Treg cells in the gut, we performed a multiple group comparison of Treg cell percentages among patients affected by T1D only, patients affected by T1D in association with CD, individuals with CD only, and HC subjects. As shown in Fig. 2C, the celiac condition did not significantly alter the percentages of CD4+CD25+FoxP3+CD127− Treg cells in the intestinal mucosa of both T1D and nondiabetic individuals, and the Treg cell deficiency was exclusively associated with the T1D condition (P < 0.001 with ANOVA). We also verified that the intestinal CD4+CD25+FoxP3+CD127− T cells that we enumerated were bona fide Treg cells by isolating CD4+CD25+ T cells (>70% FoxP3+CD127−) from normal surgical samples of small intestine (the number of Treg cells in bioptic material was not sufficient to perform such an experiment) and assessing their suppressive capacity upon proliferation of Teff cells (Fig. 2D).
TABLE 1.
Clinical data
| Cohort | n | Age (years) | Age | Sex (women/men) | T1D+CD | Early onset T1D | Long-lasting T1D |
|---|---|---|---|---|---|---|---|
| T1D | 10 | 3–58 | 29 ± 5.2 | 7/3 | 5 of 10 | 3 of 10 | 7 of 10 |
| Healthy | 16 | 2–68 | 11.6 ± 4 | 10/6 | NA | NA | NA |
| CD | 20 | 2–19 | 7.9 ± 1.2 | 15/5 | NA | NA | NA |
Data are means ± SD unless otherwise indicated. All patients (N = 46) underwent esophago-gastro-duodenal endoscopy for a clinical suspect of CD. The diagnosis of CD was made out of the histological examination of the intestinal mucosa and of the presence of antitissue transglutaminase antibodies (>95% of celiac individuals were tissue transglutaminase IgG and IgA positive). Hence, all the patients with CD were on a normal (not gluten-free) diet at the time of biopsy collection. HC subjects and patients affected only by T1D were all tissue transglutaminase IgG/IgA negative (100%). The mean age in the T1D group was higher than that of control individuals (healthy individuals and subjects with CD); however, we found no statistical correlation between age and the percentage of CD4+CD25+FoxP3+CD127− Treg cells in the gut mucosa (r2 = 0.05). Early onset T1D, <6 months from diagnosis; long-lasting T1D, ≥6 months from diagnosis. All samples analyzed were donated for research purposes and each individual signed an informed consent.
FIG. 1.
The relative percentages of total CD4+ T cells, CD8+ T cells, NK cells, and γδ T cells in the lamina propria of the small-intestinal mucosa were comparable in patients with T1D, HC subjects, and patients with CD. Lamina propria cells were isolated from the small-intestinal mucosa; simultaneously stained with Pacific Blue–conjugated anti-human CD4, APC-conjugated anti-human NKG2D, FITC-conjugated anti-human TCRδ1, and AmCyan-conjugated anti-human CD3 monoclonal antibodies; and FACS analyzed. Means of percentages ± SEM of CD4+ T cells (CD3+CD4+ cells), CD8+ T cells (CD3+CD8+ cells), γδ T cells (CD3+ TCRδ1+ cells), and NK cells (CD3− NKG2D+ cells) out of total lamina propria lymphocytes (left) and the means of percentages ± SEM of CD4+ T cells, CD8+ T cells, and γδ T cells out of CD3+ T cells (right) are indicated.
FIG. 2.
