Abstract
OBJECTIVE
The purpose of our study was to accurately describe facility characteristics among community-based screening and diagnostic mammography practices in the United States.
MATERIALS AND METHODS
A survey was developed and applied to community-based facilities providing screening mammography in three geographically distinct locations in the states of Washington, Colorado, and New Hampshire. The facility survey was conducted between December 2001 and September 2002. Characteristics surveyed included facility type, services offered, charges for screening and diagnostic mammography, information systems, and interpretation methods, including the frequency of double interpretation.
RESULTS
Among 45 responding facilities, services offered included screening mammography at all facilities, diagnostic mammography at 34 facilities (76%), breast sonography at 30 (67%), breast MRI at seven (16%), and nuclear medicine breast scanning at seven (16%). Most facilities surveyed were radiology practices in nonhospital settings. Eight facilities (18%) reported performing clinical breast examinations routinely along with screening mammography. Only five screening sites (11%) used computer-aided detection (CAD) and only two (5%) used digital mammography. Nearly two thirds of facilities interpreted screening mammography examinations on-site, whereas 91% of facilities interpreted diagnostic examinations on-site. Only three facilities (7%) interpreted screening examinations on line as they were performed. Approximately half of facilities reported using some type of double interpretation, although the methods of double interpretation and the fraction of cases double-interpreted varied widely across facilities. On average, approximately 15% of screening examinations and 10% of diagnostic examinations were reported as being double-interpreted.
CONCLUSION
Comparison of this survey’s results with those collected a decade earlier indicates dramatic changes in the practice of mammography, including a clear distinction between screening and diagnostic mammography, batch interpretation of screening mammograms, and improved quality assurance and medical audit tools. Diffusion of new technologies such as CAD and digital mammography was not widespread. The methods of double-interpretation and the fraction of cases double-interpreted varied widely across study sites.
In the past 15 years, most European and other developed countries have implemented population-based, nationally or regionally organized breast screening programs [1]. The United States is one of the few developed nations without an organized population-based screening program. With passage of the Mammography Quality Standards Act of 1992 [2], the U.S. Congress required the Department of Health and Human Services to establish a pilot program to monitor the performance of mammography in the United States. In 1994, the National Cancer Institute began the National Breast Cancer Surveillance Consortium (NBCSC) [3]. Today, the NBCSC is an affiliation of seven data collection and monitoring systems that have collected data on more than 1,640,000 women undergoing mammography. Three of the seven NBCSC groups participated in the collection of data for this survey of mammography facilities.
Only a handful of studies have surveyed multiple U.S. facilities performing mammography to obtain a picture of the practice of mammography in the United States. One survey, conducted in 1992 of a 10% random sample of U.S. mammography facilities, revealed that 40% of facilities did not distinguish screening from diagnostic mammography, only 20% of facilities used batch interpretation of screening mammography, only 13% of facilities operated at high volume, and the average cost of screening mammography was $89 (range, $10–225) [4]. The authors concluded that screening mammography in the United States did not appear to be organized for high volume or low cost [4].
Double interpretation of screening mammograms is known to increase sensitivity to breast cancer, while incurring a higher recall rate and additional costs [5–8]. Although double interpretation of mammograms is common in organized screening programs in other countries [9], its rate of use in the United States has not, to our knowledge, previously been evaluated.
As part of a project exploring the practice of mammography in the United States, a survey was conducted of 45 community-based screening centers in three geographically distinct locations of the United States. This article reports the results of survey responses concerning mammography practice setting, services offered, charges for screening and diagnostic mammography, interpretation methods, and audit systems.
