Abstract
Background
Developing valid control groups that generate similar perceptions and expectations to experimental complementary and alternative (CAM) treatments can be challenging. The perceived credibility of treatment and outcome expectancy often contributes to positive clinical responses to CAM therapies, thereby confounding efficacy data. As part of a clinical feasibility study, credibility and expectancy data were obtained from subjects suffering from migraine who received either CranioSacral therapy (CST) or an attention-control, sham, and low-strength magnet (LSSM) intervention.
Objective
The objective of this study was to evaluate whether the LSSM intervention generated similar levels of subject credibility and expectancy compared to CST.
Design
This was a two-arm randomized controlled trial.
Subjects
Sixty-five (65) adults with moderate to severe migraine were the subjects of this study.
Interventions
After an 8-week baseline, subjects were randomized to eight weekly treatments of either CST (n=36) or LSSM (n=29). The latter involved the use of a magnet-treatment protocol using inactive and low-strength static magnets designed to mimic the CST protocol in terms of setting, visit timing, body positioning, and therapist–subject interaction.
Outcome measures
A four-item, self-administered credibility/expectancy questionnaire, based on a validated instrument, was completed after the first visit.
Results
Using a 0–9 rating scale, the mean score for perceived logicality of treatment was significantly less for LSSM (5.03, standard deviation [SD] 2.34) compared to CST (6.64, SD 2.19). Subject confidence that migraine would improve was greater for CST (5.94, SD 2.01) than for LSSM (4.9, SD 2.21), a difference that was not statistically significant. Significantly more subjects receiving CST (6.08, SD 2.27) would confidently recommend treatment to a friend than those receiving LSSM (4.69, SD 2.49).
Conclusions
Although LSSM did not achieve a comparable level of credibility and expectancy to the CST, several design and implementation factors may have contributed to the disparity. Based on analysis of these factors, the design and implementation of a future study may be improved.
Introduction
Amajor challenge in research on complementary and alternative medicine (CAM) is the development of a valid control group with which to compare the intervention of interest.1 In a well-designed study, the ideal control intervention should closely resemble or mimic the intervention in terms of procedure, treatment duration and frequency, and therapist attention.2 In this way, researchers can assess and control for placebo effects induced by a range of heterogeneous contextual, personal, and relational factors experienced by the patient during treatment.3
Patient perceptions about treatment credibility and expectancy of treatment outcome can play a large role in persistent clinical improvement.3–7 For example, in a meta-analysis of four randomized trials of acupuncture for chronic pain, Linde et al. reported that more subjects with high expectations for improvement actually improved, compared with those who had low expectations.8 In another systematic review, positive subject expectations were consistently associated with better outcomes in 15 of 16 moderate to high-quality clinical trials.4
Treatment credibility in a research context can be defined as the extent to which subjects perceive experimental and control modalities to be rational and believable approaches to their clinical problem.9 Expectancy is the belief that clinical improvement will occur as a result of the intervention. Both factors must be accounted for in studies of treatment efficacy, usually by using a control intervention that is equally potent in establishing treatment credibility and expectancy of improvement without affecting the biologic mechanism engendered by the intervention under study.9,10
This study reports the credibility and expectation of benefit of a novel attention-control procedure in a feasibility study of CranioSacral therapy (CST) as adjunctive treatment for migraine. The control procedure, involving a sham magnet treatment protocol using inactive and low-strength static magnets (LSSM), was designed to generate similar levels of credibility and expectation of benefit among the subjects in the control group compared to the active intervention group.
Materials and Methods
Intervention development
A feasibility study was undertaken for developing a randomized, controlled trial to compare the effectiveness of CST as adjunctive treatment for migraine compared to an attention-control intervention using LSSM. The study protocol has been described elsewhere.11 CST was developed by Dr. John Upledger, DO using the concept that abnormal cerebrospinal fluid rhythms may follow birth injury or later traumas and lead to a variety of neurophysiologic disturbances and symptoms.11 CST, which purportedly releases tissue restrictions and eliminates stasis within the hydraulic system of the brain and spinal cord, is increasingly sought by the public for the relief of multiple conditions, including (1) headache, (2) asthma, (3) arthritis, (4) insomnia, (5) cerebral palsy, (6) autism, (7) memory disturbances, (8) whiplash injuries, and (9) fibromyalgia.11
The proposed randomized trial for which this feasibility study was undertaken would compare CST with a control intervention, as measured by headache frequency and intensity, and quality of life, (using the Headache Impact Test), perception of benefit, migraine-related disability, general health status (SF 36), and health care utilization.12–15 This feasibility study was needed to develop, standardize, and clarify treatment and control protocols, recruitment strategies, and measurement and data-collection methods. The development and credibility of treatment and control protocols in the management of moderate to severe migraine headaches are reported here.
