Abstract
There is a national focus on electronic health records (EHRs) and health information exchange to improve quality, efficiency, and safety across healthcare settings. The purpose of this study is to describe pharmacists' views and practices about the adoption and use of EHRs and the sharing of health information by pharmacists in the state of Nebraska. A U.S. mail survey of all pharmacists holding a Nebraska license (N = 1,953) was conducted in June-August 2008. Only 12 percent of pharmacists indicated using an EHR. Most pharmacists (63 percent) indicated that their pharmacy had no plans to adopt an EHR system, while 13 percent indicated their pharmacy planned to adopt an EHR system in the future. Only 8 percent of respondents currently had access to EHRs for their patients created by other providers. Despite a national focus on electronic health information exchange, there remains a low uptake of EHRs by pharmacists.
Keywords: electronic health record, pharmacy record, electronic medical record, health information exchange, health information technology, Nationwide Health Information Network
Background
The national focus on the adoption and use of electronic health records (EHRs) is expected to facilitate electronic health information exchange (HIE) between healthcare providers and assist in more effective and informed healthcare decision making.1,2,3 Though pharmacists are experienced users of technology and electronic record-keeping systems to manage patients' medications and insurance information, there has been little discussion regarding their experiences with EHRs and health information exchange.4 Though exchange will ultimately involve the larger healthcare team, it remains to be seen if pharmacists will embrace the adoption of EHRs in all practice settings.
The pharmacy record currently serves as a repository for patient information relevant to medication use in nearly all healthcare settings. The pharmacy record in the hospital, home care, nursing home, and community pharmacy settings typically contains information about patients' prescription medications; allergies to drugs and other exposures; pharmacists' care plan notes that include patient-specific considerations (e.g., preferred medication use decisions governed by formularies); and a variety of elements included in a patient's medication use history often including over-the-counter medication and herbal supplement use. In the outpatient setting, pharmacy records have been used to reveal patient medication use patterns based upon pharmacy refills, often recognized as a relatively accurate proxy for a patient's general adherence to medication regimens.5 The detail maintained in an outpatient pharmacy record about medication management typically exceeds that documented in EHRs maintained by other provider types and settings in order to serve the needs of the patient-pharmacist relationship. Outpatient pharmacy records indicate what prescribed medications a patient has chosen to pick up from the pharmacy for use, and may also make reference to the patient's medication use behaviors and outcome responses to prescribed therapies. Pharmacists use the pharmacy record as a source of information about the patient's overall medication use as a safety and quality-of-care check when filling prescription orders. The pharmacy record is also a resource to aid pharmacists in assessing appropriateness of the prescribed therapy in the context of each patient's individual situation. Examples of pharmacy record software include McKesson EnterpriseRx and Cerner Etreby Pharmacy Management System.6 Pharmacists in inpatient care settings or those part of an integrated health system such as Kaiser Permanente or the Veterans Affairs system may work with a pharmacy record that is integrated with other providers' records, or may use a separate electronic pharmacy record that either “crosstalks” electronically with a patient's health record or from which the pharmacist can toggle between screens to review the larger record and process the orders in the pharmacy record.
In comparison, EHRs are expected to contain comprehensive information about a patient's health, including medical conditions and care received from multiple providers who have access to the patient's record and privileges to use or modify it. The national goal of implementing interoperable EHRs to create a Nationwide Health Information Network (NHIN) will allow healthcare providers to have not only access to patients' health history (both within a single health system and across multiple health systems) but also real-time access to the most up-to-date patient information, including lab results and progress notes.7,8 Access to additional information beyond that maintained in the pharmacy record has the potential to improve pharmacists' ability to provide optimal medication therapy management. Some proposed ways that both pharmacists and patients could benefit from the introduction of an EHR into pharmacy practice are improvements in the medication reconciliation process both within healthcare organizations and between care settings, progression of public health initiatives, and enhancement of the patient-pharmacist relationship.9,10
The introduction of HIE will facilitate pharmacists' efforts to better assist patients in the management of their own disease states and medications. This will further enhance communication between pharmacists and patients, contributing to an evolving patient-pharmacist relationship that is impacted by the increased use of health information technology (e.g., EHRs, personal health records, e-prescribing, and patient-specific technologies already being used). Pharmacists are accessible resources for healthcare, a role that will likely be enhanced by HIE and one that will continue to grow as the HIE movement evolves.11,12 The use of pharmacists to manage patients' care for chronic conditions, such as through the use of collaborative practice agreements, can be enhanced through the additional patient information available in the EHR. Competency levels will need to be established for pharmacists to demonstrate the ability to obtain, utilize, and contribute to the patient information maintained in the EHR, leading to evolving privileging and credentialing of pharmacists.13 For instance, obtaining a pharmacotherapy specialist credential or developing a collaborative practice agreement allowing pharmacists to directly manage patients' care may require a pharmacist to demonstrate an understanding of the benefits and limitations of EHRs and/or the technical skills to use the EHR system. The health information management (HIM) profession needs to be informed about pharmacists' adoption and use of EHRs to better understand how this will affect the profession in ways not previously considered.
