Abstract
Mobile technologies are being used to deliver health behavior interventions. The study aims to determine how health behavior theories are applied to mobile interventions. This is a review of the theoretical basis and interactivity of mobile health behavior interventions. Many of the mobile health behavior interventions reviewed were predominately one way (i.e., mostly data input or informational output), but some have leveraged mobile technologies to provide just-in-time, interactive, and adaptive interventions. Most smoking and weight loss studies reported a theoretical basis for the mobile intervention, but most of the adherence and disease management studies did not. Mobile health behavior intervention development could benefit from greater application of health behavior theories. Current theories, however, appear inadequate to inform mobile intervention development as these interventions become more interactive and adaptive. Dynamic feedback system theories of health behavior can be developed utilizing longitudinal data from mobile devices and control systems engineering models.
Keywords: Mobile phones, Handheld computers, Health behavior interventions, Smoking cessation, Weight management, Adherence, Chronic disease management, Health behavior theory, Dynamical systems, Control systems engineering
The development, evaluation, and dissemination of computerized health behavior interventions have expanded rapidly in the last decade. Advances in Internet-based infrastructure and accessibility promoted the migration of computerized health behavior interventions from prototype stand-alone software to robust, scalable, interactive, and tailored web-based programs. As a result, web-based health behavior interventions have proliferated in recent years and appear to be an efficacious method for delivering health behavior interventions in a cost-effective manner [1–3].
The next evolution, or revolution, of computerized health interventions, mobile technology and health (mHealth), appears to be underway. Mobile phones have achieved rapid and high penetration. There are over 285 million wireless subscribers in the USA alone [4], and an estimated 67.6% of adults worldwide own cell phones [5]. Approximately 75% of US high school students own a mobile phone [6]. In contrast to the initial Internet digital divide which limited the reach of computerized health behavior interventions for those in lower socioeconomic groups, mobile phone use has been widely adopted across socioeconomic and demographic groups and appears greater among those populations most in need of these interventions [6, 7]. The penetration rates in developing countries, where wireless technologies have leapfrogged the wired computer infrastructure, have produced considerable excitement in the global health community to reach and follow individuals who were previously unreachable via traditional communication channels [8, 9].
Compared to Internet interventions delivered to desktop and laptop computers, mobile interventions have the capacity to interact with the individual with much greater frequency and in the context of the behavior. As sensing technologies integrated with the mobile phone via Bluetooth or other data transmission process continue to develop, health behavior change interventions can be delivered based not only on self-reports and time/location parameters but also on psychophysiological state, social context, activity level, and behavior patterns [10]. The availability of these rich, complex, and frequent data inputs provides the potential to deliver health behavior interventions tailored not only to the person’s baseline characteristics but also to his/her frequently changing behaviors and environmental contexts [11].
To better leverage the potential of mobile technologies for health behavior interventions, health behavior theories and models need to be able to guide the development of complex interventions that adapt rapidly over time in response to various inputs. Existing health behavior theories and models have served for many years as guides to intervention development and delivery, and these theories have been the basis not only for face-to-face counseling interventions but also mass media and social marketing efforts. Models such as the Health Belief Model [12], Theory of Planned Behavior [13], Social Cognitive Theory [14], the Transtheoretical Model [15], and Self-Determination Theory [16] have served as the basis for many of the eHealth web and desktop/laptop computer interventions and have informed how interventions can be tailored to the individual’s baseline status.
As intervention developers take full advantage of mobile technologies, health behavior models will be required to guide not only tailored adjustments at intervention initiation but also the dynamic process of frequent iterative intervention adjustments during the course of intervention. The content and timing of a specific mobile phone intervention delivered via voice, text, resident application, mobile web, or other modality can be driven by a range of variables including (a) the target behavior frequency, duration, or intensity; (b) the effect of prior interventions on the target behavior; and (c) the current context of the individual (time, location, social environment, psychophysiological state, etc.). Such interventions require health behavior models that have dynamic, regulatory system components to guide rapid intervention adaptation based on the individual’s current and past behavior and situational context. Some have argued that current health behavior models are inadequate even for low-tech interventions [17], but the predominately linear and static nature of these models severely limits their ability to guide the dynamic, adaptive interventions possible via mobile technologies.
To evaluate the theoretical basis and adaptive nature of mobile interventions, the current literature on mobile technology health behavior interventions was reviewed. For this review, we define “mobile technology” as computer devices that are intended to be always on and carried on the person throughout the day (i.e., during normal daily activities). Mobile phones are the prototype device within this space, and most of the interventions reviewed used mobile phone platforms, but precursors to current smart phones and text messaging systems such as personal digital assistants (PDAs) and two-way pagers also are consistent with this definition. Excluded from this definition are devices that are portable (e.g., laptops, netbooks, iPads) but are not intended to be carried on the person throughout the day. Although technically mobile, we also excluded interventions that involved phone-based counseling, whether live or by interactive voice response (IVR), that could be delivered similarly via landline (i.e., phone-based counseling via mobile phone). Prior to the advent and widespread use of multipurpose mobile devices, special purpose devices were developed for the delivery of health behavior interventions [18, 19], but these pioneering prototypes often lacked the portability, connectivity, input–output interface, and/or computing power of current multipurpose devices and are not included in this review. This review is also limited to the use of these mobile devices for delivering health behavior interventions, not assessments. There is a substantive literature on the use of mobile devices for health behavior assessment (e.g., ecological momentary assessment), and self-monitoring alone has been shown to be an effective health behavior intervention [20], but we excluded from this review mobile programs that involved assessment input only or that used mobile device output solely for the purpose of encouraging input (i.e., reinforcing recording adherence).
For this review, a Medline search of “mobile phone,” “cell phone,” “text messaging,” “personal digital assistant,” “PDA,” “palmtop,” “handheld computer,” and “pager” published through June 2010 was conducted. Articles meeting the definition described above were selected, and additional articles were identified from references of these initially selected articles. A considerable number of these articles were proof-of-concept reports that described technical development, an ongoing study, or reported only usability/satisfaction data. To insure review of fully functional mobile interventions, we narrowed the selection criteria to studies that reported some form of clinical outcome data, with or without randomized controlled conditions. Nearly all of the articles identified meeting these criteria fell into one of four major health behavior areas: smoking, weight loss (including diet and exercise interventions), treatment adherence (i.e., adherence to medical recommendations including both taking medication and attending appointments), and chronic disease management. Therefore, we limited this review to mobile health behavior interventions in these four areas. Others have reviewed subsets of the research reviewed here for the purposes of estimating effect sizes (e.g., [21, 22]). In contrast to meta-analytic reviews of effect size, the purpose of this review is to assess how theory has been employed in the development of mobile health behavior interventions and how the interactive and adaptive potential of these interventions may require new dynamic systems theories of health behavior.
REVIEW OF MOBILE HEALTH BEHAVIOR INTERVENTIONS
Smoking cessation
Seven studies were identified that used mobile technology to deliver smoking cessation interventions. In Table 1 and subsequent tables of the other three areas reviewed, we summarize for each study the basic study characteristics (e.g., sample, design), a brief description of the intervention, the theoretical basis of the intervention if reported, the interactivity of the intervention, and the primary outcome. For interactivity, we specify if the intervention output was adjusted based on input provided by the user, if this adjustment was manual (e.g., healthcare professional reviewed data and determined intervention output) or automatic (e.g., intervention output generated by computer algorithms), and if the adjustment occurred at intervention initiation (i.e., tailored or personalized based on initial assessment) or during the course of the intervention, or both. The concept of “just-in-time” of Intille et al. is used to characterize interventions that adjust based on data obtained during the course of the intervention [30]. As opposed to the term “real-time” which is commonly is used in the mobile assessment literature to denote input occurring at the time of a recording prompt or the behavior being monitored, mobile interventions are often lagged over minutes, hours, or days as sufficient data are obtained to adapt the intervention, hence the use of “just-in-time” to describe adaptations occurring during the course of the intervention.
Table 1.
Smoking cessation mobile intervention studies
| Reference | Study characteristics | Intervention description | Theoretical basis | Interactivity | Outcome |
|---|---|---|---|---|---|
| Obermayer et al. [23] | N = 46, age 18–25-year smokers; pre–post | SMS for managing urges timed and tailored to likely high-risk situations and to stage of change; additional messages provided by text request | Self-Regulation; Transtheoretical Model | Output auto-adjusted initially and just-in-time | Quit rate (bio-validated) of 17% at 6 weeks |
| Rodgers et al. [24] | N = 1,705 adult smokers; RCT of SMS messages vs. no treatment | SMS with motivational support, quit information, and distraction (general interest info); additional messages provided by text request | None reported | Output auto-adjusted initially and just-in-time | Quit rate of 28% for intervention vs. 13% for control at 6 weeks |
| Riley et al. [25] | N = 31, age 18–25-year smokers; pre–post | Same as Obermayer et al. [23] | Self-Regulation; Transtheoretical Model | Output auto-adjusted initially and just-in-time | Quit rate (bio-validated) of 42% at 6 weeks |
| Whittaker et al. [26] | N = 17, age 16–45-year smokers; pre–post | Videos of role model quitting experiences interspersed with SMS messages providing quitting assistance | Social Cognitive Theory; Social Marketing | Output auto-adjusted initially and just-in-time | Quit rate of 53% at 4 weeks |
| Brendryen and Kraft [27] | N = 396 adult smokers; RCT of intervention vs. self-help booklet | IVR and SMS messages as part of multi-channel smoking cessation intervention tailored to smoking status; most also received NRT | Self-Regulation; Social Cognitive Theory; Cognitive–Behavioral Model | Output auto-adjusted initially and just-in-time | Quit rate of 38% for intervention vs. 24% for self-help booklet at 12 months |
| Brendryen et al. [28] | N = 290 adult smokers; RCT of intervention vs. self-help booklet | Same as Brendryen and Kraft [27] | Self-Regulation; Social Cognitive Theory; Cognitive–Behavioral | Output auto-adjusted initially and just-in-time | Quit rate of 20% for intervention vs. 10% for self-help booklet at 12 months |
| Free et al. [29] | N = 200 adult smokers; RCT of intervention vs. generic text messages | Same as Rodgers et al. with SMS texts adapted for UK participants | None reported | Output auto-adjusted initially and just-in-time | Quit rate (bio-validated) of 8% for intervention vs. 6% for control at 6 months |
As shown in Table 1, the seven studies identified are from three research groups who developed and evaluated interventions delivered via mobile phone text messaging (aka short messaging service (SMS)). These interventions consisted primarily of text message output although Whittaker et al. [26] also delivered mobile videos of role models and their quitting experiences. All of the interventions were computer-tailored at treatment initiation. The intervention developed by Riley and colleagues [23, 25] tailored both content and timing of the text messages to the times users indicated via an associated Internet site that urges and high-risk situations were likely to occur. All of these interventions also adjusted just-in-time via text message requests from users for assistance which generated immediate return text messages with tips and strategies to manage urges or withdrawal. The Brendryen [27, 28] and Riley interventions [23, 25] also adjusted the intervention based on smoking status (e.g., different messages before vs. after quitting, resetting quit dates if relapse occurred).