Materials and Methods
Study Population
Data for this project were acquired from a survey of community-based, multicenter facilities in three geographically distinct breast cancer surveillance programs: Group Health Cooperative Breast Cancer Surveillance System [10, 11], a nonprofit health plan in the Pacific Northwest that includes more than 100,000 women 40 years old and older; the New Hampshire Mammography Network [12–14], which provides mammography to more than 85% of the women in the state of New Hampshire; and the Colorado Mammography Advocacy Program, which provides mammography to approximately half of the women in the six-county metropolitan area of Denver [15]. These three breast cancer screening programs are members of the federally funded NBCSC [3]. Eligible facilities included those performing screening mammography within the three national consortium programs between December 2001 and September 2002. The current study was approved by the institutional review boards of the University of Washington School of Medicine, the Group Health Cooperative of Puget Sound, Dartmouth College, Northwestern University, and the Colorado Mammography Advocacy Program.
Mammography Facility Survey
A facility survey was developed by a panel of experts in breast imaging, medical physics, economics, biostatistics, and epidemiology. The criteria, construct, and content validity of the survey were established through expert opinion. The survey was pilot-tested in community settings among mammography facilities not taking part in the study. The survey included basic questions on breast imaging and clinical care services, charges for screening and diagnostic mammography, interpretation methods, and patient databases (survey available on request). The survey did not request data on revenues collected for mammography services.
Surveys were mailed or hand-delivered to a designated contact person at each facility. Nonresponding facilities were followed up with telephone calls or facility visits to ensure survey completion. If necessary, data were obtained from multiple individuals at a facility. Therefore, the respondent was noted for each survey question in the following categories: lead technologist, other technologist, radiologist, radiology department or facility business manager, and breast cancer screening surveillance research office.
Two individuals at each of the three breast cancer consortium groups independently entered survey data into a relational database with programmed data checks. The site coordinator resolved any discrepancies between the two data entries. All survey data were sent encrypted via FTP (file transfer protocol) to the central analytic center at Group Health Cooperative. Charge data were not available for the six health plan facilities in Washington State.
Other Data
Facilities responding to the survey were identified as having low, medium, or high mammography volume (Table 1) on the basis of previous definitions, to obtain comparable data to those reported a decade earlier [4]. Facilities responding to the survey were identified as being “urban” or “rural” by the zip code in which they were located, defined by the Rural Urban Commuting Area Code (RUCA) classification system [16, 17]. The zip codes of all certified mammography facilities in the United States in 2002 were obtained from the U.S. Food and Drug Administration (FDA). These facilities were classified as urban or rural using the same classification system. This allowed comparison of the urban–rural distribution of surveyed facilities with that of FDA-approved mammography facilities in operation at the time of the survey. Data on total mammography volume (screening plus diagnostic examinations) for each facility in 2001 were obtained directly from the three NBCSC facilities.
TABLE 1.
Available Breast Services Among 45 Mammography Facilities
| Services | No. of Facilities | % of Total Facilities |
|---|---|---|
| Imaging technique (n = 45) | ||
| Screening mammography | 45 | 100 |
| Diagnostic mammography | 34 | 76 |
| Breast sonography | 30 | 67 |
| Ductography | 16 | 36 |
| Breast MRI | 7 | 16 |
| Breast nuclear medicine scanning | 7 | 16 |
| Digital mammography | 2 | 5 |
| Computer-aided detection | 5 | 11 |
| Other | 7 | 16 |
| Interventional procedures (n = 45) | ||
| Cyst aspiration | 24 | 53 |
| Needle localization | 23 | 51 |
| Core biopsy | 18 | 40 |
| Fine-needle aspiration | 12 | 27 |
| Vacuum-assisted biopsy | 11 | 24 |
| Annual mammography volume (n = 42)a | ||
| Low | 6 | 14 |
| Medium | 30 | 71 |
| High | 6 | 14 |
Note.—Low volume = < five examinations per mammography unit per day, Medium = 5–14 examinations, High = ≥15 examinations [4].
Annual volume included total screening and diagnostic mammography examinations performed in 2001. Data were available for only 42 facilities.
Results
Forty-five of 53 eligible facilities responded to our survey, for a response rate of 85%. Most surveys were completed by the lead technologist at each facility. Among the 45 responding facilities, 10 (22%) were associated with an academic medical center. Seventeen (38%) were hospital-based nonacademic centers and 24 (53%) were non-hospital-based clinics or office-based practices. One facility was an off-site office owned by a hospital and another was owned by a combination of a hospital and radiologists.