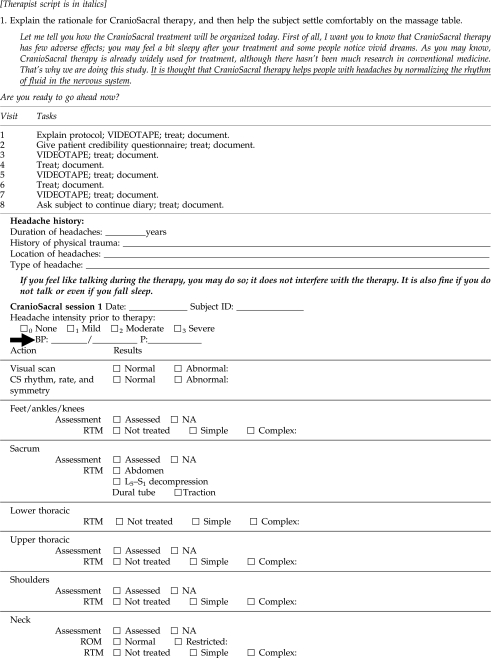
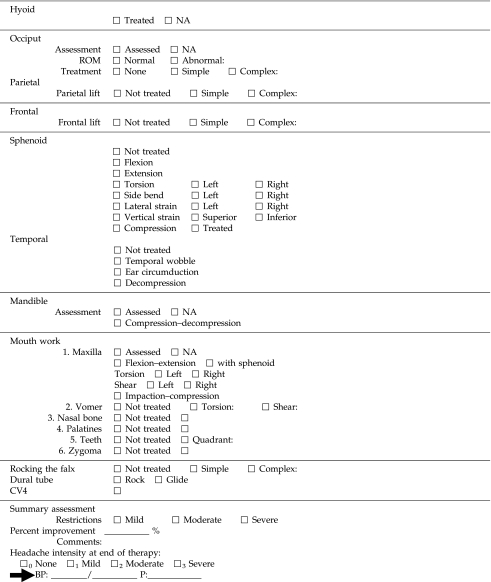
Development of treatment protocols
CST and LSSM protocols required development, standardization, and evaluation for their practical and efficient application in the eventual efficacy trial. A CST protocol was based on the clinical evaluation and treatment system developed by the Upledger Institute, comprising the intervention elements shown in Table 1 and described previously.11,15 An LSSM protocol was designed as an attention-control condition matching such features of the CST protocol as frequency and duration of visits, therapist–subject interaction, and treatment setting. Table 1 compares the two treatment protocols. The complete CST and LSSM protocols are described in the Appendix.
Table 1.
Comparison of Treatment Protocols: CranioSacral Therapy and Magnet Therapy for Migraine
| All subjects: |
|---|
| • Initial brief review of recent headache and general symptoms |
| • Assessment of any adverse effects of prior treatment |
| • Blood pressure and pulse recorded before and after visit |
| • Headache severity recorded before and after visit |
| • Visual scan |
| • Subject remains supine for treatment |
| • Total clinic visit time=45 minutes |
| CranioSacral therapy | Magnet therapy |
|---|---|
| Evaluation of the CranioSacral rhythm,a including amplitude, quality, and rate | Fixed magnets (12) applied around the table Magnet strength assessed at each position |
| Magnet strength assessed at each position | |
| CranioSacral assessment and treatment | Magnet pad application |
| Pelvis | Pelvis |
| Lower respiratory | Lower diaphragm |
| Thoracic inlet | Upper thorax (front and back) |
| Shoulders | Upper thorax toward shoulders |
| Neck | Neck |
| Occiput | Occiput (front and back) |
| Frontal/parietal bone lifts | Head and feet |
| Sphenoid and mandible mouth work |
The CranioSacral rhythm is palpated by the practitioner (at the feet) and assessed for rate, quality, and symmetry.
A normal rate is 8–12 cycles per minutes. A normal rhythm shows a balanced vitality.