With the exception of the Rodgers intervention [24, 29], these mobile smoking cessation interventions provided a theoretical basis, citing Social Cognitive Theory, Self-Regulation Theory, the Transtheoretical Model, and cognitive–behavioral theory. These theories primarily appear to have informed the content of the text messages which included skills to manage urges and the facilitation of social support. The Transtheoretical Model was used to adapt the content of the text messages to the preparation, action, and maintenance stages of the quit process. In a separate report, Brendryen and colleagues [31] provided a detailed description of the intervention mapping process for the development of the Happy Ending intervention based on Self-Regulation Theory, Social Cognitive Theory, cognitive–behavioral therapy, motivational interviewing, and relapse prevention. In a stepwise approach, they performed a needs assessment and devised proximal change objectives based on the self-observation, self-evaluation, and self-reaction processes of Self-Regulation Theory and the behavioral determinants posited by Social Cognitive Theory and related models. They generated theory-based methods and practical strategies to address these change objectives and developed the resulting intervention to deliver each of these strategies. This report provides a well-devised framework for the application of theory to a mobile health behavior intervention.
Quit rates from the interventions evaluated in these studies range from 8% [29] to 53% [26] with a follow-up period ranging from 4 weeks to 12 months. A recent Cochrane review of randomized studies of mobile phone-based interventions for smoking cessation, which included all of the randomized controlled trials (RCT) reviewed here, found a significant short-term increase in self-reported quitting (relative risk = 2.18; 95% confidence interval 1.80 to 2.65) but considerable heterogeneity and lack of sufficient evidence for long-term effects [32]. Although promising, the effects of mobile technologies for smoking cessation require more study, especially of the long-term effects of these interventions.
Weight loss, diet, and physical activity
We identified 12 studies reporting on mobile health behavior interventions for weight loss, diet, and/or physical activity. Four of these interventions were delivered via PDA, and eight were delivered via mobile phone, predominately SMS. These interventions represent a range of interactivity from non-tailored weekly informational text messages [33] to real-time diet and exercise monitoring with multiple daily customized messages based on input [34]. Most auto-adjusted the intervention based on computer algorithms, but the two interventions encouraging walking in Chronic Obstructive Pulmonary Disease (COPD) patients were manually adjusted by health professionals [35, 36]. The mobile weight loss program developed by Bauer et al. [37] computer-generated text messages based on weekly input from the overweight children in the study, but these messages were reviewed and modified by staff before sending. Diet, weight, and exercise data were provided via self-report for all interventions except the Hurling et al. [38] study which used accelerometer data wirelessly transmitted via Bluetooth to the mobile phone. Output from these interventions was predominately text although tabular and graphic comparisons to targets/goals were provided by some interventions (e.g., [34, 39, 40]) and one intervention used a mobile phone program that adjusted music tempo to encourage an appropriate walking pace [35].
Of the 12 studies summarized in Table 2, seven specified a theoretical basis for the mobile weight loss, diet, or physical activity intervention developed. Consistent with the more general weight loss intervention literature, Social Cognitive Theory was the primary theoretical basis for these interventions although the Theory of Planned Behavior was cited by one study [38]. In a well-controlled evaluation of a theoretically-based program, Haapala and colleagues [40] randomly assigned overweight adults to control or a mobile phone weight loss program. The intervention was based on Self-Efficacy Theory and a Systems Contingency Approach described by Hiltz [45] in which the amount, frequency, and type of computer-mediated communication are hypothesized to influence learning effectiveness. These theories were combined in a contingency model of mobile phone weight loss that combines program factors (e.g., content), frequency of interaction with the program, exogenous variables, and changes in processes and outcomes. Text messages instructed users in a staggered reduction of food intake and prompted daily weight reporting with immediate tailored feedback. The program evaluated weight balance, calculated daily energy requirement, set daily weight goals and food consumption recommendations, and provided feedback on the days remaining to the long-term weight target. Weight loss goals were user defined, but typically averaged 2 kg/month. Weight was reported via mobile phone on average 4.4 times per week. Compared to controls, those in the mobile phone intervention lost significantly more weight (4.5 vs. 1.1 kg) and had a greater reduction in waist circumference (6.3 vs. 2.4 cm) after 1 year in the program.
Table 2.
Weight loss (diet, physical activity) mobile intervention studies
| Reference | Study characteristics | Intervention description | Theoretical basis | Interactivity | Outcome |
|---|---|---|---|---|---|
| Joo and Kim, [33] | N = 927 adult public health center patients; pre–post | Weekly informational SMS messages regarding diet and exercise | None reported | Output not adjusted | Weight loss of 1.6 kg at 12 weeks |
| Hurling et al. [38] | N = 77 normal and overweight adults; RCT of intervention vs. exercise advice alone | Web-based program for managing perceived barriers and scheduling weekly exercise; reminders via email or SMS messaging; accelerometer data obtained and transmitted via mobile phone for real-time web feedback | Theory of Planned Behavior; Components of other theories | Output auto-adjusted initially | Physical activity increase of 12 MET min for intervention vs. 4 MET min for control at 9 weeks |
| Atienza et al. [41] | N = 36 healthy adults; RCT of intervention vs. print materials | PDA program assessing vegetable and whole grain intake and providing behavioral strategies to motivate changes to dietary intake | Self-Regulation Theory; Social Cognitive Theory | Output manually adjusted initially | Servings of vegetables or grain fiber per 1,000 kcal of 1 for intervention vs. 0 for controls at 8 weeks |
| King et al. [42] | N = 37, age ≥50 years underactive adults; RCT of intervention vs. print materials | PDA program assessing physical activities, vegetable and whole grain intake, and providing behavioral strategies to motivate changes to dietary intake | Self-Regulation Theory; Social Cognitive Theory | Output auto-adjusted initially and just-in-time | Increase of moderate + physical activity of 178 min/week for intervention vs. decrease of 80 min/week for control at 8 weeks |
| Beasley et al. [39] | N = 174 overweight or obese adults; RCT of intervention vs. paper diary | PDA dietary self-monitoring program with feedback compared to personalized targets for very low fat diet recommendations | None reported | Output auto-adjusted initially and just-in-time | Total fat intake decrease of 31 g/day for intervention vs. 22 g/day for control at 3 weeks |
| Liu et al. [35] | N = 48 adult COPD patients; RCT of intervention vs. no treatment | Music tempo delivered via mobile phone program adjusted based on ISWT to encourage a waking pace at 80% max effort | None reported | Output manually adjusted initially and just-in-time | ISWT distance increase of 68.4 m for intervention from baseline to 12 weeks |
| Nguyen et al. [36] | N = 17 adult COPD patients; RCT of mobile coached vs. mobile monitoring alone | Daily log via SMS of exercise and symptoms; Weekly SMS messages reinforcing logged exercise by nurse | None reported | Output manually adjusted just-in-time | Incremental cycle test change of +1.3 W for monitoring vs. −5.5 W for coached |
| Haapala et al. [40] | N = 125 overweight adults; RCT of intervention vs. no treatment | Contingency program via SMS that instructed users in a staggered reduction of food intake based on weight, daily energy requirements, and short- and long-term weight goals | Self-Efficacy Theory; Systems Contingency Approach | Output auto-adjusted initially and just-in-time | Weight loss of 4.5 kg for intervention vs. 1.1 kg for control at 12 months |
| Patrick et al. [43] | N = 65 overweight adults; RCT of intervention vs. print information | Tailored SMS messages that encouraged goal setting, self-monitoring, and addressed barriers to weight loss | None reported | Output auto-adjusted initially and just-in-time | Weight loss of 2.9 kg for intervention vs. 0.9 kg for print information at 4 months |
| Fjeldsoe et al. [44] | N = 88 postnatal women; RCT of intervention vs. initial behavioral counseling only | Tailored SMS messages encouraging physical activity sent 3–5 times per week provided in conjunction with two behavioral counseling sessions; weekly SMS goal check with response | Social Cognitive Theory | Output auto-adjusted initially and just-in-time | Walking for exercise duration increase of 6.7 min for intervention vs. 0.3 min for control at 13 weeks |
| Burke et al. [34] | N = 210 overweight or obese adults; RCT of PDA + tailored feedback, PDA monitoring, and paper-based monitoring | In addition to 20 group sessions over 6 months, PDA program of self-monitoring and summary output of dietary intake (same dietary monitoring program as Beasley et al. [39]) and exercise activity with or without custom tailored multiple daily messages based on input | Self-Regulation Theory | Output auto-adjusted initially and just-in-time | Weight loss of 6.5% for PDA + tailored feedback, 4.8% for PDA alone, and 4.6% for paper-based dietary monitoring at 6 months |
| Bauer et al. [37] | N = 40 overweight children; pre–post | Weekly text message questions on maintaining diet and physical activity following 12-week group intervention. Feedback based on responses provided reinforcement, promoted social support, reminded skills learned during treatment, and motivated participants (reviewed and modified by staff before sending) | Cognitive–Behavioral | Output (semi) auto-adjusted initially and just-in-time | BMI standard deviation score reduction of 0.07 from end of group intervention to 12 months |
ISWT Intermittent Shuttle Walk Test
As an example of interactivity in mobile weight management interventions, Patrick and colleagues [43] reported on a 4-month, randomized trial of a mobile phone text messaging program for weight loss that, although not specified, appeared consistent with Social Cognitive Theory and that involved considerable interactivity. Text messages were personalized and varied not only in content but also in their interactive nature. Some texts were simple push reminders while others queried the user about their dietary behavior, obtained a reply, and then provided an intervention based on the reply. Although weight loss in the text messaging condition was modest over 4 months (2.88 kg), it was significantly greater than in the print only condition.
In a recently published study, Burke et al. [34] provided another example of intervention interactivity via mobile device. They compared paper-based dietary and exercise monitoring to PDA-based monitoring and PDA-based monitoring plus daily feedback message in an RCT of 210 overweight and obese adults. The PDA monitoring program was based on the platform developed by Beasley et al. [39], but the PDA monitoring plus feedback condition added daily messages of positive reinforcement and guidance for goal attainment tailored to the input provided based on self-regulation theory. All three conditions also received 20 group intervention sessions over a 6-month period. Compared to the monitoring only conditions which obtained a percent weight loss of 4.8 (PDA) and 4.6 (paper-based), the PDA plus daily feedback condition obtained a mean percent weight loss of 6.5.