A broad range of breast imaging services were provided (Table 1), including diagnostic mammography (at 76% of screening facilities), breast sonography (67%), breast MRI (16%), breast nuclear medicine scanning (scintimammography or PET of the breast, 16%), digital mammography (5%), and computer-assisted diagnosis (11%). Breast interventional procedures included cyst aspiration (at 53% of screening facilities), needle localization (51%), core biopsy (40%), fine-needle aspiration (27%), and vacuum-assisted biopsy (24%). Most facilities (71%) performed at medium medical volume, defined as between five and 15 examinations per mammography unit (machine) per day. No significant differences were noted in volume among facilities by association with academic medical center or financial profit status (data not shown). Eight facilities (18%) reported performing clinical breast examinations routinely along with screening mammography.
Total facility charges (technical plus professional) were compared with 2002 total Medicare reimbursement rates of $69.23 for screening mammography (Fig. 1) and $89.14 for diagnostic mammography (Fig. 2). All facilities charged more than Medicare rates for both screening and diagnostic mammography. The median total charge for screening mammography was $141 (range, $75–233.50; n = 39) or 2.0 times the typical Medicare reimbursement. The median total charge for diagnostic mammography was $153.35 (range, $96–264.40; n = 28) or 1.7 times the typical Medicare reimbursement.
Fig. 1.
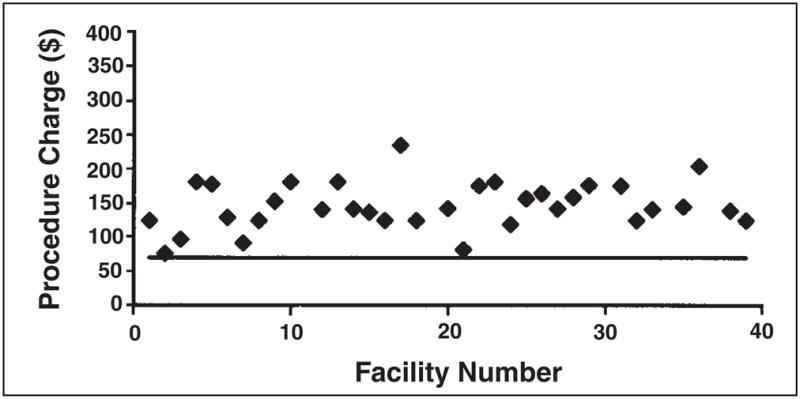
Graph shows total charges (technical and interpretation charges) for screening mammography (individual points) compared with the Medicare reimbursement rate for screening mammography (solid line).
Fig. 2.
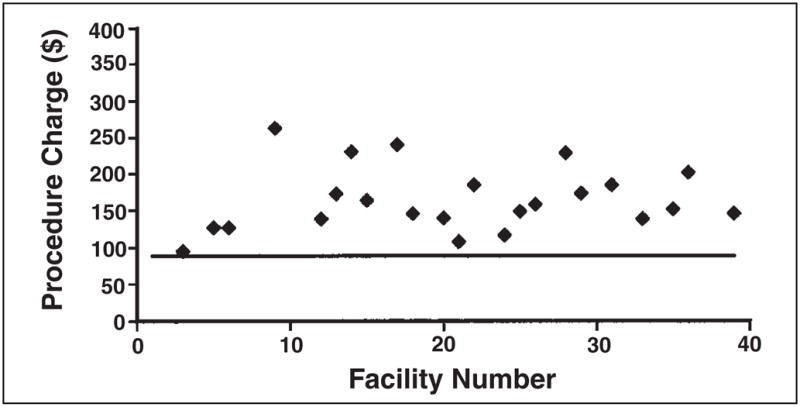
Graph shows total charges (technical and interpretation charges) for diagnostic mammography (individual points) compared with Medicare reimbursement rate for diagnostic mammography (solid line).