CST intervention
The CST assessment and intervention was performed by 1 practicing therapist, who is also a registered nurse and licensed massage therapist, with extensive training and experience in CST. Only 1 therapist was utilized at this phase of the research because it was believed that a single individual, with training and close supervision in this research setting, was more likely to achieve a standardized approach to each subject than could be achieved by a variety of therapists, especially in a modality where weak clinical reliability between practitioners has been reported.16,17
Control intervention
One important question was whether CST (a manual technique) could be effectively mimicked as a sham procedure, or whether a different but appropriate complementary modality could be used as an effective control procedure. Two options were considered.
Option 1: Sham CST
Sham maneuvers have been widely used as controls in osteopathic medicine and chiropractic research.9,18,19 An ideal control method for CST, which consists of assessment and treatment using gentle muscle palpation and mobilization techniques, would be to exactly replicate the CST protocol without producing any treatment effect. Sham CST would have to be given either by an expert CST practitioner or by a specially trained massage therapist. Furthermore, the CST sham procedure would have to last a comparable amount of time (i.e., 45 minutes) as the CST treatment and be standardized and replicable at each visit. Ultimately, it was concluded that it was unlikely a sham manual procedure could be created that would closely mimic CST without producing an unintended biologic effect.
Option 2: LSSM
Inert and active magnets were provided courtesy of American Health Services Magnets, Palatine, IL. Instead of a sham CST arm, it was decided to develop a control protocol that could generate similar elements of placebo effects. These elements included (1) a similar procedural treatment sequence using gentle physical contact directed at the same anatomical areas; and (2) replication of the CST visit context using the same therapist in the same location (i.e., the therapist's treatment room in an integrative outpatient clinic) as that used for subjects receiving the true CST intervention. It was posited that magnet therapy, widely used by the public for pain syndromes, could generate equivalent therapeutic credibility and outcome expectations if delivered in the same context and by the same therapist as in the CST arm. Static magnet therapy is a popular and near-zero risk modality that, at low to moderate intensities (300–800+ G), has been shown to affect nerve cells and increase local tissue blood flow and oxygenation when magnets are in direct contact with the skin.20–22
The CST therapist was trained in the LSSM protocol for this study. To ensure that the LSSM control protocol had no human biologic effects, the protocol called for the therapist to place six identical inert ceramic magnets (1.6 cm in diameter and 0.4-cm thick) and six weakly active bipolar magnets (300–500 G) at intervals around the perimeter of the examination table on which the control subject was resting. Both the active and inert magnets were placed at distances of 3 to 5 inches from the subject's body, with the active magnets positioned further than the inert magnets. (The inverse square law, as applied to electromagnetism, states that doubling the distance between subject and magnet reduces field intensity by 75%.) At each session, the therapist used a magnetometer to confirm that for the active magnets the field intensity at the subject's skin was close to zero (no more than 30–80 G) (DC Magnetometer Model 1, with a resolution of 0.1 G, manufactured by AlphaLab, Inc., Salt Lake City, UT). The magnetometer was also used by the therapist to display a positive reading when placed up against an active magnet in order to enhance the believability of the magnet intervention for curious subjects.
In order to replicate more exactly the sequence and anatomical location of the CST protocol, three inert magnets (rectangular 2×5 cm by 0.4-cm thick) contained inside a cloth pad were applied by the therapist to several locations on the center of the body (over clothes, from the lower part of the abdomen to the head). This cloth pad was applied to the same locations at the same time intervals as in the CST procedure (Table 2). In contrast to the CST, no soft-tissue pressure or motion was exerted by the pad, and there was no direct touching of the subject by the therapist (other than assistance in getting on and off the table). The therapist remained attentive and in the room with the subject during the entire procedure, either sitting or moving about the room to apply the magnets and monitor their strength. In both the CST and LSSM protocols, conversation between subject and therapist was driven by subjects' preferences.
Table 2.
