Abstract
Background
Intercellular communication can occur via the release of membrane vesicles. Exosomes are nanovesicles released from the endosomal compartment of cells. Depending on their cell of origin and their cargo they can exert different immunoregulatory functions. Recently, fungi were found to produce extracellular vesicles that can influence host-microbe interactions. The yeast Malassezia sympodialis which belongs to our normal cutaneous microbial flora elicits specific IgE- and T-cell reactivity in approximately 50% of adult patients with atopic eczema (AE). Whether exosomes or other vesicles contribute to the inflammation has not yet been investigated.
Objective
To investigate if M. sympodialis can release nanovesicles and whether they or endogenous exosomes can activate PBMC from AE patients sensitized to M. sympodialis.
Methods
Extracellular nanovesicles isolated from M. sympodialis, co-cultures of M. sympodialis and dendritic cells, and from plasma of patients with AE and healthy controls (HC) were characterised using flow cytometry, sucrose gradient centrifugation, Western blot and electron microscopy. Their ability to stimulate IL-4 and TNF-alpha responses in autologous CD14, CD34 depleted PBMC was determined using ELISPOT and ELISA, respectively.
Results
We show for the first time that M. sympodialis releases extracellular vesicles carrying allergen. These vesicles can induce IL-4 and TNF-α responses with a significantly higher IL-4 production in patients compared to HC. Exosomes from dendritic cell and M. sympodialis co-cultures induced IL-4 and TNF-α responses in autologous CD14, CD34 depleted PBMC of AE patients and HC while plasma exosomes induced TNF-α but not IL-4 in undepleted PBMC.
Conclusions
Extracellular vesicles from M. sympodialis, dendritic cells and plasma can contribute to cytokine responses in CD14, CD34 depleted and undepleted PBMC of AE patients and HC. These novel observations have implications for understanding host-microbe interactions in the pathogenesis of AE.
Introduction
Exosomes are nanovesicles (30–100 nm) of endosomal origin produced by different cells [1], [2], [3]. They can be secreted into the extracellular space and act as means of intercellular communication by transferring functional proteins and RNA molecules between cells [4], [5]. They can also carry antigens from microorganisms such as viruses and bacteria [6], [7]. Exosomes can be isolated from body fluids such as plasma [8], bronchoalveolar lavage (BAL) fluid [9], breast milk [10] and urine [11]. Previous studies have found that B-cells and dendritic cells (DC) release MHC class II containing exosomes which could activate immune responses in vitro and in vivo [12], [13]. Due to their immunostimulatory capacity, exosomes from antigen presenting dendritic cells (APC) are currently being tested as vaccine vehicles in cancer [14], [15], [16], [17] and against infections [18], [19]. However, it is still unclear which role exosomes have in vivo and during human inflammatory diseases. Only one previous study has investigated the immunostimulatory effects of exosomes from cells of patients with allergy. Here, B-cell exosomes directly loaded with birch pollen allergen could induce Th2-cytokine responses in PBMC of sensitised patients [20].
Atopic eczema (AE) is a common chronic inflammatory skin disease. While the pathogenesis of the disease remains unclear, studies suggest that a genetic predisposition in combination with defects in the skin barrier facilitate the development of AE [21], [22]. A defective skin barrier in turn might assist the entry of microorganisms which can trigger symptoms by acting as allergens. One such microorganism is the lipophilic yeast M. sympodialis, which belongs to our common cutaneous microbial flora [23]. 30–80% of adult AE patients are reactive to M. sympodialis in terms of specific IgE- and T-cell reactivity and/or positive atopy patch test (APT) reactions indicating a link between AE and M. sympodialis [24]. Sensitization to M. sympodialis is most likely mediated by APC such as DC in the skin. We have previously found that human monocyte-derived dendritic cells (MDDC) rapidly internalize M. sympodialis [25] and in response upregulate the maturation marker CD83 and the co-stimulatory molecules CD80 and CD86 [26]. Furthermore M. sympodialis induces lymphocyte proliferation and a Th2-like immune response in sensitized AE patients [27].
Recently, the release of extracellular vesicles has been described for the fungi Cryptococcus neoformans, Histoplasma capsulatum and Saccharomyces cerevisiae [28], [29]. It is speculated that these vesicles function in enzymatic nutrient degradation and in host-microbe interactions [30], e.g. by modulating murine macrophage functions in vitro [31].
In this study we hypothesised that M. sympodialis releases nanovesicles with immune modulating functions. We compared their capacity to induce cytokine responses in autologous PBMC of AE patients and healthy controls (HC) with that of exosomes derived from MDDC co-cultured with M. sympodialis or isolated from plasma. We demonstrate for the first time that M. sympodialis releases extracellular vesicles (MalaEx) carrying allergen. These vesicles induced IL-4 and TNF-α responses in PBMC with a significantly higher IL-4 production in the patients compared to the controls. Furthermore, we report that exosomes from MDDC co-cultured with M. sympodialis (DCexo Mala) elicit IL-4 and TNF-α responses whereas plasma exosomes induced TNF-α but not IL-4 production in AE patients and HC. These novel findings suggest that nanovesicles, autologous or derived from fungi, serve diverse immunoregulatory functions which might contribute to the inflammation in AE.
Methods
Ethics Statement
The study was approved by the Regional Ethical Review Board in Stockholm and all participants gave their written informed consent.
AE patients and healthy controls
Male AE patients and HC (Table 1) were recruited from the Stockholm area using the same inclusion and exclusion criteria as described previously [32] (see Online Repository S1). Patients and controls were asked to come back for a full blood donation of 450 ml for generation of MDDC, storage of plasma at −80°C and of PBMC at −150°C. The blood donations and following experiments were performed pairwise with one AE patient and one HC. Twelve additional healthy blood donors were included from the Karolinska University Hospital Solna Blood Bank.
Table 1. Characterisation of study subjects.
| Individual | Age(years) | SubjectiveSCORAD1) | Plasma IgE(kU/L)2) | Phadiatop®,3) | M.sympodialis specificIgE (kU/L)4) |
| HC*1 | 25 | - | 22 | Neg | <0.35 |
| HC 2 | 57 | - | 6.5 | Neg | <0.35 |
| HC 3 | 63 | - | 8.7 | Neg | <0.35 |
| HC 4 | 25 | - | 11 | Neg | <0.35 |
| HC 5 | 22 | - | 14 | Neg | <0.35 |
| HC 6 | 43 | - | 6.9 | Neg | <0.35 |
| HC 7 | 41 | - | 8.5 | Neg | <0.35 |
| HC 8 | 24 | - | 35 | Neg | <0.35 |
| Median (range) | 33 (22–63) | 9.9 (6.5–35) | <0.35 | ||
| AE†1 | 25 | 65 | 140 | Pos | 0.83 |
| AE 2 | 20 | 68 | 1600 | Pos | 25 |
| AE 3 | 39 | 76 | 11000 | Pos | 27 |
| AE 4 | 57 | 42 | 1400 | Pos | 21 |
| AE 5 | 51 | 48 | 2200 | Pos | 29 |
| AE 6 | 31 | 73 | 680 | Pos | 11 |
| AE 7 | 21 | 62 | 120 | Pos | 1.6 |
| AE 8 | 33 | 51 | 36 | Pos | 2.3 |
| Median (range) | 32 (20–57) | 63.5 (42–76) | 1040 (36–11000) | 16 (1.6–29) |
HC = Healthy control.