The purpose of this study is to describe pharmacists' views and practices about the adoption and use of EHRs and the sharing of health information in all pharmacy practice settings in the state of Nebraska.
Methods
A statewide survey of pharmacists was conducted in June-August 2008 to assess patient safety issues currently faced in practice.14 A modified Dillman technique was used to distribute the survey through U.S. mail to all individuals holding a Nebraska pharmacists' license and actively practicing in the state (N = 1,953).15 The survey was developed by a team consisting of pharmacists, health services researchers, and key members of state health organizations in order to provide an evidence base to aid pharmacists in identifying possible practice improvements and strategies to address newly emerging problems in patient safety. Questions on the survey included items about the state of EHR adoption in pharmacy practice and pharmacists' interactions with other healthcare providers regarding the sharing of patient health information. This study was approved by the Creighton University Institutional Review Board and received exempt status.
Results
Demographics
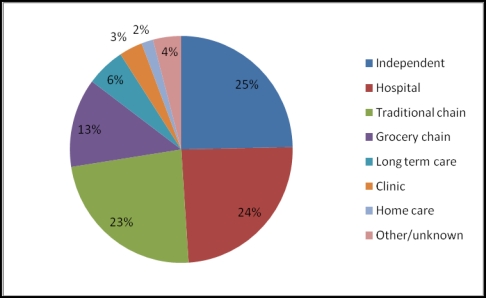
The survey was completed by 535 pharmacists for a 27 percent response rate. Respondents practiced across a range of pharmacy settings (Figure 1), including independent pharmacies (25 percent), hospital pharmacies (24 percent), traditional chain pharmacies (23 percent), and grocery chain pharmacies (13 percent). Respondents had been in practice for an average of 21 years, and 56 percent were female.
Figure 1.
Primary Practice Setting of Nebraska Pharmacists
EHR Adoption Status
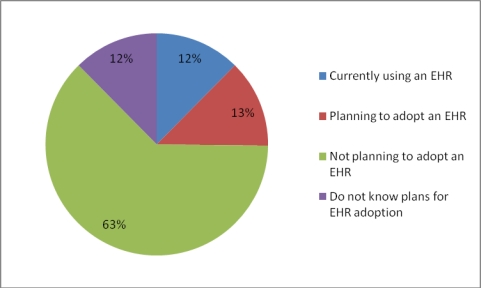
Figure 2 displays the EHR adoption status of respondents. Only 12 percent of respondents indicated that they were currently using an EHR. Of these 12 percent, nearly three-fourths (72 percent) indicated they worked in a hospital setting. The remaining EHR users were located in traditional chain pharmacies (12 percent), clinic pharmacies (10 percent), home care pharmacies (3 percent), and independent pharmacies (3 percent). Most pharmacists (63 percent) indicated that their pharmacy had no plans to adopt an EHR. This was most frequently reported by pharmacists in independent pharmacies (33 percent), followed by traditional chain pharmacies (20 percent), grocery chain pharmacies (17 percent), hospital pharmacies (14 percent), long-term care pharmacies (7 percent), clinic pharmacies (4 percent), home care pharmacies (2 percent), and other (4 percent). A small percentage of respondents (13 percent) indicated that their pharmacy planned to adopt an EHR in the future. Of these pharmacists, 37 percent indicated working in a hospital setting, with the remaining pharmacists in traditional chain pharmacies (26 percent), independent pharmacies (19 percent), grocery chain pharmacies (8 percent), long-term care pharmacies (6 percent), home care pharmacies (2 percent), and clinic pharmacies (2 percent). Twelve percent of respondents reported not knowing their pharmacy's plans regarding EHR adoption. Few pharmacists reported having any prior experience using an EHR (16 percent).