Characteristics of the Study Sample: CranioSacral Therapy for Migraine, 2006–2008
| Characteristic | CranioSacral therapy group (N=36)a | Magnet therapy group (N=33) |
|---|---|---|
| Mean (range) | Mean (range) | |
| Age (years) | 42.9 (12–71) | 41.2 (19–72) |
| Education (years of school) | 16.7 (7–28) | 16.9 (12–20) |
| Average number of monthly headache days, pretreatmentb | 13.4 (5–28) | 13.6 (6–27) |
| N (%) | N (%) | |
|---|---|---|
| Female | 33 (91.7) | 32 (97.0) |
| White | 28 (77.8) | 29 (87.9) |
| Living with partner | 24 (66.7) | 23 (69.7) |
| Employed | 24 (66.7) | 29 (87.9) |
| Household income | ||
| <$20,000 | 6 (16.7) | 1 (3.03) |
| $20,000–59,999 | 12 (33.3) | 8 (24.2) |
| $60,000–99,999 | 4 (11.1) | 8 (24.2) |
| >$100,000 | 13 (36.1) | 10 (30.3) |
| Missing | 1 | 6 |
Reported N reflects the 69 randomized subjects.
The mean number of headache days was calculated from the mean number of headaches in the 2 months prior to the intervention and the mean number of days reported in the diaries.
In the process of informed consent, the study volunteers were given a description of CST and magnet therapy and their potential usefulness for improving migraine headaches. At the beginning of the first treatment, the therapist described, per scripted protocol, how CST and magnets might produce a biologic effect, referring to available articles and pamphlets describing the benefits of CST and magnet therapy, available in her treatment room (see the Appendix for therapist's script for CST and LSSM conditions).
Reliability of the therapist
The therapist was a key participant in the initial development of both CST and magnet protocols (subject communication, technique, and sequencing) and was subsequently trained in the procedures over several weeks. Particular emphasis was given to standardizing communication, movement, and contact with the subject to eliminate bias; the first, third, fifth, and seventh treatment sessions with each subject were videotaped and evaluated by research staff for communication or physical bias toward one or other of the protocols.
Assessment of treatment credibility and expectancy
The credibility of the protocols and the expectancy of improvement for each subject were assessed by their completion of a commonly used and adapted self-report instrument that had been originally developed by Borkovec and Nau.23,24 Borkovec and Nau used a 0- to 9-point scale for five questions to which the subject could mark his/her degree of confidence in treatment rationale and expected outcome, regarding psychologic interventions for a specific psychologic problem: anxiety in public speaking. Others have successfully modified this scale, adapting it for use with other illnesses and interventions.25,26 The first three of the original five items in Borkovec and Nau's instrument were adapted: (1) How logical does this type of treatment seem to you? (2) How confident would you be that this treatment would be successful? and (3) How confident would you be in recommending this treatment to a friend? An attempt was made to adapt the final two questions of Borkovec and Nau's original questionnaire, which deal with hypothetical situations involving anxiety23 (i.e., “If you were extremely anxious in speech situations, would you be willing to undergo such treatment?” and “How successful do you feel this treatment would be in decreasing a different fear, for example, strong anxiety about taking tests?”). Instead, a question was added regarding the subject's confidence in the therapist's competence—a factor closely linked to treatment credibility. The resulting four-item questionnaire was completed by each subject at the beginning of the second treatment visit and was placed in an envelope for retrieval by the research staff. The four questions were worded as follows:
1. How logical does this type of therapy seem to you for helping people treat or prevent their headache? (Not logical [0]—very logical [9])
2. How confident are you that this treatment will be successful in reducing your headache symptoms if you were to have approximately eight such treatments over the course of 2 months? (Not at all confident [0]—very confident [9])
3. How confident would you be in recommending this treatment to a friend who has a problem with headaches? (Not at all confident [0]—very confident [9])
4. How competent do you consider the therapist who gave you treatment to be? (Not at all competent [0]—very competent [9])
Results
Sixty-five (65) of 69 randomized subjects completed the credibility/expectancy instrument. Subjects were predominantly white, female, and college educated. The mean age in the CST group was 42.9 and that in the LSSM group was 41; ages ranged from 12 to 71 years in the CST group (Table 2).
Using a 0–9 rating scale, the mean score for perceived logicality of treatment (question 1) was significantly less for LSSM (5.03, SD 2.34) compared to the CST group (6.64, SD 2.19), p=0.005. Although subjects' confidence that migraine would improve (question 2) was greater for CST (5.94, SD 2.01) than for LSSM (4.9, SD 2.21), this difference was not statistically significant (p=0.06). In response to question 3, significantly more subjects receiving CST (6.08, SD 2.27) would confidently recommend treatment to a friend than those receiving LSSM (4.69, SD 2.49), p=0.03 (Table 3). On the other hand, subjects from both groups were equally and strongly positive about the competence of the therapist (question 4), with no between-group differences (8.41, SD 0.95 versus 8.31, SD 1.09), p=0.815 on the Wilcoxon sum rank test. The withdrawal/dropout rate was very similar between the groups (11.1% for CST and 15.2% for LSSM [p=0.62]).