AE = Atopic eczema patient.
SCORAD = Severity scoring of atopic eczema [48].
ImmunoCAP™ (Phadia AB), reference range 1.6–122 kU/L.
A positive Phadiatop® (Phadia AB) was defined as having plasma IgE to any of 11 common aeroallergens ≥0.35 kU/L.
Specific plasma IgE to M. sympodialis analysed with ImmunoCAP™ (m70 Phadia AB).
All values (except SCORAD) were determined at the time of blood donation (AE 3 and 4 donated blood twice; values of the first donation are displayed).
Generation of monocyte derived dendritic cells (MDDC)
MDDC were generated as previously described [33] with some modifications. PBMC were depleted of CD34+ cells and CD14+ monocytes by magnetic bead separation (Miltenyi Biotech, Bergisch Gladbach, Germany) and the remaining cells were frozen (CD14, CD34 depleted PBMC). CD14+ monocytes were cultured for 6 days in exosome-free medium [34] supplied with 1 ng/ml IL-4 (Biosource International, Camarillo, CA) and 10 ng/ml GM-CSF (Invitrogen/GIBCO, Paisley, UK) for differentiation into MDDC. On day 6, cells were phenotyped by flow cytometry (see below). The cells showed a typical phenotype of immature MDDC as previously described [35] without any significant differences between AE patients and HC (see Online Repository S1).
Culture of M. sympodialis
M. sympodialis (ATCC strain 42132) was cultured on modified Dixon agar plates [26] for 4 days at 32°C and contamination was excluded using blood and Sab-oxoid agar plates. Colonies were harvested and resuspended in RPMI-1640 (Hyclone, Logan, UT). The cells were washed once and counted by the trypan blue exclusion method. Supernatants from M. sympodialis cultured at a concentration of 2×106 cells/ml for 48 hr at 37°C in exosome-free medium [34] were stored at −80°C for later nanovesicle preparation.
Co-culture of MDDC with M. sympodialis
Immature MDDC were cultured with or without live M. sympodialis. After 48 hr, culture supernatants were harvested and kept at −80°C until exosome preparation and cells were phenotyped using flow cytometry (see below and Online Repository S1).
Flow cytometric analysis of cells
MDDC were phenotyped before and after culture with M. sympodialis using flow cytometry and fluorescein-isothiocyanate (FITC)- or phycoerythrin (PE)-labelled mouse monoclonal antibodies (mAbs) using a FACS Calibur or FACS Aria (BDBiosciences, Bedford, MA) (see Online Repository S1).
Nanovesicle preparations
Nanovesicles from M. sympodialis culture supernatants, the different MDDC culture supernatants and from plasma were prepared by serial ultracentrifugation as described previously [8], [35] with slight modifications (see Online Repository S1). Pellets were resuspended in PBS or RPMI, and protein content was measured using a Bradford assay (BioRad, Hercules, CA) (Table S1). Nanovesicle preparations were stored at −80°C.
Characterisation of nanovesicles
Exosomes were phenotyped on anti-MHC class II coated Dynabeads (Invitrogen/Dynal, Paisley, UK) using mAbs and a FACS Calibur (BDBiosciences) [20]. To verify the presence of phenotypic cell markers or M. sympodialis antigens on vesicles, sucrose gradient analysis was performed as previously described [10] using uncoated latex beads (Invitrogen) or anti-MHC class II Dynabeads (Invitrogen/Dynal) (see Online Repository S1).
Negative staining (TEM)
Three µL drops of DCexo, DCexo Mala or MalaEx samples were added to carbon coated formvar grids for 10 min. The excess solution was removed by a filter paper and grids were directly stained by 2% uranyl acetate for 10 sec followed by a quick rinsing in distilled water. Grids were analyzed in a Tecnai 12 transmission electron microscope (FEI company, Eindhoven, The Netherlands) and images were taken by a Veleta digital camera (Olympus Soft Imaging Solutions, GmbH, Münster, Germany).
Immuno-negative staining (iEM)
DCexo, DCexo Mala or MalaEx coated grids were blocked from unspecific binding by floating grids face down on drops of 10% normal goat serum (NGS) in 0.1 M phosphate buffer (PB) for 10 min followed by incubation with a mAb against HLA-DR (BD Biosciences) or a purified rabbit anti-M. sympodialis Ab (generated in house) for 2 hr. As controls, the primary antibodies were replaced by IgG2a (BDBiosciences) and normal rabbit IgG from non-immunized mice (DAKO Cytomation, Glostrup, Denmark). Grids were washed several times in phosphate buffer containing 0.1% NGS and bound antibodies were detected by secondary gold-particle conjugated goat anti-rabbit (10 nm) and anti-mouse (5 nm) (Biocell, BBInternational, Cardiff, England). Grids were stained and analyzed as described above.
ELISPOT and ELISA analyses
CD14, CD34 depleted PBMC were cultured alone, or with nanovesicles from M. sympodialis, or with exosomes from MDDC cultured alone, or co-cultured with M. sympodialis at different concentrations while PBMC were cultured with plasma exosomes in the absence or presence of M. sympodialis. IL-4 ELISPOT assays were performed in triplicates for 48 hr according to the manufacturer's instructions (Mabtech, Stockholm, Sweden) and analysed by an ELISPOT automated reader (AID Diagnostika, Straßberg, Germany) (see Online Repository S1). ELISPOT supernatants were harvested and analysed for TNF-α using ELISA according to the manufacturer's instructions (Mabtech). The detection limit was 8 pg/ml. Results are expressed as the mean of triplicates.
Western Blot
The pelleted sucrose gradient fractions from M. sympodialis extracellular vesicles were denatured in Laemmli sample buffer (BioRad), separated on SDS polyacrylamide gels (BioRad) and the separated proteins were transferred to polyvinylidene difluoride membrane (Millipore) using a semi dry blotting system (BioRad). M. sympodialis specific bands were detected by using polyclonal rabbit IgG raised against M. sympodialis extract (generated in house) in 1∶2000 dilution, or serum from a patient with AE, sensitized to M. sympodialis (M. sympodialis specific IgE (m70, Phadia AB) 39 kU/L, total serum IgE 1700 kU/L) in a 1∶5 dilution. Serum from HC no 6 (Table 1) was used as negative control. Antibodies used for detection were rabbit anti-human IgE (1∶2000, MIAB Antibodies, Uppsala, Sweden) and horseradish peroxidase (HRP)-linked goat anti-rabbit IgG (1∶2000, Cell Signaling, Danvers, MA). Membranes were developed using the enhanced chemiluminescence (ECL) advanced detection kit (GE Healthcare).