Figure 2.
Electronic Health Record Adoption Status Reported by Nebraska Pharmacists
Patient Health Information in the Pharmacy Record
Few pharmacists were using EHRs, citing a large amount of patient health information already available in the pharmacy record (Table 1). Pharmacists indicated that allergies (91 percent) were the most common type of information maintained in the pharmacy record. Other information contained in the pharmacy record varied in frequency, including patients' chronic conditions (48 percent), renal function (34 percent), hepatic function (28 percent), height (26 percent), weight (26 percent), smoking status (14 percent), alcohol consumption (13 percent), and pregnancy status (39 percent) or lactation status (24 percent) in women.
Table 1.
Patient Health Information Kept in the Pharmacy Record
| Type of Patient Health Information | N (%) |
|---|---|
| Allergies | 487 (91.0) |
| Chronic conditions | 254 (47.5) |
| Pregnancy | 210 (39.3) |
| Renal impairment | 183 (34.2) |
| Liver impairment | 151 (28.2) |
| Weight | 141 (26.4) |
| Height | 139 (26.0) |
| Lactation | 129 (24.1) |
| Smoking status | 76 (14.2) |
| Alcohol consumption | 67 (12.5) |
Sharing of Patient Health Information with Other Providers
Concerning issues of sharing patient health information, 80 percent of pharmacists believed they should have access to patient EHRs created by other providers; however, only 8 percent of respondents currently had access to these records. These 8 percent of pharmacists practiced primarily in a hospital setting (72 percent), followed by traditional chain pharmacies (12 percent), clinic pharmacies (10 percent), independent pharmacies (3 percent), and home care pharmacies (3 percent). Pharmacists believed they should share the following information with other providers (Table 2): medication history (94 percent), allergies (93 percent), health history (72 percent), immunizations (69 percent), laboratory data (64 percent), and progress notes (57 percent).
Table 2.
Patient Health Information Pharmacists Would Share with Other Health Providers
| Type of Information | N (%) |
|---|---|
| Medication history | 504 (94.2) |
| Allergies | 496 (92.7) |
| Health history | 384 (71.8) |
| Immunizations | 371 (69.3) |
| Laboratory data | 343 (64.1) |
| Progress notes | 305 (57.0) |
Discussion
The support for the 2004 national mandate for every American to have an EHR by 2014 has recently taken the form of financial funding through the Health Information Technology for Economic and Clinical Health (HITECH) Act, a part of the larger American Recovery and Reinvestment Act of 2009.16 This funding is intended to facilitate EHR adoption, primarily in physician practices. This is a crucial component for the formation of a NHIN that will connect healthcare providers across the United States for HIE.17
This study revealed that few pharmacists are engaging in HIE with other providers or patients, and those that are currently exchanging health information practice in predominantly a hospital setting. This is not unexpected given the state of physician EHR adoption observed around the nation and within the state of Nebraska.18,19,20 It can be argued that pharmacists will not adopt EHRs until more physician practices do so, due to a lack of perceived benefits (i.e., no increased access to patient health information not maintained in the pharmacy record).