Only small average differences in charges were found between facilities on the basis of affiliation with hospitals, affiliation with academic medical centers, and financial profit status for both screening and diagnostic mammography (Table 2). On average, academic centers charged 6% more for screening mammography and 13% more for diagnostic mammography than nonacademic centers (data not shown). Facilities located in hospitals, on average, charged 4% more for screening mammography and 13% more for diagnostic mammography than facilities not located in hospitals. On average, nonprofit centers charged 8% more for screening mammography and 2% more for diagnostic mammography than for-profit centers.
TABLE 2.
Facility Charges for Screening and Diagnostic Mammography Examinations By Hospital Location and Profit Status
| Facility Charges | Located in a Hospital | For-Profit Institutions | ||||||
|---|---|---|---|---|---|---|---|---|
| Yes | No | Yes | No | |||||
| Mean ($) | SE ($) | Mean ($) | SE ($) | Mean ($) | SE ($) | Mean ($) | SE ($) | |
| Screening mammography (n = 39) | (n = 15) | (n = 20) | (n = 25) | (n = 14) | ||||
|
| ||||||||
| Facility fee | 103.11 | 7.79 | 104.36 | 5.12 | 103.64 | 4.76 | 106.71 | 8.77 |
| Radiologist fee | 40.74 | 5.15 | 35.75 | 4.11 | 35.88 | 3.70 | 41.74 | 5.13 |
|
| ||||||||
| Total fee | 147.58 | 11.60 | 142.21 | 7.01 | 141.38 | 6.13 | 152.47 | 12.40 |
|
| ||||||||
| Diagnostic mammography (n = 28) | (n = 15) | (n = 10) | (n = 14) | (n = 14) | ||||
|
| ||||||||
| Facility fee | 126.57 | 9.55 | 113.57 | 13.78 | 124.45 | 13.80 | 120.22 | 8.82 |
| Radiologist fee | 44.36 | 5.74 | 41.56 | 5.32 | 41.87 | 4.82 | 44.45 | 5.74 |
|
| ||||||||
| Total fee | 174.61 | 13.26 | 155.13 | 14.64 | 164.13 | 13.51 | 167.77 | 12.97 |
Among facilities offering both screening and diagnostic mammography, we assessed availability of same-day evaluation of screening mammograms with abnormal findings (data not shown): not available (38%), available for some but fewer than 25% of screening mammograms (26%), available for 25–75% of screening mammograms (12%), and available for more than 75% of abnormal screening mammograms (24%).
Table 3 presents survey results on interpretation systems. It indicates that 62% of facilities interpreted screening mammography examinations on-site, and 91% of facilities offering diagnostic mammography interpreted those examinations on-site. Among screening facilities, only three (7%) interpreted 80% or more of screening studies on line as they were performed. Thirty-eight facilities (84%) used batch interpretation of screening mammograms. Table 3 also shows that 59% of facilities performing diagnostic examinations interpreted those examinations while women waited for the results.
TABLE 3.
Mammography Interpretation System
| Mammography | Screening Mammography (Total Facilities = 45) | Diagnostic Mammography (Total Facilities = 34) | ||
|---|---|---|---|---|
| No. | % | No. | % | |
| Interpretation | ||||
| Interpreted on-sitea | 28 | 62 | 31 | 91 |
| Interpreted on line as they were performedb | 3 | 7 | — | — |
| Interpreted while woman waited (always) | 0 | 0 | 20 | 59 |
| Interpreted while woman waited (sometimes) | 6 | 13 | 9 | 27 |
| Used batch interpretationc | 38 | 84 | — | — |
| Second radiologist knew interpretation of first | 15 | 65 | — | — |
| All interpretations recorded for multiple interpretations | 16 | 70 | — | — |
| Double interpretation summary | ||||
| No double interpretation | 21 | 47 | 15 | 44 |
| Double interpretation | 23 | 51 | 19 | 56 |
| All | 5 | 11 | 2 | 6 |
| Random subset | 14 | 31 | 17 | 50 |
Note.—Dash (—) indicates that no diagnostic facility responded positively in these categories.