Statistical analysis
Nonparametric tests were performed using Graphpad Prism version 5 for Windows (Graphpad Software Inc., San Diego, CA, USA, www.graphpad.com). Wilcoxon matched pairs test was used within one group, and unpaired Mann-Whitney test between groups. A p-value<0.05 was considered statistically significant.
Results
M. sympodialis secretes extracellular vesicles which elicit IL-4 and TNF-α responses
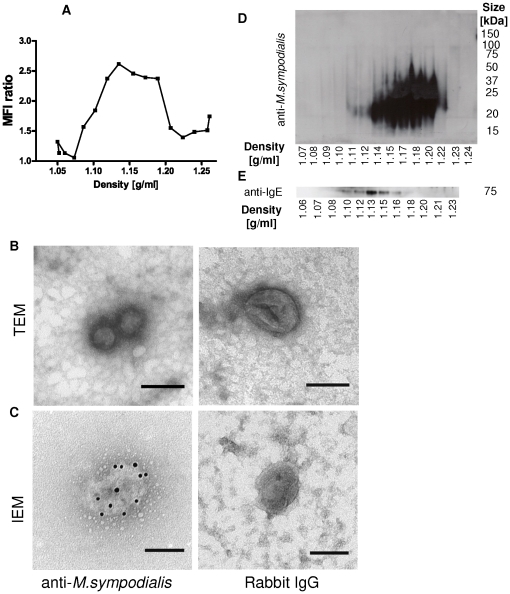
We first cultured M. sympodialis alone to test whether the yeast releases extracellular vesicles. Sucrose gradient fractions of pelleted culture supernatants revealed the presence of M. sympodialis derived antigens in density fractions ranging from 1.10 to 1.20 g/ml using flow cytometry (Fig. 1A). TEM analysis of these fractions showed the presence of vesicular structures with a size between 50–200 nm, with an average of approximately 100 nm (Fig. 1B). When performing iEM we could locate M. sympodialis antigens on these vesicular structures while controls showed negligible and unspecific labelling (Fig. 1C). Western blot analysis of the sucrose gradient fractions using polyclonal rabbit IgG raised against M. sympodialis showed the presence of antigens in vesicle fractions ranging in density from 1.12 g/ml to 1.22 g/ml (Fig. 1D) and 1.10–1.21 g/ml in two independent experiments, respectively. We then continued to look for IgE-binding epitopes using a separate sucrose gradient. When using serum from an AE patient containing specific IgE against M. sympodialis we could detect an IgE-binding protein with a size of approximately 70 kDa in fractions ranging in density between 1.10–1.18 g/ml (Fig. 1E) in two independent experiments. No bands were detected when using serum of HC no 6 (Table 1, data not shown). Thus, M. sympodialis can produce nanovesicles which contain antigens and among those also allergen.
Figure 1. M. sympodialis releases extracellular vesicles.
(A) M. sympodialis culture supernatants were ultracentrifuged and sucrose gradient fractions coated onto latex beads and analysed for the presence of M. sympodialis epitopes using flow cytometry. Data is from one representative out of 6 independent experiments and displayed as mean MFI ratio of a rabbit antibody against M. sympodialis and unspecific rabbit IgG. Fractions ranging in density from 1.11–1.20 g/ml were pooled and analysed by (B) TEM and (C) IEM with the same antibody as in A. Scale bars correspond to 100 nm. Pictures are representative in (B) of 4 independent experiments and in (C) of two independent experiments. (D) Western blot analysis of sucrose gradient fractions analysed using a rabbit antibody against M. sympodialis and (E) using serum from an AE patient sensitized to M. sympodialis to detect IgE-binding epitopes. Data shown in (D) and (E) are from one out of 2 experiments using separate sucrose gradients.
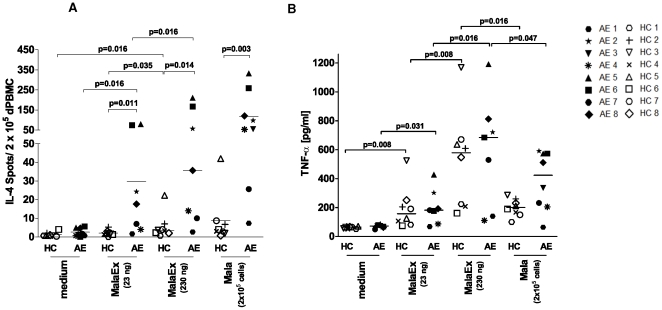
Next we assessed the effect of M. sympodialis vesicles, designated MalaEx, on CD14, CD34 depleted PBMC from AE patients and HC in an IL-4 ELISPOT assay for 48 hr. MalaEx significantly enhanced IL-4 production in CD14, CD34 depleted PBMC compared to the medium control in a dose dependent manner (Fig. 2A). The IL-4 responses were significantly higher in AE patients compared to HC both for MalaEx and for whole M. sympodialis cells (Mala) used as a control. MalaEx also induced a dose dependent TNF-α response in both AE patients and HC but without any significant differences between the two groups (Fig. 2B). These data indicate that M. sympodialis derived vesicles can elicit cytokine responses and that there is a difference in IL-4 reponse to MalaEx between HC and AE patients.
Figure 2. MalaEx elicit IL-4 and TNF-α responses.
(A) IL-4 production in CD14, CD34 depleted PBMC as measured by ELISPOT from HC and AE patients when cultured alone (medium) or with MalaEx or M. sympodialis (Mala) for 48 hr. (B) TNF-α levels in the IL-4 ELISPOT supernatants were measured by ELISA. Data represent mean values of triplicates for each individual (Table 1); lines indicate median.
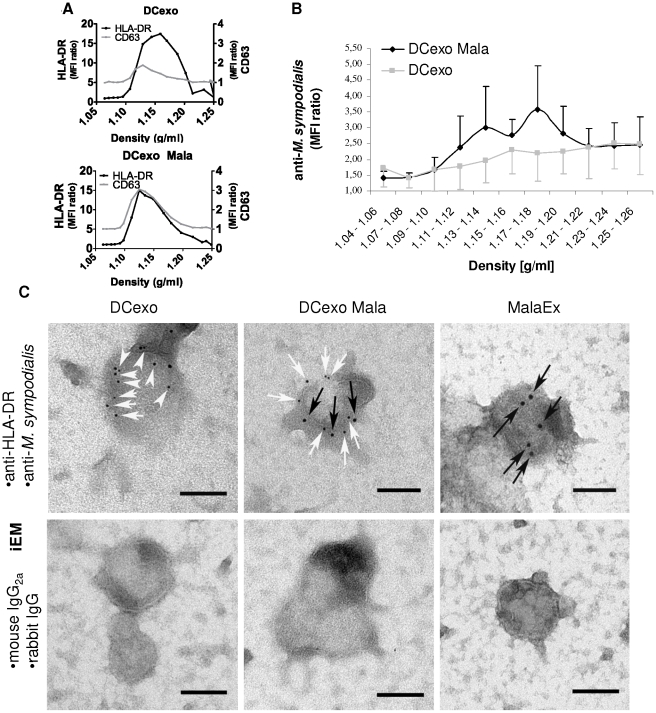
Exosomes from MDDC and M. sympodialis co-cultures contain M. sympodialis antigens
Since DCs are among the first cells to encounter M. sympodialis in the skin, we prepared vesicles from MDDC and M. sympodialis co-cultures (DCexo Mala) and from MDDC alone (DCexo) to investigate the possible presence of M. sympodialis antigens on endogenous exosomes.