Table 3.
Comparison of Mean Credibility Scores by Treatment Type: CranioSacral Therapy for Migraine
| Survey items | Magnet therapy (N=29) Mean (SD) | CranioSacral therapy (N=36) Mean (SD) | p-Valuea |
|---|---|---|---|
| 1. Therapy is logical | 5.03 (2.34) | 6.64 (2.19) | 0.005 |
| 2. Confident in success | 4.90 (2.21) | 5.94 (2.01) | 0.062 |
| 3. Willing to recommend to a friend | 4.69 (2.49) | 6.08 (2.27) | 0.029 |
| 4. Therapist is competent | 8.41 (0.95) | 8.31 (1.09) | 0.815 |
Based on Wilcoxon two-sample, two-sided test.
SD, standard deviation.
Upon examining individual responses, it was noted that scores for some subjects—1 in the CST group and 4 in the magnet group—differed dramatically from the norm. These individuals had responded with a 0 or 1 for every item, except confidence in the therapist, indicating a complete lack of confidence in the proposed treatment. When the data from these five outliers were removed, the only significant difference remaining between LSSM and CST on any of the items was in logicalness of therapy (Table 4).
Table 4.
Comparison of Mean Credibility Scores by Treatment Type: CranioSacral and Magnet Therapy for Migraine with Removal of Outliers (>1 SD)
| Survey items | Magnet therapy (N=25) Mean (SD) | CranioSacral therapy (N=35) Mean (SD) | p-Valuea |
|---|---|---|---|
| 1. Therapy is logical | 5.54 (1.88) | 7.03 (1.51) | 0.004 |
| 2. Confident in success | 5.56 (1.53) | 6.11 (1.76) | 0.200 |
| 3. Willing to recommend to a friend | 5.36 (1.96) | 6.25 (2.05) | 0.095 |
| 4. Therapist is competent | 8.44 (0.96) | 8.40 (0.95) | 0.815 |
Based on Wilcoxon two-sample, two-sided test.
SD, standard deviation.
Discussion
Study participants in the CST and LSSM groups responded significantly differently in terms of treatment credibility and expectancy of benefit. Removal from the analysis of outlier data from those subjects in either group who perceived that their treatment had no credibility and expressed no confidence in it (1 in the CST group and 4 in the LSSM group) revealed that the only remaining significant difference between LSSM and CST was in the logicality of the procedure.
Since the credibility/expectancy scores diverged significantly between the CST and LSSM groups, and since beliefs about logicality and expectation of benefit have been known to influence outcomes, it was important to explore and identify possible factors in the management and implementation of this feasibility study that may have contributed to differences in credibility scores between the CST and LSSM treatments, as follows: (1) Was there any bias in recruiting subjects and explaining the protocols? (2) Was the design or execution of the LSSM protocol less than optimal? (3) Was the assessment of credibility flawed in terms of validity or timing?23,27 (4) How credible were either of the interventions?
These questions are addressed below.
-
1. Possible bias in recruiting subjects and explaining the protocols. At recruitment, and on the first treatment visit, subjects may have received inadequate information or may not have clearly understood the rationale of one or both interventions. The degree of understanding was assessed verbally by the therapist at the recruitment and first treatment visit but not measured quantitatively. Horvath reported that treatment expectancy was closely linked to the amount and quality of information presented to subjects as part of explaining therapeutic rationales.28 A communication disparity between CST and LSSM groups might have adversely affected the credibility score of LSSM. In a future study, this possible disparity could be remedied by applying a survey instrument to test understanding and knowledge.