Despite many concerns patients have regarding HIE, they believe it is important for their healthcare providers to use electronic or computer-based records instead of paper records.21 A recent consumer survey noted that the majority of respondents believed that if the United States adopted an interoperable medical record system, the overall quality of medical care would likely improve, fewer people would get sick and die as a result of medical errors, and doctors would do a better job of coordinating their care.22 Our findings indicate this is potentially true, specifically concerning pharmacists, as the information that would become available could greatly enhance the information currently being maintained in the pharmacy record. Table 1 indicates that nearly all (91 percent) of the respondents have information about patient allergies, almost half (48 percent) have information about patients' chronic conditions, over a third have information about patients' pregnancy status (39 percent) and renal impairment (34 percent), and over a quarter have information about patients' liver impairment (28 percent). This information allows pharmacists to make the best possible assessment regarding the appropriateness of a patient's medication therapy. If many pharmacists already maintain this information in the pharmacy record without the advantage of HIE, enhanced access to additional clinical information for medication therapy management through an EHR would prove highly beneficial. Additionally, the type of information that pharmacists believe they should share with their physician counterparts suggests that the use of EHRs to integrate this information potentially holds high value for physicians and overall is likely to improve the quality of information that is available to manage patients' care. Physicians who have used EHRs reported experiencing a positive effect on quality of clinical decisions, communication with other providers, timely access to medical records, and avoidance of medical errors.23 Despite these potential benefits and the national focus on EHRs, the technology has yet to be widely adopted by physicians as well. It is estimated that only 4 percent of ambulatory care physician practices nationwide have a fully functional EHR system, and only 13 percent have a basic system.24 Nebraska ambulatory care physicians reported that 30 percent currently use EHRs in some form.25 There are similar adoption rates in hospitals, as only 1.5 percent of U.S. hospitals have a comprehensive EHR system, and only 7.6 percent have a basic system.26
HIM professionals need to continue to stay informed about the role of pharmacists in the health information technology (HIT) movement. As HIE takes greater hold throughout the nation, the issues of pharmacist privileging, credentialing, and expertise necessary to utilize these new sources of information will continue to grow.27 HIM professionals are also integrally involved in issues pertaining to access to and use of electronic health information. Findings from this study indicate that HIM professionals will have to understand the evolving role of different health professionals in the context of EHR and HIT use in order to understand which providers will need access to patient health information and how best to address issues related to this access.
The state of Nebraska has led discussions among the various stakeholders in EHR adoption through the state eHealth Council.28 The coauthors of this work have been directly engaged in these early conversations and have observed the early interactions of the pharmacy profession's participation in this movement. This state-level view of pharmacists and HIE may help to inform pharmacists, health information managers, and policy makers about the progress being made toward achieving the formation of a NHIN that includes the pharmacist, and about the potential role that pharmacists may play in this movement.
Limitations
The survey used in this study yielded a 27 percent response rate. This relatively low response rate is likely to represent a biased sample in favor of those who were both motivated and able to participate. On the other hand, the entire population was surveyed, resulting in over one-fourth of the entire population contributing to the data. With a simple random sample, we would only need responses from a small portion of the population. Inspection of the distribution of responses from pharmacists suggests that the distribution is representative of each major type of pharmacy practice setting.
Conclusion
Despite a national focus on HIE, there remains a low uptake of EHRs by health providers, including pharmacists. Though HIT offers great promise for enhancing availability of information for pharmacists to improve patient safety and quality of care, further study on barriers to and solutions for EHR adoption from the pharmacy perspective and the effectiveness of implementation strategies is needed.
Support
Funding for this study was provided by the Nebraska Department of Health and Human Services Office of Rural Health and the Nebraska State Board of Pharmacy, through the Dyke Anderson Patient Safety Grant.
Contributor Information
Kevin T Fuji, Kevin T. Fuji, PharmD, is a resident assistant professor at the Center for Health Services Research and Patient Safety in the School of Pharmacy and Health Professions at Creighton University in Omaha, NE..
Kimberly A Gait, Kimberly A. Gait, PharmD, PhD, FASHP, is a professor of pharmacy practice and director of the Center for Health Services Research and Patient Safety in the School of Pharmacy and Health Professions at Creighton University in Omaha, NE..
Mark V Siracuse, Mark V. Siracuse, PharmD, PhD, is an associate professor of pharmacy sciences at the Center for Health Services Research and Patient Safety in the School of Pharmacy and Health Professions at Creighton University in Omaha, NE..
J. Scott Christoffersen, J. Scott Christoffersen is a PharmD candidate in the School of Pharmacy and Health Professions at Creighton University in Omaha, NE..