In agreement with a previous study, M. sympodialis induced maturation of MDDC, with a significant upregulation of CD80, CD83 and CD86 on MDDC [26], with no significant differences between AE patients and HC (Figure S1). M. sympodialis did not induce significant differences in the other molecules investigated (HLA-ABC, HLA-DR, CD11c, CD14, CD40, CD54 and CD63) compared to the medium control (data not shown).
Flow cytometry analysis of sucrose gradient fractionated vesicles revealed the presence of HLA-DR and the tetraspanin CD63 in DCexo and DCexo Mala in fractions corresponding to exosomes (density 1.11–1.20 g/ml, [12], Fig. 3A). We could also detect M. sympodialis epitopes in sucrose gradient fractions of DCexo Mala ranging in density from 1.11–1.20 g/ml using flow cytometry, but not in the corresponding fractions of DCexo (Fig. 3B). Double iEM with a mAb to HLA-DR and a rabbit antibody to M. sympodialis revealed the presence of double positive vesicles in DCexo Mala preparations while the majority of the DCexo only bound the anti-HLA-DR antibody. Vesicles in MalaEx preparations only bound the antibody against M. sympodialis while isotype IgG controls showed negligible labelling (Fig. 3C).
Figure 3. DCexo Mala contain M. sympodialis antigens.
(A) Sucrose gradient fractions of exosomes from MDDC cultured alone (DCexo) or with M. sympodialis (DCexo Mala) were analysed for the expression of HLA-DR and CD63 using flow cytometry. Data are representative for one out of 3 experiments each using a pool of exosomes from 2 healthy blood donors and displayed as MFI ratio between specific antibody and isotype control. (B) Sucrose gradient fractions of DCexo and DCexo Mala analysed using flow cytometry. Data are from 5 independent experiments and displayed as mean MFI ratio ± SEM between a rabbit antibody against M. sympodialis and unspecific rabbit IgG. (C) Double IEM was performed on pools of DCexo and DCexo Mala from 5 AE patients and 3 HC as well as 2 independent preparations of MalaEx using a mAb against HLA-DR (detected with a 5 nm gold-particle conjugated goat anti-mouse Ab, white arrows) and a rabbit antibody against M. sympodialis (detected with a 10 nm gold-particle conjugated goat anti-rabbit Ab, black arrows) and the corresponding isotype controls. Scale bars correspond to 100 nm.
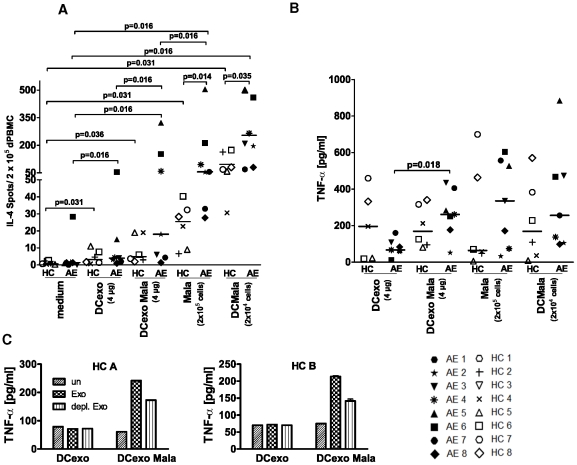
Exosomes from MDDC and M. sympodialis co-cultures induce IL-4 and TNF-α responses
To test whether endogenous nanovesicles have similar effects on cytokine responses as exogenous MalaEx, we added DCexo Mala in an IL-4 ELISPOT assay. We found that DCexo Mala induced significantly higher IL-4 responses than DCexo in autologous CD14, CD34 depleted PBMC from AE patients but not in CD14, CD34 depleted PBMC from HC (Fig. 4A). IL-4 responses were highest in response to M. sympodialis whole cells (Mala) and MDDC co-cultured with M. sympodialis (DCMala) with a statistically significant induction of IL-4 also in the HC group compared to the medium control (Fig. 4A). However, the levels were significantly lower than those observed in the AE patients. The TNF-α levels were significantly increased when stimulating CD14, CD34 depleted PBMC with DCexo Mala compared to DCexo in AE patients (Fig. 4B). A similar trend was seen for HC (Fig. 4B, C).
Figure 4. DCexo Mala elicit IL-4 and TNF-α responses.
(A) IL-4 production in autologous CD14, CD34 depleted PBMC from AE patients and HC as measured by ELISPOT when cultured alone (medium), with DCexo, DCexo Mala, M. sympodialis (Mala) or MDDC co-cultured with M. sympodialis (DCMala) for 48 hr. (B) TNF-α levels in the IL-4 ELISPOT supernatants were measured by ELISA. Data represent mean values of triplicates for each individual (Table 1); lines indicate median. (C) TNF-α levels in supernatants of CD14, CD34 depleted PBMC of two additional healthy blood donors (HC A and HC B) when cultured alone (un), with DCexo or DCexo Mala (Exo) or with DCexo and DCexo Mala that were depleted of MHC class II positive vesicles (depl. Exo). Bars indicate mean value of duplicates.
To investigate whether TNF-α induction indeed was due to DC-derived vesicles, exosome preparations from two additional healthy blood donors were depleted of MHC class II containing vesicles using anti-MHC class II Dynabeads. The DCexo Mala induced TNF-α levels were decreased by 38% (donor A) or 52% (donor B) after depletion (Fig. 4C), indicating that responses were at least in part due to DC-derived exosomes from the co-cultures.