Consistent with other reviews [46], these initial studies of mobile interventions for weight loss show modest but significant weight loss and related outcomes. Mobile interventions for weight loss, diet, and physical activity are poised to take advantage of a number of advances in monitoring that could be leveraged to improve outcomes. Computerized dietary monitoring has been used extensively in this field [47], and these self-monitoring procedures have been adapted to mobile platforms. Recent research has begun to use cell phone cameras to assess dietary intake [48, 49] which may result in less underreporting of intake than from self-monitoring. As mobile phones increasingly incorporate accelerometers, the potential exists to use the automated data obtained from these accelerometers to monitor activity levels and provide just-in-time interventions [50, 51]. These richer and potentially more precise measures of dietary intake and physical activity can provide the basis for robust and interactive weight loss interventions delivered via mobile devices.
Treatment adherence
Ten studies were identified that evaluated the use of mobile technology to improve treatment adherence (Table 3). Of these, eight targeted medical appointment adherence and two addressed medication adherence, specifically HIV treatment adherence. All of the appointment adherence interventions were delivered via SMS while both of the medication adherence interventions were delivered via two-way pager. Given the substantial use of technology for measuring medication adherence [52] and the availability of smart pillboxes for improving adherence [53], it is surprising that only two studies have developed and evaluated a medication adherence intervention on a mobile platform, both using two-way pagers which have limited capabilities.
Table 3.
Adherence mobile intervention studies
| Reference | Study characteristics | Intervention description | Theoretical basis | Interactivity | Outcome |
|---|---|---|---|---|---|
| Safren et al. [54] | N = 82 HIV + patients; RCT of intervention vs. monitoring only | Tailored dose reminders via two-way pager, along with other reminders (e.g., meals, appointments) | None reported | Output manually adjusted initially | Dose adherence of 64% for intervention vs. 52% for control at 12 weeks |
| Bos et al. [57] | N = 343 orthodontic patients; nonrandomized comparison of text message, phone, mail, and no reminder | SMS appointment reminder | None reported | Output not adjusted | Appointment attendance of 90.6% for mail, 90.4% for phone, 82.4% for SMS, and 83.7% for no reminder over 3 weeks |
| Downer et al. [109] | N = 2,864 general medical outpatients with mobile phones; historic control of intervention vs. no reminder | SMS appointment reminder | None reported | Output not adjusted | Appointment adherence of 85.8% for intervention vs. 76.6% for control over 1 month |
| Downer et al. [110] | N = 45,110 general medical outpatients; historic control of intervention vs. no reminder | SMS appointment reminder | None reported | Output not adjusted | Appointment adherence of 90.2% for intervention vs. 80.5% for control over 3 months |
| Leong et al. [58] | N = 993 primary care outpatients; RCT of SMS, phone or no reminder | SMS appointment reminder | None reported | Output not adjusted | Appointment adherence of 59.6% for SMS, 59.0% for phone, and 48.1% for control over 3 months |
| Koshy et al. [56] | N = 9,512 ophthalmology outpatients; nonrandomized comparison of intervention vs. no reminder | SMS appointment reminder with ability to text reply to cancel appointment | None reported | Output not adjusted | Appointment adherence of 88.8% for SMS vs. 81.9% for control over 6 months |
| Chen et al. [59] | N = 1,859 preventive screening patients; RCT of SMS, phone or no reminder | SMS appointment reminder | None reported | Output not adjusted | Appointment adherence of 87.5% for SMS, 88.3% for phone, and 80.5% for control over 2 months |
| Simoni et al. [55] | N = 224 HIV + patients; RCT of pager + peer support, pager only, peer support only, or usual care | Tailored dose reminders via two-way pager along with educational, entertainment, and adherence assessment texts | None reported | Output manually adjusted initially | Dose adherence of 50.1% for pager + peer support, 41.8% for pager, 47.0% for peer support and 44.4% for usual care at 3 months |
| Foley et al. [111] | N = 276 pediatric dental patients; historical control of intervention vs. no reminder | SMS appointment reminder | None reported | Output not adjusted | Appointment adherence of 89.6% for SMS vs. 76.1% for control over 1 month |
| Da Costa et al. [112] | N = 7,890 general outpatient appointments; nonrandomized comparison of intervention vs. no reminder | SMS appointment reminder | None reported | Output not adjusted | Appointment adherence of 80.6% for SMS vs. 74.4% for control over 11 months |
In 2003, Safren and colleagues [54] published the earliest evaluation of a mobile technology identified in this review. In HIV patients with poor adherence, they used a commercial system (Medimom) to enter patients’ drug regimens and transmit pager alerts to remind patients to take their medications at the specified times. Based on electronic pill bottle data (MEMS), those randomly assigned to the pager reminder condition had significant improvements in medication adherence compared to those in a medication monitoring only condition at 2 and 12 weeks. In a more recent study, Simoni and colleagues [55] developed and evaluated a similar pager dosing reminder program for HIV patients with additional texts providing education, adherence assessments, and entertainment. This intervention, however, failed to produce significant improvements in adherence over the 9-month trial relative to usual care or peer support, possibly due to the mixed functions of the pager prompt (i.e., prompt taking medications, provide education). Neither study provided a theoretical basis for the intervention provided. Both studies tailored the intervention at initiation based on the medication regimen of each patient, but there were no adjustments made during the course of the intervention.
Among the eight studies providing appointment reminders via mobile technologies, all provided only a single, unadjusted output reminding the patient of their appointment, usually timed to within a few days of the scheduled appointment. The only two-way interaction was in the Koshy et al. study [56] which provided the patient with the ability to text reply to cancel the appointment. None of the studies provided a theoretical basis for the intervention provided.
Despite the simple nature of these appointment adherence interventions and their lack of interactivity and theoretical basis, most resulted in a significant increase in appointment adherence. The only exception was Bos et al. [57], which had high appointment adherence rates to orthodontic visits across conditions. It is important to note, however, that only two studies used randomized controls [58, 59]; the others used historical or nonrandomized controls. Additionally, the three studies that compared SMS to traditional phone call reminders found no difference between these two modalities [57–59].
Disease management
In addition to the treatment adherence research reviewed above, a number of treatment adherence interventions are incorporated within a chronic disease management program. The use of mobile phones for disease management has been substantially reviewed elsewhere [46, 60–62], particularly in the area of diabetes management. Based on the criteria for this review, we identified 20 studies: 16 in diabetes management, three in asthma management, and one in hypertension management (Table 4). Across the 20 studies, only one [63] specified a theoretical basis for the intervention, using Social Cognitive Theory to provide personalized SMS messages to support diabetes management in children with type 1 diabetes. In part, this lack of theoretical basis may reflect the well-established practice guidelines for managing type I and type 2 diabetes [64], but as the field extends these interventions beyond medication adjustments and integrates automated measures of physical activity, medication adherence, food intake, and other target variables into these systems [65], using health behavior theories to inform these interventions could improve outcomes.
Table 4.
Disease management mobile intervention studies
| Reference | Study characteristics | Intervention description | Theoretical basis | Interactivity | Outcome |
|---|---|---|---|---|---|
| Kwon et al. [113] | N = 185 adult diabetes patients; pre–post | Glucose readings recorded via SMS, reviewed by provider who sent recommendations via SMS | None reported | Output manually adjusted just-in-time | HbA1c decreased 7.5% to 7.0% at 3 months |
| Leu et al. [75] | N = 50 adult diabetes patients; RCT of pager reminders vs. routine care | Two-way pager reminders for various diabetes self-management activities (customized) | None reported | Output manually adjusted at baseline | HbA1c decreased 8.5% to 8.2% for intervention vs. 8.5% to 7.9% for controls at 3 to 6 months |
| Ostojic et al. [114] | N = 26 adult asthma patients; RCT of text vs. no text message recording | Daily SMS recording of peak flow reviewed by provider who sent weekly treatment adjustment messages via text | None reported | Output manually adjusted just-in-time | FEV1 increased from 77.63% to 81.25% for intervention vs. 78.88% to 78.25% for controls at 16 weeks |
| Kim et al. [115] | N = 42 adult type 2 diabetes patients; pre–post | SMS messages sent by providers based on review of data provided by patient via Internet | None reported | Output manually adjusted just-in-time | Fasting plasma glucose decreased from 174 to 145.4 m/dL at 12 weeks |
| Kim et al. [116] | N = 45 adult type 2 diabetes patients; pre–post | Same as Kim et al. [116] | None reported | Output manually adjusted just-in-time | HbA1c decreased 8.1% to 7.0% at 12 weeks |
| Franklin et al. [63] | N = 92, age 8–18-year type 1 diabetes patients; RCT of conventional insulin therapy, conventional therapy with SMS, and intensive therapy with SMS | Personalized daily SMS messages to support diabetes management | Social Cognitive Theory | Output auto-adjusted at initiation | HbA1c decreased 10.0 to 9.2 for intensive therapy + SMS; no change in other groups |
| Rami et al. [70] | N = 36, age 10–19-year type 1 diabetes patients; randomized crossover design of intervention vs. usual care paper diary recording | SMS recording of blood glucose, insulin dose, and carbohydrate intake with weekly feedback (automated if OK, generated by diabetologists if adjustments needed) | None reported | Output manually adjusted just-in-time | HbA1c change of 9.1% to 8.9% (intervention) to 9.2% (control); and 8.9% to 9.9% (control) to 8.9% (intervention) at 3 and 6 months |
| Ma et al. [66] | N = 15 adult type 2 diabetes patients; pre–post | PDA dietary monitoring with glycemic index feedback used to augment a six-contact diabetes management intervention | None reported | Output auto-adjusted just-in-time | HbA1c decrease from 8.0% to 7.5% at 6 months |
| Kim and Jeong, [117] | N = 51 adult diabetes patients; pre–post | Same as Kim et al. [115] | None reported | Output manually adjusted just-in-time | HbA1c decreased from 8.1% to 7.0% for intervention and 7.6% to 7.7% for control at 6 months |
| Benhamou et al. [118] | N = 30 adult type 1 diabetes patients; randomized crossover of SMS feedback vs. self-monitoring only | Providers acknowledged receipt of weekly transmitted glucose logs and provided recommendations | None reported | Output manually adjusted just-in-time | HbA1c change of 8.3% to 8.2% for intervention and 8.2% to 8.3% at 6 months |
| Forjuoh et al. [67] | N = 43 adult type 2 diabetes patients; pre–post | PDA recording of blood glucose, medications, meals, exercise, etc., with summary output | None reported | Output auto-adjusted just-in-time | HbA1c reduction from 9.7% to 8.0% at 6 months |
| Logan et al. [74] | N = 33 adult hypertensive type 2 diabetes patients; pre–post | Mobile phone obtained and transmitted BP measurements; summary data available and alerts sent to patients if BP out of range (take additional measures, contact physician) | None reported | Output auto-adjusted just-in-time | 24-h ambulatory systolic BP decreased from 141 to 132 over 2 weeks |