Selective reduction of FoxP3+ Treg cells in the gut of T1D patients. A: The percentages of CD4+CD25+FoxP3+CD127− Treg cells out of total lymphocytes were measured in single cell suspensions isolated from the small-intestinal mucosa (duodenal biopsies) of patients with T1D (n = 10), HC subjects (n = 16), and individuals with CD (n = 20). The CD4+CD25+FoxP3+CD127− Treg cells in gut mucosa were identified by multiparametric FACS analysis. Data are presented as means ± SEM of all experiments. *P = 0.03; **P = 0.003. B: Blood samples were collected from the same individuals simultaneously with the duodenal biopsy. PBMCs were isolated and analyzed as in A. Data are presented as means ± SEM of all experiments. NS, not significant; P > 0.05. C: The percentages of CD4+CD25+FoxP3+CD127− Treg cells were compared among patients with T1D (n = 5), patients with T1D and CD (T1D+CD, n = 5), HC subjects (n = 16), and patients with CD only (n = 20). Groups were compared using two-way ANOVA. ***P = 0.0001 (T1D vs. nondiabetic). D: Gut CD4+CD25+FoxP3+CD127− T cells were bona fide Treg cells and showed a suppressive capacity similar to that of their blood counterparts. A suppression assay was used to test 105 CD4+CD25+ Treg cells or CD4+CD25− Teff cells isolated from the mucosa of normal surgical samples of small intestine or PBMCs of HC subjects. Briefly, Treg or Teff cells were added at 1:1 ratio to responder CFSE-labeled CD4+CD25− T cells stimulated with plate-bound anti-CD3 monoclonal antibody, soluble anti-CD28 monoclonal antibody, and rhIL-2. The percentage of suppression was measured by the percent reduction of proliferation of responder Teff cells (measured by mean of CFSE dilution). Data are expressed as means ± SEM of four independent experiments.
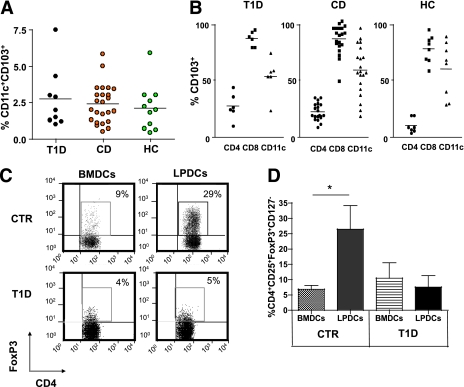
The reduced percentage of intestinal FoxP3+ Treg cells in T1D patients could be due to defective gut homing of naturally occurring FoxP3+ Treg cells that originate in the thymus. Alternatively, the quantitative defect of FoxP3+ Treg cells could be attributable to impaired de novo differentiation and/or expansion of FoxP3+ Treg cells in the intestinal mucosa and/or gut-associated lymphoid tissue of T1D patients. Small-intestinal LPDCs expressing the integrin αEβ7 (also called CD103) have the unique capacity to drive peripheral development and/or expansion (from precursors of thymic origin) of FoxP3+ Treg cells (18,19). Although few reports on human LPDCs exist, those studies show that human LPDCs express classical DC markers—such as CD11c, MHC class II, and CD83—as well as the typical marker of murine LPDCs, the CD103 molecule, and have some of their functional properties, such as ability to induce gut tropism on T cells (22) and FoxP3+ Treg cell differentiation (23). Hence, we specifically analyzed percentages and tolerogenic antigen-presenting function (i.e., capacity to induce FoxP3+ Treg cell differentiation/expansion) of CD103+CD11c+ LPDCs residing in the small-intestinal mucosa of T1D patients and control subjects. We did not detect any difference in the percentages of intestinal CD103+CD11c+ LPDCs (Fig. 3A) or in the percentages of LPDCs that expressed the CD103 marker (Fig. 3B) among the three groups of individuals. Next, we performed conversion assays to test the capacity of LPDCs of T1D patients to induce FoxP3+ Treg cell differentiation. Because of the limited amount of bioptic material, we could not sort CD103+CD11c+ LPDCs from total intestinal cells. Alternatively, we enriched the CD103+CD11c+ LPDCs from the small intestine of T1D patients and control subjects by culturing adherent intestinal cells with rhIL-4 and rhGM-CSF for 10 days and evaluated their ability to induce de novo differentiation of CD4+CD25+FoxP3+CD127− Treg cells (Supplementary Fig. 4A). Those in vitro–cultured DCs showed phenotypical features of CD11c+CD103+ DCs residing in the lamina propria (ex vivo LPDCs), such as expression of DC markers CD11c and CD103 and maturation markers (Supplementary Fig. 4B). As shown in Fig. 3C, human CD11c+CD103+ LPDCs from the intestinal mucosa of nondiabetic control subjects were able to convert CD4+CD25− T cells into CD4+CD25+FoxP3+CD127− Treg cells as previously demonstrated (23). Conversely, CD103+CD11c+ LPDCs from T1D patients completely lacked that function and failed to induce Treg cell differentiation/expansion (Fig. 3C). Interestingly, we found that the addition of TGF-β was necessary for human CD103+CD11c+ LPDCs to promote Treg cell conversion in control individuals (Supplementary Fig. 5). However, the addition of TGF-β to LPDCs of T1D patients was not capable of restoring the capacity to induce de novo generation and/or expansion of CD4+CD25+FoxP3+CD127− Treg cells (Fig. 3C and D). Our data represent the first evidence that the tolerogenic properties of CD11c+CD103+ DCs from the gut mucosa are impaired in T1D patients. However, because the CD103+ LPDC subset was enriched in vitro with a 10-day culture period with IL-4 and GM-CSF, we cannot exclude that the reduced tolerogenic properties of T1D LPDCs were related to their defective response to those cytokines.