100% of mammograms interpreted at the facility.
≥ 80% of screening studies interpreted on line as they are performed.
≥ 10 mammograms interpreted at a time.
In response to survey choices about double interpretation of screening examinations, five facilities (11% of screening facilities) reported double interpretation of all screening mammograms, 14 sites reported double interpretation of a “random subset” of screening mammograms, three sites did not specify the subset being double interpreted, and one site reported double interpretation when requested by one patient (Table 3). For sites responding that they double-interpreted a subset of screening mammograms, responses to the fraction of cases double-interpreted ranged from 2% (two sites) to 30% (three sites), with a median fraction of screening cases double-interpreted of 6.5%. Of the nine sites that reported double interpretation of a subset of screening mammograms and provided a fraction of screening mammograms that were double-interpreted, a mean of 13.4% of screening cases were double-interpreted, weighing each site equally. Therefore, among sites that reported double interpretation of some subset of screening mammograms, we estimate that between 6.5% and 13.4% of screening cases were double-interpreted. Because 11% of screening facilities double-interpreted all examinations, 40% of facilities double-interpreted an average of between 6.5% and 13.4% of examinations, and the remaining 49% of facilities
Among the 34 sites performing diagnostic mammography, two facilities (6%) reported double interpretation of all diagnostic mammograms and 17 facilities (50%) reported double interpretation a subset of diagnostic mammograms. Among this last category, the specific fraction of diagnostic mammograms double-interpreted ranged from 1% (two sites) to 80% (one site). The median fraction of diagnostic cases double-interpreted was 5% and the mean fraction double-interpreted was 12%, weighing each site equally. Because 6% of facilities performing diagnostic mammography double-interpreted all examinations, 50% of facilities double-interpreted between 5% and 12% of examinations, and the remaining 44% of facilities double-interpreted no examinations, we estimate that between 8.5% and 12% of diagnostic mammography examinations were double-interpreted, weighing each site equally for number of examinations performed.
Among the 23 facilities performing double interpretation of screening mammograms, the methods used to obtain final results were variable (Fig. 3). Double interpretation was un-blinded (i.e., the second radiologist knew the interpretation of the first) at 65% of facilities, and all interpretations were recorded at 70%. At 9% of facilities performing double interpretation, the final interpretation was reached by consensus between the two interpreting radiologists. At 48% of facilities performing double interpretation, the opinion of the second radiologist was final. At two facilities (9%), a third radiologist made the decision blinded to the two prior conflicting interpretations. At one facility (4%), a third radiologist made the final decision taking into account the two prior conflicting interpretations, and at one facility (4%), the highest Breast Imaging Reporting and Data System (BI-RADS) [18] interpretation was considered final.
Fig. 3.
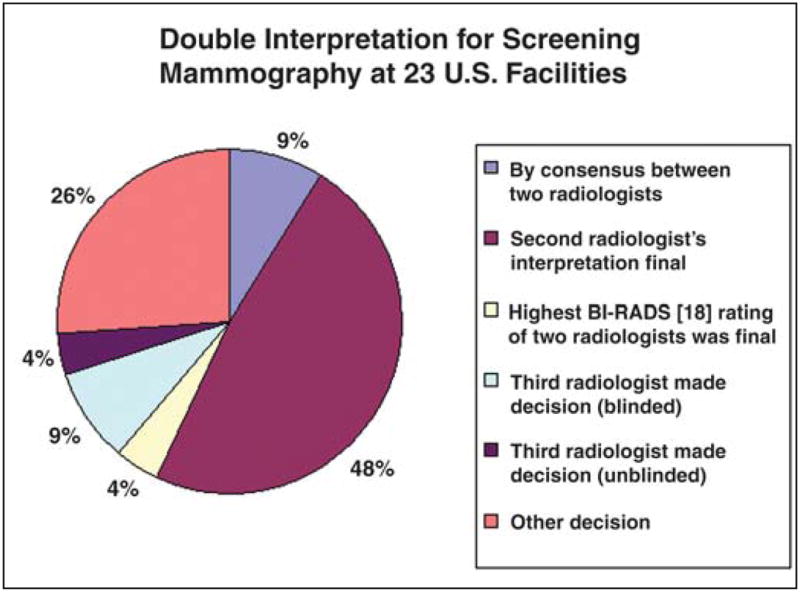
Pie chart shows double-interpretation methods for screening mammograms at 23 U.S. facilities. BI-RADS = Breast Imaging Reporting and Data System [18].