| Quinn et al. [71] | N = 30 type 2 diabetes patients; RCT of automated glucose transmission via phone vs. faxing or calling in glucose logs every 2 weeks | Mobile phone wirelessly obtained and transmitted glucose readings with real-time feedback and lifestyle recommendations provided via mobile phone application | None reported | Output auto-adjusted initially and just-in-time | HbA1c decrease of 9.51% to 7.48% for intervention vs. 9.05% to 8.37% at 3 months |
| Yoon et al. [119] | N = 51; RCT of intervention vs. usual care | Same as Kim et al. [115] | None reported | Output manually adjusted just-in-time | HbA1c change of 8.09% to 6.77% for intervention vs. 7.59 to 8.40 for control at 12 months |
| Newton et al. [120] | N = 78, age 11–18-year diabetes patients; RCT of mobile intervention vs. usual care | Weekly SMS reminders to wear pedometer and be active | None reported | Output not adjusted | Median step count decreased by 22 steps for intervention vs. 840 steps for control at 12 weeks |
| Turner et al. [72] | N = 23 type 2 diabetes patients; pre–post | Mobile phone wirelessly obtained and transmitted glucose readings; real-time feedback of input and semi-automated messages for self-management | None reported | Output auto-adjusted initially and just-in-time | HbA1c decrease from 9.5% to 9.0% at 3 months |
| Hanauer et al. [76] | N = 40, age 12–25-year diabetes patients; RCT of SMS vs. email reminders | Customized schedule for SMS reminders to obtain blood glucose readings. Reading submitted via SMS resulted in positive feedback if in range, and instructions if out of range | None reported | Output auto-adjusted initially and just-in-time | HbA1c change of 8.8% to 8.7% for intervention and 8.6% to 8.8% for control at 3 months |
| Cho et al. [73] | N = 69 type 2 diabetes patients; RCT of phone vs. internet diabetes monitoring and management | Combination mobile phone and glucometer transmitting glucose reading to provider who sent treatment adjustments via SMS | None reported | Output manually adjusted just-in-time | HbA1c decrease of 8.3% to 7.1% for phone program and 7.6% to 6.9% for Internet program |
| Strandbygaard et al. [77] | N = 54 adult asthma patients; RCT of SMS vs. no SMS | Daily SMS reminder to take asthma medication | None reported | Output not adjusted | Inhaler dose adherence from 77.9% to 81.5% for intervention vs. 84.2% to 70.1% for control at 12 weeks |
| Prabhakaran et al. [121] | N = 120 adult asthma patients; RCT of SMS vs. no SMS | Daily × 2 weeks, then weekly SMS messages to obtain symptom and medication adherence data; weekly SMS feedback on progress | None reported | Output auto-adjusted initially and just-in-time | Asthma Control Test improvement (to score ≥20) in 62% of SMS vs. 49% of controls |
BP blood pressure
The interventions developed and evaluated in these studies focused primarily on patient input (e.g., blood glucose readings, insulin doses, carbohydrate intake, exercise, forced expiratory volume (FEV1), or blood pressure) which were reviewed by a health professional to provide periodic regimen adjustments and treatment recommendations. Therefore, except for the two PDA interventions that did not transfer data to a central server [66, 67], any just-in-time intervention adjustments were made manually. These manually adjusted interventions are consistent with telemedicine models, but they have limited scalability due to the provider burden required to review and deliver these interventions. Lanzola and colleagues have proposed a multi-tier intervention model in which lower-tier disease management interventions are provided via automated treatment algorithms and higher tier interventions involving the healthcare provider occur only if the lower-tier interventions are ineffective [68].
Although advances in automating disease management intervention output are needed, the field is leveraging advances in objective, real-time input. Data entry burden is a persistent problem in disease management [69]. In one study of adolescents on intensified insulin therapy, one quarter failed to send at least 50% of their four daily blood glucose values [70]. With the advent of Bluetooth-enabled glucometers, data entry burden is eliminated. Since 2008, three of the studies reviewed used this or similar technology and found significant reductions in HbA1c [71–73]. Another study used Bluetooth-enabled blood pressure devices to provide automated transmission for hypertension control in diabetes patients [74].
Although the automatic transmission of testing data eliminates data entry burden, it does not eliminate the responsibility of the patient to perform regular testing, and a number of the studies used reminders via pager or mobile phone SMS to obtain blood glucose [72, 75, 76] or to take medications [77]. For example, Turner and colleagues provided blood glucose measurement reminders in an interactive manner with type 2 diabetes patients [72]. If no blood glucose data were automatically transmitted for 3 days, or if hypo- or hyper-glycemia persisted, patients received additional reminders.
Outcomes from the mobile disease management studies were generally positive and statistically significant. Among the 12 diabetes management studies with HbA1c as a primary outcome, ten found significant reductions in HbA1c. This is consistent with a recent systematic review of mobile phone use for diabetes self-management in which nine of ten studies reviewed reported significant improvement in HbA1c [46]. All three mobile asthma management interventions found significant improvements in the primary outcome. For example, in a small randomized controlled trial of no SMS vs. SMS daily reminders to take asthma medication, Strandbygaard et al. [77] found that the percent adherence based on objective inhaler dose counts decreased in the control condition (84.2% to 70.1%) but increased in the intervention condition (77.9% to 81.5%) over the 12-week study period. Therefore, the ability of mobile disease management programs to assess patient status frequently and adjust treatment remotely appears to improve treatment outcomes and to serve as a basis for more comprehensive and automated mobile disease management interventions.
SUMMARY OF MOBILE HEALTH BEHAVIOR INTERVENTION FEATURES
The application of mobile technologies to health behavior interventions is a nascent but rapidly growing field that has only begun to leverage the full capabilities of mobile phones and other mobile technologies. Most of the mobile interventions described in this review used text messaging (aka SMS) functionality of mobile phones. Text messages can be delivered simply and inexpensively across mobile phone operating platforms and to a large percentage of mobile phone users given the ubiquitous nature of this feature even on “less smart” mobile phones. As smart phone penetration rates increase and interoperability between operating platforms improves, however, additional features of mobile phones can be used.
In addition to voice, text, and data inputs, researchers have begun to use video input via camera features on these phones. Although video input has been primarily used for telemedicine purposes [78, 79], health behavior researchers have begun to use cameras for dietary assessment [48]. Another significant set of input features are automated sensors, either resident on the smartphone (e.g., accelerometers and GPS) or connected via Bluetooth. Much of the mobile health behavior interventions to date have focused on transmitting data from glucometers and spirometers, but an expanding variety of sensor technologies can be used to assess physiological states, movement, location, and other variables using mobile phones.
These early mobile health behavior interventions also have only begun to leverage the output functionality of these phones. As with input, most of the output delivery to date has been via text messaging. A few studies have used other output functions such as audio (e.g., [35]) or video (e.g. [26]), but device-resident or wireless Internet applications on smartphones provide a rich array of possible data and display outputs (e.g., progress charts, animation, videos, games) that could be used to deliver health behavior interventions.
Most apparent from this review, however, is the limited use of the rapid two-way interaction of inputs and outputs that could be used to deliver just-in-time health behavior interventions. Disease management and weight loss mobile health interventions have relied predominately on input while adherence and smoking cessation mobile health interventions have relied predominately on output. Among applications relying on input, many employed a user-initiated or unprompted input procedure despite a considerable ecological momentary assessment literature supporting the use of prompted inputs [80]. Following input, some applications provided tailored intervention responses, but others failed to deliver even a confirmation message, despite the potential importance of this feature for encouraging continued input. Of the applications that predominately pushed out intervention messages, a few encouraged confirmation of receipt or some other reply response (e.g., [43]), but most did not. None of the adherence interventions made just-in-time adjustments, but most of these interventions were single prompt appointment reminders with no longitudinal basis for adjustment, and none obtained the input necessary to make treatment adjustments. Most of the smoking and weight loss mobile interventions provided some form of “just-in-time” response based on a prior input, but the frequency or intensity of interactivity varied substantially among these interventions from requests for additional text message assistance common among the smoking interventions (e.g., [23, 27]) to regular intervention adjustments based on dietary and exercise inputs [34, 43]. The disease management interventions also typically provided just-in-time intervention adjustments, but most relied on manual adjustments by a health care professional to do so. Although more complex intervention adjustments might be best reserved for health professional judgment, standard treatment algorithms can be used to automate, with 100% treatment fidelity, many of these treatment adjustments, greatly improving scalability, and reducing professional time and costs.
Given the lag between intervention development, evaluation, and eventual publication, the articles reviewed, although published as recently as the June 2010, describe interventions developed a number of years ago. Therefore, the limited interactivity of the mobile interventions reviewed may not reflect current status, and the National Institutes of Health currently funds a number of ongoing projects that use more intensive interactivity and just-in-time interventions than described in this review [81]. To insure that the mobile interventions reviewed were mature enough for actual use, we limited our review to studies that subjected these interventions to some form of clinical outcome assessment. As a result, we did not report on recent mobile intervention development from proof-of-concept (e.g., [82]), usability/feasibility (e.g., [83]), or ongoing research reports (e.g., [84]) in which more recently developed interventions are described. Given the recent interest in and rapid progression of mHealth interventions, reports on more intensively interactive mobile health behavior interventions are likely to be published in the coming years.
THEORETICAL BASIS FOR MOBILE HEALTH BEHAVIOR INTERVENTIONS AND NEW DIRECTIONS
Our review of the studies of health behavior interventions delivered via mobile technologies reveals a paucity of discussion regarding the health behavior theories or models that provide the basis of the intervention. Even among those studies that provided a theoretical basis, very few attempted to evaluate any of the theoretical components hypothesized to be affected by the intervention. Studies in the smoking and weight loss areas tended to use a theoretical model for their intervention, drawing predominately from Social Cognitive Theory or its variants (e.g., self-efficacy). Among these studies are extensive and thoughtful examples of using theory to guide mobile intervention development (e.g., [31, 40]). In contrast, most of the mobile interventions studied in the treatment adherence and disease management areas did not report a theoretical basis for intervention development, but this may be the result of reliance on evidence based clinical guidelines (e.g., diabetes management) or on the simplicity of the intervention delivered (e.g., appointment reminders).
