Epidemiological studies indicate that use of third generation oral contraceptives increases the risk of venous thromboembolism more than does use of second generation oral contraceptives.1−3 Critics have suggested that this finding may be confounded by indication, since third generation pills were considered to be safer and were therefore perhaps prescribed more often to women at high risk. If confounding by indication is the only explanation for the observed association, the incidence of venous thromboembolism in the population should not have changed when prescribing patterns changed from second generation to third generation pills with no increase in overall use of oral contraceptives. Vandenbroucke et al and Thomas reported increasing mortality from venous thromboembolism among young women in the Netherlands and in England and Wales from the mid-1980s to the 1990s, when the use of third generation pills was increasing.4,5 Since mortality from venous thromboembolism depends on both aetiological and prognostic factors, however, it may be more appropriate to look at incidence.
In Denmark, roughly a quarter of women aged 15-44 used oral contraceptives during the 1980s and the beginning of the 1990s. The first third generation oral contraceptive, containing desogestrel, was released in 1984, and the third generation preparations containing gestodene and norgestimate were introduced in 1988 and 1990, respectively. Use of third generation pills represented 0.2% of the total use of oral contraceptives in 1984, 17% in 1988, 40% in 1990, and 66% in 1993.
Subjects, methods, and results
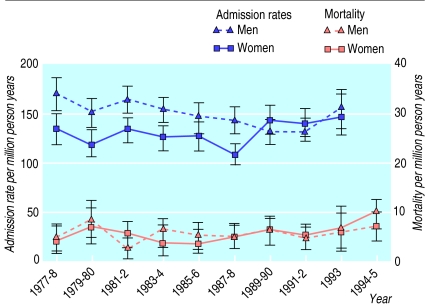
We used admission rates for venous thromboembolism in Denmark as a proxy measure of the incidence of this condition. For people aged 15-49 all admissions during 1977-93 with a registration of pulmonary embolism (ICD-8 (international classification of diseases, 8th revision) code 450.9), deep venous thrombosis (ICD-8 code 451), and other embolic or thrombotic disorders (ICD-8 code 453) were obtained from the Danish National Registry of Patients. Patients were excluded if they had cancer before the venous thromboembolism, surgery within the six months before the venous thromboembolism, or a pregnancy or obstetric diagnosis in the nine months before or three months after the venous thromboembolism or if venous thromboembolism was recorded as a supplemental diagnosis. Multiple admissions for venous embolism for a given person were counted in the numerator of the admission rates provided that the admissions were separated by at least three months. Death rates were calculated from the death certificate file, with no exclusions; during 1994-5 these rates were based on ICD-10 (codes I26, I80, I82). All rates were standardised to the world standard population. Admission rates for primary venous thromboembolism among women fluctuated around 120 per million person years during 1977-88 but increased to about 140 per million person years during 1989-93 (figure). For men the admission rates remained stable throughout the period, at a rate similar to that for women in recent years. The mortality curves for men and women followed largely the same course throughout the period. For women the admission rates were based on a total of 2883 discharges with venous thromboembolism during 1977-93, while the death rates were based on only 120 deaths from venous thromboembolism in the same years.
Comment
The increase in admission rates for venous thromboembolisrn among women seems to correlate with the increase in use of third generation oral contraceptives. The increase is not likely to be explained by changes in diagnostic procedures or in the threshold for admission since no increase was seen for men.
These data support the hypothesis that third generation oral contraceptives increase the risk of venous thromboembolism to a greater extent than other oral contraceptives, and the result cannot be explained by confounding by indication. Our result must, however, be interpreted with caution: the numbers are small, and it is based on data that are subject to misclassification.
Figure.
Admission rates and mortality from venous thromboembolism per million person years for men and women aged 15-49, by calendar year. Rates standardised to world standard population; bars show 95% confidence intervals
Acknowledgments
We thank Andrea Bautz at the Institute of Cancer Epidemiology, Danish Cancer Society, for programming support.
Footnotes
Funding: The study was supported by the Danish Medical Research Council (grant No 9700677). The activities at the Institute of Cancer Epidemiology are financed by the Danish Cancer Society, while the activities at the Danish Epidemiology Science Centre are financed by a grant from the Danish National Research Foundation.
Competing interests: None declared.
References
- 1.World Health Organisation Collaborative Study of Cardiovascular Disease and Steroid Hormone Contraception. Venous thromboembolic disease and combined oral contraceptives: results of international multicentre case-control study. Lancet. 1995;346:1575–1582. [PubMed] [Google Scholar]
- 2.Jick H, Jick S, Gurewich V, Myers M, Vasilakis C. Risk of idiopathic cardiovascular death and nonfatal venous thromboembolism in women using oral contraceptives with differing progestogen components. Lancet. 1995;346:1589–1593. doi: 10.1016/s0140-6736(95)91928-7. [DOI] [PubMed] [Google Scholar]
- 3.Spitzer W, Lewis M, Heinemann L, Thorogood M, MacRae K. Third generation oral contraceptives and risk of venous thromboembolic disorders: an international case-control study. BMJ. 1996;312:83–88. doi: 10.1136/bmj.312.7023.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vandenbroucke J, Bloemenkamp K, Helmerhorst F, Rosendaal F. Mortality from venous thromboembolism and myocardial infarction in young women in the Netherlands. Lancet. 1996;348:401–402. doi: 10.1016/s0140-6736(96)24032-2. [DOI] [PubMed] [Google Scholar]
- 5.Thomas S. Mortality from venous thromboembolism and myocardial infarction in young adults in England and Wales. Lancet. 1996;348:402. doi: 10.1016/s0140-6736(05)65016-7. [DOI] [PubMed] [Google Scholar]