Notes
- 1.Hillestad Richard, Bigelow James, Bower Anthony, Girosi Federico, Meili Robin, Scoville Richard, Taylor Roger. “Can Electronic Medical Record Systems Transform Health Care? Potential Health Benefits, Savings, and Costs”. Health Affairs. 2005;24(no. 5):1103–17. doi: 10.1377/hlthaff.24.5.1103. [DOI] [PubMed] [Google Scholar]
- 2.Chaudry Basit, Wang Jerome, Wu Shinyi, Maglione Margaret, Mojica Walter, Roth Elizabeth, Morton Sally C, Shekelle Paul G. “Systematic Review: Impact of Health Information Technology on Quality, Efficiency, and Costs of Medical Care”. Annals of Internal Medicine. 2006;144:E12–E22. doi: 10.7326/0003-4819-144-10-200605160-00125. [DOI] [PubMed] [Google Scholar]
- 3.Institute of Medicine . Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001. [PubMed] [Google Scholar]
- 4.Downard Susan, Gait Kimberly A, Reel Adam B. “Pharmacists' Use of Electronic Health Records: Silent Leaders No More”. Journal of the American Pharmacists Association. 2008;47(no. 6):680–92. doi: 10.1331/JAPhA.2007.07531. [DOI] [PubMed] [Google Scholar]
- 5.Bubalo Joseph, Clark Roger K, Jiing Susie S, Johnson Nathan B, Miller Katherine A, Clemens-Shipman Colleen J, Sweet Amanda L. “Medication Adherence: Pharmacist Perspective”. Journal of the American Pharmacists Association. 2010;50(no. 3):394–406. doi: 10.1331/JAPhA.2010.08180. [DOI] [PubMed] [Google Scholar]
- 6.Surescripts. “Surescripts Certified Pharmacy Software.” Available at http://www.surescripts.com/connect-to-surescripts/pharmacy-software.aspx Accessed February 18,2011.
- 7.Downard, Susan, Kimberly A. Gait, and Adam B. Reel. “Pharmacists' Use of Electronic Health Records: Silent Leaders No More.” [DOI] [PubMed]
- 8.U.S. Department of Health and Human Services. “Nationwide Health Information Network.” Available at http://healthit.hhs.gov/portal/server.pt?open=512&mode=2&cached=true&objID=1142 Accessed December 21, 2010.
- 9.Downard, Susan, Kimberly A. Gait, and Adam B. Reel. “Pharmacists' Use of Electronic Health Records: Silent Leaders No More.” [DOI] [PubMed]
- 10.American Society of Health-System Pharmacists “ASHP Long-Range Vision for the Pharmacy Work Force in Hospitals and Health Systems”. American Journal of Health-System Pharmacy. 2007;64:1320–30. doi: 10.2146/ajhp070057. [DOI] [PubMed] [Google Scholar]
- 11.American Society of Health-System Pharmacists “ASHP Long-Range Vision for the Pharmacy Work Force in Hospitals and Health Systems”. American Journal of Health-System Pharmacy. 2007;64:1320–30. doi: 10.2146/ajhp070057. [DOI] [PubMed] [Google Scholar]
- 12.Berens, D., Kimberly Gait, and Karen A. Paschal. Security and Privacy Barriers to Health Information Interoperability Report 3: Consumer Views about Privacy and Electronic Health Information Exchange. Available at http://chrp.creighton.edu/share/sharedfiles/UserFiles/file/HISPCReport3.pdf Accessed December 20, 2010.
- 13.Gait Kimberly A. “Credentialing and Privileging for Pharmacists”. American Journal of Health-System Pharmacy. 2004;61:661–70. doi: 10.1093/ajhp/61.7.661. [DOI] [PubMed] [Google Scholar]
- 14.Creighton Health Services Research Program. State of Patient Safety in Nebraska Pharmacy. December 2008. Available at http://chrp.creighton.edu/share/sharedfiles/UserFiles/file/State_of_Patient_Safety_in_Nebraska_Pharmacy_December_2008.pdf Accessed December 20, 2010.