A simple reminder intervention, however, is an excellent example for the necessity of theory to guide intervention. Text messaging reminders to attend appointments, take medications, exercise, etc. appear relatively straightforward and are consistent with the “cue to action” component of many health behavior theories, but the history of health behavior theories cautions us about assuming that behavior change is straightforward or that innovative modes of delivery alone are sufficient to produce behavior change. In the 1950s, mobile neighborhood tuberculosis screenings were innovative, but the added salience and convenience did not substantially increase screenings. Researchers studying uptake of these neighborhood screenings learned that the perceived threat (severity and susceptibility) of tuberculosis, the perceived benefit of being screened, and the perceived barriers to getting screened contributed to a person obtaining these screenings. These findings led to the Health Belief Model [85] and the various health behavior theories and models that followed. Therefore, a greater reliance on health behavior theories to guide mobile technology intervention development, even for apparently simple interventions, should result in interventions that address more comprehensively the potential mechanisms of behavior change, resulting in more effective interventions.
While mobile technology applications of health behavior interventions should be guided by our current health behavior models, it is important to acknowledge that these current models appear inadequate to answer many of the intervention development questions likely to arise as interventions better leverage the interactive capabilities of mobile technologies. Some have argued that these theories are inadequate even for traditional interventions [17], but they are particularly limited at informing just-in-time intervention adaptations. Dunton and Atienza have noted that the increasing availability of time-intensive information (i.e., longitudinal data obtained at an intensive frequency) allows for the intra-individual tailoring of interventions but that current health behavior theories are based on delineating between, not within-person differences [86]. Boorsboom and colleagues have argued that between-person theories do not imply, test, or support causal accounts valid at the individual level [87]. As a result, these theories and models have been used with considerable success to tailor health behavior interventions based on pre-intervention factors, but typically have not been used to adapt the intervention to the individual over the course of the intervention [88, 89]. As these interventions become deliverable on mobile devices, the content of interventions can be adapted for each individual not only initially but also over time based on his/her prior outcome data, prior responses to specific intervention outputs, current environmental and/or social context, and a range of other variables that might influence the optimal intervention based on the current state of the individual (i.e., ecological momentary interventions) [90].
In addition to adapting the content of the intervention over time, mobile technology applications of health behavior interventions also have the ability to adapt the timing of the interventions based on these same data. For example, following a prompt to exercise, how long should the program wait before prompting again and how should the timing and content of the follow-up prompt be tailored based on prior pattern of responses to prompts? In this review, only a few studies adjusted the timing of the interventions, usually during the transition from behavior change to maintenance (e.g., [23, 40]), but these timing adjustments were set a priori across all participants and were not dynamically determined at the individual level.
The development of time-intensive, interactive, and adaptive health behavior interventions via mobile technologies demands more intra-individual dynamic regulatory processes than represented in our current health behavior theories. These theories do not preclude the possibility that some conceptual components change over time, and some concepts such as reciprocal determinism in Social Cognitive Theory are explicitly dynamic in nature [14]. Moreover, a rich behavior change process–outcome literature describes dynamic interactions in face-to-face behavioral interventions that could be applied to behavioral interventions via mobile technologies [91]. Adoption of dynamical system models for mobile health behavior interventions does not require that our current health behavior theories and models be discarded, but the predominately static, linear nature of these theories appears to be a poor fit with the intra-individual dynamics of future mobile technology interventions.
Control systems engineering [92] may provide the dynamical system models needed to transform our current health behavior theories into the dynamic theories required for the time-intensive, interactive, and adaptive health behavior interventions delivered via mobile technologies. Control systems engineering examines how to influence dynamical systems to achieve a desired outcome. These dynamical systems are multivariate, time-varying processes, often nonlinear in nature, in which variables that can be manipulated (e.g., system input variables) lead to changes in outcomes of interest (e.g., system output variables) adjusting for exogenous effects (e.g., disturbance variables). Control engineering approaches have been proposed for adaptive interventions to determine, for example, when and how much to change the frequency of family counseling to prevent the development of conduct disorder in children [93].
There are a number of practical advantages of using dynamical systems to inform adaptive, time-intensive interventions delivered via mobile technologies. Control systems engineering principles and procedures are mature and provide a robust computational framework for modeling, simulation, and systematic decision making over time. These control system principles and procedures fit well with the rich longitudinal data and real-time intervention adaptations potentially available via mobile technologies. Interventions based on theories enriched by control system models also provide engineers and health behavior researchers with a common language for collaborating on new interventions delivered via mobile technologies [94].
Perhaps more importantly, these feedback control systems have the potential to reshape health behavior theories and improve our understanding of human behavior. Feedback regulatory processes are core to neurobiology. Basic neuronal processes are time-intensive, adaptive interactions of excitatory and inhibitory synaptic processes that have been modeled at the single neuron level [95]. The communalities between brain circuitry and control system engineering principles are so compelling that some brain processes are described via engineering feedback systems (e.g., [96]). Since the brain appears to regulate itself and other organs using feedback control processes, it seems reasonable that the brain also regulates human behavior via similar feedback control processes. Optimal feedback control systems have been applied to basic sensorimotor control [97] and to reinforcement learning models [98]. Therefore, the application of feedback control systems to current health behavior theory concepts provides not only potential theoretical models that are amenable to the time-intensive, interactive nature of mobile health behavior interventions but also theoretical models that are more consistent with the putative neurobiological and environmental processes that regulate these behaviors.
One significant example of regulatory feedback for disease management processes is in diabetes where frequent adjustments to diet and insulin dose are determined based on blood glucose levels. Control engineering approaches have been applied to the glucose–insulin closed-loop system [99], and this application illustrates the potential of this approach to produce the desired outcome in systems that possess measurement error, model uncertainty, noise, and lagged effects. This work could serve as a basis for developing mobile technologies for diabetes management that take advantage of advanced closed-loop control system models to automate and better regulate blood glucose for insulin-dependent patients.
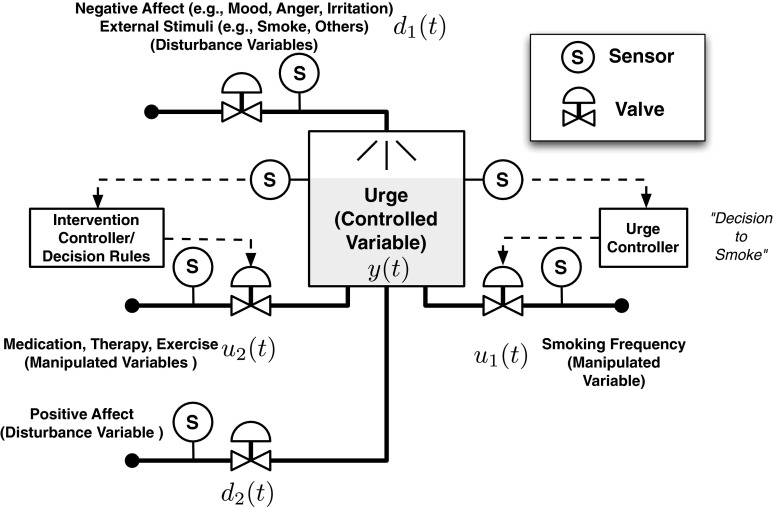
Detailed descriptions of applications of control systems engineering to other health behavior interventions such as substance use have been described elsewhere [93, 100], but to illustrate the application of control systems engineering to mobile health behavior interventions, we provide a simple model for intervening on smoking urges depicted in Fig. 1 which represents an individual’s smoking behavior in terms of a production–inventory model [101]. Using a fluid analogy, smoking urge is accumulated as an inventory that is built up by an “inflow” of negative emotional stimuli (e.g., sadness, irritation) and external stimuli (e.g., presence of others smoking, drinking coffee) and depleted by an urge “outflow” resulting from smoking events and the salutary effects of positive affect and dosages of intervention components such as medications and psychosocial interventions. In a control systems conceptualization, smoking urge (y(t)) is the controlled variable, while smoking activity represents a manipulated variable (u1(t)) whose action serves to reduce the urge to smoke. Environmental stimuli and positive and negative affect represent external disturbance variables (d1(t), d2(t)) whose changes build up or deplete the smoking urge inventory. The dose of intervention components represents additional manipulated variables (u2(t)) that can be selected adaptively by a set of decision rules or mathematical algorithms (referred to as the intervention controller in Fig. 1) based on assessed participant response. A differential equation drawn from the general principle of conservation of matter can be used to describe the relationship between these variables [102]
 |
where Kd1, Kd2, Ku1, and Ku2 represent coefficients that quantify the rate of change in urge based on changes in manipulated variables (intervention dosages, smoking activity) and disturbance variables (negative and positive affect, environmental stimuli). The inherent dynamics of smoking behavior in Fig. 1 constitutes a closed-loop feedback system in which increases in smoking urge precipitate a decision to smoke (the relationship between urge and smoking activity is denoted by the “urge controller” box in Fig. 1).
Fig. 1.
Illustration of control systems dynamical model for smoking urge
The potential of mobile technologies to generate the intensive longitudinal data sets reflecting the behavior of a smoker over time and observed in different settings and contexts is important for building a dynamical system model such as the individual smoking behavior model illustrated above. Mobile devices can collect information in real time about the controlled, manipulated, and disturbance variables, as represented by sensor locations in Fig. 1. Model estimation techniques such as system identification [103] and functional data analysis [104] can be used to estimate the Kd1, Kd2, Ku1, and Ku2 coefficients from these data. These modeling techniques also can be applied to reverse-engineer the functional relationship underlying the urge controller which reflects the actions of an individual smoker. With a dynamical systems model, it becomes possible to apply control systems engineering to develop algorithms that use real-time assessments and predicted responses from the model to adaptively decide on the timing and dose of the intervention components. Mobile technology is an enabler to advanced control algorithms such as model predictive control [105] that employ formal optimization methods to decide on current and future doses of intervention components while satisfying clinical practice preferences and restrictions [100]. The use of these control technologies in a smoking cessation intervention as shown in Fig. 1 parallels the closed-loop control system for diabetes management described previously. The optimization process leads to specific intervention decisions (u2(t)) for providing behavioral strategies and/or medication prompts to replace smoking as a means of reducing smoking urge.
In addition to being sensitive to threshold (or mean) levels of key variables, a control system framework can adapt to and consider variability of key controlling or explanatory variables. Most theories of health behavior change to date have focused on mean levels of predictive variables, but with the advent of newer data technologies, we can develop models that focus on lability or stability of key controlling factors. For many health behaviors, maintaining a stable level or tighter range for some key variables may be as or more important than increasing or decreasing mean levels.
Novel dynamic health behavior theories and their application to health behavior interventions via mobile technologies will require empirical validation. Adaptive treatment methodologies has been applied to interventions that adjust over the course of weeks or months, not hours or days, but these methodologies can be applied to mobile technology interventions [106]. Other methodological considerations for adaptive interactive technologies applied to eHealth also may be appropriate to consider for mHealth interventions [107, 108]. The opportunity via mobile devices to collect intensive context- and time-dependent (longitudinal) data and to systematically vary intervention components enables researchers to test not only these components but also the theoretical concepts and dynamic models that underlie them.