All but one surveyed facility reported providing feedback at least annually to interpreting radiologists (Table 4). Three facilities failed to report the frequency of feedback to radiologists; the remainder reported providing feedback between one and four times per year. More than 80% of facilities generated audit reports that included the number of screening examinations, the number of diagnostic examinations, and the number of cancers diagnosed by each radiologist.
TABLE 4.
Radiologist Audit Reporting System
| Reporting Description | No. of Facilities (n = 45) | % of Total Facilities |
|---|---|---|
| Times per year audit data reported back to radiologist | ||
| 0 | 1 | 2 |
| 1 | 18 | 40 |
| 2 | 14 | 31 |
| 4 | 6 | 13 |
| Report given but number of times unknown | 3 | 7 |
| Audit report contained | ||
| No. of screening mammograms interpreted | 35 | 85 |
| No. of diagnostic mammograms interpreted | 35 | 85 |
| No. of sonograms obtained | 15 | 37 |
| No. of cancers diagnosed | 38 | 93 |
| Recall rate | 20 | 49 |
| Review of radiologist information | ||
| Radiologist-only meeting | 18 | 44 |
| Department meeting | 2 | 5 |
| Each radiologist alone | 16 | 39 |
| Department or facility manager meeting alone | 4 | 10 |
| Other | 12 | 29 |
| Computer-based radiologist information system | ||
| No | 11 | 24 |
| Yes | 32 | 71 |
Facilities responding to the survey matched U.S. mammography facilities in terms of geographic distribution, with 27% of study facilities located in zip codes identified as rural and 73% identified as urban, compared with 30% of all U.S. mammography facilities located in zip codes identified as rural and 70% in zip codes identified as urban [16, 17].
Discussion
The 1992 survey of mammography facilities by Houn and Brown [4] provides a useful touchstone for assessing changes in mammography practice during the past decade. In the prior survey, only 60% of facilities providing mammography services in the United States distinguished between screening and diagnostic mammography [4]. In our survey conducted a decade later, all facilities distinguished between these two services. In 1992, 20% of surveyed facilities used batch interpretation of screening mammograms [4]; a decade later, we found that 84% of facilities were using batch interpretation of screening mammograms. This striking change to batch interpretation of screening mammograms reflects the fact that batch interpretation is more time-efficient and cost-effective than interpreting screening examinations while patients wait for results.
The 1992 survey of mammography facilities found that 13.5% performed at high volume, 45.7% at medium volume, and 40.8% at low volume [4]. In 2002, 14.3% of facilities were performing mammography at high volume, 71.4% at medium volume, and 14.3% at low volume. This reflects a change over the past decade of 26% more facilities operating at medium volume and 26% fewer facilities operating at low volume, without a significant change in high-volume facilities.
During the past decade, the proportion of facilities having a computer-based medical audit system has nearly doubled, from 39% to 71%. In 1992, Medicare reimbursement for screening mammography was $55, whereas the mean total charge for screening mammography among facilities surveyed was $89 [4]. Applying a 3% per year inflation rate between 1992 and 2002, the 1992 Medicare charge would have increased to $74 and the mean facility charge would have been $119 in 2002. In 2002, Medicare actually reimbursed $69.23 for screening mammography, whereas the mean total charge for screening mammography among facilities surveyed in 2002 was $145.29, slightly greater than twice the Medicare reimbursement. This increase in the difference between charges and reimbursement rates over the past decade is due to the increased difference between costs and reimbursement rates during this same period. These cost data reflect the continuing problems that facilities and radiologists face in providing mammography services [19].