FIG. 3.
CD103+CD11c+ LPDCs are present in the small intestine of T1D patients but fail to induce FoxP3+ Treg cell differentiation. A: Percentages of CD103+CD11c+ LPDCs in the gut mucosa of patients with T1D, HC subjects, and patients with CD. Cells were gated on the DC region (see Supplementary Fig. 4). B: Percentages of cells that express the gut receptor CD103 among various gut lymphocyte subsets (CD4+ T cells, CD8+ T cells, and CD11c+ DCs) in the three groups. C: The capacity of small-intestinal CD11c+CD103+ LPDCs of T1D patients and control subjects (healthy or celiac individuals [CTRs]) to induce CD4+CD25+FoxP3+CD127− Treg cell differentiation was evaluated in conversion assays. BMDCs or small-intestinal CD11c+CD103+ LPDCs were obtained from T1D patients and CTRs and added at 1:10 ratio (DC to T cells) to autologous naive CD4+CD25− T cells isolated from PBMC and stimulated with soluble anti-human CD3 monoclonal antibody in the presence of rhIL-2 and rhTGF-β. Cells were collected after 4 days and FACS analyzed to measure percentages of CD4+CD25+FoxP3+CD127− Treg cells. One representative experiment out of three (T1D) or four (CTR) is shown (cells gated on CD4+CD25+CD127− cells). D: Means ± SEM of CD4+CD25+FoxP3+CD127− Treg cell percentages obtained in conversion assays with BMDCs or LPDCs in three (T1D) or four (CTR) independent experiments are shown. *P = 0.028. (A high-quality color representation of this figure is available in the online issue.)
DISCUSSION
The identification and characterization of a specific defect of gut immune regulation in T1D patients could provide new insights in the current understanding of the disease pathogenesis. An immunological axis between the gastrointestinal tract and pancreatic tissues exists (20), so that gut T cells continuously travel from the intestinal mucosa to pancreatic lymph nodes and tissues as documented by their expression of gut-homing receptors such as α4β7 and CCR9 on self-reactive T cells in T1D patients (24) and T cells infiltrating pancreatic islets of NOD mice (25,26). The existence of an immunological gut–pancreas axis implies that the defective de novo generation of CD4+CD25+FoxP3+CD127− Treg cells in the intestinal mucosa of T1D patients may have a direct negative influence on the Teff/Treg cell balance in pancreatic lymph nodes and islets and, thus, ultimately may promote Teff cell responses against pancreatic self-antigens.
Further studies are necessary to dissect whether defective intestinal differentiation of FoxP3+ Treg cells by CD103+CD11c+ LPDCs in T1D patients is genetically determined or induced by environmental factors that alter the gut milieu, such as the intestinal microbiota. Recent studies demonstrate that the enteric commensal microbiota modulate gut immunity and represent a key epigenetic factor modifying T1D predisposition (9,27). It has been proposed that pathogenic microbiota promote T1D by activating self (islet)-reactive T cells in the gut (27). However, it is now clear that intestinal bacteria are crucial to controlling immune regulation and dampening T-cell immunity in the intestine, either directly or through interaction with intestinal epithelial cells (28). This raises the suggestive hypothesis that the microbiota, and possibly environmental factors such as diet and drugs that modify microbiota, impinge on T1D pathogenesis by altering tolerogenic DC function and impairing peripheral differentiation of CD4+CD25+FoxP3+CD127− Treg cells.