The application of mobile technologies to health behavior interventions is an exciting and rapidly growing field. The ability to provide frequent, time-intensive interventions in the context of the behavior holds considerable promise but also poses many challenges to our current health behavior theories and models. To meet these challenges, our current health behavior theories and models need to expand from elucidating between-person differences to explaining within-person changes over time and to evolve to incorporate dynamic feedback control systems to “close the loop.” Health behavior interventions delivered via mobile technologies offer not only the impetus to transform our current theories into more dynamic feedback control models but also the potential to provide the intensive longitudinal data necessary to test and improve our theoretical intervention models. To date, only a subset of mobile health behavior interventions have been theory-based, but a theory-driven iterative model of mobile intervention development holds promise for improving not only our mobile health behavior interventions but also our theoretical and empirical understanding of health behavior change.
Footnotes
Implications
Practice: Mobile technologies are rapidly evolving as a method for delivering health behavior interventions that can be tailored to the individual throughout the intervention, but the content and timing of these interventions have not been consistently grounded in health behavior theories, so practitioners need to consider the theoretical and empirical basis of mobile health behavior interventions.
Policy: Investment in the development of mobile health behavior interventions needs to be balanced with investment in theoretically grounded content development and evaluation procedures that are responsive to this rapidly evolving area.
Research: In addition to the responsive evaluation of mobile health behavior interventions, researchers need to utilize these applications to test and advance more dynamic health behavior theories, taking advantage of control systems engineering and other dynamic feedback models to advance new theories that can be better applied to the intensive adaptability possible from mobile health behavior interventions.
References
- 1.Webb TL, Joseph J, Yardley L, Michie S. Using the Internet to promote health behavior change: A systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. Journal of Medical Internet Research. 2010;12:e4. doi: 10.2196/jmir.1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tate DF, Finkelstein EA, Khavjou O, Gustafson A. Cost effectiveness of Internet interventions: Review and recommendations. Annals of Behavioral Medicine. 2009;38:40–45. doi: 10.1007/s12160-009-9131-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Norman GJ, Zabinski MF, Adams MA, Rosenberg DE, Yaroch AL, Atienza AA. A review of eHealth interventions for physical activity and dietary behavior change. American Journal of Preventive Medicine. 2007;33:336–345. doi: 10.1016/j.amepre.2007.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.CTIA. (2009). http://www.ctia.org/advocacy/research/index.cfm/AID/10323
- 5.International Communications Union. (2010). http://www.itu.int/ITU-d/ict/publications/idi/2010/Material/MIS_2010_Summary_E.pdf
- 6.Pew Internet &American Life Project. (2010). http://www.pewInternet.org/~/media//Files/Reports/2010/PIP_Mobile_Access_2010.pdf
- 7.Leena K, Tomi L, Arja R. Intensity of mobile phone use and health compromising behaviours: How is information and communication technology connected to health-related lifestyle in adolescence? Journal of Adolescence. 2005;28:35–47. doi: 10.1016/j.adolescence.2004.05.004. [DOI] [PubMed] [Google Scholar]
- 8.Kosaraju A, Barrigan CR, Poropatich RK, Casscells SW. Use of mobile phones as a tool for United States health diplomacy abroad. Telemed J E Health. 2010;16:218–222. doi: 10.1089/tmj.2009.0095. [DOI] [PubMed] [Google Scholar]
- 9.Kaplan WA. Can the ubiquitous power of mobile phones be used to improve health outcomes in developing countries? Global Healthcare. 2006;2:9–22. doi: 10.1186/1744-8603-2-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pharow P, Blobel B, Ruotsalainen P, Petersen F, Hovsto A. Portable devices, sensors and networks: Wireless personalized eHealth services. Studies in Health Technology and Informatics. 2009;150:1012–1016. [PubMed] [Google Scholar]
- 11.Patrick K, Griswold WG, Raab F, Intille SS. Health and the mobile phone. American Journal of Preventive Medicine. 2008;35:177–181. doi: 10.1016/j.amepre.2008.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Becker, M. H. (Ed.) (1974). The health belief model and personal health behavior. Health Education Monographs, 2, 324–473.
- 13.Godin G, Kok G. The theory of planned behavior: A review of its applications to health-related behaviors. American Journal of Health Promotion. 1996;11:87–98. doi: 10.4278/0890-1171-11.2.87. [DOI] [PubMed] [Google Scholar]
- 14.Bandura A. Social cognitive theory: An agentic perspective. Annual Review of Psychology. 2001;52:1–26. doi: 10.1146/annurev.psych.52.1.1. [DOI] [PubMed] [Google Scholar]
- 15.Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. American Journal of Health Promotion. 1997;12:38–48. doi: 10.4278/0890-1171-12.1.38. [DOI] [PubMed] [Google Scholar]
- 16.Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Amer Psychol. 2000;55:68–78. doi: 10.1037//0003-066x.55.1.68. [DOI] [PubMed] [Google Scholar]
- 17.Ogden J. Some problems with social cognition models: A pragmatic and conceptual analysis. Health Psychology. 2003;22:424–428. doi: 10.1037/0278-6133.22.4.424. [DOI] [PubMed] [Google Scholar]
- 18.Burnett KF, Taylor CB, Agras WS. Ambulatory computer-assisted therapy for obesity: A new frontier for behavior therapy. J Cons Clin Psychol. 1985;53:698–703. doi: 10.1037//0022-006x.53.5.698. [DOI] [PubMed] [Google Scholar]
- 19.Prue DM, Riley A, Orlandi MA, Jerome A. Development of a computer-assisted smoking cessation program: A preliminary report. J Adv Med. 1990;3:131–139. [Google Scholar]
- 20.Brownell KD. Adherence to dietary regimens. 2: Components of effective interventions. Behavioral Medicine. 1995;20:155–164. doi: 10.1080/08964289.1995.9933732. [DOI] [PubMed] [Google Scholar]
- 21.Fjeldsoe BS, Marshall AL, Miller YD. Behavior change interventions delivered by mobile telephone short-message service. American Journal of Preventive Medicine. 2009;36:165–173. doi: 10.1016/j.amepre.2008.09.040. [DOI] [PubMed] [Google Scholar]
- 22.Krishna S, Boren SA. Healthcare via cell phone: A systematic review. Telemed e-Health. 2009;15:231–240. doi: 10.1089/tmj.2008.0099. [DOI] [PubMed] [Google Scholar]
- 23.Obermayer JL, Riley WT, Asif O, Jean-Mary J. College smoking-cessation using cell phone text messaging. J Amer Coll Health. 2004;53:71–78. doi: 10.3200/JACH.53.2.71-78. [DOI] [PubMed] [Google Scholar]
- 24.Rodgers A, Corbett T, Bramley D, et al. Do u smoke after txt? Results of a randomized trial of smoking cessation using mobile phone text messaging. Tobacco Control. 2005;14:255–261. doi: 10.1136/tc.2005.011577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Riley WT, Obermayer J, Jean-Mary J. Internet and mobile phone text messaging intervention for college smokers. J Amer Coll Health. 2008;57:245–248. doi: 10.3200/JACH.57.2.245-248. [DOI] [PubMed] [Google Scholar]
- 26.Whittaker R, Maddison R, McRobbie H, et al. A multimedia mobile phone-based youth smoking cessation intervention: Findings from content development and piloting studies. Journal of Medical Internet Research. 2008;10:e49. doi: 10.2196/jmir.1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brendryen H, Kraft P. Happy Ending: A randomized controlled trial of a digital multi-media smoking cessation intervention. Addiction. 2008;103:478–484. doi: 10.1111/j.1360-0443.2007.02119.x. [DOI] [PubMed] [Google Scholar]
- 28.Brendryen H, Drozd F, Kraft P. A digital smoking cessation program delivered through Internet and cell phone without nicotine replacement (happy ending): Randomized controlled trial. Journal of Medical Internet Research. 2008;10:e51. doi: 10.2196/jmir.1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Free C, Whittaker R, Knight R, Abramsky T, Rodgers A, Roberts G. Txt2stop: A pilot randomized controlled trial of mobile phone-based smoking cessation support. Tobacco Control. 2009;18:88–91. doi: 10.1136/tc.2008.026146. [DOI] [PubMed] [Google Scholar]
- 30.Intille SS, Kukla C, Farzanfar R, Bakr W. Just-in-time technology to encourage incremental, dietary behavior change. In AMIA 2003 symposium proceedings, p 874 [PMC free article] [PubMed]
- 31.Brendryen H, Kraft P, Schaalma H. Looking inside the black box: Using intervention mapping to describe the development of an automated smoking cessation intervention happy ending. The Journal of Smoking Cessation. 2010;5:29–56. [Google Scholar]
- 32.Whittaker R, Borland R, Bullen C, Lin RB, McRobbie H, Rodgers A. Mobile phone-based interventions for smoking cessation. Cochrane Database of Systematic Reviews. 2009;4:CD006611. doi: 10.1002/14651858.CD006611.pub2. [DOI] [PubMed] [Google Scholar]
- 33.Joo N, Kim B. Mobile phone short message service messaging for behaviour modification in a community-based weight loss programme in Korea. Journal of Telemedicine and Telecare. 2007;13:416–420. doi: 10.1258/135763307783064331. [DOI] [PubMed] [Google Scholar]
- 34.Burke, L. E., Conroy, M. B., Sereika, S. M., et al. (2011). The effect of electronic self-monitoring on weight loss and dietary intake: A randomized behavioral weight loss trial. Obesity, 19, 338–344. [DOI] [PMC free article] [PubMed]
- 35.Liu WT, Wang CH, Lin HC, et al. Efficacy of a cell phone-based exercise programme for COPD. The European Respiratory Journal. 2008;32:651–659. doi: 10.1183/09031936.00104407. [DOI] [PubMed] [Google Scholar]
- 36.Nguyen HQ, Gill DP, Wolpin S, Steele BG, Benditt JO. Pilot study of a cell phone-based exercise persistence intervention post-rehabilitation for COPD. Int J COPD. 2009;4:301–313. doi: 10.2147/copd.s6643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bauer S, de Niet J, Timman R, Kordy H. Enhancement of care through self-monitoring and tailored feedback via text messaging and their use in the treatment of childhood overweight. Patient Education and Counseling. 2010;79:315–319. doi: 10.1016/j.pec.2010.03.014. [DOI] [PubMed] [Google Scholar]