Newer technical innovations such as computer-aided detection (CAD) systems and digital mammography became available for clinical use in mammography relatively recently: CAD was first approved for use with screening mammography by the U.S. FDA in 1998; digital mammography was first approved in 2000. Our survey showed that in 2002, only five screening sites (11%) were using CAD and only two screening sites (5%) were using digital mammography, indicating that the diffusion of these new breast imaging technologies is not occurring rapidly.
Half (51%) of screening facilities surveyed reported that radiologists performed some type of double interpretation of screening mammograms, with 11% of screening facilities performing double interpretation of all screening mammograms. Sites performing double interpretation of a subset of screening mammograms reported doing so in 2–30% of cases, with the average fraction of cases double-interpreted being between 6.5% (median) and 13.4% (mean).
More than half of responding diagnostic mammography facilities reported using some type of double interpretation for diagnostic mammograms, with two sites (6% of diagnostic sites) reporting double interpretation of all diagnostic mammograms. Among the 17 sites reporting double interpretation of diagnostic mammograms, the fraction of cases double-interpreted ranged from 1% to 80%, with an average fraction of diagnostic cases double-interpreted being between 5% (median) and 12% (mean). To our knowledge, these rates for screening and diagnostic mammography are the first reported rates of double interpretation in the United States. Note the wide range of rates of double interpretation and the lack of standardization in methods of double interpretation reported by surveyed facilities (Fig. 3).
Strengths of this study are that the facilities surveyed constitute a varied cross-section, both geographically and demographically, of facilities providing screening mammography services. One NBCSC group is a large health plan, another serves approximately 90% of women in a primarily rural state, and the third serves approximately half of the women in a large metropolitan area. Another strength is that data are relatively recent, having been collected between late 2001 and mid 2002.
A potential weakness of this study is that the surveyed facilities were not a random sample of all facilities in the United States but an inclusive sample of facilities participating in the NBCSC in three distinct locations. Therefore, the facilities surveyed may not be representative of U.S. mammography facilities. Because of their participation in the NBCSC, surveyed sites may have more feedback about their performance and higher levels of quality assurance than typical mammography facilities.
In conclusion, facilities providing screening mammography services in the United States have changed dramatically during the past decade. Most facilities providing screening services are non-hospital-based multiservice radiology practices. Most provide on-site, batch interpretation of screening mammograms. Few surveyed sites use new technical innovations such as digital mammography (5%) or CAD (11%). Approximately 15% of screening mammography examinations and 10% of diagnostic mammography examinations were double-interpreted, with wide site-to-site variations in the rates and methods of double interpretation.
Acknowledgments
This project was supported by Public Health Service grant HS-10591 from the Agency for Healthcare Research and Quality, and the National Cancer Institute, National Institutes of Health and the Department of Health and Human Services (J. Elmore, Principal Investigator). We are also grateful for support from the Lynn Sage Breast Cancer Research Foundation. We would like to thank the staff of each participating mammography facility.