In retrospect, there were subtle biases toward promoting CST in the recruitment and consent materials, such as describing the therapist as highly experienced in CST but not giving an equivalent statement for her skills with LSSM; and placing CST description text first in the consent and informational materials, possibly emphasizing its relative importance. Also, all subjects were treated in the CST therapist's office, which was located in a holistic health treatment facility that offered CST. Flyers available in the waiting area regarding CST, while not related to the study, may have introduced bias in the participants, since information about LSSM was available only in the treatment room.29
2. LSSM protocol: Possible flaws and solutions. Several factors may have limited the credibility of the LSSM protocol and could be improved in a subsequent study: (1) The magnets were located in Velcro pockets, created by a local seamstress, and may not have had the same cachet as the use of commercially marketed magnet products. (2) The therapist, an expert in CST, had no prior experience with magnet therapy and may have been subconsciously biased against giving this form of treatment. Thus, hiring a separate therapist who used magnets regularly in a CAM practice might have added to the credibility of the intervention. (3) Also, blinding the therapist to the relative activity of the magnets might have increased her own belief in magnet capability, and her belief could have been passed on to subjects. (4) Moreover, the therapist reported that some subjects mentioned to her that they had been especially attracted to the study by the opportunity to receive CST and were disappointed when they found that they were assigned to the LSSM group.
-
3. Possible flaws in use of credibility instrument. The use or timing of the credibility instrument may not have been optimal. (1) The credibility instrument was modified, as was done in previous studies, but was not revalidated. It is unclear whether the modified instrument remains entirely valid. It has become common practice to administer the credibility instrument after the first exposure to the treatment. Would other timing be more useful? Or should the expectancy question have been asked immediately after randomization? (2) Should the credibility questionnaire have been re-administered at the end of the treatment period? (3) From the data and careful review of the study design and trajectory, several problems were identified that probably influenced the credibility and expectancy scores.
The time point during the study at which these beliefs are measured may be important. Martin et al. reported that although valid expectancies of treatment can often be derived from patient perceptions before therapy begins, these beliefs can sometimes change quickly after the first treatment experience.28,30 In the current study, the credibility data were obtained just before the second treatment, in keeping with current thinking about appropriate timing of expectancy measures; but timing can affect response validity. For example, although question 3 in the credibility instrument asks the subject to score his/her confidence in recommending the modality to a friend, in this study the question was asked after only one treatment session. Hence, subject response would have been more likely the result of guesswork than derived from a thorough experience with the intervention. Currently, there is no general agreement in the literature on when and how often credibility and expectancy measures should be undertaken.
Although data from the credibility surveys showed that LSSM therapy was less credible than CST with diminished expectancy of improved outcome, there are some concerns that the instrument may not be measuring what has been claimed for it.23,28 Although labeled a “credibility” instrument, the second and third questions in this assessment tool deal with treatment expectancy. Given the fact that, over time, Borkovec and Nau's instrument has been modified and adapted in terms of questions and type of scale with little further validation, it would be useful to re-assess the constructs of the instrument with particular reference to complementary therapies.
It is interesting that the dropout rate during treatment was not significantly different between the groups. A high subject dropout rate would have been expected for a CAM therapy that lacked credibility and generated low expectations of success. Second, some validation of the LSSM control in terms of producing similar expectancy and placebo effects to CST comes from the high ratings of the procedural competence of the therapist by both study groups. Rating the therapist highly would not fit easily with the perception that they were receiving illogical treatment and had low expectations of improvement.
-
4. Credibility of either intervention. Apart from the high positive scores regarding the competence of the therapist, overall expectancy scores in this study were only in the moderate range of the scale. Goossens et al. reported similar findings of moderate expectancy scores in their study of behavioral interventions in chronic pain,28 suggesting that patients suffering from a chronic problem might well have low expectations and credibility because of previous disappointments. It is possible that many migraine subjects in this study fell into this chronic symptom category. However, this result may have been influenced by the fact that the questionnaire was given to the subject by the therapist just before the second intervention session.
Second, the often lackluster medical experience of migraine sufferers might produce a degree of skepticism and reticence toward the claims of benefit for either CST or LSSM made during recruitment. Thus, it might be useful in the future to probe responses to such credibility surveys in more detail to explore why subjects do, or do not, believe in the potential efficacy of any therapies they are receiving.
Conclusions
While several design and implementation factors may have contributed to the observed differences, LSSM did not achieve comparable levels of credibility and expectancy to CST. Valuable information has been gained that will assist with interpretation of outcomes, for which analysis is under way, and that will improve the design and execution of a future clinical trial. First, the authors have developed and tested a popular CAM therapeutic modality, CST, with a population of patients with migraine headache and found that it is at least moderately credible as an intervention. Second, the authors have developed and tested the feasibility of using a novel attention-control intervention, LSSM, gaining important information about possible improvements in design and implementation of future studies. Finally, an improved attention-control strategy could offer a viable attention-control methodology for research on CAM interventions in which establishing a rigorously mimicked control group is required but problematic.