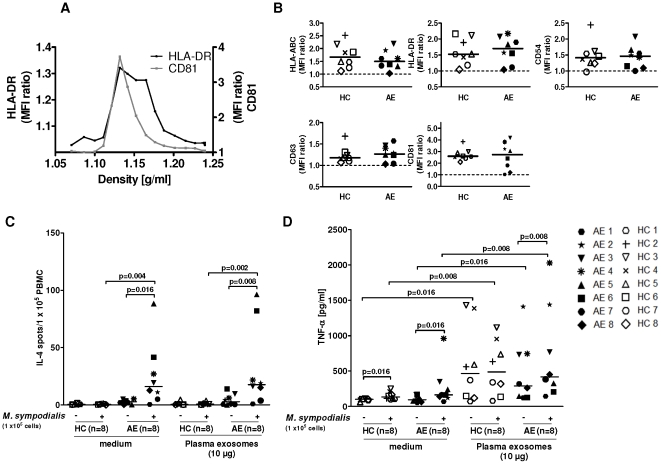
Plasma exosomes elicit TNF-α but not IL-4 in autologous PBMC
Finally we prepared nanovesicles from plasma to find out whether their phenotype or function differed between AE patients and HC. Sucrose gradient analysis of plasma exosomes revealed the presence of CD81 and HLA-DR in density fractions ranging from 1.10 to 1.18 g/ml (Fig. 5A). Phenotypic analysis showed the presence of HLA-ABC, HLA-DR, CD54, CD63, and CD81 on plasma exosomes without any significant differences between AE patients and HC (Fig. 5B) while neither CD3, CD19, CD86, FasL, the B-cell activating factor of the TNF-family (BAFF) nor TGFβ1 could be detected on plasma exosomes (data not shown).
Figure 5. Plasma exosomes elicit TNF-α but not IL-4 responses.
(A) Sucrose gradient fractions of plasma exosomes pooled from 2 healthy blood donors were loaded onto anti-MHC class II Dynabeads and analysed for the presence of HLA-DR and CD81 using flow cytometry. MFI ratio was calculated by dividing the sample MFI by the isotype control MFI. Data are from one out of two experiments. (B) plasma exosomes isolated from HC and AE patients were loaded onto anti-MHC class II Dynabeads and phenotyped using flow cytometry. Lines indicate the median. (C) PBMC were either cultured in only medium in the absence (−) or presence (+) of M. sympodialis or with autologous plasma exosomes in the absence (−) or presence (+) of M. sympodialis. IL-4 production in PBMC were measured by ELISPOT. (D) Culture supernatants from (C) were analysed for TNF-α levels using ELISA. Data represent mean values of triplicates for each individual (Table 1); lines indicate median.
To assess whether these plasma exosomes could elicit cytokine responses they were added to autologous PBMC. In addition, we added M. sympodialis to the assay to see whether plasma exosomes could suppress or potentiate the immune response as seen in murine models of allergic sensitisation and delayed-type hypersensitivity [36], [37]. Plasma exosomes alone could neither elicit nor inhibit IL-4 responses in PBMC in any of the two groups at a concentration of 10 µg/ml (Fig. 5C). However, plasma exosomes as well as whole yeast cells significantly increased TNF-α production in PBMC of both AE patients and HC compared to the medium control and plasma exosomes enhanced the M. sympodialis induced TNF-α response in AE patients (Fig. 5D). These data suggest that plasma exosomes can contribute to innate immune responses in both AE patients and healthy controls.
Discussion
Studies on the role of exosomes in human diseases are still hampered by the difficulties to isolate enough exosomes for functional studies in combination with their small size requiring demanding special techniques for their characterization [34]. We were here fortunate to obtain a full blood donation from the participants. Our study provides new insights into host-microbe interactions between a fungi and cells of our immune system. We found that exosomes from DCs co-cultured with M. sympodialis (DCexo Mala) carried M. sympodialis antigens and could stimulate cytokine production in autologous CD14, CD34 depleted PBMC from AE patients and HC. Furthermore, we show for the first time that M. sympodialis, a commensal yeast associated with AE [21], [24], secretes extracellular vesicles (MalaEx). These nanovesicles contain antigens and allergen from the fungi and can induce cytokine responses in CD14, CD34 depleted PBMC of AE patients and HC with a significantly higher IL-4 response in the M. sympodialis sensitized patients. The variation in IL-4 production between patients is in line with our previous study using extract of whole M. sympodialis cells [32]. Similar variation in cytokine responses in culture supernatants of PBMC stimulated with recombinant birch allergen, measured by cytometric bead array, has been reported for patients sensitised to birch pollen [38]. Our data suggest that extracellular vesicles, whether derived from M. sympodialis or from APC exposed to the fungi, may have a role in the pathogenesis of AE.
It has previously been shown that host exosomes can carry antigens from viruses and bacteria [6], [7] Exosomes from murine macrophages infected with intracellular pathogens have been found to contain pathogen associated molecular patterns (PAMPs) which could elicit pro-inflammatory responses in vitro and in vivo [6]. In case of infection with Mycobacterium avium, bacterial glycopeptidolipids could be traced through the endosomal compartment and were found in multivesicular bodies (MVBs) and on exosomes [39]. In analogy with this, M. sympodialis antigens might be processed by DCs and released on DC-derived exosomes which then induce cytokine responses.
With three different techniques we found M. sympodialis derived epitopes on MalaEx in vesicle containing sucrose gradient fractions ranging in density between 1.10–1.22 g/ml (Fig. 1A, D and E). By using patient serum we could detect an IgE-binding epitope with a size of approximately 70 kDa on MalaEx (Fig. 1E). Several IgE binding components in the 10–100 kDa molecular weight range have been identified in Malassezia and so far 10 M. sympodialis allergens have been cloned and sequenced (www.allergen.org, [24]). Thus, the observation that extracellular vesicles released by the yeast cells carry antigens and allergen and have the capacity to activate CD14, CD34 depleted PBMC raises questions on their role in the sensitization process and maintenance of the inflammatory response in AE. The nanovesicles are much smaller in size compared to whole yeast cells, which might lead to a different dissemination in the host and involve other mechanisms of cellular uptake and cell targeting. MalaEx were more potent than DCexo Mala to induce immune responses (cf Figs 2 and 4, and Table S2) which is why we speculate that MalaEx accumulate immunogenic molecules on their surface to enhance host-microbe interactions. Furthermore, a different set of molecules exposed on the surface of vesicles compared to that of yeast cells could lead to altered allergenicity. Interestingly, the elevated pH of AE skin [40] can induce an enhanced allergen release from M. sympodialis [41]. Future studies will show if altered pH will stimulate the production and allergenicity of Malassezia nanovesicles.
MalaEx and DCexo Mala also induced TNF-α responses in AE patients and HC. No statistically significant difference in TNF-α production were detected between AE patients and HC in response to any stimuli used (Table S2). It has previously been reported that M. sympodialis cells as well as the allergen Mala s 11 induce TNF-α production in MDDC and PBMC of healthy subjects [26], [42], [43]. This suggests that the TNF-α response is independent of previous sensitisation to M. sympodialis and represents an innate immune response. Our preliminary results indicate that TNF-α production in response to M. sympodialis or MalaEx involves NK-cells and possibly γδ-T-cells since an upregulation of the activation marker CD69 was seen on these cells (Gehrmann U. et al, unpublished observations).