Supplementary Material
ACKNOWLEDGMENTS
This work was supported by Juvenile Diabetes Research Foundation grant 217-5-2008.
No potential conflicts of interest relevant to this article were reported.
E.B. and C.S. researched data. M.C. contributed to discussion and reviewed and edited the manuscript. V.U. researched data. L.M. and A.M.B. collected clinical data and samples. M.S. performed statistical analysis and reviewed and edited the manuscript. A.M. collected clinical data and samples. C.K. and E.B. contributed to discussion. M.F. designed the experiments, analyzed data, supervised the project, and wrote the manuscript.
The authors thank Maria Rescigno, Department of Experimental Oncology, European Institute of Oncology, Milan, Italy, and Silvia Gregori and Maria Grazia Roncarolo, San Raffaele Scientific Institute, Milan, Italy, for their helpful suggestions; Kevin Maloy, University of Oxford, Sir William Dunn School of Pathology, Oxford, U.K., and Manuela Battaglia, San Raffaele Scientific Institute, Milan, Italy, for critical reading of the manuscript; Dr. Graziano Borera and Dr. Riccardo Bonfanti, Pediatric Department, San Raffaele Hospital, Milan, Italy; and all the participants who kindly agreed to donate gut mucosa samples for research purposes.
Footnotes
This article contains Supplementary Data online at http://diabetes.diabetesjournals.org/lookup/suppl/doi:10.2337/db10-1201/-/DC1.
M.C. is currently affiliated with the Sir William Dunn School of Pathology, University of Oxford, Oxford, U.K.
REFERENCES
- 1.Ermann J, Fathman CG. Autoimmune diseases: genes, bugs and failed regulation. Nat Immunol 2001;2:759–761 [DOI] [PubMed] [Google Scholar]
- 2.Bach J-F. The effect of infections on susceptibility to autoimmune and allergic diseases. N Engl J Med 2002;347:911–920 [DOI] [PubMed] [Google Scholar]
- 3.Casu A, Pascutto C, Bernardinelli L, Songini M. Type 1 diabetes among Sardinian children is increasing: the Sardinian diabetes register for children aged 0-14 years (1989-1999). Diabetes Care 2004;27:1623–1629 [DOI] [PubMed] [Google Scholar]
- 4.Dotta F, Censini S, van Halteren AG, et al. Coxsackie B4 virus infection of beta cells and natural killer cell insulitis in recent-onset type 1 diabetic patients. Proc Natl Acad Sci USA 2007;104:5115–5120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Honeyman MC, Coulson BS, Stone NL, et al. Association between rotavirus infection and pancreatic islet autoimmunity in children at risk of developing type 1 diabetes. Diabetes 2000;49:1319–1324 [DOI] [PubMed] [Google Scholar]
- 6.Vaarala O, Knip M, Paronen J, et al. Cow’s milk formula feeding induces primary immunization to insulin in infants at genetic risk for type 1 diabetes. Diabetes 1999;48:1389–1394 [DOI] [PubMed] [Google Scholar]
- 7.Norris JM, Barriga K, Klingensmith G, et al. Timing of initial cereal exposure in infancy and risk of islet autoimmunity. JAMA 2003;290:1713–1720 [DOI] [PubMed] [Google Scholar]
- 8.Ziegler AG, Schmid S, Huber D, Hummel M, Bonifacio E. Early infant feeding and risk of developing type 1 diabetes-associated autoantibodies. JAMA 2003;290:1721–1728 [DOI] [PubMed] [Google Scholar]
- 9.Wen L, Ley RE, Volchkov PY, et al. Innate immunity and intestinal microbiota in the development of type 1 diabetes. Nature 2008;455:1109–1113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mooradian AD, Morley JE, Levine AS, Prigge WF, Gebhard RL. Abnormal intestinal permeability to sugars in diabetes mellitus. Diabetologia 1986;29:221–224 [DOI] [PubMed] [Google Scholar]
- 11.Meddings JB, Jarand J, Urbanski SJ, Hardin J, Gall DG. Increased gastrointestinal permeability is an early lesion in the spontaneously diabetic BB rat. Am J Physiol 1999;276:G951–G957 [DOI] [PubMed] [Google Scholar]