References
- 1.International Agency for Research on Cancer. Breast cancer screening. Vol. 7. Lyon, France: IARC Press; 2002. Handbooks of cancer prevention. [Google Scholar]
- 2.The Mammography Quality Standards Act (Public L No. 102–539), October 27, 1992
- 3.Ballard-Barbash R, Taplin SH, Yankaskas BC, et al. Breast Cancer Surveillance Consortium: a national mammography screening and outcomes database. AJR. 1997;169:1001–1008. doi: 10.2214/ajr.169.4.9308451. [DOI] [PubMed] [Google Scholar]
- 4.Houn F, Brown ML. Current practice of screening mammography in the United States: data from the National Survey of Mammography Facilities. Radiology. 1994;190:209–215. doi: 10.1148/radiology.190.1.8259406. [DOI] [PubMed] [Google Scholar]
- 5.Thurfjell EL, Lernevall K, Taube AAS. Benefit of independent double reading in a population-based mammography screening program. Radiology. 1994;191:241–244. doi: 10.1148/radiology.191.1.8134580. [DOI] [PubMed] [Google Scholar]
- 6.Ciatto S, Rosselli del Turco M, Morrone D, et al. Independent double reading of screening mammograms. J Med Screen. 1995;2:99–101. doi: 10.1177/096914139500200209. [DOI] [PubMed] [Google Scholar]
- 7.Taplin SH, Rutter CM, Elmore JG, Seger D, White D, Brenner RJ. Accuracy of screening mammography using single versus independent double interpretation. AJR. 2000;174:1257–1262. doi: 10.2214/ajr.174.5.1741257. [DOI] [PubMed] [Google Scholar]
- 8.Harvey SC, Geller B, Oppenheimer RG, et al. Increase in cancer detection and recall rates with independent double reading of screening mammography. AJR. 2003;180:1461–1467. doi: 10.2214/ajr.180.5.1801461. [DOI] [PubMed] [Google Scholar]
- 9.Ballard Barbash R, Klabunde C, Paci E, et al. Breast cancer screening in 21 countries: delivery of services, notification of results and outcomes ascertainment. Eur J Cancer Prev. 1999;8:417–426. doi: 10.1097/00008469-199910000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Taplin SH, Mandelson MT, Anderman C, et al. Mammography diffusion and trends in late-stage breast cancer: evaluating outcomes in a population. Cancer Epidemiol Biomarkers Prev. 1997;8:625–361. [PubMed] [Google Scholar]
- 11.Taplin SH, Rutter CM, Finder C, Mandelson MT, Houn F, White E. Screening mammography: clinical image quality and the risk of interval breast cancer. AJR. 2002;178:797–803. doi: 10.2214/ajr.178.4.1780797. [DOI] [PubMed] [Google Scholar]
- 12.Poplack SP, Tosteson AN, Grove MR, Wells WA, Carney PA. Mammography in 53,803 women from the New Hampshire mammography network. Radiology. 2000;217:832–840. doi: 10.1148/radiology.217.3.r00dc33832. [DOI] [PubMed] [Google Scholar]
- 13.Carney PA, Goodrich ME, O’Mahony D, et al. Mammography in New Hampshire: characteristics of the women and the exams they receive. J Community Health. 2000;25:183–198. doi: 10.1023/a:1005151914471. [DOI] [PubMed] [Google Scholar]
- 14.Carney PA, Poplack SP, Wells WA, Littenberg B. The New Hampshire Mammography Network: the development and design of a population-based registry. AJR. 1996;167:367–372. doi: 10.2214/ajr.167.2.8686606. [DOI] [PubMed] [Google Scholar]
- 15.Hendrick RE, Chrvala CA, Plott CA, Wilcox-Buchalla P, Jessop N, Cutter GA. Improvement in Mammography Quality Control, 1987–1995. Radiology. 1998;207:663–668. doi: 10.1148/radiology.207.3.9609888. [DOI] [PubMed] [Google Scholar]
- 16.University of Washington. WWAMI Rural Health Research Center. [Accessed December 8, 2004];The use of RUCAs [rural-urban commuting area codes] in health care. Available at: www.fammed.washington.edu/wwamirhrc/
- 17.Morrill R, Cromartie J, Hart LG. Metropolitan, urban, and rural commuting areas: toward a better depiction of the U.S. settlement system. Urban Geog. 1999;20:727–748. [Google Scholar]
- 18.American College of Radiology. Breast imaging reporting and data system: BI-RADS atlas. 4. Reston, VA: American College of Radiology; 2003. [Google Scholar]
- 19.Enzmann DR, Anglada PM, Haviley C, Venta LA. Providing professional mammography services: financial analysis. Radiology. 2001;219:467–473. doi: 10.1148/radiology.219.2.r01ma18467. [DOI] [PubMed] [Google Scholar]