- 38.Hurling R, Catt M, De Boni M, et al. Using Internet and mobile phone technology to deliver an automated physical activity program: Randomized controlled trial. Journal of Medical Internet Research. 2007;9:e7. doi: 10.2196/jmir.9.2.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Beasley JM, Riley WT, Davis A, Singh J. Evaluation of a PDA-based dietary assessment and intervention program: A randomized controlled trial. Journal of the American College of Nutrition. 2008;27:280–286. doi: 10.1080/07315724.2008.10719701. [DOI] [PubMed] [Google Scholar]
- 40.Haapala I, Barengo NC, Biggs S, Surakka L, Manninen P. Weight loss by mobile phone: A 1-year effectiveness study. Public Health Nutrition. 2009;12:2382–2391. doi: 10.1017/S1368980009005230. [DOI] [PubMed] [Google Scholar]
- 41.Atienza AA, King AC, Oliveira BM, Ahn DK, Gardner CD. Using hand-held computer technologies to improve dietary intake. American Journal of Preventive Medicine. 2008;34:514–518. doi: 10.1016/j.amepre.2008.01.034. [DOI] [PubMed] [Google Scholar]
- 42.King AC, Ahn DK, Oliveira BM, Atienza AA, Castro CM, Gardner CD. Promoting physical activity through hand-held computer technology. American Journal of Preventive Medicine. 2008;34:138–142. doi: 10.1016/j.amepre.2007.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Patrick K, Raab F, Adams MA, et al. A text message-based intervention for weight loss: Randomized controlled trial. Journal of Medical Internet Research. 2009;11:e1. doi: 10.2196/jmir.1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fjeldsoe BS, Miller YD, Marshall AL. MobileMums: A randomized controlled trial of an SMS-based physical activity intervention. Annals of Behavioral Medicine. 2010;39:101–111. doi: 10.1007/s12160-010-9170-z. [DOI] [PubMed] [Google Scholar]
- 45.Hiltz SR. Productivity enhancement from computer-mediated communication: A systems contingency approach. Communications of the ACM. 1988;31:1438–1454. [Google Scholar]
- 46.Krishna S, Boren SA. Diabetes self-management care via cell phone: A systematic review. J Diabetes Sci Technol. 2008;2:509–517. doi: 10.1177/193229680800200324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ngo J, Engelen A, Molag M, Roesle J, Garcia-Segovia P, Serra-Majem L. A review of the use of information and communication technologies for dietary assessment. British J Nutr. 2009;101:S12–S112. doi: 10.1017/S0007114509990638. [DOI] [PubMed] [Google Scholar]
- 48.Boushey CJ, Kerr DA, Wright J, Lutes KD, Ebert DS, Delp EJ. Use of technology in children’s dietary assessment. Euro J Clin Nutr. 2009;63:S50–S57. doi: 10.1038/ejcn.2008.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Six BL, Schap TE, Zhu FM, Mariappan A, Bosch M, Delp EJ, Ebert DS, Kerr DA, Boushey CJ. Evidence-based development of a mobile telephone food record. Journal of the American Dietetic Association. 2010;110:74–79. doi: 10.1016/j.jada.2009.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hynes M, Wang H, Kilmartin L. Off-the-shelf mobile handset environments for deploying accelerometer based gait and activity analysis algorithms. Conf Proc IEEE Eng Med Biol Soc. 2009;2009:5187–5190. doi: 10.1109/IEMBS.2009.5333715. [DOI] [PubMed] [Google Scholar]
- 51.Bexelius C, Lof M, Sandin S, Trolle Lagerros Y, Forsum E, Litton JE. Measure of physical activity using cell phones: Validation using criterion measures. J Med Internet Res. 2010;29:e2. doi: 10.2196/jmir.1298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Farmer KC. Methods for measuring and monitoring medication regimen adherence in clinical trials and clinical practice. Clinical Therapeutics. 1999;21:1074–1090. doi: 10.1016/S0149-2918(99)80026-5. [DOI] [PubMed] [Google Scholar]
- 53.Naditz A. Medication compliance—helping patients through technology: Modern “smart” pillboxes keep memory-short patients on their medical regimen. Telemed J E Health. 2008;14:875–880. doi: 10.1089/tmj.2008.8476. [DOI] [PubMed] [Google Scholar]
- 54.Safren SA, Hendriksen ES, Desousa N, Boswell SL, Mayer KH. Use of an on-line pager system to increase adherence to antiretroviral medications. AIDS Care. 2003;15:787–793. doi: 10.1080/09540120310001618630. [DOI] [PubMed] [Google Scholar]
- 55.Simoni JM, Huh D, Frick PA, et al. Peer support and pager messaging to promote antiretroviral modifying therapy in Seattle: A randomized controlled trial. Journal of Acquired Immune Deficiency Syndromes. 2009;52:465–473. doi: 10.1097/qai.0b013e3181b9300c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Koshy E, Car J, Majeed A. Effectiveness of mobile-phone short messaging service (SMS) reminders for ophthalmology outpatient appointments: Observational study. BMC Ophthalmology. 2008;8:9. doi: 10.1186/1471-2415-8-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bos A, Hoogstraten J, Prahl-Andersen B. Failed appointments in an orthodontic clinic. BAm J Orthod Dentofacial Orthop. 2005;127:355–357. doi: 10.1016/j.ajodo.2004.11.014. [DOI] [PubMed] [Google Scholar]
- 58.Leong KC, Leong KW, Mastura I, et al. The use of text messaging to improve attendance in primary care: A randomized controlled trial. Family Practice. 2006;23:699–705. doi: 10.1093/fampra/cml044. [DOI] [PubMed] [Google Scholar]
- 59.Chen ZW, Fang LZ, Chen LY, Dai HL. Comparison of an SMS text messaging and phone reminder to improve attendance at a health promotion center: A randomized controlled trial. Journal of Zhejiang University. Science B. 2008;9:34–38. doi: 10.1631/jzus.B071464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Blake H. Mobile phone technology in chronic disease management. Nursing Standard. 2008;23:43–46. doi: 10.7748/ns2008.11.23.12.43.c6728. [DOI] [PubMed] [Google Scholar]
- 61.Russel-Minda E, Jutai J, Speechly M, Bradley K, Chudyk A, Petrella R. Health technologies for monitoring and managing diabetes: A systematic review. J Diabetes Sci Technol. 2009;3:1460–1471. doi: 10.1177/193229680900300628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Skinner C, Finkelstein J. Using cell phones for chronic disease prevention and management. AMIA Annual Symposium Proceedings. 2008;6:1137. [PubMed] [Google Scholar]
- 63.Franklin VL, Waller A, Pagliari C, Greene SA. A randomized controlled trial of Sweet Talk, a text messaging system to support young people with diabetes. Diabetes Med. 2006;23:1332–1338. doi: 10.1111/j.1464-5491.2006.01989.x. [DOI] [PubMed] [Google Scholar]
- 64.American Diabetes Association Executive summary: Standards of medical care in diabetes—2009. Diabetes Care. 2009;32:S6–S12. doi: 10.2337/dc09-S006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hedtke PA. Can wireless technology enable new diabetes management tools. J Diabetes Sci Technol. 2008;2:127–130. doi: 10.1177/193229680800200118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ma Y, Olendzki BC, Chiriboga D, et al. PDA-assisted low glycemic index dietary intervention for type 2 diabetes: A pilot study. Euro J Clin Nutr. 2006;60:1235–1243. doi: 10.1038/sj.ejcn.1602443. [DOI] [PubMed] [Google Scholar]
- 67.Forjuoh SN, Reis MD, Couchman GR, Ory MG. Improving diabetes self-care with a PDA in ambulatory care. Telemed Health. 2008;14:273–279. doi: 10.1089/tmj.2007.0053. [DOI] [PubMed] [Google Scholar]
- 68.Lanzola G, Capozzi D, D’Annunzio G, Ferrari P, Bellazzi R, Larizza C. Going mobile with a multi-access service for the management of diabetes patients. J Diabetes Sci Technol. 2007;1:730–737. doi: 10.1177/193229680700100518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Arsand E, Tufano JT, Ralston JD, Hjortdahl P. Designing mobile dietary management support technologies for people with diabetes. Journal of Telemedicine and Telecare. 2008;14:329–332. doi: 10.1258/jtt.2008.007001. [DOI] [PubMed] [Google Scholar]
- 70.Rami B, Popow C, Horn W, Waldhoer T, Schober E. Telemedical support to improve glycemic control in adolescents with type 1 diabetes mellitus. European Journal of Pediatrics. 2006;165:701–705. doi: 10.1007/s00431-006-0156-6. [DOI] [PubMed] [Google Scholar]
- 71.Quinn CC, Clough SS, Minor JM, Lender D, Okafor MC, Gruber-Baldini A. WellDocTM mobile diabetes management randomized controlled trial: Change in clinical and behavioral outcomes and patient and physician satisfaction. Diabetes Technology and Therapeutics. 2008;10:160–168. doi: 10.1089/dia.2008.0283. [DOI] [PubMed] [Google Scholar]
- 72.Turner J, Larsen M, Tarassenko L, Neil A, Farmer A. Implementation of telehealth support for patients with type 2 diabetes using insulin treatment: An exploratory study. Inform Prim Care. 2009;17:47–53. doi: 10.14236/jhi.v17i1.714. [DOI] [PubMed] [Google Scholar]
- 73.Cho JH, Lee HC, Lim DJ, Kwon HS, Yoon KH. Mobile communication using a mobile phone with a glucometer for glucose control in type 2 patients with diabetes: As effective as an Internet-based glucose monitoring system. Journal of Telemedicine and Telecare. 2009;15:77–82. doi: 10.1258/jtt.2008.080412. [DOI] [PubMed] [Google Scholar]
- 74.Logan AG, McIsaac WJ, Tisler A, et al. Mobile phone-based remote patient monitoring system for management of hypertension in diabetic patients. Amer J Hypertension. 2007;20:942–948. doi: 10.1016/j.amjhyper.2007.03.020. [DOI] [PubMed] [Google Scholar]
- 75.Leu MG, Norris TE, Hummel J, Isaac M, Brogan MW. A randomized controlled trial of an automated wireless messaging system for diabetes. Diabetes Technology and Therapeutics. 2005;7:710–718. doi: 10.1089/dia.2005.7.710. [DOI] [PubMed] [Google Scholar]
- 76.Hanauer DA, Wentzell K, Laffel N, Laffel LM. Computerized automated reminder diabetes system (CARDS): Email and SMS cell phone text messaging reminders to support diabetes management. Diabetes Technology and Therapeutics. 2009;11:99–106. doi: 10.1089/dia.2008.0022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Strandbygaard U, Thomsen SF, Backer V. A daily SMS reminder increases adherence to asthma treatment: A three-month follow-up study. Respiratory Medicine. 2010;104:166–171. doi: 10.1016/j.rmed.2009.10.003. [DOI] [PubMed] [Google Scholar]
- 78.Chung P, Yu T, Scheinfeld N. Using cellphones for teledermatology, a preliminary study. Dermatology Online Journal. 2007;13:2. [PubMed] [Google Scholar]
- 79.Tang FH, Law MY, Lee AC, Chan LW. A mobile phone integrated health care delivery system for medical images. Journal of Digital Imaging. 2004;17:217–225. doi: 10.1007/s10278-004-1015-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annual Review of Clinical Psychology. 2008;4:1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415. [DOI] [PubMed] [Google Scholar]
- 81.National Institutes of Health. (2010). http://projectreporter.nih.gov (reporter_searchresults.cfm?&new=1&icde=5933670&loc=2&CFID=17945345&CFTOKEN=13189329). Accessed 29 Oct 2010.