- 12.Westerholm-Ormio M, Vaarala O, Pihkala P, Ilonen J, Savilahti E. Immunologic activity in the small intestinal mucosa of pediatric patients with type 1 diabetes. Diabetes 2003;52:2287–2295 [DOI] [PubMed] [Google Scholar]
- 13.Graham S, Courtois P, Malaisse WJ, Rozing J, Scott FW, Mowat AM. Enteropathy precedes type 1 diabetes in the BB rat. Gut 2004;53:1437–1444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Secondulfo M, Iafusco D, Carratù R, et al. Ultrastructural mucosal alterations and increased intestinal permeability in non-celiac, type I diabetic patients. Dig Liver Dis 2004;36:35–45 [DOI] [PubMed] [Google Scholar]
- 15.Maurano F, Mazzarella G, Luongo D, et al. Small intestinal enteropathy in non-obese diabetic mice fed a diet containing wheat. Diabetologia 2005;48:931–937 [DOI] [PubMed] [Google Scholar]
- 16.Bosi E, Molteni L, Radaelli MG, et al. Increased intestinal permeability precedes clinical onset of type 1 diabetes. Diabetologia 2006;49:2824–2827 [DOI] [PubMed] [Google Scholar]
- 17.Wing K, Sakaguchi S. Regulatory T cells exert checks and balances on self tolerance and autoimmunity. Nat Immunol 2010;11:7–13 [DOI] [PubMed] [Google Scholar]
- 18.Coombes JL, Siddiqui KR, Arancibia-Cárcamo CV, et al. A functionally specialized population of mucosal CD103+ DCs induces Foxp3+ regulatory T cells via a TGF-β and retinoic acid-dependent mechanism. J Exp Med 2007;204:1757–1764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sun CM, Hall JA, Blank RB, et al. Small intestine lamina propria dendritic cells promote de novo generation of Foxp3 T reg cells via retinoic acid. J Exp Med 2007;204:1775–1785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Turley SJ, Lee JW, Dutton-Swain N, Mathis D, Benoist C. Endocrine self and gut non-self intersect in the pancreatic lymph nodes. Proc Natl Acad Sci USA 2005;102:17729–17733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brusko T, Wasserfall C, McGrail K, et al. No alterations in the frequency of FOXP3+ regulatory T-cells in type 1 diabetes. Diabetes 2007;56:604–612 [DOI] [PubMed] [Google Scholar]
- 22.Jaensson E, Uronen-Hansson H, Pabst O, et al. Small intestinal CD103+ dendritic cells display unique functional properties that are conserved between mice and humans. J Exp Med 2008;205:2139–2149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Iliev ID, Spadoni I, Mileti E, et al. Human intestinal epithelial cells promote the differentiation of tolerogenic dendritic cells. Gut 2009;58:1481–1489 [DOI] [PubMed] [Google Scholar]
- 24.Paronen J, Klemetti P, Kantele JM, et al. Glutamate decarboxylase-reactive peripheral blood lymphocytes from patients with IDDM express gut-specific homing receptor alpha4beta7-integrin. Diabetes 1997;46:583–588 [DOI] [PubMed] [Google Scholar]
- 25.Hänninen A, Salmi M, Simell O, Jalkanen S. Mucosa-associated (beta 7-integrinhigh) lymphocytes accumulate early in the pancreas of NOD mice and show aberrant recirculation behavior. Diabetes 1996;45:1173–1180 [DOI] [PubMed] [Google Scholar]
- 26.McGuire HM, Vogelzang A, Ma CS, et al. A subset of interleukin-21(+) chemokine receptor CCR9(+) T helper cells target accessory organs of the digestive system in autoimmunity. Immunity 2011;34:602–615 [DOI] [PubMed] [Google Scholar]
- 27.Vaarala O, Atkinson MA, Neu J. The “perfect storm” for type 1 diabetes: the complex interplay between intestinal microbiota, gut permeability, and mucosal immunity. Diabetes 2008;57:2555–2562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Artis D. Epithelial-cell recognition of commensal bacteria and maintenance of immune homeostasis in the gut. Nat Rev Immunol 2008;8:411–420 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.