Future Directions
Future research will focus on incorporating changes in design of the LSSM intervention, based on the above findings. If credibility/expectancy equivalence is established, the authors will proceed to test the effectiveness of CST in migraine using a larger study population. In addition, it is planned to revisit the construct and validity of measuring credibility as it applies to CAM interventions.
Appendix: Protocol for CranioSacral Therapy
Acknowledgments
The authors gratefully acknowledge funding support for this trial from the National Institutes of Health, Center for Complementary and Alternative Medicine Grant #5 R21 AT002750-02. This research is supported in part by a grant (RR00046) from the General Clinical Research Centers program of the Division of Research Resources, National Institutes of Health. The authors would also like to thank Laurel Wilkinson, RN, LMBT for delivering both interventions and helping to define the treatment protocols. We wish to thank Gloria Suarez, Christine Meyer, Nicholas Scott, Paula Umstead, and Stuart Scott for their research assistance.
Disclosure Statement
There were competing financial interests.
References
- 1.Lewith GTJWB. Clinical Research in Complementary Therapies: Principles, Problems and Solutions. Edinburgh, New York: Churchill Livingstone; 2002. [Google Scholar]
- 2.Turner JA. Deyo RA. Loeser JD, et al. The importance of placebo effects in pain treatment and research. JAMA. 1994;271:1609–1614. [PubMed] [Google Scholar]
- 3.Price DD. Finniss DG. Benedetti F. A comprehensive review of the placebo effect: Recent advances and current thought. Annu Rev Psychol. 2008;59:565–590. doi: 10.1146/annurev.psych.59.113006.095941. [DOI] [PubMed] [Google Scholar]
- 4.Mondloch MV. Cole DC. Frank JW. Does how you do depend on how you think you'll do? A systematic review of the evidence for a relation between patients' recovery expectations and health outcomes. CMAJ. 2001 Jul 24;165:174–179. [PMC free article] [PubMed] [Google Scholar]
- 5.Barron CJ. Moffett JA. Potter M. Patient expectations of physiotherapy: Definitions, concepts, and theories. Physiother Theory Practice. 2007;23:37–46. doi: 10.1080/09593980601147843. [DOI] [PubMed] [Google Scholar]
- 6.Whitehead WE. Control groups appropriate for behavioral interventions. Gastroenterology. 2004;126(suppl 1):S159–S163. doi: 10.1053/j.gastro.2003.10.038. [DOI] [PubMed] [Google Scholar]
- 7.Dorn SD. Kaptchuk TJ. Park JB, et al. A meta-analysis of the placebo response in complementary and alternative medicine trials of irritable bowel syndrome. Neurogastroenterol Motil. 2007;19:630–637. doi: 10.1111/j.1365-2982.2007.00937.x. [DOI] [PubMed] [Google Scholar]
- 8.Linde K. Witt CM. Streng A, et al. The impact of patient expectations on outcomes in four randomized controlled trials of acupuncture in patients with chronic pain. Pain. 2007;128:264–271. doi: 10.1016/j.pain.2006.12.006. [DOI] [PubMed] [Google Scholar]
- 9.Licciardone JC. Russo DP. Blinding protocols, treatment credibility, and expectancy: Methodologic issues in clinical trials of osteopathic manipulative treatment. J Am Osteopath Assoc. 2006;106:457–463. [PubMed] [Google Scholar]
- 10.Borkovec TD. Nau SD. Credibility of analogue therapy rationales. J Behav Ther Exp Psychiatry. 1972;3:257–260. [Google Scholar]
- 11.Upledger JE. Craniosacral therapy is an integral part of general osteopathic education and training: An approach to diagnosis and treatment. In: DiGiovanna EL, editor; Schiowitz S, editor. An Osteopathic Approach to Diagnosis and Treatment. 2nd. Philadelphia: Lippincott-Raven; 1997. pp. 126–140. [Google Scholar]