It is reasonable to assume that exosomes from the host and extracellular vesicles from M. sympodialis coexist in vivo and contribute to host-microbe interactions. This might also be the case in our in vitro co-culture system. However, we believe that most of the immune responses recorded with DCexo Mala are induced by the exosomes from the DC and not the yeast for the following reasons: First, using iEM we found that the vast majority of vesicles in the DCexo Mala preparations were HLA-DR positive indicating their DC origin. Secondly, we have previously found that MDDC rapidly phagocytose live M. sympodialis cells within the first hr of culture [25] and we observed only few M. sympodialis cells in the medium after 48 hr of co-culture with MDDC using light microscopy (data not shown). Thirdly, by partially removing HLA-DR expressing DCexo Mala the TNF-α response was reduced by 40–50% (Fig. 3D). Due to limited amounts of exosomes we could not titrate the depletion with MHC class II beads but with a full titration an even stronger inhibition might have been seen.
Finally, we asked whether exosomes isolated from plasma could induce cytokine responses in PBMC. Human plasma exosomes are today mainly investigated as diagnostic markers for neoplastic diseases [44] and very little is known about the immunostimulatory or suppressive capacities of plasma exosomes. We found that plasma exosomes alone had no significant effect on IL-4 production indicating that they were not able to activate or suppress M. sympodialis specific responses. This might either be due to the absence of M. sympodialis antigens on plasma exosomes or to a small number of antigen-bearing plasma exosomes. Interestingly, plasma exosomes could induce TNF-α production in PBMC of both AE patients and HC (Fig. 5D) This induction could be due to the presence of PAMPs on exosomes, alternatively, pre-formed mRNA or mRNA stabilizing molecules for TNF-α [45]. One possible interpretation of these results is that plasma exosomes circulate as mediators capable of inducing a pro-inflammatory response when reaching high concentrations e.g. in local inflammatory settings. Since plasma exosomes contain leukotriene producing enzymes [46] the formation of pro-inflammatory lipid mediators and production of TNF-α might coincide and contribute to local inflammation. The capacity to induce TNF-α production has also been shown for other exosomes such as melanoma derived exosomes [47]. Although coming from different sources, the underlying mechanism for TNF-α induction might be similar for both types of exosomes.
In summary, we here present novel data that a microorganism releases extracellular vesicles that contain allergen and can contribute to inflammatory cytokine responses. This study also suggests that exosomes from DCs exposed to M. sympodialis can elicit IL-4 and TNF-α responses while plasma exosomes might be able to contribute to inflammation by inducing TNF-α. These observations have implications for understanding host-microbe interactions in the sensitisation and maintenance of the inflammation in AE.
Supporting Information
M. sympodialis induces maturation in MDDC. Phenotypes of MDDC generated from AE patients and HC assessed by flow cytometry after 48 hr culture without (−) or with (+) M. sympodialis in a 1∶5 ratio. Data show median of mean fluorescence intensity (MFI) of the sample divided by the isotyope control, 25th–75th percentile and range.
(TIF)
Protein content1) of vesicle preparations. * HC = Healthy control. † AE = Atopic eczema patient. 1)as determined by Bradford assay (BioRad, Hercules, CA). 2)Exosomes were resuspended in RPMI. 3)Exosomes were resuspended in PBS.
(PPT)
Exosome-induced cytokine responses in AE patients and healthy controls. § HC = Healthy control. † AE = Atopic eczema patient. ND = not done. 1)as determined by ELISPOT. 2)as determined by ELISA. *Mann-Whitney test to compare AE and HC, p-value<0.05.
(PPT)
(DOC)
Acknowledgments
The authors wish to thank the patients who donated blood to this study, Nurse Ingrid Eriksson and MD Maria Tengvall-Linder (Karolinska University Hospital Solna) for skillful patient handling, Ylva Gustafsson for help with experimental work and Daniel Olsson at the Department of Learning, Informatics, Management and Ethics, Karolinska Institutet, for providing help with statistical analysis.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: This work was supported by the Swedish Research Council (www.vr.se), Center for Allergy Research Karolinska Institutet (ki.se/ki/jsp/polopoly.jsp?d = 4477&l = en), the Hesselman Foundation, the Swedish Heart and Lung Association (http://www.hjart-lungfonden.se), the Groshinsky Memory Foundation, the Swedish Society for Medical Research (SSMF, www.ssmf.se), the Cancer and Allergy Association, the Swedish Asthma and Allergy Association's Research Foundation (www.astmaoallergiforbundet.se), and through the regional agreement on medical training and clinical research (ALF) between Stockholm County Council and the Karolinska Institutet (ki.se/ki/jsp/polopoly.jsp;jsessionid = a3fQhAvJt7chzjc6I5?l = en&d = 7121). U.G. holds a PhD grant from Karolinska Institutet (ki.se/ki/jsp/polopoly.jsp?l = en&d = 13467). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Pan BT, Johnstone RM. Fate of the transferrin receptor during maturation of sheep reticulocytes in vitro: selective externalization of the receptor. Cell. 1983;33:967–978. doi: 10.1016/0092-8674(83)90040-5. [DOI] [PubMed] [Google Scholar]
- 2.Pan BT, Teng K, Wu C, Adam M, Johnstone RM. Electron-microscopic evidence fore externalization of the transferrin receptor in vesicular form in sheep reticulocytes. Journal of Cell Biology. 1985;101:942–948. doi: 10.1083/jcb.101.3.942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Admyre C, Telemo E, Almqvist N, Lotvall J, Lahesmaa R, et al. Exosomes - nanovesicles with possible roles in allergic inflammation. Allergy. 2008;63:404–408. doi: 10.1111/j.1398-9995.2007.01600.x. [DOI] [PubMed] [Google Scholar]
- 4.Valadi H, Ekstrom K, Bossios A, Sjostrand M, Lee JJ, et al. Exosome-mediated transfer of mRNAs and microRNAs is a novel mechanism of genetic exchange between cells. Nat Cell Biol. 2007;9:654–659. doi: 10.1038/ncb1596. [DOI] [PubMed] [Google Scholar]