- 15.Dillman D.A, Smyth Jolene D, Christian Leah M. Internet, Mail, and Mixed-Mode aSurveys: The Tailored Design Method. 3rd ed. Hoboken, NJ: Wiley; 2009. [Google Scholar]
- 16.U.S. Congress. American Recovery and Reinvestment Act of 2009. Available at http://frwebgate.access.gpo.gov/cgi-bin/getdoc.cgi?dbname=l1l_cong_bills&docid=f:hlenr.pdf Accessed December 19, 2010.
- 17.U.S. Department of Health and Human Services. “Nationwide Health Information Network.”
- 18.DesRoches Catherine M, Campbell Eric G, Rao Sowmya R, Donelan Karen, Ferris Timothy G, Jha Ashish, Kaushal Rainu, Levy Douglas E, Rosenbaum Sara, Shields Alexandra E, Blumenthal David. “Electronic Health Records in Ambulatory Care-A National Survey of Physicians”. New England Journal of Medicine. 2008;359:50–60. doi: 10.1056/NEJMsa0802005. [DOI] [PubMed] [Google Scholar]
- 19.Jha Ashish K, DesRoches Catherine M, Campbell Eric G, Donelan Karen, Rao Sowmya R, Ferris Timothy G, Shields Alexandra, Rosenbaum Sara, Blumenthal David. “Use of Electronic Health Records in U.S. Hospitals”. New England Journal of Medicine. 2009;360:1628–38. doi: 10.1056/NEJMsa0900592. [DOI] [PubMed] [Google Scholar]
- 20.Gait, Kimberly A., James D. Bramble, Andjela Drincic, Mark V. Siracuse, Karen A. Paschal, Amy A. Abbott, Ted A. Kasha, and Kevin T. Fuji. Status of Health Information Technology in Nebraska: Focus on Electronic Health Records in Physician Offices. March 2008. Available at http://chrp.creighton.edu/share/sharedfiles/UserFiles/file/Status_of_Health_Information_TechnologyinNebraskaMarch2008.pdf Accessed December 16, 2010.
- 21.NPR, Kaiser Family Foundation, and Harvard School of Public Health. The Public and the Health Care Delivery System. April 2009. Available at http://www.kff.org/kaiserpolls/upload/7887.pdf Accessed December 22, 2010.
- 22.NPR, Kaiser Family Foundation, and Harvard School of Public Health. The Public and the Health Care Delivery System. April 2009. Available at http://www.kff.org/kaiserpolls/upload/7887.pdfhttp://www.kff.org/kaiserpolls/upload/7887.pdf Accessed December 22, 2010.
- 23.DesRoches, Catherine M., Eric G. Campbell, Sowmya R. Rao, Karen Donelan, Timothy G. Ferris, Ashish Jha, Rainu Kaushal, Douglas E. Levy, Sara Rosenbaum, Alexandra E. Shields, and David Blumenthal. “Electronic Health Records in Ambulatory Care-A National Survey of Physicians.” [DOI] [PubMed]
- 24.DesRoches, Catherine M., Eric G. Campbell, Sowmya R. Rao, Karen Donelan, Timothy G. Ferris, Ashish Jha, Rainu Kaushal, Douglas E. Levy, Sara Rosenbaum, Alexandra E. Shields, and David Blumenthal. “Electronic Health Records in Ambulatory Care-A National Survey of Physicians.” [DOI] [PubMed]
- 25.Gait, Kimberly A., James D. Bramble, Andjela Drincic, Mark V. Siracuse, Karen A. Paschal, Amy A. Abbott, Ted A. Kasha, and Kevin T. Fuji. Status of Health Information Technology in Nebraska: Focus on Electronic Health Records in Physician Offices.
- 26.Jha, Ashish K., Catherine M. DesRoches, Eric G. Campbell, Karen Donelan, Sowmya R. Rao, Timothy G. Ferris, Alexandra Shields, Sara Rosenbaum, and David Blumenthal. “Use of Electronic Health Records in U.S. Hospitals.”
- 27.Gait, Kimberly A. “Credentialing and Privileging for Pharmacists.”
- 28.Nebraska Information Technology Commission. “eHealth Council.” Available at http://www.nitc.nebraska.gov/ehc/ Accessed December 18, 2010.