- 12.Kosinski M. Bayliss MS. Bjorner JB, et al. A six-item short-form survey for measuring headache impact: The HIT-6. Qual Life Res. 2003;12:963–974. doi: 10.1023/a:1026119331193. [DOI] [PubMed] [Google Scholar]
- 13.Stewart WF. Lipton RB. Dowson AJ. Sawyer J. Development and testing of the Migraine Disability Assessment (MIDAS) Questionnaire to assess headache-related disability. Neurology. 2001;56(suppl 1):S20–S28. doi: 10.1212/wnl.56.suppl_1.s20. [DOI] [PubMed] [Google Scholar]
- 14.McHorney CA. Ware JE., Jr Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Medical Care. 1993;31:247–263. doi: 10.1097/00005650-199303000-00006. [DOI] [PubMed] [Google Scholar]
- 15.Mann JD. Faurot KR. Wilkinson L, et al. Craniosacral therapy for migraine: Protocol development for an exploratory controlled clinical trial. BMC Complement Altern Med. 2008;8:28. doi: 10.1186/1472-6882-8-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hartman SE. Norton JM. Interexaminer reliability and cranial osteopathy. Sci Rev Altern Med. 2002;6:23–34. [Google Scholar]
- 17.Moran RW. Gibbons P. Intraexaminer and interexaminer reliability for palpation of the cranial rhythmic impulse at the head and sacrum. J Manipulative Physiol Therapeut. 2001;24:183–190. [PubMed] [Google Scholar]
- 18.Ernst E. Harkness E. Spinal manipulation: A systematic review of sham-controlled, double-blind, randomized clinical trials. J Pain Symptom Manage. 2001;22:879–889. doi: 10.1016/s0885-3924(01)00337-2. [DOI] [PubMed] [Google Scholar]
- 19.Hawk C. Azad A. Phongphua C. Long CR. Preliminary study of the effects of a placebo chiropractic treatment with sham adjustments. J Manipulative Physiol Therapeut. 1999;22:436–443. doi: 10.1016/s0161-4754(99)70031-x. [DOI] [PubMed] [Google Scholar]
- 20.Chang-zer H. Static magnetic influence on human nerve function. Arch Phys Med. 1987;68:162–164. [PubMed] [Google Scholar]
- 21.Ochsman JL. Clinical aspects of biological fields: An introduction for health care professionals. J Bodywork Mov Therap. 2002;6:117–125. [Google Scholar]
- 22.Wolsko PM. Eisenberg DM. Simon LS, et al. Double-blind placebo-controlled trial of static magnets for the treatment of osteoarthritis of the knee: Results of a pilot study. Altern Ther Health Med. 2004;10:36–43. [PubMed] [Google Scholar]
- 23.Borkovec TD. Nau SD. Credibility of analogue therapy rationales. J Behav Ther Exp Psychiatry. 1972;3:257–260. [Google Scholar]
- 24.Devilly GJ. Borkovec TD. Psychometric properties of the credibility/expectancy questionnaire. J Behav Ther Exp Psychiatry. 2000;31:73–86. doi: 10.1016/s0005-7916(00)00012-4. [DOI] [PubMed] [Google Scholar]
- 25.Vincent CA. Credibility assessments in trials of acupuncture. Comp Med Res. 1990;4:8–11. [Google Scholar]
- 26.Wood R. Lewith GT. The credibility of placebo controls in acupuncture studies. Complement Ther Med. 1998;6:79–82. [Google Scholar]
- 27.Birch S. Credibility of treatment in controlled trials of acupuncture. J Altern Complement Med. 1997;3:315–321. doi: 10.1089/acm.1997.3.315. [DOI] [PubMed] [Google Scholar]
- 28.Goossens ME. Vlaeyen JW. Hidding A, et al. Treatment expectancy affects the outcome of cognitive-behavioral interventions in chronic pain. Clin J Pain. 2005;21:18–26. doi: 10.1097/00002508-200501000-00003. discussion 69–72. [DOI] [PubMed] [Google Scholar]
- 29.Horvath P. Treatment expectancy as a function of the amount of information presented in therapeutic rationales. J Clin Psychol. 1990;46:636–642. doi: 10.1002/1097-4679(199009)46:5<636::aid-jclp2270460516>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 30.Martin PJ. Moore JE. Sterne AL. Lindsey CJ. Patients' expectancies and hospital outcome. J Clin Psychol. 1977;33:254–258. doi: 10.1002/1097-4679(197701)33:1+<254::aid-jclp2270330159>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]