- 5.Korkut C, Ataman B, Ramachandran P, Ashley J, Barria R, et al. Trans-synaptic transmission of vesicular Wnt signals through Evi/Wntless. Cell. 2009;139:393–404. doi: 10.1016/j.cell.2009.07.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bhatnagar S, Shinagawa K, Castellino F, Schorey J. Exosomes released from macrophages infected with intracellular pathogens stimulate a proinflammatory response in vitro and in vivo. Blood. 2007;110:3234–3244. doi: 10.1182/blood-2007-03-079152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nguyen DG, Booth A, Gould SJ, Hildreth JE. Evidence that HIV budding in primary macrophages occurs through the exosome release pathway. J Biol Chem. 2003;278:52347–52354. doi: 10.1074/jbc.M309009200. [DOI] [PubMed] [Google Scholar]
- 8.Caby MP, Lankar D, Vincendeau-Scherrer C, Raposo G, Bonnerot C. Exosomal-like vesicles are present in human blood plasma. Int Immunol. 2005;17:879–887. doi: 10.1093/intimm/dxh267. [DOI] [PubMed] [Google Scholar]
- 9.Admyre C, Grunewald J, Thyberg J, Gripenback S, Tornling G, et al. Exosomes with major histocompatibility complex class II and co-stimulatory molecules are present in human BAL fluid. Eur Respir J. 2003;22:578–583. doi: 10.1183/09031936.03.00041703. [DOI] [PubMed] [Google Scholar]
- 10.Admyre C, Johansson SM, Qazi KR, Filen JJ, Lahesmaa R, et al. Exosomes with immune modulatory features are present in human breast milk. J Immunol. 2007;179:1969–1978. doi: 10.4049/jimmunol.179.3.1969. [DOI] [PubMed] [Google Scholar]
- 11.Pisitkun T, Shen RF, Knepper MA. Identification and proteomic profiling of exosomes in human urine. Proc Natl Acad Sci U S A. 2004;101:13368–13373. doi: 10.1073/pnas.0403453101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Raposo G, Nijman HW, Stoorvogel W, Liejendekker R, Harding CV, et al. B lymphocytes secrete antigen-presenting vesicles. J Exp Med. 1996;183:1161–1172. doi: 10.1084/jem.183.3.1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thery C, Duban L, Segura E, Veron P, Lantz O, et al. Indirect activation of naive CD4+ T cells by dendritic cell-derived exosomes. Nat Immunol. 2002;3:1156–1162. doi: 10.1038/ni854. [DOI] [PubMed] [Google Scholar]
- 14.Chaput N, Schartz NE, Andre F, Taieb J, Novault S, et al. Exosomes as potent cell-free peptide-based vaccine. II. Exosomes in CpG adjuvants efficiently prime naive Tc1 lymphocytes leading to tumor rejection. J Immunol. 2004;172:2137–2146. doi: 10.4049/jimmunol.172.4.2137. [DOI] [PubMed] [Google Scholar]
- 15.Hao S, Yuan J, Xiang J. Nonspecific CD4(+) T cells with uptake of antigen-specific dendritic cell-released exosomes stimulate antigen-specific CD8(+) CTL responses and long-term T cell memory. J Leukoc Biol. 2007;82:829–838. doi: 10.1189/jlb.0407249. [DOI] [PubMed] [Google Scholar]
- 16.Hao S, Liu Y, Yuan J, Zhang X, He T, et al. Novel exosome-targeted CD4+ T cell vaccine counteracting CD4+25+ regulatory T cell-mediated immune suppression and stimulating efficient central memory CD8+ CTL responses. J Immunol. 2007;179:2731–2740. doi: 10.4049/jimmunol.179.5.2731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Andre F, Chaput N, Schartz NE, Flament C, Aubert N, et al. Exosomes as potent cell-free peptide-based vaccine. I. Dendritic cell-derived exosomes transfer functional MHC class I/peptide complexes to dendritic cells. J Immunol. 2004;172:2126–2136. doi: 10.4049/jimmunol.172.4.2126. [DOI] [PubMed] [Google Scholar]
- 18.Beauvillain C, Juste MO, Dion S, Pierre J, Dimier-Poisson I. Exosomes are an effective vaccine against congenital toxoplasmosis in mice. Vaccine. 2009;27:1750–1757. doi: 10.1016/j.vaccine.2009.01.022. [DOI] [PubMed] [Google Scholar]
- 19.Beauvillain C, Ruiz S, Guiton R, Bout D, Dimier-Poisson I. A vaccine based on exosomes secreted by a dendritic cell line confers protection against T. gondii infection in syngeneic and allogeneic mice. Microbes Infect. 2007;9:1614–1622. doi: 10.1016/j.micinf.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 20.Admyre C, Bohle B, Johansson SM, Focke-Tejkl M, Valenta R, et al. B cell-derived exosomes can present allergen peptides and activate allergen-specific T cells to proliferate and produce TH2-like cytokines. J Allergy Clin Immunol. 2007;120:1418–1424. doi: 10.1016/j.jaci.2007.06.040. [DOI] [PubMed] [Google Scholar]
- 21.Akdis CA, Akdis M, Bieber T, Bindslev-Jensen C, Boguniewicz M, et al. Diagnosis and treatment of atopic dermatitis in children and adults: European Academy of Allergology and Clinical Immunology/American Academy of Allergy, Asthma and Immunology/PRACTALL Consensus Report. J Allergy Clinl Immunol. 2006;118:152–169. doi: 10.1016/j.jaci.2006.03.045. [DOI] [PubMed] [Google Scholar]
- 22.Bieber T, Novak N. Pathogenesis of atopic dermatitis: new developments. Curr Allergy Asthma Rep. 2009;9:291–294. doi: 10.1007/s11882-009-0041-2. [DOI] [PubMed] [Google Scholar]
- 23.Ashbee HR, Scheynius A. Malassezia. Pathogenic Yeasts, The Yeast Handbook. 2010:209–230. [Google Scholar]
- 24.Gaitanis G, Mayser P, Scheynius A, Crameri R. Malassezia Yeasts in Seborrhoeic and Atopic Eczemas. Malassezia and the Skin. 2010:201–229. [Google Scholar]
- 25.Buentke E, Zargari A, Heffler LC, Avila-Carino J, Savolainen J, et al. Uptake of the yeast Malassezia furfur and its allergenic components by human immature CD1a+ dendritic cells. Clin Exp Allergy. 2000;30:1759–1770. doi: 10.1046/j.1365-2222.2000.00937.x. [DOI] [PubMed] [Google Scholar]
- 26.Buentke E, Heffler LC, Wallin RP, Lofman C, Ljunggren HG, et al. The allergenic yeast Malassezia furfur induces maturation of human dendritic cells. Clin Exp Allergy. 2001;31:1583–1593. doi: 10.1046/j.1365-2222.2001.01199.x. [DOI] [PubMed] [Google Scholar]
- 27.Johansson C, Eshaghi H, Linder MT, Jakobson E, Scheynius A. Positive atopy patch test reaction to Malassezia furfur in atopic dermatitis correlates with a T helper 2-like peripheral blood mononuclear cells response. J Invest Dermatol. 2002;118:1044–1051. doi: 10.1046/j.1523-1747.2002.01758.x. [DOI] [PubMed] [Google Scholar]