- 82.Skevofilakas M, Mougiakakou SG, Zarkogianni K, et al. A communication and information technology infrastructure for real-time monitoring and management of type 1 diabetes patients. Conf Proc IEEE Eng Med Biol Soc. 2007;2007:3685–3686. doi: 10.1109/IEMBS.2007.4353131. [DOI] [PubMed] [Google Scholar]
- 83.Holtz B, Whitten P. Managing asthma with mobile phones: A feasibility study. Telemed J E Health. 2009;15:907–909. doi: 10.1089/tmj.2009.0048. [DOI] [PubMed] [Google Scholar]
- 84.Ryan D, Pinnock H, Lee AJ, et al. The CYMPLA trial. Mobile phone-based structured intervention to achieve asthma control in patients with uncontrolled persistent asthma: A pragmatic randomized controlled trial. Primary Care Respiratory Journal. 2009;18:343–345. doi: 10.4104/pcrj.2009.00064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Rosenstock IM. Historical origins of the Health Belief Model. Health Education Monographs. 1974;2:328–335. doi: 10.1177/109019817800600406. [DOI] [PubMed] [Google Scholar]
- 86.Dunton and Atienza The need for time-intensive information in healthful eating and physical activity research: A timely topic. JADA. 2009;109(1):30–35. doi: 10.1016/j.jada.2008.10.019. [DOI] [PubMed] [Google Scholar]
- 87.Boorsboom D, Mellenbergh GJ, van Heerden J. The theoretical status of latent variables. Psychological Review. 2003;110:202–219. doi: 10.1037/0033-295X.110.2.203. [DOI] [PubMed] [Google Scholar]
- 88.Neville LM, O'Hara B, Milat AJ. Computer-tailored dietary behaviour change interventions: A systematic review. Health Education Research. 2009;24:699–720. doi: 10.1093/her/cyp006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Lustria ML, Cortese J, Noar SM, Glueckauf RL. Computer-tailored health interventions delivered over the Web: Review and analysis of key components. Patient Education and Counseling. 2009;74:156–173. doi: 10.1016/j.pec.2008.08.023. [DOI] [PubMed] [Google Scholar]
- 90.Heron KE, Smyth JM. Ecological momentary interventions: Incorporating mobile technology into psychosocial and health behaviour treatments. British Journal of Health Psychology. 2010;15:1–39. doi: 10.1348/135910709X466063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Llewelyn S, Hardy G. Process research in understanding and applying psychological therapies. The British Journal of Clinical Psychology. 2001;40:1–21. doi: 10.1348/014466501163436. [DOI] [PubMed] [Google Scholar]
- 92.Åström, K. J. & Murray, R. M. (2008). Feedback systems: An introduction for scientists and engineers. http://www.cds.caltech.edu/~murray/amwiki.
- 93.Rivera DE, Pew MD, Collins LM. Using engineering control principles to inform the design of adaptive interventions: A conceptual introduction. Drug and Alcohol Dependence. 2007;88(suppl. 2):S31–S40. doi: 10.1016/j.drugalcdep.2006.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Navarro-Barrientos JE, Rivera DE, Collins LM. A dynamical systems model for understanding behavioral interventions for weight loss. In: Chai SK, Salerno JJ, Mabry PL, editors. 2010 international conference on social computing, behavioral modeling, and prediction (SBP 2010) Heidelberg: Springer; 2010. pp. 170–179. [Google Scholar]
- 95.Deco G, Jirsa VK, Robinson PA, Breakspear M, Friston K. The dynamic brain: From spiking neurons to neural masses and cortical fields. PLoS Computational Biology. 2008;4:e1000092. doi: 10.1371/journal.pcbi.1000092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Saper CB, Chou TC, Scammell TE. The sleep switch: Hypothalamic control of sleep and wakefulness. Trends Neuroscience. 2001;24:726–731. doi: 10.1016/s0166-2236(00)02002-6. [DOI] [PubMed] [Google Scholar]
- 97.Todorov E. Optimality principles in sensorimotor control. Nature Neuroscience. 2004;7:907–915. doi: 10.1038/nn1309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Lewis FL, Vamvoudakis KG. Reinforcement learning for partially observable dynamic processes: Adaptive dynamic programming using measured output data. IEEE Transactions on Systems, Man, and Cybernetics. Part B, Cybernetics. 2010;41:14–25. doi: 10.1109/TSMCB.2010.2043839. [DOI] [PubMed] [Google Scholar]
- 99.Bequette BW. Glucose clamp algorithms and insulin time–action profiles. J Diabetes Sci Technol. 2009;3:1005–1013. doi: 10.1177/193229680900300503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Nandola, N., Rivera, D. E. (2010). A robust model predictive control formulation for hybrid systems with application to adaptive behavioral interventions. In American Control Conference, Baltimore, MD, pp. 6286–6292. [DOI] [PMC free article] [PubMed]
- 101.Schwartz JD, Rivera DE. A process control approach to tactical inventory management in production-inventory systems. Int J Production Economics. 2010;125:111–124. [Google Scholar]
- 102.Ogunnaike BA, Ray WH. Process dynamics, modeling, and control. New York: Oxford University Press; 1994. [Google Scholar]
- 103.Ljung L. System identification: Theory for the user. Prentice Hall information and system sciences series. New York: Prentice Hall; 1999. [Google Scholar]
- 104.Ramsay J, Silverman B. Functional data analysis. New York: Springer; 2005. [Google Scholar]
- 105.Camacho EF, Bordons C. Model predictive control. 2. New York: Springer; 2004. [Google Scholar]
- 106.Collins LM, Murphy SA, Bierman KL. A conceptual framework for adaptive preventive interventions. Prevention Science. 2004;5:185–196. doi: 10.1023/b:prev.0000037641.26017.00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.O’Grady L, Witteman H, Bender JL, Urowitz S, Wiljer D, Jaded AR. Measuring the impact of a moving target: Towards a dynamic framework for evaluating collaborative adaptive interactive technologies. Journal of Medical Internet Research. 2009;11:e20. doi: 10.2196/jmir.1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Resnicow K, Strecher V, Couper M, et al. Methodologic and design issues in patient-centered e-health research. American Journal of Preventive Medicine. 2010;38:98–102. doi: 10.1016/j.amepre.2009.09.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Downer SR, Meara JG, Da Costa AC. Use of SMS text messaging to improve outpatient adherence. MJA. 2005;183:366–368. doi: 10.5694/j.1326-5377.2005.tb07085.x. [DOI] [PubMed] [Google Scholar]
- 110.Downer SR, Meara JG, Da Costa AC, Sethuraman K. SMS text messaging improves outpatient attendance. Australian Health Review. 2006;30:389–396. doi: 10.1071/ah060389. [DOI] [PubMed] [Google Scholar]
- 111.Foley J, O’Neill M. Use of mobile short message service (SMS) as a reminder: The effect on patient attendance. European Archives of Paediatric Dentistry. 2009;10:15–18. doi: 10.1007/BF03262661. [DOI] [PubMed] [Google Scholar]
- 112.da Costa TM, Salomao PL, Martha AS, Pisa IT, Sigulem D. The impact of short message service text messages sent as appointment reminders to patients’ cell phones at outpatient clinics in Sao Paulo, Brazil. International Journal of Medical Informatics. 2010;79:65–70. doi: 10.1016/j.ijmedinf.2009.09.001. [DOI] [PubMed] [Google Scholar]
- 113.Kwon HS, Cho JH, Kim HS, et al. Development of web-based diabetic patient management system using short message service (SMS) Diabetes Research and Clinical Practice. 2004;66S:S133–S137. doi: 10.1016/j.diabres.2003.10.028. [DOI] [PubMed] [Google Scholar]
- 114.Ostojic V, Cvoriscec B, Ostojic SB, Reznikoff D, Stipic-Markovic A, Tudjman Z. Improving asthma control through telemedicine: A study of short-message service. Telemed J E Health. 2005;11:28–35. doi: 10.1089/tmj.2005.11.28. [DOI] [PubMed] [Google Scholar]
- 115.Kim HS, Yoo YS, Shim HS. Effects of an Internet-based intervention on plasma glucose levels in patients with type 2 diabetes. Journal of Nursing Care Quality. 2005;20:335–340. doi: 10.1097/00001786-200510000-00009. [DOI] [PubMed] [Google Scholar]
- 116.Kim HS, Kim NC, Ahn SH. Impact of a nurse short message service intervention for patients with diabetes. Journal of Nursing Care Quality. 2006;21:266–271. doi: 10.1097/00001786-200607000-00012. [DOI] [PubMed] [Google Scholar]
- 117.Kim HS, Jeong HS. A nurse short message service by cellular phone in type-2 diabetic patients for six months. Journal of Clinical Nursing. 2007;16:1082–1087. doi: 10.1111/j.1365-2702.2007.01698.x. [DOI] [PubMed] [Google Scholar]
- 118.Benhamou PY, Melki V, Boizel R, et al. One-year efficacy and safety of Web-based follow-up using cellular phone in type 1 diabetic patients under insulin pump therapy: The PumpNet study. Diabetes Metabol. 2007;33:220–226. doi: 10.1016/j.diabet.2007.01.002. [DOI] [PubMed] [Google Scholar]
- 119.Yoon KH, Kim HS. A short message service by cellular phone in type 2 diabetic patients for 12 months. Diabetes Research and Clinical Practice. 2008;79:256–261. doi: 10.1016/j.diabres.2007.09.007. [DOI] [PubMed] [Google Scholar]
- 120.Newton KH, Wiltshire EJ, Elley CR. Pedometers and text messaging to increase physical activity: Randomized controlled trial of adolescents with type 1 diabetes. Diabetes Care. 2009;32:813–815. doi: 10.2337/dc08-1974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Prabhakaran L, Chee WY, Chua KC, Abisheganaden J, Wong WM. The use of text messaging to improve asthma control: A pilot study using mobile phone short messaging service (SMS) Journal of Telemedicine and Telecare. 2010;16:286–290. doi: 10.1258/jtt.2010.090809. [DOI] [PubMed] [Google Scholar]