- 28.Albuquerque PC, Nakayasu ES, Rodrigues ML, Frases S, Casadevall A, et al. Vesicular transport in Histoplasma capsulatum: an effective mechanism for trans-cell wall transfer of proteins and lipids in ascomycetes. Cell Microbiol. 2008;10:1695–1710. doi: 10.1111/j.1462-5822.2008.01160.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rodrigues ML, Nimrichter L, Oliveira DL, Frases S, Miranda K, et al. Vesicular polysaccharide export in Cryptococcus neoformans is a eukaryotic solution to the problem of fungal trans-cell wall transport. Eukaryot Cell. 2007;6:48–59. doi: 10.1128/EC.00318-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Casadevall A, Nosanchuk JD, Williamson P, Rodrigues ML. Vesicular transport across the fungal cell wall. Trends Microbiol. 2009;17:158–162. doi: 10.1016/j.tim.2008.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Oliveira DL, Freire-de-Lima CG, Nosanchuk JD, Casadevall A, Rodrigues ML, et al. Extracellular vesicles from Cryptococcus neoformans modulate macrophage functions. Infect Immun. 78:1601–1609. doi: 10.1128/IAI.01171-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Johansson C, Ahlborg N, Andersson A, Lundeberg L, Karlsson MA, et al. Elevated peripheral allergen-specific T cell response is crucial for a positive atopy patch test reaction. Int Arch Allergy Immunol. 2009;150:51–58. doi: 10.1159/000210380. [DOI] [PubMed] [Google Scholar]
- 33.Sallusto F, Lanzavecchia A. Efficient presentation of soluble antigen by cultured human dendritic cells is maintained by granulocyte/macrophage colony-stimulating factor plus interleukin 4 and downregulated by tumor necrosis factor alpha. J Exp Med. 1994;179:1109–1118. doi: 10.1084/jem.179.4.1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Thery C, Amigorena S, Raposo G, Clayton A. Isolation and characterization of exosomes from cell culture supernatants and biological fluids. Curr Protoc Cell Biol Chapter. 2006;3:Unit 3 22. doi: 10.1002/0471143030.cb0322s30. [DOI] [PubMed] [Google Scholar]
- 35.Johansson SM, Admyre C, Scheynius A, Gabrielsson S. Different types of in vitro generated human monocyte-derived dendritic cells release exosomes with distinct phenotypes. Immunology. 2008;123:491–499. doi: 10.1111/j.1365-2567.2007.02714.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kim SH, Bianco NR, Shufesky WJ, Morelli AE, Robbins PD. MHC class II+ exosomes in plasma suppress inflammation in an antigen-specific and Fas ligand/Fas-dependent manner. J Immunol. 2007;179:2235–2241. doi: 10.4049/jimmunol.179.4.2235. [DOI] [PubMed] [Google Scholar]
- 37.Almqvist N, Lonnqvist A, Hultkrantz S, Rask C, Telemo E. Serum-derived exosomes from antigen-fed mice prevent allergic sensitization in a model of allergic asthma. Immunology. 2008;125:21–27. doi: 10.1111/j.1365-2567.2008.02812.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gafvelin G, Thunberg S, Kronqvist M, Grönlund H, Grönneberg R, Troye-Blomberg M, et al. Cytokine and antibody responses in birch pollen-allergic patients treated with genetically modified derivatives of the major bitch pollen allergen bet v 1. Int Arch Allergy Immunol. 2005;138:59–66. doi: 10.1159/000087358. [DOI] [PubMed] [Google Scholar]
- 39.Bhatnagar S, Schorey JS. Exosomes released from infected macrophages contain Mycobacterium avium glycopeptidolipids and are proinflammatory. J Biol Chem. 2007;282:25779–25789. doi: 10.1074/jbc.M702277200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rippke F, Schreiner V, Doering T, Maibach HI. Stratum corneum pH in atopic dermatitis: impact on skin barrier function and colonization with Staphylococcus Aureus. Am J Clin Dermatol. 2004;5:217–223. doi: 10.2165/00128071-200405040-00002. [DOI] [PubMed] [Google Scholar]
- 41.Selander C, Zargari A, Mollby R, Rasool O, Scheynius A. Higher pH level, corresponding to that on the skin of patients with atopic eczema, stimulates the release of Malassezia sympodialis allergens. Allergy. 2006;61:1002–1008. doi: 10.1111/j.1398-9995.2006.01108.x. [DOI] [PubMed] [Google Scholar]
- 42.Vilhelmsson M, Johansson C, Jacobsson-Ekman G, Crameri R, Zargari A, et al. The Malassezia sympodialis allergen Mala s 11 induces human dendritic cell maturation, in contrast to its human homologue manganese superoxide dismutase. Int Arch Allergy Immunol. 2007;143:155–162. doi: 10.1159/000099082. [DOI] [PubMed] [Google Scholar]
- 43.Kesavan S, Walters CE, Holland KT, Ingham E. The effects of Malassezia on pro-inflammatory cytokine production by human peripheral blood mononuclear cells in vitro. Med Mycol. 1998;36:97–106. [PubMed] [Google Scholar]
- 44.Skog J, Wurdinger T, van Rijn S, Meijer DH, Gainche L, et al. Glioblastoma microvesicles transport RNA and proteins that promote tumour growth and provide diagnostic biomarkers. Nat Cell Biol. 2008;10:1470–1476. doi: 10.1038/ncb1800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pfeiffer JR, McAovy BL, Fecteau RE, Deleault KM, Brooks SA. CARHSP1 is required for effective TNF-{alpha} mRNA stabilization and localizes to processing bodies and exosomes. Mol Cell Biol. 2011;31:277–286. doi: 10.1128/MCB.00775-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Esser J, Gehrmann U, D'Alexandri FL, Hidalgo-Estevez AM, Wheelock CE, et al. Exosomes from human macrophages and dendritic cells contain enzymes for leukotriene biosynthesis and promote granulocyte migration. J Allergy Clin Immunol. 2010;126:1032–1040. doi: 10.1016/j.jaci.2010.06.039. [DOI] [PubMed] [Google Scholar]
- 47.Hood JL, Pan H, Lanza GM, Wickline SA Consortium for Translational Research in Advanced Imaging and Nanomedicine (C-TRAIN) Paracrine induction of endothelium by tumor exosomes. Lab Invest. 2009;89:1317–1328. doi: 10.1038/labinvest.2009.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kunz B, Oranje AP, Labreze L, Stalder JF, Ring J, et al. Clinical validation and guidelines for the SCORAD index: consensus report of the European Task Force on Atopic Dermatitis. Dermatology. 1997;195:10–19. doi: 10.1159/000245677. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
M. sympodialis induces maturation in MDDC. Phenotypes of MDDC generated from AE patients and HC assessed by flow cytometry after 48 hr culture without (−) or with (+) M. sympodialis in a 1∶5 ratio. Data show median of mean fluorescence intensity (MFI) of the sample divided by the isotyope control, 25th–75th percentile and range.
(TIF)
Protein content1) of vesicle preparations. * HC = Healthy control. † AE = Atopic eczema patient. 1)as determined by Bradford assay (BioRad, Hercules, CA). 2)Exosomes were resuspended in RPMI. 3)Exosomes were resuspended in PBS.
(PPT)
Exosome-induced cytokine responses in AE patients and healthy controls. § HC = Healthy control. † AE = Atopic eczema patient. ND = not done. 1)as determined by ELISPOT. 2)as determined by ELISA. *Mann-Whitney test to compare AE and HC, p-value<0.05.
(PPT)
(DOC)